Abstract
Different strategies exist to treat intervertebral disc degeneration. Biological attempts to regenerate the disc are promising. However, degeneration of the disc is always accompanied by alterations of disc height, intradiscal pressure, load distribution, and motion patterns, respectively. Since those preconditions are independent factors for disc degeneration, it is unlikely that regeneration may occur without firstly restoring the physiological status of the affected spinal segment. In vitro and in vivo animal studies demonstrate that disc distraction normalizes intradiscal height and pressure. Furthermore, histological and radiological examinations provided some evidence for regenerative processes in the disc. Only dynamic stabilization systems currently offer the potential of a mechanical approach to intervertebral disc regeneration. Dynamic stabilization systems either using pedicle screws or with an interspinous device, demonstrate restabilization of spinal segments and reduction of intradiscal pressure. Clinical reports of patients with degenerative disc disease who underwent dynamic stabilization are promising. However, there is no evidence that those implants will lead to disc regeneration. Future treatment concepts should combine intradiscal cell based therapy together with dynamic restoration of the affected spinal segment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A degenerate intervertebral disc is associated with significant structural failure such as radial fissures, prolapse, endplate damage, annular protrusion, internal disc disruption, and disc space narrowing. In the beginning of the degenerative course the water content of the nucleus pulposus decreases and the proteoglycane composition alters. This leads to reduction of intradiscal pressure and disc height, and later to alteration of the load distribution and results in an overloading of the annulus fibrosus and the facet joints. Degeneration in the form of radial tears and fissures is the consequence. The disc bulges towards the spinal canal, disc height decreases, osteophytes form and Schmorls nodes may occur, as well as facet joint arthritis. These degenerative changes cause instability in advanced disease [56, 58]. Typically, patients complain about low back pain with pseudoradicular sensations. The so called operative “gold standard” to treat degenerative disc disease (DDD) is fusion of the affected segment. Unfortunately, this may lead to adjacent disc degeneration in a large number of patients [31, 42].
Another consequence of ongoing disc degeneration especially in younger patients is disc protrusion and ultimately protrusion of nuclear material into the spinal canal. Patients then suffer from sciatica with radicular symptoms. If conservative therapy fails, discectomy or minimal invasive nucleotomy have to be carried out. Approximately, 200,000 discectomies per year are performed in the United States. However, operative treatment frequently leads to progression of degeneration [6, 14, 15] depending on the amount of the nucleus removed and the degree of damage of the posterior vertebral structures [43]. Approximately 10% of all operated discs reherniate and approximately 27% of all operated patients have to undergo a second operation within 10 years [24]. Consecutive procedures up to implantation of nucleus and disc prosthesis or even fusions are often necessary.
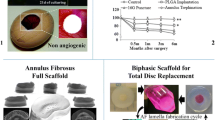
Different strategies have been developed to treat the degenerate disc in an early state. In addition to isolated treatment of the annulus and nucleus (nucleotomy, nucleoplasty, IDET, nucleus replacement, chemonucleosis etc.), arthroplasty is promising and may have the potential to replace fusion in the long term.
Current treatment options are very invasive and alter the composition of the disc. A totally different treatment approach is disc regeneration either by cellular or mechanical strategies. Spinal implants have not been designed for disc regeneration yet. Therefore, almost nothing is known about their influence on disc degeneration. Only the so called dynamic stabilization implants, which allow motion to a certain extent, are suitable for a mechanical treatment to restore the disc. The concept of dynamic stabilization includes maintenance of function as well as restriction of non-physiological motion of the spinal segment. Dynamic stabilization systems do not harm essential structures and may be removed at some stage following implantation.
This article deals with the concepts of disc regeneration by mechanical implants. Biomechanical and biological principles, as well as experimental and clinical studies have to be reviewed.
Biomechanical considerations
Most of the studies which deal with the effects of mechanical influence on the biology of disc degeneration are in vitro studies.
Degeneration is accompanied by non-physiological motion patterns. Moderate degeneration with radial tears of the annulus causes greater motion and therefore destabilizes the spinal segment. In contrast, in advanced degeneration with disc space collapse and osteophyte formation, motion decreases until spontaneous fusion occurs [53]. With degeneration, the neutral zone increases in all loading directions while the range of motion decreases for flexion and extension. This may be explained by higher joint laxity [36]. If the potential instability cannot be stabilized by muscles and ligaments sufficiently, loss of spinal balance and lordosis are resultant problems.
