Abstract
Percutaneous vertebroplasty is an efficient procedure to treat pain due to osteoporotic vertebral compression fractures. However, refracture of cemented vertebrae occurs occasionally after vertebroplasty. It is unclear whether such fractures are procedure-related or part of the natural course of osteoporosis. The effect of potentially important covariates on refracture risk in cemented vertebrae has not been evaluated previously. We retrospectively analyzed the incidence and possible causative mechanism of refracture in patients who had received only one vertebroplasty for a single level of vertebral compression fracture. We assessed the following covariates: age, sex, body weight, height, lumbar spine bone mineral density, treated vertebral level, pre-existing untreated vertebral compression fracture, and gas-containing vertebrae before treatment. Surgical variables, including surgical approach, cement injected, and anterior vertebral height restoration, were also analyzed. Anti-osteoporotic treatment after surgery was recorded. Multiple logistic regression analysis was used to determine the relative risk of refractures of cemented vertebrae. Over all, 98 patients were evaluated with a mean follow-up of 26.9 ± 12.4 months (range, 7–55 months). We identified 62 refractures and the mean loss of anterior vertebral height was 13.3% (range 3.2–40.3%). The greater the anterior vertebral height obtained from vertebroplasty, the greater the risk of refracture occurring (P < 0.01). Gas-containing vertebrae were also prone to refracture after the procedure (P = 0.01). Anti-osteoporotic treatment was of borderline significance between refractured and non-refractured vertebrae (P = 0.07). Only restoration of anterior vertebral height was positively associated with refracture during the follow-ups (P < 0.01). In conclusion, refractures of cemented vertebrae after vertebroplasty occurred in 63% of osteoporotic patients. Significant anterior vertebral height restoration increases the risk of subsequent fracture in cemented vertebrae.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Percutaneous vertebroplasty has been demonstrated to relieve pain in symptomatic osteoporotic vertebral compression fracture safely and effectively [11, 18, 22]. By percutaneous injection of bone cement, these fractures were stabilized and the vertebrae strengthened [1]. Aside from rapid pain improvement, the immediate effect was an increase of anterior vertebral height (AVH) reported in some studies [10, 23, 30]. The presence of an intraosseous vacuum cleft represented a situation well suited to vertebroplasty and was associated with significant AVH increase after initial vertebroplasty [30]. The restoration of AVH reduced the wedge angle of the vertebra and kyphosis in patients [30]. The realigned spinal column and regained height in the fractured vertebra may decrease pulmonary and gastro-intestinal complications and early morbidity related to compression fractures [9].
Progressive kyphosis in osteoporotic patients usually results from new vertebral compression fractures and further collapse of previously fractured vertebrae. The occurrence of new vertebral compression fractures in the untreated vertebral bodies after vertebroplasty has been found and widely discussed. Multiple covariate analysis, such as patient characteristics and procedural techniques, has been used to identify risk factors for development of new vertebral compression fractures [2, 12, 13, 17, 32]. A greater degree of height restoration in cemented vertebrae was proved to increase the fracture risk in adjacent vertebrae after vertebroplasty [12].
In our clinical work, refracture of cemented vertebrae also occurs after vertebroplasty. Whether or not vertebroplasty can avoid further collapse of cemented vertebrae remains uncertain. It is also unclear whether such fractures are procedure-related or part of the natural course of osteoporosis. The effect of potentially important covariates on refracture in cemented vertebrae has not been evaluated. In this study, we retrospectively assessed the incidence and possible causative mechanism of refracture in cemented vertebrae in 98 patients with osteoporotic vertebral compression fractures treated with percutaneous vertebroplasty.
Materials and methods
Patients
Between October 2001 and January 2005, we performed percutaneous vertebroplasty in 163 vertebral bodies for 137 patients at a tertiary referral center. Osteoporotic patients were selected to receive vertebroplasty if they had severe vertebral fracture pain with failure of medical treatment. Pre-vertebroplasty radiographic evaluation of the patients included plain radiographs and magnetic resonance imaging (MRI) for all patients. The exclusion criteria for vertebroplasty were the following: (1) obvious compromise of the spinal canal by the protruded fragments with neurological signs; (2) collapse of the vertebral body with a residual height less than 10% making needle placement into the vertebral body difficult. All patients signed an informed consent at the time of vertebroplasty.
