Abstract
The aim of this study was to compare the incidences of leakage from the catheter insertion site during continuous femoral nerve block when using the catheter-through-needle, Contiplex Touhy™ (CT) and the newly developed catheter-over-needle, Contiplex C™ (CC). Forty adult patients who were scheduled to undergo continuous femoral nerve block for pain control following knee surgery were enrolled and were randomly assigned to a CT group or a CC group. After finishing surgery, a catheter for continuous femoral nerve block was placed using ultrasound. A catheter was advanced along the femoral nerve 5–6 cm beyond the needle tip. Then 0.25% levobupivacaine was continuously administered at a rate of 5 ml/h until 9:00 am on postoperative day 1. The incidence of leakage of the local anesthetic from the insertion site in the CT group was significantly higher than that in the CC group. In the CT group, leakage from the catheter insertion site was observed in 11 of 20 patients during the observation period. On the other hand, none of the patients in the CC group showed leakage. Contiplex C™ is more effective than Contiplex Touphy™ for prevention of leakage of local anesthetics from the insertion site during continuous femoral nerve block.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Continuous femoral nerve block provides effective pain relief after total knee arthroplasty (TKA) [1]. The catheter-through-needle method, in which the catheter is placed through the needle, is usually used for continuous peripheral nerve block. Since the diameter of the needle puncture hole is larger than that of the catheter in the catheter-through-needle method, leakage of local anesthetics sometimes occurs from the catheter insertion site [2]. Recently, a catheter-over-needle, Contiplex C™ (B. Braun, Meisungen, Germany) for continuous peripheral nerve block, in which the catheter diameter is larger than that of the needle puncture hole, has become clinically available in Japan. However, it has not been determined whether the Contiplex C™ is useful to prevent leakage of local anesthetics. In this study we compared the incidences of leakage during continuous femoral nerve block when using the conventional catheter-through-needle, Contiplex Touhy™, (B. Braun, Meisungen, Germany) and Contiplex C™.
Methods
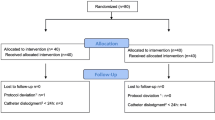
The protocol of this study was approved by the ethics committee of our institution (approval number 1598), and the trial was registered in the UMIN Clinical Trial Registry (UMIN000019895). Written informed consent was obtained from all participants.
Patients aged 20–75 year old who were scheduled to undergo continuous femoral nerve block for pain control after TKA were enrolled in this study. Patients with morbid obesity (BMI > 35), increased susceptibility to infection, or sensory/motor disturbance of the femoral nerve were excluded. Each patient was randomly assigned to the Contiplex Touhy™ (CT) group or the Contiplex C™ (CC) group using a web-based random-number generator.
Anesthesia was induced with propofol and remifentanil. After tracheal intubation, anesthesia was maintained with remifentanil and propofol or desflurane. After finishing surgery, continuous femoral nerve block was performed. All of the blocks were done by the same anesthesiologist. First, a single-shot femoral nerve block was performed to make a space to place a catheter. A transverse cross-sectional view of the femoral nerve was obtained at the inguinal crease by S-Nerve Ultrasound System™ (Sonosite, Bothell, USA). A 21-gauge needle (Sonolect needle™, Hakko, Nagano, Japan) attached to a nerve stimulator (RasinPlex HRP-10™, Hakko, Nagano, Japan) was inserted laterally near the femoral nerve by an in-plane approach. Twenty ml of 0.125% levobupivacaine was injected via the needle. After withdrawal of the 21-gauge needle, a needle of CC or CT was inserted into a perineural space by an out-of-plane approach. Then, a catheter was advanced along the femoral nerve 5–6 cm beyond the needle tip. A bolus of 20 ml of 0.25% levobupivacaine was administered via the catheter over 200 s, and the insertion site of the catheter was covered with sterile occlusive dressings (3 M™ Tegaderm™ I.V. Port Dressings, 3M, Tokyo, Japan). Then 0.125% levobupivacaine was continuously administered at 5 ml/h using an infusion pump (COOPDECH balloonjector™, Daiken iki, Osaka, Japan) until 9:00 am on postoperative day (POD) 1. Since femoral nerve block alone is insufficient to reduce postoperative pain after TKA [3], single-shot sciatic nerve block or iv PCA using fentanyl was added at each anesthesiologist’s discretion. After completion of catheter placement, the patient was extubated and moved to a ward. At 9:00 am on POD 1, bolus administration of 20 ml of 0.125% levobupivacaine via the catheter was done after removal of occlusive dressings. And then the catheter was removed.
The primary outcome was the incidence of leakage of local anesthetics. Leakage was visually assessed at three time points: after the bolus administration of levobupivacaine before starting continuous administration and before and after the bolus administration of levobupivacaine on POD 1. Leakage after bolus administration was assessed by direct observation of leakage from the insertion site (Fig. 1, left). In addition, we assessed leakage of local anesthetics by change in the color tone of the white portion of the dressing before a bolus administration on POD1 (Fig. 1, right). Secondary outcomes included time for catheter insertion (needle insertion to withdrawal), pain score using a numeric rating scale (NRS) before catheter removal on POD 1, distance from the skin to the femoral nerve, number of attempts at catheter placement, and procedure-related complications including nerve injury. Anesthesiologists, who were different from the physician who performed placement of a catheter, evaluated outcomes. Although patients were blinded to the type of catheter, evaluators were not blinded.
