Abstract
The object of this study is to review the early clinical results and radiographic outcomes following insertion of the Bryan Cervical Disc Prosthesis (Medtronic Sofamor Danek, Memphis, TN), together with its effect on maintaining sagittal alignment of the functional spinal unit (FSU) and overall sagittal balance of the cervical spine for the treatment of single-level or two-level symptomatic disc disease. Forty-seven patients with symptomatic single or two-level cervical disc disease who received the Bryan Cervical Artificial Disc were reviewed prospectively. A total of 55 Bryan disc were placed in 47 patients. A single-level procedure was performed in 39 patients and a two-level procedure in the other eight. Radiographic and clinical assessments were made preoperatively and at 1.5, 3, 6, 9, 12, and 18 and up to 33 months postoperatively. Mean follow-up duration was 24 months, ranging from 13 to 33 months. Periods were categorized as early follow up (1.5–3 months) and late follow up (6–33 months). The visual analogue scale (VAS), neck disability index(NDI), Odom’s criteria were used to assess pain and clinical outcomes. Static and dynamic radiographs were measured by hand and computer to determine the range of motion (ROM), the angle of the functional segmental unit (FSU), and the overall cervical alignment (C2–7 Cobb angle). With all of these data, we evaluated the change of the preoperative lordosis (or kyphosis) of the FSU and Overall sagittal balance of the cervical spine during the follow-up period. There was a statistically significant improvement in the VAS score from 7.0 ± 2.6 to 2.0 ± 1.5 (paired-t test, P = 0.000), and in the NDI from 21.5 ± 5.5 to 4.5 ± 3.9 (paired-t test P = 0.000). All of the patients were satisfied with the surgical results by Odom’s criteria. The postoperative ROM of the implanted level was preserved without significant difference from preoperative ROM of the operated level. Only 36% of patients with a preoperative lordotic sagittal orientation of the FSU were able to maintain lordosis following surgery. However, the overall sagittal alignment of the cervical spine was preserved in 86% of cases at the final follow up. Interestingly, preoperatively kyphotic FSU resulted in lordotic FSU in 13% of patients during the late follow-up, and preoperatively kyphotic overall cervical alignment resulted in lordosis in 33% of the patients postoperatively. Clinical results are encouraging, with significant improvement seen in the Bryan Cervical Artificial disc. The Bryan disc preserves motion of the FSU. Although the preoperative lordosis (or kyphosis) of the FSU could not always be maintained during the follow-up period, the overall sagittal balance of the cervical spine was usually preserved.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
For the past 50 years, anterior cervical decompression and fusion (ACDF) has been the standard treatment of symptomatic cervical radiculopathy [5–7, 25]. However, there is clear evidence that the treatment of ACDF will increase the stress on the nonoperated discs and therefore, adversely impact the rate of adjacent disc degeneration which may be a result of the disease as well as the mechanical effects of the fusion treatment [2, 4, 9–11, 14, 16, 17, 24, 27].
Currently, the demand for a better solution in the treatment of symptomatic cervical radiculopathy beyond arthrodesis is universally increasing. The expected advantage of arthroplasty is its ability to restore and maintain the motion, segmental anatomy and function, while successfully treating the patient’s radicular symptoms.
The basis for arthroplasty is dependent on the altered mechanical forces being the key factor promoting the accelerated degenerative changes. A cervical arthroplasty demonstrates reduced stresses in the adjacent annulus compared with motion segments stabilized with fusion [28]. On the other hand, kyphotic deformity following anterior cervical discectomy and fusion has been implicated in the development of segmental instability, clinically significant adjacent-segment disease, and poor functional recovery.
The Bryan Cervical Disc Prosthesis is one of early ahead used cervical disc replacement designed to allow motion similar to the normal cervical spine functional unit (Fig. 1) [12, 13, 18]. However, because of its passive nature of design, that is, Bryan has smooth soft elastic polyurethane nucleus and relatively softer than any other types of polymer artificial disc, patients who underwent arthroplasty with a Bryan cervical artificial disc developed a focal loss of lordosis after surgery at the treated levels. Nevertheless, the overall sagittal alignment could maintain after insertion of the Bryan disc. The purpose of this study is to evaluate its effect on maintaining lordosis at the treated levels and overall sagittal alignment of the cervical spine after insertion of the Bryan disc during the follow-up period.
