Abstract
This prospective longitudinal randomized clinical and radiological study compared the evolution of instrumented posterolateral lumbar and lumbosacral fusion using either coralline hydroxyapatite (CH), or iliac bone graft (IBG) or both in three comparable groups, A, B and C, which included 19, 18 and 20 patients, respectively, who suffered from symptomatic degenerative lumbar spinal stenosis and underwent decompression and fusion. The patients were divided randomly according to the graft used and the side that it was applied. The spines of group A received autologous IBG bilaterally; group B, IBG on the left side and hydroxyapatite mixed with local bone and bone marrow on the right side; group C, hydroxyapatite mixed with local bone and bone marrow bilaterally. The age of the patients in the groups A, B and C was 61±11 years, 64±8 years and 58±8 years, respectively. The SF-36, Oswestry Disability Index (ODI), and Roland-Morris (R-M) surveys were used for subjective evaluation of the result of the surgery and the Visual Analogue Scale (VAS) for pain severity. Plain roentgenograms including anteroposterior, lateral and oblique views, and lateral plus frontal bending views of the instrumented spine and CT scan were used to evaluate the evolution of the posterolateral fusion in all groups and sides. Two independent senior orthopaedic radiologists were asked to evaluate first the evolution of the dorsolateral bony fusion 3–48 months postoperatively with the Christiansen’s radiologic method, and secondly the hydroxyapatite resorption course in the spines of groups B and C. The diagnosis of solid spinal fusion was definitively confirmed with the addition of the bending views, CT scans and self-assessment scores. The intraobserver and interobserver agreement (r) for radiological fusion was 0.71 and 0.69, respectively, and 0.83 and 0.76 for evaluation of CH resorption. T12−S1 lordosis and segmental angulation did not change postoperatively. There was no radiological evidence for non-union on the plain roentgenograms and CT scans. Radiological fusion was achieved 1 year postoperatively and was observed in all groups and vertebral segments. Six months postoperatively there was an obvious resorption of hydroxyapatite granules at the intertransverse intersegmental spaces in the right side of the spines of group B and both sides of group C. The resorption of hydroxyapatite was completed 1 year postoperatively. Bone bridging started in the third month postoperatively in all instrumented spines and all levels posteriorly as well as between the transverse processes in the spines of the group A and on the left side of the spines of group B where IBG was applied. SF-36, ODI, and R-M score improved postoperatively in a similar way in all groups. There was one pedicle screw breakage at the lowermost instrumented level in group A and two in group C without radiologically visible pseudarthrosis, which were considered as having non-union. Operative time and blood loss were less in the patients of group C, while donor site complaints were observed in the patients of the groups A and B only. This study showed that autologous IBG remains the “gold standard” for achieving solid posterior instrumented lumbar fusion, to which each new graft should be compared. The incorporation of coralline hydroxyapatite mixed with local bone and bone marrow needs adequate bleeding bone surface. Subsequently, hydroxyapatite was proven in this series to not be appropriate for intertransverse posterolateral fusion, because the host bone in this area is little. However, the use of hydroxyapatite over the decorticated laminae that represents a wide host area was followed by solid dorsal fusion within the expected time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Posterolateral instrumented fusion with supplementary use of autologous iliac bone graft (IBG) is the most commonly performed procedure for the treatment of degenerative conditions of the lumbar spine. Although IBG is the material most likely to encourage spinal fusion, pseudarthrosis rates range from 5% to 35% [39]. IBG harvesting is associated with complications including muscle herniations, vascular and nerve injuries, hematomas, deep infections and iliac fractures, ranging from 0% to 17.9% [1, 3, 4, 13, 16, 23].
Because of the above-mentioned complications associated with IBG, alternative graft materials as allograft, xenograft and ceramics have been introduced in the spine surgery and have an important role as autograft substitute or extender.
Ceramics, including coralline hydroxyapatite (CH), are increasingly used in orthopaedic surgery and recently in spine surgery [29, 30, 32], and are available in many types. CH has osteoconductive properties, does not induce an inflammatory or foreign body response, possess excellent bone-bonding capacity [11], harbors no risk of infectious disease transmission, and no increased risk for deep infection [29]. In their present form, calcium phosphate ceramics allow propagation of new bone formation on their surface from the preexisting nearby bone. However, unlike autograft or some allograft bone, these ceramics are not osteoinductive, or capable of inducing new bone formation de novo.
Pro-Osteon 500 R (Interpore Cross, International, Irvine, Calif., USA), a type of CH, is a porous mineral material that is currently used as an effective alternative to autologous cancellous bone graft material in posttraumatic metaphyseal defects [5, 28]. Pro-Osteon 500 R has a predictable resorption, in contrast to other forms of CH (Pro-Osteon 200 and Pro-Osteon 500), which resorb slowly, if at all. Resorption of Pro-Osteon 500 R makes the assessment of ingrowth easier and has been used for several years in our practice in more than 250 spine surgeries [29, 30].
