Abstract
Background
The overlap between functional dyspepsia (FD) and irritable bowel syndrome (IBS) is associated with more severe gastrointestinal (GI) symptoms and lower quality of life. However, the gender differences in FD-IBS overlap remain unclear. This study aimed to investigate the gender differences in patients with FD-IBS overlap.
Methods
Controls and cases were prospectively enrolled from July 2019 to June 2020 at nine tertiary referral centers. The patients underwent esophagogastroduodenoscopy, and their symptoms were evaluated using a questionnaire including GI symptom-related items and the Hospital Anxiety Depression Scale (HADS). FD and IBS were diagnosed according to the Rome IV criteria, and the clinical characteristics of the FD-IBS overlap group were compared with those of the FD-only or IBS-only group.
Results
Among 667 subjects (334 healthy controls, 168 with FD-only, 37 with IBS-only, 128 with FD-IBS overlap), the FD-IBS overlap group (19.2%) showed a higher rate of preference for dairy products, a higher rate of history of Helicobacter pylori eradication, and higher HADS scores than the non-overlap group (P < 0.05). In the FD-IBS overlap group, men complained of reflux symptom and loose/watery stools more than women (P < 0.05), whereas women showed more severe GI symptoms, especially epigastric pain/burning symptoms, and higher depression scores than men (all P < 0.05).
Conclusions
FD-IBS overlap patients are associated with severe upper GI symptoms and depression compared to non-overlap patients. Moreover, women with FD-IBS overlap experience more severe GI and depression symptoms than men.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Functional gastrointestinal (GI) disorders (FGIDs) are chronic recurrent GI symptoms in the absence of organic abnormalities [1]. FGID is a common disease category encountered in gastroenterology clinics, and is considerably associated with psychosocial factors such as stress, anxiety, and depression compared with organic GI diseases [2, 3]. FGIDs can change from one disorder to another or overlap with each other during the follow-up [4, 5]. Overlap between functional dyspepsia (FD) and irritable bowel syndrome (IBS) has been commonly reported [6]. Patients with FD-IBS overlap experience frequent severe GI symptoms as well as anxiety, depression, and sleep disorder compared with patients with FD-only or IBS-only [7,8,9].
According to previous studies, most subtypes of FGIDs show a higher prevalence in women than in men [10]. In addition, different coexisting subtype patterns in men and women with FD-IBS overlap have been reported. For example, FD with postprandial distress syndrome (FD-PDS) and constipation-dominant IBS (IBS-C) are more frequent in women, whereas FD with epigastric pain syndrome (FD-EPS) and diarrhea-dominant IBS (IBS-D) are more common in men [11]. However, the gender differences in FD-IBS overlap are not well known, and previous studies either included a small number of patients or were performed at a single center, limiting the representativeness of their results. Thus, we performed a prospective nationwide multicenter study to investigate the clinical features of FD-IBS overlap compared with FD-only or IBS-only, and to evaluate the gender differences in patients with FD-IBS overlap.
Methods
Study subjects
The study subjects were prospectively enrolled from among patients who visited the gastroenterology clinic at nine tertiary referral hospitals in Korea between July 2019 and June 2020. The inclusion criteria were as follows: provision of consent to participate in the study, aged 18–80 years, and scheduled upper endoscopy procedure. Colonoscopy and abdominal imaging studies (e.g., abdominal ultrasound or abdominopelvic computed tomography) were performed with upper endoscopy in the presence of clinical indications. Healthy control subjects and patients with FGID were collected as follows: subjects who underwent GI evaluations as a health check-up or for other problems based on a family history of gastric or colon cancer were categorized as healthy controls, whereas those who visited the GI clinic for the evaluation of upper or lower GI symptoms were classified as cases upon consenting to participate in this study. This classification of healthy controls and cases was finally revised in the analysis step of the questionnaire survey. The exclusion criteria were as follows: age < 18 or > 80 years, organic GI disease (e.g., malignancy), previous gastrectomy, relevant comorbidities (e.g., moderate to severe cardiovascular, respiratory, hepatobiliary, pancreatic, renal, or neurologic disorder), recent use of medications that may affect GI symptoms (e.g., proton pump inhibitors or anti-histamine agents, or antibiotics), and pregnant or breastfeeding status among women. The number of subjects allocated to the healthy control and case groups at each hospital were agreed on by the participating GI doctors. The study protocol was approved by the institutional review board of each participating center. Informed consent was obtained from all subjects.