Clinical material and methods
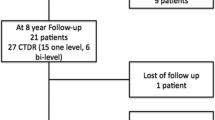
The study consisted of 47 patients with symptomatic single or two-level cervical disc disease who received the Bryan Cervical Artificial Disc prosthesis (Medtronic Sofamor Danek, Memphis, TN). A total of 55 Bryan disc were placed in 47 patients. A single-level procedure was performed in 39 patients and a two-level procedure in the other eight. The C4-5 level was treated in 9 patients, C5-6 was treated in 26 patients and C6-7 was treated in 20 patients. Since November 2003, information on clinical and radiographic outcomes after Bryan cervical arthroplasty has been collected prospectively. Mean follow up period was 24 months (range 13–33 months).
Forty-two of 47 patients presented with radiculopathy and five with myelopathy. The study group consisted of 30 men and 17 women. Their age ranged from 22 to 54 years. All patients were evaluated using static and dynamic cervical spine radiographs as well as MR imaging. Preoperative MR imaging was performed in all patients to determine the origin of radiculopathy and/or myelopathy.
All of them underwent anterior cervical discectomy followed by implantation of the Bryan artificial disc prosthesis, following the standard surgical technique with drilling and milling of endplates to a predetermined size (14–18 mm) [12]. All procedures were completed through a transverse skin incision made on the right side of the neck, and all procedures were performed by one surgeon (S. W. K).
Clinical evaluation included Odom’s criteria by the surgeon, visual analogue scale (VAS), and neck disability index (NDI) by the patient. Radiographic evaluation included static and dynamic flexion-extension lateral images in standing position. These were assessed preoperatively and postoperatively at 1.5, 3, 6, 9, 12, 18, 24 months and every 6 months thereafter until final follow-up at the surgeon’s clinic [21]. The pre- and postoperative segmental sagittal rotation (that is, ROM) in each spinal level was examined. Radiographic measurement data were collected from three observers. Each of them measured twice, and the mean value was used for analysis. Radiographs were analyzed to determine the sagittal range of motion (ROM) of the shell angle, defined as the angle of the disc space formed preoperatively by the natural endplates and postoperatively by the shells of the prosthesis, the functional spinal unit (FSU) angle, defined as the angle formed by lines drawn at the superior margin of the superior vertebral body and the inferior margin of the inferior body, and the Cobb angles from C2–7 to ascertain overall cervical alignment (Fig. 2). Periods were categorized as early follow-up (1.5–3 months) and late follow-up (6–33 months). Angles were measured using measurement analysis software (Mediface), which calculates the intersecting angle between two lines drawn by the investigator. In FSU or C2–7 alignment, curvatures were defined as follows; kyphosis: Cobb angle < 0, straight: 0 ≤ Cobb angle < 5, lordosis: Cobb angle ≥ 5.
Time points for postoperative radiographic follow-up evaluations were defined as early (1.5–3 months) and late (6–33 months). Paired t test was carried out with significance level of 0.05 using SPSS ver 12.0. No patient has been lost to follow up.
Results
Clinical and surgical outcome
All patients noted immediate improvement in preoperative symptomatology. On clinical assessment there was a statistically significant improvement in the VAS score from 7.0 ± 2.6 to 2.0 ± 1.5 (paired t test, P = 0.000), and in the NDI from 21.5 ± 5.5 to 4.5 ± 3.9 (paired t test P = 0.000) (Fig. 3). When surgical outcome was measured using Odom criteria, as assessed by the surgeon who had performed the operation, it was observed that most of the patients had a satisfactory outcome (excellent, good or fair) and no patient was allocated to ‘poor’ (Table 1), regardless of single-level or two-level prosthesis implantation. There was no evidence of complications such as heterotopic ossification during the follow-up period.
Clinical results of visual analogue scale (VAS) and neck disability index (NDI) in box plot. The preop VAS significantly decreased at early and late postop period (paired t test P = 0.000, P = 0.000 respectively) The preop NDI also significantly decreased at early and late postop period (paired t test P = 0.000, P = 0.000 respectively). Significant difference (P < 0.05) is indicated with an asterisk
Radiographic analysis
All patients demonstrated a good range of cervical motion on fluoroscopic screening at the final postoperative assessment.