Discs are loaded in compression throughout life, but can withstand this pressure normally. However, compression of the disc influences disc cell metabolism and leads to remodelling of the tissue. Depending on the duration and magnitude of compressive loads, reversible or irreversible degeneration occur [21, 40], but not only duration and magnitude influence disc properties. Ching et al. [10] found less decrease of disc height after cyclic compression in comparison to static compression in a mouse tail model. Therefore, cyclic compression may cause less harm to the disc than static compression.
Compression combined with repetitive flexion and extension causes disc herniation in an experimental porcine model. In the laboratory disc herniation could be provoked even in young and healthy animals [8]. It is likely that in an already degenerate disc, compression together with repetitive motion can cause similar effects.
Ongoing degeneration of the disc alters intradiscal pressure and load transfer with high peak pressures anteriorly in flexion, posteriorly in extension, and inward bulging of the inner annulus under axial compression [1, 35].
In the course of disc degeneration, parts of the nucleus, annulus and cartilaginous endplate can get separated and may cause high pressure spots under load with consecutive pain. This “stone in the shoe” hypothesis may explain the typical sudden onset of pain as well as the pain relief which some patients experience through distraction (unloading) of the spine [39].
In these mechanical conditions every biological attempt to regenerate the disc is likely to fail. From a biomechanical point of view disc regeneration may only occur in the following conditions: Restoration of physiological motion, lordosis, spinal balance, disc height, intradiscal pressure, and load distribution. None of these are achieved by current implants.
Interrelation between mechanics and biology
Disc degeneration and its causes have been thoroughly examined, but the biological effects of altered mechanics in the spine are not fully understood. It seems that any change in load distribution has an impact on disc cells and matrix.
Lotz et al. [33, 34] showed that compression of mouse tail discs leads to an increase of apoptosis, disorganization of the annulus, and a down-regulation of collagen II and aggrecan gene expression. There was no restoration of the annulus architecture after terminating the compression. The extent of apoptosis depended on the time and magnitude of spinal loading. Similar results were reported by Court et al. [12] for static bending stresses. Bending forces applied to a mouse tail resulted in increased cell death, decreased aggrecan gene expression and decreased tissue organization preferentially on the concave side of the disc.
Not only excessive load causes degeneration: Handa et al. [21] found decreased synthesis of proteoglycan and increase synthesis of MMP-3 after application of pressures above and below the physiological level. The authors concluded that a physiologic level of hydrostatic pressure is essential to maintain the matrix of the disc. These findings are supported by Hsieh and Lotz [23] who could demonstrate increased activation of MMP-2 after prolonged static overload of mouse coccygeal discs.
In summary, excessive load causes loss of disc height, degradation of the extracellular matrix, increased apoptosis and disorganization of the cellular architecture. The extent of these degenerative changes depends on the magnitude, duration and frequency of load and pressure, respectively.
Effects of distraction on disc regeneration
Physiologic motion, load distribution, and intradiscal pressure are mandatory for disc viability. Since a degenerate disc cannot regenerate itself, external devices may provide conditions for biological attempts of regeneration.
Theoretically, the easiest way to restore the height of the disc is distraction, but so far, little is known about the biomechanical and biological effects of disc distraction.
Kwon et al. [29] performed a study with calf spines. They implanted PMMA spacers in between the spinous processes and demonstrated reduced intradiscal pressure values in the nucleus and posterior annulus, mainly in extension.
Hsieh et al. [22] demonstrated less matrix degradation from collagenase in a devitalised mouse tail model when discs were exposed to tensional stress. The findings match their previous results demonstrating that tension can maintain lamellar architecture after injurious loading.
The study group around Kroeber, Guehring and Unglaub performed several studies concerning the influence of compression followed by dynamic distraction in a small animal model:
In an in vivo study with New Zealand white rabbits the study group [28, 55] applied external load to the lumbar spine with a custom-made device to induce disc degeneration over 28 days. Compression force was 2.4 MPa or 200 N, respectively. The model demonstrated induction of disc degeneration in a previous study [54]. After compression of the discs, one subgroup of animals underwent dynamic distraction with an external distraction device for 28 days. The dynamic distraction was achieved by a calibrated spring. Distraction force (120 N) was adapted to the force provided by a dynamic neutralization system for human discs.