Diagnostic questionnaire and demographic data
All subjects were requested to complete a questionnaire. The questionnaire collected demographic data such as age, sex, height, weight, current residence, education level, marital status, employment level, household income, smoking and alcohol drinking status, recent use of aspirin or non-steroidal anti-inflammatory drug (NSAID) (≥ 1/week), consumption of dairy products (≥ 5/week), consumption of high-salt diet (defined as adding salt after tasting food), consumption of spicy food, and a history of Helicobacter pylori (H. pylori) eradication. An H. pylori-positive status was defined as a positive result of either histology or rapid urease test. The presence of upper GI symptoms (e.g., dyspepsia, postprandial distress, epigastric pain, and reflux symptom) and lower GI symptoms (e.g., abdominal pain associated with bowel movement, decreased bowel movement, hard or lumpy stool, a feeling of incomplete bowel movement, use of finger enema, and loose or watery stool) during the previous 6 months were investigated. FD was defined according to the Rome IV criteria and classified as FD-PDS, FD-EPS, and mixed type (FD-mixed), as previously described [11]. IBS was defined according to the Rome IV criteria and classified as IBS-C, IBS-D, and mixed-type IBS (IBS-M), as previously described [11]. FD-IBS overlap was defined as the patients who were diagnosed as both FD and IBS. Representative GI symptoms were classified according to frequency and severity. Symptom severity was calculated by adding the severity scores (from 0 to 4, 0 = absent, 4 = severe). For mental symptoms, the Hospital Anxiety Depression Scale (HADS) score was used to identify possible anxiety and depression in the subjects [12].
Statistical analysis
Continuous variables are expressed as means ± standard deviation and compared using the t test. Categorical variables are expressed as percentages and compared using the Chi-square test or Fisher’s exact test. Comparisons among three or more groups were performed using the Chi-square test with Bonferroni correction or analysis of variance followed by Tukey’s test. P < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS 25.0 (IBM, Armonk, NY, USA).
Results
Demographic and baseline characteristics
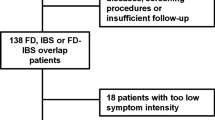
A total of 667 subjects participated in this study. The mean age was 55.3 ± 13.1 (range 20–88) years, and 393 (58.9%) were women. Among them, 333 subjects were identified as having FD or IBS, including 128 patients (38.4%) who met both the FD and IBS criteria (FD-IBS overlap), whereas 334 subjects were identified as healthy controls. The prevalence of FD in patients with IBS was 77.6% (128/165), and the prevalence of IBS in patients with FD was 43.2% (128/296) (Fig. 1). Subjects with FD-IBS overlap showed a higher rate of preference for dairy products than those with FD-only or IBS-only, and a higher rate of H. pylori eradication history than those with IBS-only (P < 0.05) (Table 1).
Frequency and severity of GI symptoms and mental symptoms
The representative upper and lower GI symptoms and mental symptoms (anxiety and depression) in each group were evaluated. All upper and lower GI symptoms, except for the use of finger enema, were significantly more frequent in the FD-IBS overlap group than in the FD-only group, and all upper GI symptoms were significantly more frequent in the FD-IBS group than in the IBS-only group (all P < 0.05) (Table 1). With respect to mental symptoms, the FD-IBS overlap group showed significantly higher HADS anxiety scores than the FD-only group and significantly higher HADS depression scores than the FD-only or IBS-only group (P < 0.05) (Table 1).