To the authors’ knowledge there are no comparative clinical and radiological studies on the radiological evolution of posterior and intertransverse instrumented lumbar spinal fusion with IBG versus CH in humans. This prospective longitudinal comparative study was conducted to investigate the correlative evolution of posterolateral bony fusion with enhancement with CH versus IBG in instrumented lumbar spine.
Materials and methods
This study was approved by the hospital’s ethics committee and all patients accepted this protocol. The exclusion criteria were: previous spinal operations in the lumbosacral spine, lumbar spinal infection, osteoporotic spinal fractures and endocrine system diseases (hyperparathyroidism, hyper-, hypothyroidism, chronic use of corticosteroids). Sixty patients were randomly selected and were divided in three equal groups (A, B and C) according to the graft or combination of grafts used. The age (mean ± standard deviation) of the patients was 61±11 years, 64±8 years and 58±8 years for groups A, B and C, respectively. The patients suffered from symptomatic degenerative lumbar spine stenosis with instability (including olisthesis, spondylolysis or/and combination) and underwent decompression using laminotomy and undercutting facectomy, transpedicular instrumentation and posterior plus lateral intertransverse fusion. The decompression aimed to adequately decompress the thecal sac, nerve roots and lateral recess. The patients to be included in each group were randomly selected. In the spines of group A, IBG was applied over the decorticated laminae and between the transverse processes bilaterally. The quantity of bone chips, bone marrow and HA granules were intraoperatively measured with a volumetric device. In the spines of group B, CH granules (15 cc per level) mixed with local bone chips (5–10 cc bone chips per segment) derived from decortication of the posterior spinal elements (laminae and spinal processes) with fine chisels and bone marrow (2–3 cc drown per pedicle) derived from aspiration from the pedicles of the instrumented vertebrae were applied on the right side and IBG on the left side (laminae and transverse processes); and in group C, CH granules (15 cc per level) mixed with local bone chips 5–10 cc bone chips per segment) derived from the posterior element (laminae and spinal processes) and bone marrow (2–3 cc drown per pedicle) were applied bilaterally on the laminae and transverse processes. All surgeries were performed by the senior author, always using the same surgical technique. The identity of the patient’s group was revealed to the surgeon after the pedicle screws were placed and the graft bed prepared, to eliminate any bias. A posterior midline approach was used to expose the posterior and posterolateral structures of the lumbar spine. Following aspiration of bone marrow, two titanium pedicle screws were inserted into each instrumented vertebra. The decompression at the level of pathology was made by means of laminotomy-underfacetectomy. A meticulous decortication of the laminae, spinal and transverse processes was performed, while removal of the articular cartilage of the facet joints at the levels of fusion was added. The transverse processes in the area of instrumentation were meticulously cleaned from soft tissues in their entire length and width, to increase the host area for intertransverse fusion. In the patients of groups A and B, autologous bone graft was taken from the external plate of the posterior iliac crest close to the sacroiliac joint and the site of bone harvesting was separately drained. The IBG was applied on the decorticated laminae and on the transverse processes and between them on the left side in group B and bilaterally in group A. In the groups B and C, bone chips derived from decortication of the posterior spinal elements were mixed with CH granules (ratio of CHA to bone 3:1) and the preserved bone marrow. The resulting mixture was symmetrically applied per vertebral level on the decorticated laminae and transverse processes on the right side (group B) and bilaterally (group C) by means of a posterior and intertransverse grafting. The volume of the graft material (HA or/and autologous IBG) was constant for each segment of fusion and was measured with the use of a volumetric vessel. After application of the graft or graft mixture the longitudinal rods were contoured to restore the lumbar lordosis and mounted to the pedicle screw heads. No posterior lumbar interbody fusion or anterior surgery was performed in any case in this series. The instrumentation and fusion in all groups included two or three levels and did not differ between the three groups. The authors instrumented only two- and three-level instrumentations for all three groups to avoid the increased risk of non-union and pseudarthrosis that is associated multilevel instrumentations. The number of three- and two-level instrumentations was equal in all groups. The wound was drained and closed in three layers. The drain was removed in the second day postoperatively. Prophylactic antibiotics were intravenously given for 3 days. The patients were mobilized 2 days postoperatively with a custom-made plastic body brace for 1 month. Postoperatively, all patients were followed with blood count analysis, C-reactive protein and erythrocyte sedimentation rate.
Self-assessment
The short-form SF-36 health survey, Oswestry Disability Index (ODI), Visual Analogue Scale (VAS 0–10) and Roland-Morris score (R-M, 0–24) were obtained preoperatively, as well as 6 months, 12 months, 24 months and 48 months postoperatively. Cigarette consumption was recorded in seven, nine and ten patients in groups A, B and C, respectively.