After compression and distraction, histological, radiological and biomechanical examinations were performed. Twenty-eight days of compression lead to a decrease of disc height, disorganization of the annulus architecture, and increased apoptosis in the annulus and cartilage endplate. Interestingly, these changes were reversible after distraction. Disc height increased and the number of apoptotic cells decreased. The lamellar morphology of the annulus was restored, too. However, flexibility of distracted discs was lower that of compressed discs. The authors concluded that axial dynamic distraction can induce disc regeneration in moderately degenerated rabbit intervertebral disc.
In a more recent published study from the same group intradiscal pressures were measured in rabbit intervertebral discs after temporary external disc compression and distraction. Compression reduced intradiscal pressure, significantly. Distraction could stabilize intradiscal pressure, but physiological levels could not be reached again [17].
Despite the promising effects of distraction in animal models one has to consider that the effects of compression and subsequent distraction are time dependent. It is not clear how long and how much compression a disc can withstand. Whether distraction has any positive influence after long lasting compression is yet to be demonstrated.
The effect on MRI and gene expression were reported by Guehring et al. [18]. The authors used the same rabbit model to demonstrate that distraction of the disc after previous compression leads to significant higher signal intensity in the nucleus on MRI. Furthermore, upregulation of the matrix genes COL 1 + 2, Decorin and Biglycan could be proved after distraction. The authors concluded a substantial possibility of disc regeneration at a cellular level due to distraction.
Theoretically distraction can be applied with various implants, but that does not mean that dynamic or rigid fixation will have any positive effects on the disc. The observation that rigid fixation does not influence disc degeneration is supported by Moore et al. [38] who created an outer annulus tear in a sheep model. To investigate the potential role of a rigid fixation they plated the injured segments. After 6 months pronounced disc degeneration was seen in the stabilized group. They concluded that disc degeneration was not prevented by this rigid stabilization.
So far, experimental studies with dynamic stabilization and distraction of intervertebral discs have only been carried out either in vitro or in small animal models. Little is known about currently available dynamic implants for humans and their effects on the course of degeneration. To answer this question, experiments with large animal have to be performed. To investigate the potential capacity of dynamic stabilization systems for humans, we developed a sheep disc degeneration model. After standardized nucleotomy of all animals, one half of the sheep underwent implantation of a new posterior soft fixation system on a pedicle screw base. Sheep were sacrificed after 3 months. Radiologically and histologically we found moderate degenerative changes in both groups. As the main difference we found less osteophyte formation in the soft stabilized group after 3 months. Our preliminary conclusion is that the restricted motion of the soft stabilized segments leads to less degenerative changes in the disc, especially with regard to osteophyte formation.
Dynamic stabilization in humans
Dynamic stabilization with disc distraction causes changes in the disc metabolism in animals, and there is some evidence that distraction may influence the regeneration of disc cells. It remains unclear if these findings will be replicated in the human disc. It has been proven that pressure-release of the disc by lying down at night or a period in a zerogravity environment causes an increase in disc height and volume [30], and therefore, one could assume that mechanical distraction of the human disc may cause similar changes.
Biomechanical tests have shown disc pressure reduction and maintenance of lordosis in dynamic stabilized segments [9, 48]. In a human in vivo study, Korovessis et al. [26] demonstrated that dynamic instrumentations restored lumbar lordosis, sacral tilt, distal lordosis and increased the foraminal diameter as effectively as rigid fixation.
The philosophy behind dynamic stabilization is restoration of physiological motion, load distribution and intradiscal pressure. As a consequence, a suitable environment may be generated for further treatment options like stem cell therapy, growth factor application, and gene transfer, respectively [49].
Dynamic stabilization with pedicle screw based systems
The most common indication for dynamic stabilization is degenerative instability. Implants include Graf ligamentoplasty (Neoligaments, UK), and the Dynesys system (Zimmer, USA). Additionally, FASS (fulcrum-assisted soft stabilization) by Sengupta and Mulholland, Cosmic (Ulrich, Germany), TOPS system (Impliant, USA) and others are emerging implants.
Some authors use dynamic stabilization systems for the treatment of facet pain caused by instability [5], spinal stenosis [27], functional instability with spinal stenosis, structural deformities and other kinds of degenerative disc disease [13, 51].