Vertebroplasty technique
The vertebroplasty procedure was performed according to the technique described by Jensen et al. [11]. Patients were placed in the prone position on the examination table and the procedure performed under intravenous conscious sedation with 25 mg diazepam (Dupin, China Chemical and Pharmaceutical, Taipei, Taiwan), and 15–30 mg of codeine for pain control, with 25-mg meperidine (both from National Bureau of Controlled Drugs, Department of Health, Taipei, Taiwan) administered intravenously if the latter was insufficient. An 11-G bone marrow biopsy needle (Hakko Electric Machine Works Co., Nagano, Japan) was used to puncture the collapsed vertebral body through either site of the pedicles, and the needle advanced to the anterior third of the vertebral body under bi-plane fluoroscopic guidance. Bone cement was prepared by mixing the copolymer powder with the monomer polymerization liquid (OsteoBond, Zimmer, Warsaw, IN, USA). The cement was injected into the vertebral body under fluoroscopic monitor and the procedure immediately terminated if any of the following was observed: (1) cement reaching the posterior fourth of the vertebral body; (2) cement migrating to drainage veins; or, (3) significant leakage into the disc space. If only ipsilateral bony trabeculae were opacified, the contralateral pedicle approach was ensued. After the procedure, plain radiographs of each treated vertebral level were assessed to ensure there was no unexpected or undesirable migration of cement.
Inclusion and exclusion criteria for analysis
Only patients previously treated with one vertebroplasty for a single level of compression fracture were enrolled in the study. For patients undergoing more than one vertebroplasty, those vertebral bodies treated initially were analyzed. All radiographs, including pre-, post-vertebroplasty and those taken more than 6 months after the procedure, were obtained with the patient in the supine position. Patient without available radiographs were not included in the study. Radiographs with low quality or malposition for comparison were also excluded by an experienced radiologist prior to analysis. The height of the anterior border of the collapsed vertebral body was measured using standard methods [30]. To correct the possible differences in magnification ratio on the radiographs acquired before and after vertebroplasty, the ratio of the height of the collapsed vertebral body at the anterior border on the lateral view to that of the posterior border of an adjacent normal vertebral body was used as reference. After careful discussion between authors to avoid any biases from cement protrusion, measurement of AVH was performed by one radiologist. The lines for measurement were stored and confirmed by another radiologist. Differences of AVH within 1 mm were considered unchanged [10] to avoid biases from technical factors or inappropriate measurement.
Retrospective data collection
Patients were divided into two groups: those with and those without AVH loss. Anterior vertebral height loss (HL) was defined as more than 1 mm decrease of AVH between post-procedure and follow-up. Patient demographics including age, sex, body weight, height, and lumbar spine bone mineral density (BMD) were recorded at the time of surgery. Lumbar spine BMD was measured before operation and at the time of follow-up by dual energy X-ray absorptiometry (Hologic Delphi A). Parameters related to the selection of the vertebral body for treatment were considered, including: vertebral level of compression fracture; presence of older untreated compression fractures; gas content in the vertebra before treatment; whether the surgical approach was through the pedicle (uni- or bilateral); and the amount of cement injected. Vertebrae were categorized into two groups: vertebrae at the thoracolumbar junction (from T10 to L2) and vertebrae outside the thoracolumbar junction (from T4 to T9 or L3 to L5). Gas-containing vertebrae were defined as “bony cleft” if the radiographs or MRI revealed air or fluid within the vertebrae.
Treatment of osteoporosis after surgery was recorded, including use of 70 mg/week alendronate (Fosamax, Merck & Co. Inc, Whitehouse Station, NJ, USA) or 60 mg/day raloxifene (Evista, Eli Lilly & Co., Indianapolis, IN, USA). The duration of treatment and follow-up was calculated at the time of review.