Radiological evaluation
Plain roentgenograms (standing anteroposterior and lateral views, supine oblique right and left, frontal right-left bending and sitting lateral bending views) were obtained preoperatively and 3 months, 6 months, 12 months, 24 months and 48 months postoperatively. Oblique views of the instrumented spine were used in the present study to accurately evaluate intersegmental bony fusion because the presence of hardware made it difficult to interpret bony fusion on the classical anteroposterior (AP) and lateral views. In the bending tests, angular motion on flexion-extension radiographs of 5° or more and sagittal plane translation (olisthesis) on flexion–extension radiographs of 3 mm or more were considered as instability [26]. CT scans were performed in all cases preoperatively, as well as 12 months and 24 months postoperatively, to evaluate facet joint arthrodesis (Fig. 1). The radiological evolution of the posterolateral fusion (CH resorption and bone formation) on the plain roentgenograms was evaluated by two independent senior orthopaedic radiologists who were considered as unbiased observers 3 months, 6 months, 12 months to 48 months postoperatively. There was a consensus between the radiologists on the definition of fusion according to Christiansen’s classification [15]: grade 3=continuous intersegmental bony bridge; grade 2=doubtful fusion intersegmental bony bridge; grade 1=no intersegmental bony bridging fusion. As fusion (grade 3) was considered continuous bridging at all levels of instrumentation, at least at one plain roentgenogram associated with no pathologic movement in the bending roentgenograms. In particular the intertransverse bridging and dorsal (laminae) and facet joint fusion between right and left side was compared on the AP and oblique views. The observers re-evaluated the plain roentgenograms within 3 weeks to test interobserver reliability. The resorption of CH granules between the transverse processes in the spines of groups B and C were evaluated by the same observers using the following classification: grade 2=continuous bridging, grade 1=doubtful bridging, and grade 0=no bridging.
Statistical analysis
The ANOVA was used to compare fusion grade and SF-36, R-M and VAS and ODI between different periods of observation and between different groups. The Pearson correlation coefficient (r) was used to test the intra- and interobserver reliability of roentgenographic evaluation of bony fusion and intertransverse CHA resorption. All result values are shown as average ± standard deviation.
Results
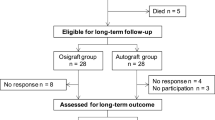
One patient from group A, and two from group B developed deep infection in the first month postoperatively and were excluded from this study. Thus, 19, 18 and 20 patients from the groups A, B and C, respectively, were definitively enrolled in this study and evaluated for development of solid fusion. All these patients were followed up to 4 years postoperatively, with a minimal observation of 3 years.
It is well known that smoking is deleterious for spinal fusion. In the present series no difference in the fusion rate between smokers and non-smokers as well as between individuals of different groups was shown in any of the three groups on the plain roentgenograms and axial CT-scan views. However, quantitative analysis of bony mass fusion is required to accurately estimate fusion mass.
There were 30 patients with two and 27 with three instrumented levels in this series. In particular, ten patients in group A, nine in group B and nine in group C had two level instrumentation, while nine patients of group A, nine in group B and 11 in group C received three levels instrumentation.
The duration of surgery was 135±18 min for group A, 146±30 min for group B and 118±18 min for group C. The duration of surgery in the group C was significantly lower than that of groups B and A (P=0.02 and 0.04, respectively).
The measured intraoperative and postoperative blood loss was 554±76 cc for group A, 504±125 cc for group B and 371±36 cc for group C. The perioperative blood loss in group C was significantly less than at in group A (P=0.001) and B (P=0.01).
Significant disturbing donor site complaints were reported by four patients of group A and three patients of group B.
The average intraobserver and interobserver coefficient values (r) in the radiologic evaluation of spinal fusion (Christiansen’s grading system) were 0.71 and 0.69, respectively. The average intraobserver and interobserver values (r) in the radiologic evaluation of coralline resorption in the intertransverse region were 0.83 and 0.76, respectively.
The sagittal alignment of the lumbar spine was preserved postoperatively during the entire follow-up period. No change was measured postoperatively in the preoperative value of T12−S1 lumbar lordosis in any group (P=0.6) until the last evaluation.
There was no olisthesis on the frontal and sagittal plane or increased intersegmental angulation within the instrumented spine in any spine and group during the follow up observation.