Range of motion
Motion was preserved in all cases. The ROM of the implanted level by shell angle at early and late follow-up were not significantly different when compared with the immediate postoperative shell angle (P > 0.05) (Figs. 2, 4; Table 2). The ROM by disc space angle of upper level decreased at early follow up (paired t test, P < 0.05), but the decreased postoperative ROM was significantly recovered at late follow up (paired t test, P < 0.05) (Fig. 2, Fig. 4; Table 3). Also, the ROM by disc space angle of lower level decreased at early follow up (paired t test, P < 0.05), but the decreased postoperative ROM was significantly recovered at late follow up (paired t test, P < 0.05). However, the late follow up recovery (values) did not reach the preoperative measurements (paired t test, P < 0.05) (Figs. 2, 4; Table 3). The ROM by Cobb angle of the FSU decreased at early follow up (paired t test, P < 0.05), but the decreased early ROM was significantly recovered at late follow up (paired t test, P < 0.05) (Figs. 2, 5; Table 4). The overall cervical ROM by Cobb angle of C2–7 decreased at early follow up (paired t test, P < 0.05), but the decreased early ROM was significantly recovered at late follow up (paired t test, P < 0.05). The late follow up data was not significantly different form the preoperative measurements (paired t test, P > 0.05) (Figs. 2, 5; Table 4).
ROM of the implant level (ShROM), upper adjacent level (UpROM), and lower adjacent level (LwROM) were measured on periods of preop, early (1.5–3 months) and late (6–33 months) follow up (ShROMPeriod, UpROMPeriod, and LwROMPeriod, respectively). The shell ROM, which was compared with immediate postoperative period, was preserved at early and late periods (paired t test P(preop-early) = 0.645, P(early-late) = 0.287, P(preop-late) = 0.949, respectively). Both upper and lower disc space angle decreased at early follow up (paired t test P(preop-early) = 0.000), which was recovered significantly at late follow up (paired t test P(early-late) = 0.009). However, they were not recovered to pre operative level (paired t test P(preop-late) = 0.005)
The ROM of functional spinal unit (FSROM) and the overall cervical (C2–7) alignment (OvROM) were measured on periods of preop, early, and late follow up (FSROMPeriod, and OvROMPeriod). Both FSU and overall cervical alignment decreased significantly at early follow up (paired t test FSU: P(preop-early) = 0.001, C2–7: P(preop-early) = 0.006, respectively), but was recovered significantly at late follow up (paired t test FSU: P(early-late) = 0.001, C2–7: P(early-late) = 0.21, respectively). In both FSU and C2–7 measurements, late follow up was significantly not different from the preoperative measurements (paired t test FSU: P(preop-late) = 0.223, C2–7: P(preop-late) = 0.071, respectively)
Maintenance of curvature
The preoperative lordosis (or kyphosis) of the FSU and overall cervical (C2–7) alignment was not maintained during the follow up period (Fig. 6). Most of the change occurred between preoperative and early follow-up assessments, with little change between early and late follow-up review.
Change in the FSU Angle (Table 5)
-
1.
Patients with segmental lordosis (FSU ≥ 5°) preoperatively at the treated levels. Of 28 patients with segmental lordotic alignment preoperatively, 19 patients (68%) remained lordotic at the treated levels in early follow-up evaluations. Among these 19 patients who maintained segmental lordotic alignment in early follow-up evaluations, 10 patients remained lordotic at the treated levels in late follow-up evaluations. Only 36% of patients with segmental lordosis preoperatively remained segmental lordotic alignment at the treated levels in late follow-up evaluations.
-
2.
Patients with segmental straight FSU (0°≤ FSU < 5°) preoperatively at the treated levels. Of 11 patients with preoperative segmental straight alignment, 3 patients (27%) continued to be straight, 6 patients (55%) became lordotic, and 2 patients (18%) became kyphotic alignment at the treated levels in early follow-up evaluations. Among these 3 patients who maintained their segmental straight alignment during early follow-up, all of these three patients remained straight at the treated levels during late follow up. Only 27% of patients with a preoperative segmental straight alignment continued to have a segmental straight alignment at the treated levels during late follow up. Interestingly, 6 patients who became kyphotic at early follow-up evaluations, 4 patients (67%) remained segmental lordotic alignment at the treated levels during late follow up.