The Graf system is well documented, but yet has not become accepted in managing low back pain or degenerative disc disease due to poor outcome and high revision rates [19, 20, 25].
In studies of Dynesys investigators have found promising results in patients with DDD, disc prolapses and degenerative spondylolisthesis, respectively [7, 13, 41, 46, 51]. However, not all authors report good results [16].
Interestingly, Specchia observed rehydration of the disc on MRI after implantation of Dynesys [50], although data are not published yet, and no link have been established between rehydration and regeneration.
Interspinous spacers
Interspinous spacers like Wallis (Abbott Spine, France), DIAM (Medtronic, USA), X Stop (St. Francis, USA) and others are typically used in patients with spinal stenosis. Discectomy, adjacent segment disease after fusion and degenerative disc disease are indications for some authors [47]. Preliminary published data about interspinous spacers are promising, but not yet convincing [11].
Dynamic stabilization and disc regeneration
Some biomechanical studies have been performed, showing a positive influence of dynamic stabilization systems on intradiscal pressure values:
Minns et al. [37] demonstrated reduced intradiscal pressures in flexion and upright position after implantation of an interspinous silicone spacer.
A more recent study from Swanson et al. [52] demonstrated significant reduced intradiscal pressure values in the nucleus and posterior annulus of cadaver human spines for extension and upright position after implantation of X-stop.
Similar results have been presented for Dynesys. Cew et al. [9] presented a biomechanical study, showing reduced intradiscal pressure values after implantation of Dynesys.
Schmoelz et al. [45] investigated Dynesys more thoroughly and revealed less intradiscal pressures changes in lateral flexion and extension in comparison to an intact and posterior destabilized segment. In contrast, no change in intradiscal pressures was found in neutral position and during rotation. Interestingly the same results were found with rigid fixation.
Other posterior dynamic implants provide similar possibilities. Sengupta and Mulholland developed a FASS that seems to reduce intradiscal pressure and range of motion while preserving physiological lordosis of the lumbar segment [48].
Besides those promising laboratory results it remains unclear if dynamic stabilization can slow down intervertebral disc degeneration in vivo.
Specchia [50] reported signs of rehydration of the nucleus on MRI after Dynesys implantation in patients. Guehring [18] found similar changes on MRI after distraction of rabbit intervertebral discs.
Clinical studies with patients undergoing Dynesys implantation have not focussed on the subsequent course of disc degeneration yet. In a study from Putzier et al. [41] patients underwent nucleotomy with or without implantation of Dynesys. After an average of 34 months no progression of disc degeneration could be detected in the Dynesys group. Another study of Dynesys implantation with decompression for degenerative spondylolisthesis with spinal stenosis did not find any significant decrease of the disc height after an average follow-up of 26 months [46].
In summary, dynamic stabilization systems offer the possibility of restoring physiological motion patterns and may normalize intradiscal pressure. Clinically, dynamic stabilization does not harm the disc and is likely to slow down degeneration. Furthermore, it may allow regeneration of the disc to some extent and may provide a favourable environment for disc regeneration. However, those assumptions have yet to be proven.
Limitations of dynamic stabilization
Disc degeneration is a multifactorial disease with intrinsic and extrinsic factors affecting its course. It has to be considered that there are strong genetic influences [2, 3]. Furthermore, macro- and microscopic alterations of the disc can be detected very early in life. Degeneration may start as early as the second decade [4]. Since most of our patients are already in the fourth decade or older, mechanical treatment concepts aiming for disc regeneration may fail due to irreversible structural alterations [57].
Restoration of physiological motion is the main goal of dynamic stabilization systems, but this is a myth. Schmoelz et al. [44] compared Dynesys with an internal fixator in a biomechanical study with cadaver lumbar spines, stabilization with Dynesys was almost as stiff as with the internal fixator.
Despite widespread use of dynamic stabilization systems no randomised controlled studies exist. There is little consensus among spine surgeons about the right indications for dynamic stabilization. Well designed studies are lacking and some authors have reported disappointing results. Additionally, in some published studies the success of the treatment was to a certain extent dependant on accompanying surgical interventions rather than implantation of a dynamic stabilization system [41, 46], and an additional problem of pedicle screw based systems is screw loosening [46]. For interspinous spacers no long-term data are available, but problems like fractures of the spinous processes, subsidence of the implant into the bone or dislocation may be expected. Interspinous spacers restrict motion rather than restoring it [32].