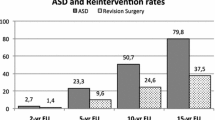
On the AP views of the spines in group A, there was an increasing intertransverse and posterior bony bridging that was present as early as 3 months postoperatively (Fig. 2a) and was completed 1 year postoperatively (Fig. 2b). Six months postoperatively, both posterior spinal element and facet joint fusion was observed on the oblique views within the instrumented spine (Fig. 2c). The CT scan showed solid fusion in the facet joints 1 year postoperatively.
a Anteroposterior view of the lumbar spine in a 46-year-old female patient 3 months postoperatively, showing increasing intertransverse bony bridging (group A). b AP view of the lumbar spine of the patient in a 1 year postoperatively, demonstrating solid intertransverse fusion. c Oblique view of the lumbar spine of the same patient in a, b 6 months postoperatively, showing complete posterior fusion and facet joint arthrodesis
On the AP views in group B, an increasing resorption of the CH granules was evident 6 months postoperatively on the right side between the transverse processes (Fig. 3a) and was completed 1 year postoperatively (Fig. 3b). The resorption was completed with the disappearance of almost all CH granules, with the exception of those situated at the base of the transverse processes and laminae at all levels of fusion. Parallel to the resorption of CH granules, an increasing intertransverse bony bridging on the contralateral side (left side) was observed in sites where autologous IBG was applied. One year postoperatively, there was a solid dorsal fusion on both sides. The oblique views (Fig. 2c) and the CT scan confirmed the solid fusion of the facet joints.
a Anteroposterior view of the lumbar spine of a 54-year-old female patient immediately postoperatively, showing coralline HA granules placed in the intertransverse spaces bilaterally (group C). b AP roentgenogram of the lumbar spine of the patient in a 1 year post-operation, demonstrating almost complete resorption of coralline HA granules on both sides. c Oblique view of the lumbar spine of the patient in a 6 months postoperatively, showing continuous bony bridging over the lamina and fused facet joints in all levels of instrumentation
On the AP views in the spines of group C, a resorption of CH on both sides was observed with an identical picture as in the right side of the spines of group B. The oblique views of the instrumented spine showed 6 months postoperatively continuous posterior bridging associated with facet fusion (Figs. 1c, 3c). One year postoperatively, solid posterior fusion and facet joint fusion was evident on the plain roentgenograms and in the CT-scan views. There were no significant differences in the pre- and postoperative responses of any of the SF-36 parameters between the individuals of the three groups.
The preoperative ODI score was improved postoperatively in all groups up to the 2-year follow-up; namely, 41±27%, 47±39% and 43±28% for groups A, B and C, respectively; thereafter no significant changes were measured.
The preoperative R-M score was improved up to the 2-year follow-up at 47±43%, 60±46%, 55±28% for groups A, B and C, respectively; thereafter no significant changes were shown in any group.
The VAS was significantly improved postoperatively in all groups and reached its highest value 2 years postoperatively. The preoperative value (average ± standard deviation) was 8±1.2 for group A, 8±1.7 for group B and 7±2 for group C. The postoperatively VAS value was 4.7±3.6 for group A, 3.5±3.1 for group B, and 3.7±2.7 for group C.
One superficial infection without deep contamination was observed in a patient in group B and one deep hematoma without contamination in a patient of group A; Both patients were operated with evacuation and drainage for 3 days plus antibiotics and showed an uneventful course.
There was one screw breakage (L5) in a patient of group A with two-segment instrumentation, 18 months postoperatively (Christiansen’s score 3 at the level of screw breakage), and two screw breakages (S1 and L5) in group C (L2–L5 instrumentation) at 3 years and (L2−S1) at 6 months postoperatively (grade 3 at the level of screw failure). Although no signs of pseudarthrosis were shown radiologically, we consider that the spines with material failure should have non-union.
Discussion
This prospective randomized longitudinal study compared the evolution of posterior and lateral (intertransverse) lumbar fusion in three comparable groups of adult patients who underwent decompression, transpedicular instrumentation and fusion for degenerative lumbar spine stenosis over a similar spinal segments and disclosed radiological solid fusion in all spines and levels in all three groups 1 year postoperatively. In particular, all spines that were augmented bilaterally with autologous IBG (group A) showed solid intertransverse plus posterior fusion 1 year post-operation. In the spines of the groups B and C where the CH mixture was applied, a progressive resorption of CH granules was shown in the intertransverse space only, which started 6 months postoperatively and completed 1 year post-surgery without significant bone bridging between the involved transverse processes. However, all patients in all groups independently of the graft they received and the levels that instrumented, showed no pathological motion in the latest postoperative AP and lateral bending tests, while the facet joint fusion was evident (X-rays, CT) in all instrumented levels, suggesting solid fusion. In addition to uneventful radiological course, all patients of all groups showed similarly improved self-assessment postoperative scores.
There are several radiological studies in humans and animals or histological studies in animals that investigated the course of CH resorption and parallel bone formation. To the authors’ knowledge there is only one histological study in humans [29] that studied the course of bone formation within CH in posterior instrumented spine fusion. According to this histological study [29] the specimens that were taken intraoperatively from the fusion area revealed osteoid and bone formation within the CHA (Pro-Osteon 500R) as early as 6 weeks postoperatively.