-
3.
Patients with segmental kyphosis (FSU < 0°) preoperatively at the treated levels. Of eight patients with segmental kyphotic alignment preoperatively, the segmental alignment became kyphotic in five patients (63%), and the other three patients became straight (24%) or lordotic (13%) in early follow-up evaluations. Among these five patients who had segmental kyphotic alignment in early follow-up evaluations, four patients remained kyphotic at the treated level in late follow-up evaluations. Fifty percent of patients with segmental kyphotic alignment preoperatively remained segmental kyphotic alignment at the treated level in late-follow up evaluations. One patient (13%) who were turned out to be lordotic at early follow up remained lordotic at late follow up.
Change in the overall cervical alignment (C2–7 Cobb angle) (Table 6)
The Cobb angle varied widely during follow-up period. Most of the change occurred between preoperative and early follow-up assessments, with little change between early and late follow-up review.
-
1.
Patients with overall cervical lordotic alignment (defined as ≥ 5°) preoperatively. In 42 patients with lordotic alignment preoperatively, the spinal alignment in 38 patients (90%) remained lordotic in early follow-up evaluations. Of 38 patients with lordotic alignment in early follow-up evaluations, the alignment in 36 patients maintained lordotic alignment in late follow-up evaluations. Therefore, 86% of the patients with lordotic alignment preoperatively exhibited lordotic alignment in late follow-up evaluations.
-
2.
Patients with overall cervical straight alignment (defined as 0 ≤ Cobb angle < 5) preoperatively. In two patients with preoperative straight alignment, the spinal alignment in one patient (50%) remained straight and one patient (50%) became lordotic in early follow-up evaluations. These alignments were maintained until late follow up.
-
3.
Patients with overall kyphotic alignment (defined as < 0) preoperatively. Of three patients with kyphotic alignment preoperatively, the alignment in one (33%) became kyphotic in early follow-up evaluations, whereas the other one was straight, and the last one was lordotic. These spinal alignments in early follow-up evaluations were maintained until late follow-up evaluations. Interestingly, one patients exhibited lordotic alignment in early follow-up evaluations, which remained lordotic in late-follow up evaluations. Thirty-three percent of patients with kyphotic alignment preoperatively exhibited lordotic alignment in late follow-up evaluations.
Discussion
Numerous authors have suggested that anterior cervical discectomy and fusion may alter the natural history of cervical spondylosis and hasten the development of degenerative changes at levels immediately above and below a fusion [2, 4, 9–11, 14, 16, 24, 27]. Patients who have undergone ACDF may display radiographic and clinical evidence of progressive degeneration. Long-term radiographic follow-up review in patients with ACDF has demonstrated hypermobility and degenerative changes in the nonfused segments of the spine, including disc space narrowing, endplate sclerosis, and osteophyte formation [2, 4, 9–11, 14, 16, 24, 27]. Although several authors have demonstrated radiographic degeneration with no clinical correlation, Gore and Sepic [15] found an association between recurrent cervical pain and progression of spondylosis.
Nevertheless, the concept of adjacent-segment disease remains unproven and the true incidence of adjacent-segment disease remains a controversial issue. Also, there are the risks of adjacent segment disease to be considered. This has been observed in approximately 3% of patients in a retrospective long-term follow-up study, with a predicted prevalence at 10 years of approximately 25% [16]. However, there is little data in the literature at this time to support this theory. More importantly, there are no natural history studies yet available to demonstrate a difference between the likelihood of adjacent segment disease between ACDF, cervical disc arthroplasty and nonoperated yet symptomatic cervical spondylosis.
However, it is clear that fusion alters spinal biomechanics. Biomechanical modeling of the cervical spine has led to predictions of increased intradiscal pressures at levels adjacent to intervertebral fusions. About 73 and 45% increase in intradiscal pressure at levels cephalad and caudad to fusion [27]. Adjacent-level motion has been shown to increase by 15% at 1 year after athrodesis [29]. This change is presumably caused by the fusion itself, rather than by other components of anterior cervical surgery such as elevation of the longus colli muscles. Increase in adjacent-level degeneration is theorized to be reduced due to preservation of the motion by an artificial joint [3, 8, 22].