Gender difference in GI and mental symptoms and risk factors of overlap syndrome
To investigate gender differences, we separately evaluated men and women with FD-IBS overlap. The distribution of the FD and IBS subtypes differed between men and women (Fig. 2). With respect to the frequency of GI symptoms, men with FD-IBS overlap had significantly higher reflux symptom (P = 0.004), and loose or watery stools (P = 0.016) than women. However, women with FD-IBS overlap were commonly to have bloating, vomiting, decreased bowel movement, and hard or lumpy stools compared to men, although there was no significant difference (Fig. 3). Concerning the severity of GI symptoms, women with FD-IBS overlap had more severe epigastric pain/burning symptom (P = 0.008) than men. However, men with FD-IBS overlap commonly had severe symptoms of vomiting, hard or lumpy stools, a feeling of incomplete bowel movement, and use of finger enema compared to women, although there was also no significant difference (Fig. 4). For mental symptoms, women with FD-IBS overlap were more likely to experience depression than men (HADS depression scores, men vs. women, 6.9 ± 2.9 vs. 8.2 ± 3.4; P = 0.029) (Fig. 5).
Distribution of subtypes of functional dyspepsia and irritable bowel syndrome in patients with overlap syndrome. a Subtypes of functional dyspepsia, b Subtypes of irritable bowel syndrome. EPS epigastric pain syndrome, FD functional dyspepsia, IBS-C constipation-dominant irritable bowel syndrome, IBS-D diarrhea-dominant irritable bowel syndrome, IBS-M mixed type irritable bowel syndrome, PDS postprandial distress syndrome
Multivariate analysis showed that the risk factors for FD-IBS overlap in men with FD were milk or dairy product consumption, gastroesophageal reflux symptom (GERS), and loose or watery stools, whereas those for FD-IBS overlap in women with FD were loose or watery stools and depression (all P < 0.05). The risk factors for FD-IBS overlap in men with IBS were bloating and GERS, whereas those for FD-IBS overlap in women with IBS was GERS (all P < 0.05) (Table 2).
Discussion
In this prospective nationwide multicenter survey study in Korea, FD-IBS overlap showed a high prevalence (19.2%; 128/667) which lies in the middle of the prevalence rates reported in previous studies (5–36.7%) [11, 13, 14]. The prevalence of FD in patients with IBS was 77.6% (128/165) and that of IBS in patients with FD was 43.2% (128/296), consistent with previous studies (29–87% and 13–48.9%, respectively) [6, 11, 13, 14]. The FD-IBS group showed frequent and severe GI symptoms and higher HADS scores compared to the non-overlap group. With respect to gender differences, women with FD-IBS overlap showed more severe GI symptoms associated with decreased bowel movement and higher HADS depression scores than men with FD-IBS overlap. Most of these main findings have been reported in several studies partly based on Rome III criteria; however, our study was a comprehensive analysis based on Rome IV criteria [15].
In the present study, the FD-IBS group showed a significantly higher preference for milk or dairy products than the non-overlap group (P < 0.05) (Table 1), especially men. Milk and dairy products are frequently identified as triggering symptoms in patients with FD, with some positive results in provocation studies [16], and are also known to aggravate IBS symptoms [17]. Lactose intolerance and fat-containing milk or dairy products are considered to be the causes of this relationship. The reason for the gender difference in FD-IBS overlap is not certain: however, it could be related to several reasons. One reason is that men usually do not pay as much attention to food as women [18,19,20]. Moreover, men with FD-IBS overlap showed higher rates of aspirin or NSAID use and preference for salty food than non-overlap patients in the present study (P < 0.05); however, women with FD-IBS overlap did not show this characteristic. In addition, there could be a gender difference in gut microbiota or small-bowel bacterial overgrowth, as suggested in previous studies [21,22,23,24,25,26]
In the present study, the FD-IBS group also showed a higher rate of H. pylori eradication history than the IBS-only group (P = 0.001). However, the rate of current H. pylori infection determined by histology or rapid urease test was not significantly different between the FD-IBS overlap group and the non-overlap group (Table 1), which is consistent with a previous report [27]. Before 2018, the Korean health insurance system allowed H. pylori eradication only for peptic ulcer, gastric cancer, and mucosa-associated lymphoid tissue lymphoma; thus H. pylori-related dyspepsia was not the main target of eradication therapy. In addition, the effect of eradication on the improvement of dyspepsia in Asia was reported to be not as significant compared to that in Western countries [28]. However, as the FD-IBS group had frequent and severe GI symptoms, H. pylori eradication might have been attempted for relieving symptoms more frequently in FD-IBS group than FD-only or IBS-only group.