This prospective study had the advantage to investigate the evolution of posterior and intertransverse lumbar fusion in adult humans in a comparative basis (autologous IBG versus resorbable CH) under the same environment and conditions provided by the implantation in the same individual.
Two significant observations were made in this study. First, the augmentation of spinal fusion either with CH mixture or with IBG was followed definitively by solid dorsal fusion 1 year postoperatively. Secondly, the use of CH mixture over the transverse processes was followed by resorption without sufficient bone formation, in contrast to the use of IBG, which was followed by solid bone formation in all cases it was applied (groups A and B). The theoretical explanations for the latter are: first, the advantage of osteogenic property of autologous IBG; secondly the probably low ratio of local bone to CH granules (1:3) that was used in this series; and thirdly, it seems that the replacement of CH granules by bone is enhanced by the presence of a wide bone host bed with a rich blood supply as the laminae, contrary to the transverse processes that do not represent the ideal wide host bed.
Delecrin et al. [17] investigated in animals, and later in human beings [18], the influence of bone enviroment on ceramic osteintegration in lumbar spinal fusion by comparing bone-poor (intertransverse) and bone-rich (laminar) sites. These authors showed that no in-growth was significantly lower for ceramic implanted at the lumbar intertransverse than laminar site. These findings of Delecrin et al. [17, 18] justify the results of the present study regarding better posterior interlaminar than intertransverse fusion as well as the absorption of CH granules from the intertransverse area.
The ratio CHA to autologous IBG in the mixture that is used for posterior spinal fusion is an issue of diversity between the investigators: Mashoof et al. [32], who used CH as an IBG extender in instrumented scoliosis, correlated radiological fusion and clinical result, while Baramki et al. [5] proposed at least a 50:50 ratio to achieve solid fusion. Thalgott et al. [42] compared CHA and demineralized bone matrix as an adjunct to autologous bone, and showed a 92.5% fusion rate. CHA is an effective bone graft extender in difficult-to-fuse patients when combined with rigid instrumentation.
The authors declare that this ratio was the maximum possible deriving from decortication of posterior spinal elements. The resorption of the CHA mixture in the intertransverse space in the groups B and C did not affect the final outcome of the posterior fusion and facet arthrodesis.
The use of CH in this series was associated by several advantages: it reduced operative time significantly and subsequently the associated blood loss, while there was no morbidity deriving from the graft donor site in the patients of groups A and B. These advantages of CH are in accordance with those previously reported by others in adolescent scoliosis surgery [32].
Delecrin et al. [19] in a clinical study compared two groups of adolescent and young adult patients who were operated posteriorly for idiopathic scoliosis autogenous and received CD instrumentation supplemented with either autologous IBG or porous biphasic calcium phosphate ceramic blocks, comprising HA and tricalcium phosphate mixed with local bone chips. These authors showed that the patients who received ceramics had lower blood loss were free from postoperative local complications, while radiographically there was demonstrated successful incorporation of the ceramic blocks within 1 year. These findings justify the results of our present study regarding successful use of CHA mixed with local bone chips in posterior instrumented lumbar fusion, which usually occurs 1 year postoperation.
Cavagna et al. [14] investigated the clinical performance of macroporous calcium ceramics mixed with bone chips and bone marrow, in reinforced with semirigid instrumentation lumbar fusion in patients with degenerative disease and showed that such ceramics are a good alternative to autografts and could decrease patient morbidity resulting from iliac bone grafting. Thus, the authors concluded that the macroporosity and the chemical compound (biphasic calcium phosphate) seem to have an important role for the lumbar fusion.
Posterolateral spinal arthrodesis with autologous IBG is the “gold standard” procedure for lumbar fusion. Autograft offers complete histocompatibility and virtually no inflammatory encapsulation of the graft material, it is non-pathogenic and possesses combined osteoconductive, osteoinductive and osteogenic properties. Complication rates associated with autografting vary significantly and depend on the source of the autograft. In particular, minor complications following autografting include superficial infections [41], seromas, hematomas, altered sensation in a rate ranging from 3.1% to 39% [1, 3], while the pseudarthrosis rate for a single-level fusion ranges from 3.5% to 40% [6, 7, 33, 40, 44] and increases as the number of segments to be fused increases. Allograft has been used as an alternative to autologous graft, but the possible risk of infection [44] and the reported inferior rate of union and healing [2, 10, 22, 24, 31] have limited its use.
Pro-Osteon 500R is formed through a hydrothermal exchange reaction of marine coral. This process converts the calcium carbonate coral exoskeleton to hydroxyapatite, a form of calcium phosphate, while maintaining its natural porous structure. Pro-Osteon 500R is being investigated for a potentially more predictable resorption profile [43].