Cervical arthroplasty aims to restore normal spinal motion following anterior cervical discectomy and avoid the abnormal kinematic stresses produced by ACDF. Favorable preliminary results have been reported with the use of the Bryan Cervical Disc Prosthesis in Europe [12, 13]. This prosthesis consists of a low-friction polyurethane nucleus surrounded by a polyurethane sheath, which is situated between two titanium alloy shells. This prosthesis provides elasticity and compressibility, allowing for unconstrained motion and translation through the normal ROM. Early clinical results from European trials of single- and two-level prosthesis implantation demonstrated that sagittal plane motion was preserved in 88% of patients treated with single-level and 86% of patients of those with two-level prostheses at 1 year, and that clinical outcomes were rated as excellent, good, or fair in more than 90% of patients at 1 year [12]. Nevertheless, although the ROM is an important feature of an artificial disc, it is only a single measure of spinal biomechanics.
Moreover, recently, some reports indicated a problem of kyphotic angulation after insertion of Bryan artificial disc prosthesis [18, 23]. Because artificial discs are not intended to restore lordosis, the question arises whether the kyphosis could be corrected while preserving the motion.
In 2001, Katsuura, et al. [19] found that degeneration of adjacent levels was significantly associated with loss of physiological cervical lordosis and implicated that physiologic lordotic fixation is required for prevention of neurological deterioration in a retrospective study of 42 patients followed for a mean of 10 years after undergoing anterior cervical discectomy and fusion for symptomatic cervical lordosis. Abd-Alrahman, et al. [1] noted that insertion of a bone plug, whether or not supplemented by anterior plate fixation, is the sole method available to restore normal lordosis.
Therefore this paper was intended to review the early clinical results and radiographic outcomes following insertion of the Bryan Disc including the ability of the prosthesis to maintain sagittal alignment of the functional spinal unit (FSU) and overall sagittal balance of the cervical spine during the follow-up period.
In our study, The ROM of the implanted level by shell angle at early and late follow-up were not significantly different when compared with the immediate postoperative shell angle (P > 0.05, respectively). The ROM of upper and lower adjacent disc space were significantly decreased at early follow up, but was significantly recovered at late follow up. However, the recovery did not reach the preoperative value (paired t test, P < 0.05). Further investigation could include whether the adjacent segment ROM recovers to the preoperative level, if not, how the partially recovered ROM influences on degeneration. The FSU and overall C2–7 alignment, on the other hand, were nearly recovered to the preoperative values (paired t test P > 0.05).
It is controversial whether cervical kyphosis influences clinical outcomes after Bryan disc insertion. In our patient group, no definite clinical deterioration due to kyphogenesis of the FSU or overall cervical alignment was observed.
The Bryan artificial disc prosthesis has a passive nature in its design, and is not designed to correct kyphosis; hence one would expect that it would be unable to restore lordosis to spine. In our study, despite the favorable clinical outcome, only 36% of patients with segmental lordosis (FSU ≥ 5°) preoperatively remained segmental lordotic alignment at the treated levels in late follow-up evaluations. However, 86% of patients with overall cervical lordotic alignment preoperatively remained lordotic alignment in late follow-up evaluations. 63% of patients with segmental kyphotic alignment (FSU < 0) preoperatively remained segmental kyphotic alignment at the treated level in late-follow up evaluations, and 33% of patients with kyphotic overall cervical alignment preoperatively exhibited kyphotic alignment in late follow-up evaluations. Most of the change occurred between preoperative and early follow-up assessments, with a little change between early and late follow-up review. This may represent progression of their disease at the treated level or worsening of the kyphosis after insertion of the artificial disc.
Interestingly, however, we observed that three patients (36%) with kyphotic (FSU < 0) alignment preoperatively at the operative level did not always exhibit kyphotic alignment in early and late follow-up evaluations (Table 5). In this small group, we could not explain a clear relationship between the preoperative focal kyphosis at the operative level and worsening of kyphosis after insertion of the prosthesis. Moreover, one patient (33%) of preoperatively kyphotic overall alignment patients showed overall lordotic alignment throughout the follow up period (Table 6).