In a previous study, patients with FD-IBS overlap showed a significantly higher prevalence of fullness, bloating, early satiety, and weight loss and higher symptom severity score than patients with FD-only [8]. Patients with FD-IBS overlap also showed higher symptom severity scores in general abdominal discomfort/pain, early satiety, postprandial fullness, bloating, nausea, and other constipation-related items than non-overlap patients [11, 13]. Interestingly, an Australian study showed that the prevalence of FD-IBS overlap was 23% based on routine clinical assessment, which increased up to 64% when based on a standardized assessment with a questionnaire, and the severity of FD and IBS symptoms were significantly higher in patients with FD-IBS overlap than in the FD-only or IBS-only [29]. In addition, a recent Chinese study showed that FD-IBS overlap patients showed significant impairment in 36-item Short-Form Health Survey, a higher level of anxiety compared to belching disorder/functional heartburn-IBS overlap, and elevated depression score compared to IBS only patients [30]. In the present study, most of the GI symptoms were more frequent and severe in the FD-IBS overlap group than in the FD-only or IBS-only group (Table 1). Accordingly, early detection of FD-IBS overlap and suggestion for proper treatment are important to improve the patients’ QoL. Patients with FD-IBS overlap have a risk of developing mental illness such as anxiety, depression, and somatization [6]. In the present study, significant differences were found in the HADS anxiety and depression scores between the FD-IBS overlap group and the FD-only group (P < 0.001), as well as in the HADS depression scores between the FD-IBS overlap group and the FD-only group (P < 0.001) or IBS-only group (P = 0.023) (Table 1).
Generally, FGIDs are more prevalent in women than in men. The reason for this trend is believed to be the differences in sex hormones, visceral hypersensitivity, response to stress, and expression of inflammatory cytokines between men and women [31, 32]. The prevalence of FD is much higher in women than in men (1.4–2.7:1)[33], and women with FD more commonly experience anxiety, depression, and reduced QoL [34]. In a previous study on the association between FD and body mass index, underweight was a risk factor for FD in men, whereas both underweight and obesity were risk factors for FD in women [35]. With respect to IBS, estrogen and progesterone affect bowel motility and estrogen enhances pain sensitivity, whereas testosterone has an analgesic effect. On the basis of these findings, women are considered to be more vulnerable to IBS than men, and we hypothesized that the FD-IBS overlap group might show a women predominance compared with the non-overlap group [8]. However, in the present study, we found no significant gender difference in each group and the proportion of women in the FD-IBS group (60.2%) was similar to that of FD-only (68.5%) or IBS-only group (64.9%) (Table 1). In a previous study, the proportion of women in the FD-IBS overlap group was significantly higher than that in the IBS-only group, but not in the FD-only group, and gender was not a significant risk factor of overlap among the FD-only and IBS-only groups [11]. Thereby, female may not be a consistent risk factor for FD-IBS overlap. Further studies are needed to confirm this finding.