Statistical analysis
Descriptive statistics were expressed as mean ± standard deviation (SD) for continuous variables, and as percentages for categorical variables. The clinical data, including gender, vertebral level of compression fracture, presence of older untreated compression fractures, gas content in the vertebra and surgical approach between the two patient groups (HL and no HL) were analyzed by means of Chi-square test or Fisher’s exact test. The mean age, body weight, height, lumbar spine BMD, the amount of cement injected, AVH restoration after procedure, length of follow-up, and length of anti-osteoporotic treatment were analyzed by Mann–Whitney test. Stepwise logistic regression was used in evaluating the relationships between clinical factors and HL, with adjustments made for other potential confounding factors.
Refracture of the cemented vertebra may lead to lower AVH even without treatment of vertebroplasty; therefore, the HL group was further categorized into two subgroups: additional height loss (aHL) and no aHL. Differences between the two subgroups were assessed using the same aforementioned method. A P-value of <0.05 was considered as significant. Corresponding 95% confidence limits (CI) were calculated with confidence interval estimation. All analyses were conducted using SAS (1990; SAS Statistical Institute, Cary, NC, USA).
Results
Thirty-nine out of 137 patients were excluded from our study (21 previously treated for more than one vertebral compression fracture, 12 patients without qualified radiographs for analysis and 6 patients lost to follow-up). Ninety-eight patients (90 women, 8 men, mean age 72.6 ± 6.9 years) met study inclusion criteria. Patients were followed after vertebroplasty for a mean of 26.9 ± 12.4 months (range 7–55 months). Fourteen (14.3%) of 98 patients were followed for 6–12 months, 43 (29.6%) were followed for 13–24 months, and 55 (56.1%) were followed for more than 24 months.
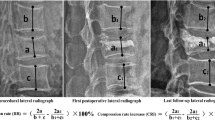
Sixty-two patients (63%) experienced AVH loss (Fig. 1). The mean AVH loss was 13.3% (range 3.2–40.3%). Patients with and without HL were followed for a mean of 23.51 ± 11.9 months (range 7–55 months) and 29.7 ± 11.2 months (range 13–49 months), respectively (P = 0.34). Patient demographics, stratified by the presence or absence of HL, are summarized in Table 1. Restoration of AVH after initial vertebroplasty and gas-containing vertebrae pre-treatment were significantly different between those patients with and without HL during the follow-ups (P < 0.01 and P = 0.01).
Sixty-two year-old female. a Preoperative sagittal T2-weight image shows gas-filled fracture cleft in L2 vertebra. b Postoperative lateral radiograph shows considerable increase in anterior vertebral height. c Radiograph 16 months after procedure shows refracture of the cemented vertebra with focal kyphosis
Refracture risk increased if a greater amount of AVH was gained from the vertebroplasty. Patients with HL had a mean 15.1% (range 1.5–58.8%) of vertebral height restored, whereas patients without HL had a mean 8.0% (range 0–31.9%) of height restored after surgery. Gas-containing vertebrae were significant for increased refracture risk (P = 0.01). Before the procedure, 41/98 patients had gas-containing vertebrae. Thirty-two (52%) of 62 vertebrae and 9 (25%) of 36 vertebrae within the HL and the no HL groups were gas-containing, respectively.
Anti-osteoporotic treatment can increase bone mass and reduce refracture risk in osteoporotic patients. The mean length of time for anti-osteoporosis therapy was 11.2 ± 7.4 months for patients with HL versus 16.8 ± 12.9 for the no HL group. Borderline statistical significance for anti-osteoporosis treatment was noted between the refractured and non-refractured vertebrae (P = 0.07). The mean amount of cement injected was not significantly different between the two groups (5.7 ± 2.3 ml versus 5.7 ± 3.1 ml; P = 0.56).
Variables, including restoration of AVH, gas-containing and post-vertebroplasty anti-osteoporosis treatment, were used in the stepwise logistic regression analysis. The results revealed that only restoration of AVH was positively associated with HL during the follow-ups (P < 0.01, OR = 1.07, 95% CI = 1.019–1.122). The risk of HL increased by 7-fold for each percentage of AVH increase after vertebroplasty.