An alternative source of autologous osteoprogenitor cells lies in the bone marrow. The bone marrow provides a rich source of cells ranging from mesenchymal stem cells, which are undifferentiated stem cells, to cells that have already committed down the osteogenic lineage and are destined to become osteoblasts. Successful use of autologous bone marrow has been described alone [12] or in combination with other graft substitutes [4, 37]. Bone marrow can be obtained from the iliac crest using percutaneous needle aspiration, which does not cause morbidity. In this series, autologous bone marrow was aspirated from the pedicles of the instrumented vertebrae before screw placement. This placement does not increase morbidity. However, the osteogenic properties of the bone marrow that was mixed with CHA and bone chips did not enhance intertransverse fusion in groups B and C, because of the small quantity of the autologous bone chips and/or bone marrow or/and a deficient bone host. An additional cause of bone marrow failure in this series of adult patients may be patient age, since the ratio of osteoprogenitor in bone marrow decreases significantly in the elderly [12].
Delecrin et al. [18] underlined the significance of bone marrow enrichment of the lumbar intertransverse site: bone marrow addition greatly facilitated ceramic osteointegration. The significance of bone marrow addition was also shown in our study.
Delecrin et al. [18] showed that the vertebral interbody site, despite theoretical richness of osteogenic precursor cells, might be bone-poor at the time of grafting compared with the reference IBG. Furthermore, Delecrin et al. [18] concluded that the bone marrow taken from the iliac crest is significantly more rich in bone marrow progenitor cells than the bone marrow taken from vertebra.
The radiologic evaluation of dorsolateral lumbar fusion is traditionally studied in non-instrumented fusions on the AP views. Hardware makes assessment of bony fusion difficult with the use of plain roentgenograms only [15]. Because of these difficulties the authors of this study used oblique views, bending tests and CT scans that justified solid fusion in all patients and all fused segments. However, in the presence of allografts and ceramics the interpretation of solid fusion seems to be difficult, particularly when hardware is added. In contrast, Christensen et al. [15] compared non-instrumented lumbar fusion versus instrumented with Cotrel Dubousset (CD) instrumentation and reported similar interobserver and intraobserver agreement. In particular Christensen et al. [15] reported in the CD group κ values of 0.63 and 0.81 for interobserver and intraobserver agreement, respectively; while in the non-instrumented spines for the interobserver and intraobserver agreement the κ values were 0.52 and 0.73, respectively. The authors in the present study used Christensen’s system to evaluate fusion in instrumented lumbar spines and had an average intraobserver and interobserver coefficient, r, of 0.71 and 0.69, respectively.
Baramki et al. [5] used interconnected CHA for experimental fusion in animals and proposed a roentgenographic method and grading (a four-point grading system) for evaluation of fusion masses in animals, with the use of CT and reconstruction images. The authors of the present study used CT scan to evaluate the facet joint arthrodesis.
In general, the literature describing the classification criteria used for radiograph interpretation of spinal posterolateral fusion has serious deficiencies. In the past, most studies analyzing the success of spinal fusion using autograft, allograft, or bone substitutes have relied mainly on plain film radiographs [8, 9, 35, 36]. The assessment of spinal fusion with autologous IBG was traditionally based on the presence or absence of trabecular bone or a fusion mass. Others [32], however, using coralline HA in adolescent scoliosis, considered the radiological appearance of “marbilization” of posterior fusion mass as complete bony fusion when it combined with clinical stability. The combined static (plain roentgenograms) and dynamic (bending roentgenograms) roentgenographic evaluation of the fusion was proven in this series a reliable method in evaluating fusion progress. Although the authors are aware that radiological fusion is not always associated by excellent clinical results, in the present study radiology, self-assessment surveys and VAS scores were in accordance in all patients. Other authors also used dynamic spinal roentgenograms for the evaluation of spinal fusion [20, 21, 25].
Baramki et al. [5] used plain roentgenograms in animals and experienced some difficulty in interpreting bone mass fusion within interconnected porous HA because of the radiodense HA granules.
The efficacy of HA in achieving lumbar spinal fusion in humans has been reported only anecdotally [34, 38]. Biomechanical studies in animals [5, 27, 42] compared spinal arthrodesis using interconnected HA alone or mixed with bone as graft material and reduced spinal segmental motion. Baramki et al. [5], however, noted that HA was not as effective as autologous bone graft material in achieving spinal arthrodesis in animals.
The surgical procedure did not produce any serious complications in any group. No pseudarthrosis or deep infection occurred in any patient and any group, while the delayed screw failures that were observed were not associated with pseudarthrosis or delayed union.
The advantages of the present study are: (1) surgical consistency, since all surgeries were performed by the principal investigator; (2) the random selection of the patients to be included in each group; (3) the minimization of bias, since the identity of the group was revealed to the surgeon after the pedicle screws were placed and the graft bed prepared; (4) the constant volume of the graft material for each segment of fusion, allowing comparison of the fusion progress per level.