A previous study suggested the aggregation of subtypes in FD-IBS overlap, such as FD-PDS/IBS-C and FD-EPS/IBS-D [11]. In the present study, the proportion of FD-mixed and IBS-C was higher in women than in men (Fig. 2). Previous studies reported that IBS-C had more common upper GI symptoms than IBS-D [7, 36], which was also confirmed in another study [6]. In the present study, symptoms associated with decreased bowel movement and increased pain sensitivity more severely affected women than men, although only epigastric pain/burning severity was statistically significant (P = 0.008). In addition, women showed significantly higher HADS depression scores than men (P = 0.029); however, there was no significant gender difference in the HADS anxiety scores. This result is not consistent with a previous Swedish study showing that anxiety was a risk factor for FD-IBS overlap [4], and another previous study showed a correlation between epigastric burning/pain score and HADS anxiety score in women [34]. The risk factors of overlap in patients with IBS or FD were also different between men and women. Men and women with FD with loose or watery stools were likely to have IBS overlap; however, milk or dairy product consumption and GERS in men and depression in women were additional risk factors (P < 0.05). Men and women with IBS and GERS were likely to have FD overlap, although bloating was an additional risk factor in men (P < 0.05). These gender differences may have been due to estrogen and progesterone effects; however, further studies are needed to evaluate this difference [20].
This study had some limitations. First, this was a hospital-based study and subjects were enrolled from the gastroenterology clinic. Healthy control subjects reported having to have some GI symptoms that did not meet the diagnostic criteria of FD or IBS compared with previous study [11]. Second, the number of patients in the IBS-only group was relatively small; thus, some GI symptoms might not have been fully evaluated. Third, some genetic polymorphisms that may increase the risk of IBS, FD, and FD-IBS have been reported in previous studies [11, 37]. However, owing to the nature of the present study, which was been performed in nine nationwide centers in Korea, genetic polymorphisms could not be evaluated. Fourth, all enrolled patients were Korean, thus the meaning of this study may be limited to the Asian FD-IBS overlap patients. Despite these limitations, our study has strengths in that the diagnoses based on the Rome IV criteria and gender differences were closely evaluated because this study was planned by the Diversity Committee of the Korean Society of Gastroenterology.
In conclusion, the overlap between FD and IBS is common and negatively affects the QoL of patients. FD-IBS overlap patients are associated with severe upper GI symptoms and depression compared to non-overlap patients. In addition, women with FD-IBS overlap experience more severe GI and depression symptoms than men. The risk factors for FD-IBS overlap in patients with FD or IBS are somewhat different between men and women. Clinicians need to understand these gender differences in FD-IBS overlap to enable personalized medicine and to help improve the QoL of patients with FGID.
Change history
26 March 2021
The original online version of this article was revised due to correct the column head of continued table 1.
Abbreviations
- FD:
-
Functional dyspepsia
- FD-EPS:
-
Functional dyspepsia with epigastric pain syndrome
- FD-PDS:
-
Functional dyspepsia with postprandial distress syndrome
- FGID:
-
Functional gastrointestinal disorder
- GERS:
-
Gastroesophageal reflux symptom
- GI:
-
Gastrointestinal
- HADS:
-
Hospital Anxiety Depression Scale
- NSAID:
-
Non-steroidal anti-inflammatory drug
- IBS:
-
Irritable bowel syndrome
- IBS-C:
-
Constipation-dominant irritable bowel syndrome
- IBS-D:
-
Diarrhea-dominant irritable bowel syndrome
- IBS-M:
-
Mixed-type irritable bowel syndrome
References
Drossman DA. Functional gastrointestinal disorders: history, pathophysiology, clinical features and Rome IV. Gastroenterology. 2016;150:1262–79.
Choung RS, Locke GR 3rd, Zinsmeister AR, et al. Psychosocial distress and somatic symptoms in community subjects with irritable bowel syndrome: a psychological component is the rule. Am J Gastroenterol. 2009;104:1772–9.
Lee SP, Sung IK, Kim JH, et al. The effect of emotional stress and depression on the prevalence of digestive diseases. J Neurogastroenterol Motil. 2015;21:273–82.
Aro P, Talley NJ, Johansson SE, et al. Anxiety is linked to new-onset dyspepsia in the Swedish population: a 10-year follow-up study. Gastroenterology. 2015;148:928–37.