During the follow-ups, residual AVH remained higher than pre-surgery AVH and stationary AVH in 46 (46.9%) and 29 (29.6%) of 98 patients, respectively. Additional AVH loss was found in the other 23 (23.5%) patients. Patient characteristics with and without aHL are summarized in Table 2. There were three (13.0%) patients with more than 20% additional loss of AVH, eight (34.8%) with 10–20% additional loss and 12 (52.2%) with less than 10% additional loss. The significant risk factors for aHL and no aHL were AVH restoration after procedure and AVH loss during the follow-ups. Patients with aHL had 6.5% of vertebral height restored, whereas patients without aHL had 20.3% of height restored (P < 0.01). In contrast, patients with aHL had a 17.9% vertebral height loss, whereas patients without aHL had 10.8% height loss (P < 0.01) during the follow-ups. Multiple logistic regression analysis showed that restoration of AVH was the only variable (P < 0.01, OR = 0.83, 95% CI = 0.75–0.92) negatively associated with aHL during the follow-ups. The amount of cement injected was not significantly different between the two subgroups. Neither gas-containing vertebrae nor the length of time for anti-osteoporosis treatment were statistically significant.
Discussion
AVH restoration after vertebroplasty is well known [10, 23, 30]. From the previous literatures, the reported range of vertebral height restorations from vertebroplasty was 2.5–8.4 mm, or 16.7–28.6% increase from the reference or normal vertebral height [10, 21, 23, 30]. In vertebrae with intraosseous vacuum cleft, the effect of AVH restoration was more prominent than in non-cleft vertebrae. In our study, the mean AVH restoration in all vertebrae was 12.5 ± 12.2%. The gas and the non-gas group were 16.3 ± 13.7% and 7.6 ± 9.0%, respectively. The result is comparable to the literatures reported.
Although, the effect of vertebroplasty is remarkable, whether or not the restored AVH can be maintained has rarely been mentioned or discussed before. Dansie et al. [5] reported an 18% vertebral height loss in 51 treated vertebrae after vertebroplasty. Some authors even reported no further collapse of cemented vertebrae after 5 years of follow-up [27]. In contrast, we found an extremely high rate of AVH loss in 63% of patients in our study. Dansie et al. [5] used mid-sagittal MRI while we used supine radiographs for AVH measurement. Since the final configuration of the injected cement was unpredictable, meaningful AVH calculation was controversial. In many instances, the vertebral height loss involved only part of the endplate and may not be representative on the mid-sagittal images. Although, it is possible to underestimate the refracture rate by using mid-sagittal MRI, one problem is that vertebral height measured on one radiograph may not be the same when measured on a second radiograph because of magnification error. However, reported height change relative to a referent vertebral height is indifferent to the issue of measurement accuracy yet allow for comparison between radiographs and between published radiographic studies as long as the precision error of the measurement is acceptable [23].
Low bone mineral density may also be contributive. Since vertebroplasty is performed on individuals with serious osteoporosis, a higher re-collapse rate would be expected over time. The average interval from the vertebroplasty to the follow-up MRI in the Dansie study was 150 days (range 2–736 days, median 81 days). Our follow-up period was longer (mean 26.9 ± 12.4 months, range 7–55 months); therefore, the re-collapse rate would reasonably be higher than in Dansie’s study.
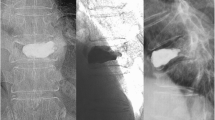
Our 63% refracture rate in cemented vertebral bodies suggests vertebroplasty cannot prevent the development of AVH loss. Patients lost more AVH during the follow-ups if they gained more AVH restoration from the initial vertebroplasty. Cleft vertebrae always gained more AVH restoration which suggests that osteonecrosis or poor healing of compressed structures may play an important role [10, 20, 30]. These vertebrae demonstrate dynamic or mobile endplate, which serves as a potential space for cement deposition [24]. Since pain relief was the major goal of vertebroplasty, we performed vertebroplasty with cement to seal off the potential fracture region instead of filling all the bone marrow. It is possible to have left some unfilled space during the procedure, although the amount of cement injected in our study is similar to other studies [4, 6, 16]. Although not in the final equation of logistic regression analysis, more gas-containing vertebrae were noted in the HL group (Table 1). We believe if the vertebrae are filled inadequately, these residual unfilled spaces within vertebrae may lead to collapse of the vertebral body or loosening of cement during the follow-ups. Our clinical results also showed that the cleft was usually located in the superior portion of the vertebra in the gas-containing vertebral body. This space is normally filled with cement by the surgeon. However, without filling the lower portion of the vertebrae, the follow-up examinations showed osteoporotic trabeculae underneath squashed by the cement contained in the upper portion (Fig. 2).