Our results should be interpreted cautiously. The results of our study are not generalized to all patients who underwent Bryan disc implantation or other types of artificial disc insertion. It is possible that our results have led us to underestimate the potential benefit of cervical disc replacement because of the subjective nature of patient selection, the small sized of patients, and the relatively short follow-up duration. Further studies to evaluate this subset of arthroplasty patients with long-term follow-up will be necessary, and many unanswered questions may be addressed.
Based on our limited observations, we presumed that the early kyphotic changes can be the result of early response of surgery such as neck pain and late kyphotic changes may be the result of various factors other than the characteristics of its design, which is not designed to correct kyphosis. These factors are included the angle of Bryan disc insertion, over-milling process at both endplates, pre-existing kyphosis, etc. Correlation of these factors and sagittal curvature however, still remains to further investigation.
Since each cervical vertebrae or FSU moves independently, yet creates concordant overall curvature of C2–7, we studied ROM and curvature change of both FSU and overall cervical curvature to investigate the effect of the prosthesis in cervical alignment. The overall cervical lordosis, assessed by Cobb angles from C2 to C7, did not change significantly in the postoperative period, regardless of changes in the segmental angles. That implicated that compensation occurs at other levels.
Although there are several reports of well-known side effects such as heterotopic ossification after Bryan disc insertion, we did not encounter notable heterotopic ossification nor spontaneous fusion in follow up period of our patient group. The incidence is varied and the cause remains to be seen for further follow up [20, 23, 26]. This study is limited to the radiographic evaluation of sagittal alignment, which is not correlated with clinical symptoms. Other limitation of this study includes Odom’s clinical evaluation which is surgeon’s evaluation carrying potential of a bias that was augmented by patients’ self administered questionnaire of VAS and NDI. Intraobserver and interobserver errors in measurements, which were compensated by calculating, mean value of twice repeated observations from three observers.
With its current configuration, characteristics of design, biomaterials, procedures, and placement techniques, it might be limited in its ability to correct kyphosis and sagittal alignment for a long-term. Despite our wide range of categorization of the patients of such as kyphosis, lordosis, and straight groups, we could find that patients with focal kyphotic (or straight or lordotic) alignment preoperatively at the operated level did not always maintain their original spinal alignment in early and late follow-up evaluations. Nevertheless, it appears that the variance of curvature in the operated segments does not significantly influence clinical deterioration or improvement. The clinical improvement would be largely attributable to surgical decompression and focal change in curvature appears to be compensated by other segments.
We conclude that the Bryan’s prosthesis allows free motion around the implanted level, its passive nature of design allows variance of the curvatures of the implanted levels which is compensated by overall cervical alignment, and suggest that clinical status is not largely affected by these change of the curvatures.
Reference
Abd-Alrahman N, Dokmak AS, Abou-Madawi A (1999) Anterior cervical discectomy (ACD) versus anterior cervical fusion (ACF). Clinical and radiological outcome study. Acta Neurochir (Wien) 141:1089–1092
Baba H, Furusawa N, Imura S, Kawahara N, Tsuchiya H, Tomita K (1993) Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy Spine 18:2167–2173
Bryan VE Jr (2002) Cervical motion segment replacement. Eur Spine J 11(Suppl)2:S92–S97
Cherubino P, Benazzo F, Borromeo U, Perle S (1990) Degenerative arthritis of the adjacent spinal joints following anterior cervical spinal fusion: clinicoradiologic and statistical correlations Ital J Orthop Traumatol 16:533–543
Clements DH, O’Leary PF (1990) Anterior cervical discectomy and fusion Spine 15:1023–1025