Future applications of dynamic stabilization systems
Distraction of the disc, restoration of physiological load distribution and motion patterns of the spinal segment seem to have positive effects on the course of disc degeneration. No current implant can provide sufficient biomechanical properties to restore the physiological situation, and therefore the focus should be on the development of more sophisticated implants.
In the meantime, the effects of dynamic stabilization systems on disc degeneration should be investigated not only in small but in large animals. Since implants are developed for humans, large animal studies are essential to examine their possible positive effects. Provided that there is consistent evidence of a positive influence of dynamic devices on the course of intervertebral disc degeneration, the next step would be to combine mechanical devices with intradiscal therapy. Gene therapy, application of growth hormones, stem cells, or biological nucleus replacement combined with mechanical dynamic stabilization systems may be options in the future.
References
Adams MA, McNally DS, Dolan P (1996) Stress distributions inside intervertebral discs. J Bone Joint Surg (Br) 78–B:965–972
Ala-Kokko L (2002) Genetic risk factors for lumbar disc disease. Ann Med 34:42–47
Battie MC, Videman T, Parent E (2004) Lumbar disc degeneration: epidemiology and genetic influences. Spine 29:2679–2690
Boos N, Weissbach S, Rohrbach H, Weiler C, Spratt KF, Nerlich AG (2002) Classification of age-related changes in lumbar intervertebral discs: 2002 Volvo Award in basic science. Spine 27:2631–2644
Brechbuhler D, Markwalder TM, Braun M (1998) Surgical results after soft system stabilization of the lumbar spine in degenerative disc disease—long-term results. Acta Neurochir 140:521–525
Brinckmann P, Grootenboer H (1991) Change of disc height radial, disc bulge, and intradiscal pressure from discectomy. An in vitro investigation on human lumbar discs. Spine 1:641–646
Cakir B, Ulmar B, Koepp H, Huch K, Puhl W, Richter M (2003) Posterior dynamic stabilization as an alternative for dorso-ventral fusion in spinal stenosis with degenerative instability. Z Orthop 141:418–424
Callaghan JP, McGill SM (2001) Intervertebral disc herniation: studies on a porcine model exposed to highly repetitive flexion/extension motion with compressive force. Clin Biomech 16:28–37
Cew A, McKinlay KJ, Freeman BJC, Shepperd J, McNally DS (2004) In vitro biomechanical effects of Dynesys. Poster at the EuroSpine 2004, Portugal
Ching CT, Chow DH, Yao FY, Holmes AD (2003) The effect of cyclic compression on the mechanical properties of the inter-vertebral disc: an in vivo study in a rat tail model. Clin Biomech 18:182–189
Christie SD, Song JK, Fessler RG (2005) Dynamic interspinous process technology. Spine 30(16 Suppl):S73–S78
Court C, Colliou OK, Chin JR, Liebenberg E, Bradford DS, Lotz JC (2001) The effect of static in vivo bending on the murine intervertebral disc. Spine J 1:239–245
Dubois B, de Germay B, Schaerer NS, Fennema P (1999) Dynamic neutralization: a new concept for restabilization of the spine. In: Szalski M, Gunzburg R, Pope MH (eds) Lumbar segmental instability. Lippincott Williams & Wilkins, Philadelphia, pp 233–240
Dunlop RB, Adams MA, Hutton WC (1984) Disc space narrowing and the lumbar facet joints. J Bone Joint Surg Br 66:706–710
Gottfried Y, Bradford DS, Oegema TR (1986) Facet joint changes after chemonucleosis-induced disc space narrowing. Spine 11:944–950
Grob D, Benini A, Junge A, Mannion AF (2005) Clinical experience with the Dynesys semirigid fixation system for the lumbar spine: surgical and patient-oriented outcome in 50 cases after an average of 2 years. Spine 30:324–331