Image of leakage of local anesthetics from the insertion site. A left picture shows leakage after bolus administration indicated by an arrow, which was assessed by direct observation of leakage from insertion site. A right picture shows leakage of local anesthetics after continuous administration, which was assessed by change in the color tone of the white portion of the dressing indicated by dot line
We calculated that 40 patients needed to be enrolled into the study to have 80% power in order to show an absolute between-group difference of 40% in the primary outcome measure at a two-sided alpha level of 0.05, assuming a 70% leakage rate in the CT group according to our preliminary study. Data are shown as mean ± SD or medians (minimum − maximum). Data were analyzed using Fisher’s exact test or Student’s t test. Pain score was analyzed using Mann–Whitney U test. P < 0.05 was considered statistically significant.
Results
Patient’s characteristics in the two groups were not different (Table 1). The catheter was successfully placed in all patients. There was no difference between the two groups in time for catheter insertion and number of attempts at catheter placement (Table 2). All catheter placements were completed at the first or second attempt. One patient in the CT group did not receive a bolus administration of 20 ml of 0.125% levobupivacaine via a catheter at 9:00 am on POD 1 because the patient showed mild motor block in the lower leg, which completely recovered after ceasing continuous administration of levobupivacaine. Therefore, data at 9:00 am on POD 1 were collected from the remaining 19 patients in the CT group.
The incidence of leakage from the insertion site in the CT group was significantly higher than that in the CC group (Table 2). Leakage was observed in 11 patients in the CT group. In 8 of the 11 patients, leakage was observed at all three time points. In 2 of the 11 patients, leakage was observed before and after the bolus administration on POD 1. In one patient, leakage was observed before the bolus administration on POD 1. On the other hand, leakage was not observed in the CC group. The duration of continuous administration was not significantly different between the CT group and the CC group. The duration of continuous administration in patients with leakage (1128 ± 55 min) was also not significantly different from that in patients without leakage (1211 ± 53 min) in the CT group (P = 0.23). The length of the catheter insertion from the skin surface was roughly maintained until end of the experiment in both groups.
The number of patients in whom iv PCA or sciatic nerve block was used was similar in the two groups. On POD 1, pain score in the CC group was not significantly different from that in the CT group (Table 2). In the CT group, NRS of the patients with leakage (3 [0–6]) was similar to that of the patients without leakage (3.0 [0–6]) (P = 0.67). None of the patients showed procedure-related complications including nerve injury, bleeding, and infection.
Discussion
Leakage of the drug from the needle insertion site is a serious problem in continuous peripheral nerve block using the catheter-through-needle method. Glue [4] or catheter tunneling [5] has been used to prevent leakage from the insertion site. This is the first randomized control study to compare the incidences of leakage of local anesthetics from the catheter insertion site during continuous femoral nerve block when using CC and CT. The results of this study showed that CC was more effective than CT for preventing leakage. CC prevented leakage even during bolus administration, which created relative high outflow pressure. On the other hand, leakage from the insertion site was observed not only during bolus administration but also during continuous administration when CT was used.
CT has an 18-guage needle and a 20-guage catheter with 6 side holes from the tip to 14.5 mm proximal site according to data from the manufacturer. The difference in diameters can make the seal between the catheter and skin loose, resulting in leakage. On the other hand, CC has the catheter fitted over the needle like an i.v. catheter design, and does not have side holes. The diameter of the puncture hole by the needle (25-guage) is smaller than that of the catheter (19-guage). Therefore, the catheter tightly fits the skin, minimizing leakage from the insertion site. Yu et al. examined the usefulness of catheter-over-needle for prevention of leakage during continuous femoral block using finer catheter (22-guage) from those we used [6]. They also concluded that the incidence of leakage with catheter-over-needle was less than that with catheter-through-needle. The leakage of local anesthetics may result in unsuccessful postoperative pain relief. However, NRS of the patients with leakage was also similar to that of the patients without leakage in the CTN group. In our study, 14 of 20 patients in each group received iv PCA in addition to continuous femoral nerve block. Iv PCA might have made it difficult to detect the difference in the postoperative pain between the two groups.
In conclusion, CC is more effective than CT for the prevention of leakage of local anesthetics from the insertion site during continuous femoral nerve block.
References
Paul JE, Arya A, Hurlburt L, Cheng J, Thabane L, Tidy A, Murthy Y. Femoral nerve block improves analgesia outcomes after total knee arthroplasty. Anesthesiology. 2010;113:1144–62.
Ilefeld BM. Continuous peripheral nerve blocks: a review of published evidence. Anesth Analg. 2011;113:904–25.
Davis AF, Segar EP, Murdoch J, Wright DE, Wilson IH. Epidural infusion or combined femoral and sciatic nerve blocks as perioperative analgesia for knee arthroplasty. Br J Anaesth. 2004;93:368–74.
Klein SM, Nielsen KC, Buckenmaler CC 3rd, Kamal AS, Rubin Y, Steele SM. 2-octyl cyanoacrylate glue for the fixation of continuous peripheral nerve catheters. Anesthesiology. 2003;98:590–1.
Boezaart AP, de Beer JF, du Toit C, van Rooyen K. A new technique of continuous interscalene nerve block. Can J Anaesth. 1999;46:275–81.
Yu B, Hu X, Zou T, He M, Cai G. Effects of postoperative continuous femoral nerve block analgesia with Braun continuous peripheral nerve block catheter set versus novel needle–over–cannula after total knee arthroplasty. Med Sci Monit. 2015;21:1843–9.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Nogawa, R., Maruyama, T., Kimoto, Y. et al. Comparison of catheter-over-needle and catheter-through-needle on leakage from the catheter insertion site during continuous femoral nerve block. J Anesth 32, 439–442 (2018). https://doi.org/10.1007/s00540-018-2479-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-018-2479-7