Cloward RB (1952) The treatment of ruptured lumbar intervertebral disc by vertebral body fusion. III. Method of use of banked bone. Ann Surg 136:987–992
Cloward RB (1958) The anterior approach for removal of ruptured cervical disks. J Neurosurg 15:602–617
Coric D, Finger F, Boltes P (2006) Prospective randomized controlled study of the Bryan Cervical Disc: early clinical results from a single investigational site. J Neurosurg Spine 4:31–35
DiAngelo DJ, Roberston JT, Metcalf NH, McVay BJ, Davis RC (2003) Biomechanical testing of an artificial cervical joint and an anterior cervical plate. J Spinal Disord Tech 16:314–323
Dohler JR, Kahn MR, Hughes SP (1985) Instability of the cervical spine after anterior interbody fusion. A study on its incidence and clinical significance in 21 patients. Arch Orthop Trauma Surg 104:247–250
Eck JC, Humphreys SC, Lim TH, Jeong ST, Kim JG, Hodges SD, An HS (2002) Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine 27:2431–2434
Goffin J, Casey A, Kehr P, Liebig K, Lind B, Logroscino C, Pointillart V, Van Calenbergh F, van Loon J (2002) Preliminary clinical experience with the Bryan Cervical Disc Prosthesis. Neurosurgery 51:840–845; discussion 845–847
Goffin J, Van Calenbergh F, van Loon J, Casey A, Kehr P, Liebig K, Lind B, Logroscino C, Sgrambiglia R, Pointillart V (2003) Intermediate follow-up after treatment of degenerative disc disease with the Bryan Cervical Disc Prosthesis: single-level and bi-level. Spine 28:2673–2678
Goffin J, van Loon J, Van Calenbergh F, Plets C (1995) Long-term results after anterior cervical fusion and osteosynthetic stabilization for fractures and/or dislocations of the cervical spine. J Spinal Disord 8:500–508; discussion 499
Gore DR, Sepic SB (1984) Anterior cervical fusion for degenerated or protruded discs. A review of one hundred forty-six patients Spine 9:667–671
Hilibrand AS, Carlson G.D, Palumbo MA, Jones PK, Bohlman HH (1999) Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am 81:519–528
Hilibrand AS, Robbins M (2004) Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J 4:190S–194S
Johnson JP, Lauryssen C, Cambron HO, Pashman R, Regan JJ, Anand N, Bray R (2004) Sagittal alignment and the Bryan cervical artificial disc Neurosurg Focus 17:E14
Katsuura A, Hukuda S, Saruhashi Y, Mori K (2001) Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels Eur Spine J 10:320–324
Mehren C, Suchomel P, Grochulla F, Barsa P, Sourkova P, Hradil J, Korge A, Mayer HM (2006) Heterotopic ossification in total cervical artificial disc replacement Spine 31:2802–2806
Odom GL, Finney W, Woodhall B (1958) Cervical disk lesions J Am Med Assoc 166:23–28
Pickett GE, Rouleau JP, Duggal N (2005) Kinematic analysis of the cervical spine following implantation of an artificial cervical disc Spine 30:1949–1954
Pickett GE, Sekhon LH, Sears WR, Duggal N (2006) Complications with cervical arthroplasty J Neurosurg Spine 4:98–105
Pospiech J, Stolke D, Wilke HJ, Claes LE (1999) Intradiscal pressure recordings in the cervical spine Neurosurgery 44:379–384; discussion 384–375
Smith GW, Robinson RA (1958) The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion J Bone Joint Surg Am 40-A:607–624
Wang Y, Xiao SH, Lu N, Zhang XS (2004) [Clinical report of cervical arthroplasty in management of spondylotic myelopathy.] Zhonghua Wai Ke Za Zhi 42:1333–1337
Weinhoffer SL, Guyer RD, Herbert M, Griffith SL (1995) Intradiscal pressure measurements above an instrumented fusion. A cadaveric study. Spine 20:526–531
Wigfield CC, Skrzypiec D, Jackowski A, Adams MA (2003) Internal stress distribution in cervical intervertebral discs: the influence of an artificial cervical joint and simulated anterior interbody fusion J Spinal Disord Tech 16:441–449
Wu W, Thuomas KA, Hedlund R, Leszniewski W, Vavruch L (1996) Degenerative changes following anterior cervical discectomy and fusion evaluated by fast spin-echo MR imaging Acta Radiol 37:614–617
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, S.W., Shin, J.H., Arbatin, J.J. et al. Effects of a cervical disc prosthesis on maintaining sagittal alignment of the functional spinal unit and overall sagittal balance of the cervical spine. Eur Spine J 17, 20–29 (2008). https://doi.org/10.1007/s00586-007-0459-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-007-0459-y