Conclusion
This prospective randomized study showed that autologous iliac bone graft remains the gold standard for achieving solid posterior instrumented lumbar fusion, to which each new graft should be compared. The incorporation of CH, mixed with local bone chips and bone marrow derived from vertebra, which, however, is inferior to that derived from the iliac crest, needs adequate bleeding bone surface. Subsequently hydroxyapatite was proven in this series to be inappropriate for intertransverse posterolateral fusion, because the host bleeding bone surface in this area is small. However, the use of hydroxyapatite over the decorticated laminae, which represents a wide host area that offers much more bone chips from decortication, was followed by solid dorsal fusion within the expected time.
References
Abott LC (1944) The use of iliac bone in the treatment of ununited fractures. In: Instructional Course Lectures. The American Academy of Orthopaedic Surgeons, Park Ridge, pp 13–22
An HS, Simpson JM, Glover JM, Stephany J (1995) Comparison between allograft plus demineralized bone matrix versus autograft in anterior cervical fusion: a prospective multicenter study. Spine 20:2211–2216
Arrington ED, Smith WJ, Cambers HG, et al (1996) Complications of iliac crest bone graft harvesting. Clin Orthop 329:300–309
Banwart JA, Asher MA, Hassanein RS(1995) Iliac crest bone graft harvest donor site morbidity. A statistical evaluation. Spine 20:1055–1060
Baramki GH, Steffen T, Lander P, Chang M, Marchesi D (2000) The efficacy of interconnected porous hydroxyapatite in achieving posterolateral lumbar fusion in sheep. Spine 25:1053–1060
Bernardt M, Swartz DE, Clothiaux PL, Crowell RR, White AA (1992) Posterolateral lumbar and lumbosacral fusion with and without pedicle screw internal fixation. Clin Orthop 284:109–115
Boachie-Adjei O, Dendrinos GK, Ogilvie JW, Bradford DS (1991) Management of adult spinal deformity with combined anterior-posterior arthrodesis and Luque-Galveston instrumentation. J Spinal Disord 4:131–141
Boden SD, Schimandle JH, Hutton WC (1995) An experimental lumbar intertransverse process spinal fusion model. Radiographic, histologic and biomechanical healing characteristics. Spine 20:412–420
Boden SD, Schimandle JH, Hutton WC et al (1997) In vivo evaluation of a resorbable osteoinductive composite as a graft substitute for lumbar spinal fusion. J Spinal Disord 10:1–11
Brantigan JW, McAfee PC, Cunningham BW, Wang H, Orbegoso CM (1994) Interbody lumbar fusion using a carbon fiber cage implant versus allograft bone: an investigational study in the Spanish goat. Spine 19:1436–1444
Bucholz MP, Carlton A, Holmes RE (1994) Interporous hydroxyapatite as a bone graft substitute in tibial plateau fractures. Clin Orthop 240:53–62
Burchardt H (1983) The biology of bone graft repair. Clin Orthop 174:28–42
Burwell RG (1985) The function of bone marrow in the incorporation of bone graft. Clin Orthop 200:125–141
Cavagna R, Daculsi G, Bouler JM (1999) Macroporous calcium phosphate ceramic: a prospective study of 106 cases in lumbar spinal fusion. J Long Term Eff Med Implants 9:403–412
Christensen BF, Laursen M, Gelineck J, Eiskj R, PS Thomsen K, Bunger EC (2001) Interobserver and intraobserver agreement of radiograph interpretation with and without pedicle screw implants. Spine 26:538–544
Connolly JF, Guse R, Lippiello L et al (1989) Development of an osteogenic bone marrow preparation. J Bone Joint Surg 71:684–691
Delecrin J, Aguado E, Nguyen JM, Royer J, Passuti N (1997) Influence of local enviroment on incorporation of ceramic for lumbar fusion. Comparison of laminar and Intertransverse fusion in a canine model. Spine 22:1683–1689
Delecrin J, Deschamps C, Romih M, Heymann D, Passuti N (2001) Influence of bone enviroment on ceramic osteointegration in spinal fusion: comparison of bone—poor and bone rich sites. Eur Spine J 10 (Suppl 2): S110–S113
Delecrin J, Takahashi S, Gouin F, Passuti N (2000) A synthetic porous ceramic as a bone substitute in the surgical management of scoliosis: a prospective randomized study. Spine 25:563–569
Dvorac J, Panjabi MM, Chang DG, Theiler R, Crob D (1991) Functional radiographiv diagnosis of the lumbar spine. Flexion–extension and lateral bending. Spine 16:562
Dvorac J, Panjabi MM, Novotny JE, Chang DG, Crob D (1991) Clinical validation of functional flexion–extension roentgenograms of the lumbar spine. Spine 16:943