Guehring T, Unglaub F, Lorenz H, Omlor G, Wilke HJ, Kroeber MW (2006) Intradiscal pressure measurements in normal discs, compressed discs and compressed discs treated with axial posterior disc distraction: an experimental study on the rabbit lumbar spine model. Eur J Spine 15:597–604
Guehring T, Omlor G, Lorenz H, Engelleiter K, Richter W, Carstens C, Kroeber W (2005) Axiale Distraktion beeinflusst Regenerationsprozesse mittelgradige degenerierter Bandscheiben. Presentation at the 1st combined German Congress of Orthopedics and Traumatology (DGU + DGOOC)
Guigui P, Chopin D (1994) Assessment of the use of the Graf ligamentoplasty in the surgical treatment of lumbar spinal stenosis. Apropos of a series of 26 patients. Rev Chir Orthop Reparatrice Appar Mot 80:681–688
Hadlow SV, Fagan AB, Hillier TM, Fraser AD (1998) The Graf ligamentoplasty procedure. Comparison with posterolateral fusion in the management of low back pain. Spine 23:1172–1179
Handa T, Ishihara H, Ohshima H, Osada R, Tsuji H, Obata K (1997) Effects of hydrostatic pressure on matrix synthesis and matrix metalloproteinase production in the human lumbar intervertebral disc. Spine 22:1085–1091
Hsieh AH, Hadi T, Lotz JC (2005) MMP Degradation of annulus fibrosus is reduced by tension. Presented at the 51st Annual Meeting of the Orthopedic Research Society
Hsieh AH, Lotz JC (2003) Prolonged spinal loading induces matrix metalloproteinase-2 activation in intervertebral discs. Spine 28:1781–1788
Jansson KA, Nemeth G, Granath F, Blomqvist P (2004) Surgery for herniation of a lumbar disc in Sweden between 1987 and 1999 an analysis of 27,576 operations. J Bone Joint Surg Br 86:841–847
Konno S, Kikuchi S (2000) Prospective study of surgical treatment of degenerative spondylolisthesis: comparison between decompression alone and decompression with graf system stabilization. Spine 25:1533–1537
Korovessis P, Papazisis Z, Lambiris E (2002) The role of rigid vs. dynamic instrumentation for stabilization of the degenerative lumbosacral spine. Stud Health Technol Inform 91:457–61
Korovessis P, Papazisis Z, Koureas G, Lambiris E (2004) Rigid, semirigid versus dynamic instrumentation for degenerative lumbar spinal stenosis: a correlative radiological and clinical analysis of short-term results. Spine 29:735–742
Kroeber M, Unglaub F, Guehring T, Nerlich A, Hadi T, Lotz J, Carstens C (2005) Effects of controlled dynamic disc distraction on degenerated intervertebral discs. An in vivo study on the rabbit lumbar spine model. Spine 30:181–187
Kwon SY, Moon SJ, Lee KS, Shim KC, Tack GR, Lee SJ (2005) Disc pressure changes with PMMA interspinous spinal spacer insertion for lumbar spinal stenosis. Poster at the 51st Annual Meeting of the Orthopedic Research Society
LeBlanc AD, Evans HJ, Schneider VS, Wendt RE III, Hedrick TD (1994) Changes in intervertebral disc cross-sectional area with bed rest and space flight. Spine 19:812–817
Lehmann TR, Spratt KF, Tozzi JE, Weinstein JN, Reinarz SJ, el-Khoury GY, Colby H (1987) Long-term follow-up of lower lumbar fusion patients. Spine 12:97–104
Lindsey DP, Swanson KE, Fuchs P, Hsu KY, Zucherman JF, Yerby SA (2003) The effects of an interspinous implant on the kinematics of the instrumented and adjacent levels in the lumbar spine. Spine 28:2192–2197
Lotz JC, Colliou OK, Chin JR, Duncan NA, Liebenberg E (1998) Compression-induced degeneration of the intervertebral disc: an in vivo mouse model and finite-element study. Spine 23:2493–2506
Lotz JC, Chin JR (2000) Intervertebral disc cell death is dependent on the magnitude and duration of spinal loading. Spine 25:1477–1483
Meakin JR, Hukins DWL (2000) Effect of removing the nucleus pulposus on the deformation of the annulus fibrosus during compression of the intervertebral disc. J Biomech 33:575–580
Mimura M, Panjabi MM, Oxland TR, Crisco JJ, Yamamoto I, Vasavada A (1994) Disc degeneration affects the multidirectional flexibility of the lumbar spine. Spine 19:1371–1380