Liebschner et al. [16] found that volume fractions of bone cement less than 15% were sufficient to restore stiffness to pre-damage levels in some cases. Molloy et al. [25] reported that restoration of strength and stiffness of the vertebral body required cement fillings of 16.2 and 29.8%, respectively. However, the effect of asymmetric cement distribution has not been well investigated. Theoretically, if vertebroplasty can reinforce the original strength of the vertebral body with a small amount of cement, it should prevent the collapse of the vertebral body. However, our results indicate that while this amount can restore some strength and stiffness to osteoporotic vertebral bodies, regional cement deposition is not pliable enough to withstand the pressures encountered in everyday life.
The transferred load on the vertebral body after the procedure may lead to this problem. Polikeit et al. [28] reported that the filling of a vertebral body with bone cement leads to a load shift toward the anterior column, which increases endplate bulge and transfers the pressure to adjacent vertebrae. Therefore, the load transfer results in a new vertebral compression fracture. The pressure resulting from the filled rigid cement can cause adjacent compression, and may also damage the marrow trabeculae of the unfilled area in the same vertebral body, especially if these vertebrae are fragile. When a more advanced technique becomes available, we suggest the surgeon consider filling the vertebra more completely, which may slow down AVH loss. However, as our findings are based on a retrospective study, there is a limitation to the interpretation of these results. A prospective study would be a better investigation of the relationship between re-collapses of cemented vertebrae and cement distribution, especially in cleft vertebrae.
As compared to pre-procedure radiographs, 23.5% of treated vertebrae developed further collapse after the procedure. Those vertebrae showing additional AVH loss had less AVH restoration after surgery and higher AVH loss during the follow-ups (Table 2). In contrast, the group showing no additional vertebral height loss actually had more vertebral height restoration right after vertebroplasty than the group with additional vertebral height loss 7 months after procedure. It is plausible that greater AVH restoration has a greater chance of avoiding deterioration and focal kyphosis. However, Kim et al. [12] and our unpublished data reveal that the risk of new adjacent vertebral compression fractures were positively correlated with AVH restoration. We do not wish to overemphasize the significance of this benefit from vertebroplasty. Since vertebroplasty could not prevent further collapse of vertebrae and may increase the risk of new adjacent compression fractures if AVH has been overcorrected, anti-osteoporotic therapy rather than over-AVH restoration may be better for long-term height stability.
In patients with compression fractures due to osteoporosis, the risk of new vertebral compression fracture is higher even without percutaneous vertebroplasty [29]. The annual incidence of vertebral compression fracture in patients conservatively treated is approximately 20% [19]. Since osteoporotic vertebral compression fracture can cause a collapse of other vertebral bodies, it usually provokes a cascade of fractures. Since there was no significant difference in BMD or presence of older untreated compression fractures noted between the HL and the group without HL, AVH loss would correlate with post-procedure medical treatment. Anti-resorptive agents can effectively increase bone mass in osteoporotic patients [3, 8, 15]. Both alendronate and raloxifene have been proven to reduce the frequency of clinical vertebral fractures in osteoporotic patients with or without existing vertebral fracture [3, 7]. The mean loss of vertebral height after 3 years of treatment was also less in the alendronate group than in the placebo group [15]. In our study, there was a trend toward statistical significance for anti-osteoporosis treatment (P = 0.07), which suggests that further increase in bone mass after vertebroplasty may avoid further collapse of cemented vertebrae. However, it is impossible to conclude any benefit of single or combination of anti-osteoporosis therapy after vertebroplasty from this retrospective study. Further investigation should emphasize patient selection, the dose and formulation of anti-osteoporosis therapy and outcome measurements.