Enneking WF, Early JL, Burchardt H et al (1980) Autogenous cortical bone grafts in the reconstruction of segmental skeletal defects. J Bone Joint Surg 62:1039–1058
Enneking WF, Mindell ER (1991) Observations on massive retrieved human allografts. J Bone Joint Surg Am 73:1123–1142
Friedlaender GE, Goldberg VM (eds) (1991) Bone and cartilage allografts: biology and clinical application. American Academy of Orthopaedic Surgeons, Park Ridge
Frobin W, Brinckmann P, Leivesth G, Biggemann M, Reikeras O (1996) Precision measurement of segmental motion from flexion–extension radiographs of the lumbar spine. Clin Biomech 11:457–465
Glaser J, Stanley M, Sayre H, Woody J, Found E, Spratt K (2003) A 10-year follow-up evaluation of lumbar spine fusion with pedicle screw fixation. Spine 28:1390–1395
Guigui P, Plais PY, Flautre B et al (1994) Experimental model of posterolateral spinal arthrodesis in sheep part 2 application of the model: evaluation of vertebral fusion obtained with coral (Porites) or with a biphasic ceramic (Triosite). Spine 19:2798–2803
Khan SN, Tomin E, Lane JM (2000) Clinical applications of bone graft substitutes. Orthop Clin North Am 31:389–398
Korovessis P, Papazisis Z, Petsinis G (2000) Unilateral psoas abscess following posterior transpedicular stabilization of the lumbar spine. Eur Spine J 9:588–590
Korovessis P, Koureas G, Repanti M. (2002) Histological findings in revision surgery of instrumented spine fusion with the use of coralline hydroxyapatite: advances in spinal fusion-molecular science, biomechanics and clinical management. Marcel Dekker, New York
Lord CF, Gebhardt MC, Tomford WW, Mankin HJ(1988) Infection in bone allografts: incidence, nature and treatment J Bone Joint Surg Am 70:369–376
Mashoof AA, Siddiqui SA, Otero M, Tucci JJ. (2002) Supplementation of autogenous bone graft with coralline hydroxyapatite in posterior spine fusion for idiopathic adolescent scoliosis. Orthopaedics 25:1073–1076
Marchesi DG, Thalgott JS, Aebi M (1998) Application and results of the AO internal fixation system in non traumatic indications. Spine 23:159–167
Martin RB, Chapman MW, Homes RE et al (1989) Effects of bone ingrowth on the strength and non-invasive assessment of a coralline hydroxyapatite material. Biomaterials 10:481–488
Morone MA, Boden SD (1998) Experimental posterolateral lumbar spinal fusion with a demineralized bone matrix gel. Spine 23:159–167
Muschler GF, Negami S, Hyodo A, Gaisser D, Easley K, Kambic H (1996) Evaluation of collagen ceramic composite graft material in a spinal fusion model. Clin Orthop 328:250–260
Ragni P, Lindholm S (1978) Interaction of allogeneic demineralized bone matrix and porous hydroxyapatite bioceramics in lumbar interbody fusion in rabbits Clin Orthop 272:292–299
Rahimi F, Maurer BT, Enzweiler MG (1997) Coralline hydroxyapatite: a bone graft alternative in foot and ankle surgery. J Foot Ankle Surg 36:192–203
Simon SR (ed) (1994) Orthopaedic basic science, 2nd edn. American Academy of Orthopaedic Surgeons, Rosemont, pp 284–293
Simmons JW, Andersson GB, Russell GS, Hadjipavlou AG (1998) Aprospective study of 342 patients using transpedicular fixation instrumentation for lumbosacral spine arthrodesis. J Spinal Disord 11:367–374
Stricker SJ, Sher JS (1997) Freeze dried cortical allograft in posteror spinal arthrodesis. Use with segmental instrumentation for idiopathic adolescent scoliosis. Orthopaedics 20:1039–1043
Thalgott SJ, Giuffre MJ, Fritts K, Timlin M, Klezl Z (2001) Instrumented posterolateral lumbar fusion using coralline hydroxyapatite with or without demineralized bone matrix, as an adjunct to autologous bone. Spine J 2:131–137
Truumees E, Herkowitz HN(1999) Alternatives to autologous bone harvest in spine surgery. Orthop J 12:77–88
Turner JA, ErSek M, Herron L, et al (1992) Patients outcomes after lumbar spinal fusions. JAMA 268:907–911
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Korovessis, P., Koureas, G., Zacharatos, S. et al. Correlative radiological, self-assessment and clinical analysis of evolution in instrumented dorsal and lateral fusion for degenerative lumbar spine disease. Autograft versus coralline hydroxyapatite. Eur Spine J 14, 630–638 (2005). https://doi.org/10.1007/s00586-004-0855-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-004-0855-5