Minns RJ, Walsh WK (1997) Preliminary design and experimental studies of a novel soft implant for correcting sagittal plane instability in the lumbar spine. Spine 22:1819–1825
Moore RJ, Latham JM, Vernon-Roberts B, Fraser RD (1994) Does plate fixation prevent disc degeneration after a lateral anulus tear?. Spine 19:2787–2790
Mulholland RC, Sengupta DK (2002) Rationale, principles and experimental evaluation of the concept of soft stabilization. Eur Spine J 11(Suppl2):S198–S205
Neufeld JH (1992) Induced narrowing and back adaptation of lumbar intervertebral discs in biomechanically stressed rats. Spine 17:811–816
Putzier M, Schneider SV, Funk JF, Tohtz SW, Perka C (2005) The surgical treatment of the lumbar disc prolapse: nucleotomy with additional transpedicular dynamic stabilization versus nucleotomy alone. Spine 30:E109–E114
Rahm MD, Hall BB (1996) Adjacent-segment degeneration after lumbar fusion with instrumentation: a retrospective study. J Spinal Disord 9:392–400
Schaller R (2004) Failed back surgery syndrome: the role of symptomatic segmental single-level instability after lumbar microdiscectomy. Eur Spin J 13:193–198
Schmoelz W, Huber JF, Nydegger T, Claes L, Wilke HJ (2003) Dynamic stabilization of the lumbar spine and its effect on adjacent segments: an in vitro experiment. J Spinal Disord Tech 16:418–423
Schmoelz W, Huber JF, Nydegger T, Claes L, Wilke HJ (2006) Influence of a dynamic stabilisation system on load bearing of a bridged disc: an in vitro study of intradiscal pressure. Eur Spine J 21:1–10
Schnake KJ, Schären S, Jeanneret B (2006) Dynamic stabilization in addition to decompression for lumbar spinal stenosis with degenerative spondylolisthesis. Spine 31:442–449
Senegas J (2002) Mechanical supplementation by non-rigid fixation in degenerative intervertebral lumbar segments: the Wallis system. Eur Spine J 11(Suppl2):S164–S169
Sengupta DK, Mulholland RC (2005) Fulcrum assisted soft stabilization system: a new concept in the surgical treatment of degenerative low back pain. Spine 30:1019–1029
Sengupta DK (2004) Dynamic stabilization devices in the treatment of low back pain. Orthop Clin North Am 35:43–56
Specchia N (2004) Dynamic neutralization of the lumbar spine can help the disc repairing process. Presentation at the 4th Dynesos Meeting, Austria
Stoll TM, Dubois G, Schwarzenbach O (2002) The dynamic neutralization system for the spine: a multi-center study of a novel non-fusion system. Eur Spine J 11:170–178
Swanson KE, Lindsey DP, Hsu KY, Zucherman JF, Yerby SA (2003) The effects of an interspinous implant on intervertebral disc pressures. Spine 28:26–32
Tanaka N, An HS, Lim TH, Fujiwara A, Jeon CH, Haughton VM (2001) The relationship between disc degeneration and flexibility of the lumbar spine. Spine J 1:47–56
Unglaub F, Lorenz H, Nerlich A, Richter W, Kroeber MW (2003) Stimulation of degenerative changes in the intervertebral disc through load in an animal model. Z Orthop 141:412–417
Unglaub F, Guehring T, Omlor G, Lorenz H, Carstens C, Kroeber MW (2006) Controlled distraction as a therapeutic option in moderate degeneration of the intervertebral disc—an in vivo study in the rabbit-spine model. Z Orthop 144:68–73
Urban JPG, Roberts S (2003) Degeneration of the intervertebral disc. Arthritis Res Ther 5:120–130
Urban JP, Smith S, Fairbank JC (2004) Nutrition of the intervertebral disc. Spine 29:2700–2709
Yu S, Haughton VM, Ho PS, Sether LA Wagner M, Ho KC (1988) Progressive and regressive changes in the nucleus pulposus II. The adult. Radiology 169:93–97
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schnake, K.J., Putzier, M., Haas, N.P. et al. Mechanical concepts for disc regeneration. Eur Spine J 15 (Suppl 3), 354–360 (2006). https://doi.org/10.1007/s00586-006-0176-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-006-0176-y