We question whether vertebral height restoration achieved after vertebroplasty matters. Lanea et al. [14] found a trend toward greater pain relief in patients with clefts that were opacified at the time of vertebroplasty. Peh et al. [26] achieved complete or partial pain relief in 78% of patients and no change in 22% of patients with intraosseous cleft vertebrae. In contrast, McKiernan et al. [21, 24] reported that partial AVH restoration did not result in additional pain relief or improved quality of life beyond cement fixation alone. They stated that patients with mobile and fixed fractures experience significant pain relief after vertebroplasty. Correlation between the initial vertebral height restoration and pain relief is controversial. It is also difficult to conclude the effect of AVH loss during follow-up from this retrospective study as there are limited literatures reported. Dansie et al. [5] believed progressive and persistent edema and interval height loss of vertebrae are so frequent that it should not be interpreted as evidence of ongoing pathology. Trout et al. [31] also reported a 33 and 21% subsequent fracture in vertebrae with and without intraosseous cleft. All the refractures were identified on the basis of imaging performed to evaluate worsening of symptoms or onset of new symptoms. Because scheduled radiographs were not obtained, subclinical fractures may have been missed in their study. We were not able to obtain all the pain relief data for all patients during their follow-ups and could not draw conclusions regarding pain relief and AVH loss and the long-term effect of AVH restoration. The clinical meaning of AVH is still unclear.
Conclusion
Refracture of cemented vertebrae is inevitable as it is evident in about 60% of our patients after vertebroplasty. Cemented vertebrae with greater AVH restoration are at higher risk for subsequent fracture. Although gas-containing vertebrae experienced obvious AVH restoration, overemphasizing the significance of this bonus effect from vertebroplasty is not expedient.
References
Belkoff SM, Mathis JM, Jasper LE et al (2001) The biomechanics of vertebroplasty: the effect of cement volume on mechanical behavior. Spine 26(14):1537–1541
Berlemann U, Ferguson SJ, Nolte LP et al (2002) Adjacent vertebral failure after vertebroplasty: a biomechanical investigation. J Bone Joint Surg Br 84(5):748–752
Black DM, Cummings SR, Karpf DB et al (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet 348(9041):1535–1541
Cotten A, Dewatre F, Cortet B et al (1996) Percutaneous vertebroplasty for osteolytic metastases and myeloma: effects of the percentage of lesion filling and the leakage of methyl methacrylate at clinical follow-up. Radiology 200(2):525–530
Dansie DM, Luetmer PH, Lane JI et al (2005) MRI findings after successful vertebroplasty. AJNR Am J Neuroradiol 26(6):1595–1600
Dean JR, Ison KT, Gishen P (2000) The strengthening effect of percutaneous vertebroplasty. Clin Radiol 55(6):471–476
Delmas PD, Genant HK, Crans GG et al (2003) Severity of prevalent vertebral fractures and the risk of subsequent vertebral and nonvertebral fractures: results from the MORE trial. Bone 33(4):522–532
Ettinger B, Black DM, Mitlak BH et al (1999) Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) Investigators. JAMA 282(7):637–645
Garfin SR, Yuan HA, Reiley MA (2001) New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine 26(14):1511–1515
Hiwatashi A, Moritani T, Numaguchi Y et al (2003) Increase in vertebral body height after vertebroplasty. AJNR Am J Neuroradiol 24(2):185–189
Jensen ME, Evans AJ, Mathis JM et al (1997) Percutaneous polymethylmethacrylate vertebroplasty in the treatment of osteoporotic vertebral body compression fractures: technical aspects. AJNR Am J Neuroradiol 18(10):1897–1904
Kim SH, Kang HS, Choi JA et al (2004) Risk factors of new compression fractures in adjacent vertebrae after percutaneous vertebroplasty. Acta Radiol 45(4):440–445
Komemushi A, Tanigawa N, Kariya S et al (2006) Percutaneous vertebroplasty for osteoporotic compression fracture: multivariate study of predictors of new vertebral body fracture. Cardiovasc Intervent Radiol 29(4):580–585
Lane JI, Maus TP, Wald JT et al (2002) Intravertebral clefts opacified during vertebroplasty: pathogenesis, technical implications, and prognostic significance. AJNR Am J Neuroradiol 23(10):1642–1646
Liberman UA, Weiss SR, Broll J et al (1995) Effect of oral alendronate on bone mineral density and the incidence of fractures in postmenopausal osteoporosis. The Alendronate Phase III Osteoporosis Treatment Study Group. N Engl J Med 333(22):1437–1443
Liebschner MA, Rosenberg WS, Keaveny TM (2001) Effects of bone cement volume and distribution on vertebral stiffness after vertebroplasty. Spine 26(14):1547–1554
Lin EP, Ekholm S, Hiwatashi A et al (2004) Vertebroplasty: cement leakage into the disc increases the risk of new fracture of adjacent vertebral body. AJNR Am J Neuroradiol 25(2):175–180
Lin WC, Chen SH, Cheng TT et al (2004) The role of imaging studies of percutaneous vertebroplasty in 63 patients with osteoporotic compression fracture: preliminary report. Chin J Radiol 29:177–184
Lindsay R, Silverman SL, Cooper C et al (2001) Risk of new vertebral fracture in the year following a fracture. JAMA 285(3):320–323
McKiernan F, Faciszewski T (2003) Intravertebral clefts in osteoporotic vertebral compression fractures. Arthritis Rheum 48(5):1414–1419
McKiernan F, Faciszewski T, Jensen R (2005) Does vertebral height restoration achieved at vertebroplasty matter? J Vasc Interv Radiol 16(7):973–979
McKiernan F, Faciszewski T, Jensen R (2004) Quality of life following vertebroplasty. J Bone Joint Surg Am 86-A(12):2600–2606
McKiernan F, Faciszewski T, Jensen R (2003) Reporting height restoration in vertebral compression fractures. Spine 28(22):2517–2521
McKiernan F, Jensen R, Faciszewski T (2003) The dynamic mobility of vertebral compression fractures. J Bone Miner Res 18(1):24–29
Molloy S, Mathis JM, Belkoff SM (2003) The effect of vertebral body percentage fill on mechanical behavior during percutaneous vertebroplasty. Spine 28(14):1549–1554
Peh WC, Gelbart MS, Gilula LA et al (2003) Percutaneous vertebroplasty: treatment of painful vertebral compression fractures with intraosseous vacuum phenomena. AJR Am J Roentgenol 180(5):1411–1417
Perez-Higueras A, Alvarez L, Rossi RE et al (2002) Percutaneous vertebroplasty: long-term clinical and radiological outcome. Neuroradiology 44(11):950–954
Polikeit A, Nolte LP, Ferguson SJ (2003) The effect of cement augmentation on the load transfer in an osteoporotic functional spinal unit: finite-element analysis. Spine 28(10):991–996
Rico H, Revilla M, Villa LF et al (1992) Crush fracture syndrome in senile osteoporosis: a nutritional consequence? J Bone Miner Res 7(3):317–319
Teng MM, Wei CJ, Wei LC et al (2003) Kyphosis correction and height restoration effects of percutaneous vertebroplasty. AJNR Am J Neuroradiol 24(9):1893–1900
Trout AT, Kallmes DF, Lane JI et al (2006) Subsequent vertebral fractures after vertebroplasty: association with intraosseous clefts. AJNR Am J Neuroradiol 27(7):1586–1591
Voormolen MH, Lohle PN, Juttmann JR et al (2006) The risk of new osteoporotic vertebral compression fractures in the year after percutaneous vertebroplasty. J Vasc Interv Radiol 17(1):71–76
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, WC., Lee, YC., Lee, CH. et al. Refractures in cemented vertebrae after percutaneous vertebroplasty: a retrospective analysis. Eur Spine J 17, 592–599 (2008). https://doi.org/10.1007/s00586-007-0564-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-007-0564-y