Halder SL, Locke GR 3rd, Schleck CD, et al. Natural history of functional gastrointestinal disorders: a 12-year longitudinal population-based study. Gastroenterology. 2007;133:799–807.
Park JM, Choi MG, Cho YK, et al. Functional gastrointestinal disorders diagnosed by Rome III questionnaire in Korea. J Neurogastroenterol Motil. 2011;17:279–86.
Talley NJ, Dennis EH, Schettler-Duncan VA, et al. Overlapping upper and lower gastrointestinal symptoms in irritable bowel syndrome patients with constipation or diarrhea. Am J Gastroenterol. 2003;98:2454–9.
Corsetti M, Caenepeel P, Fischler B, et al. Impact of coexisting irritable bowel syndrome on symptoms and pathophysiological mechanisms in functional dyspepsia. Am J Gastroenterol. 2004;99:1152–9.
Futagami S, Yamawaki H, Shimpuku M, et al. Impact of coexisting irritable bowel syndrome and non-erosive reflux disease on postprandial abdominal fullness and sleep disorders in functional dyspepsia. J Nippon Med Sch. 2013;80:362–70.
Houghton LA, Heitkemper M, Crowell M, et al. Age, gender and women’s health and the patient. Gastroenterology. 2016. https://doi.org/10.1053/j.gastro.2016.02.017.
Choi YJ, Kim N, Yoon H, et al. Overlap between irritable bowel syndrome and functional dyspepsia including subtype analyses. J Gastroenterol Hepatol. 2017;32:1553–61.
Oh SM, Min KJ, Park DB. A study on the standardization of the hospital anxiety and depression scale for Koreans: a comparison of normal, depressed and anxious groups. J Korean Neuropsychiatr Assoc. 1999;38:289–96.
Yao X, Yang YS, Cui LH, et al. The overlap of upper functional gastrointestinal disorders with irritable bowel syndrome in Chinese outpatients: a multicenter study. J Gastroenterol Hepatol. 2016;31:1584–93.
Wang A, Liao X, Xiong L, et al. The clinical overlap between functional dyspepsia and irritable bowel syndrome based on Rome III criteria. BMC Gastroenterol. 2008;8:43.
Talley NJ. What causes functional gastrointestinal disorders? a proposed disease model. Am J Gastroenterol. 2020;115:41–8.
Feinle-Bisset C, Azpiroz F. Dietary and lifestyle factors in functional dyspepsia. Nat Rev Gastroenterol Hepatol. 2013;10:150–7.
Lee HJ, Kim HJ, Kang EH, et al. Self-reported food intolerance in Korean patients with irritable bowel syndrome. J Neurogastroenterol Motil. 2019;25:222–32.
Hummel G, Zerweck I, Ehret J, et al. The influence of the arrangement of different food images on participants’ attention: an experimental eye-tracking study. Food Qual Prefer. 2017;62:111–9.
Hummel G, Ehret J, Zerweck I, et al. How eating behavior, food stimuli and gender may affect visual attention—an eye tracking study. Eat Behav. 2018;31:60–7.
Jašarević E, Morrison KE, Bale TL. Sex differences in the gut microbiome-brain axis across the lifespan. Philos Trans R Soc Lond B Biol Sci. 2016;371:20150122.
Mueller S, Saunier K, Hanisch C, et al. Differences in fecal microbiota in different European study populations in relation to age, gender, and country: a cross-sectional study. Appl Environ Microbiol. 2006;72:1027–33.
Haro C, Rangel-Zúñiga OA, Alcalá-Díaz JF, et al. Intestinal microbiota is influenced by gender and body mass index. PLoS One. 2016;11:e0154090.
Sinha T, Vich Vila A, Garmaeva S, et al. Analysis of 1135 gut metagenomes identifies sex-specific resistome profiles. Gut Microbes. 2019;10:358–66.
Kim YS, Unno T, Kim BY, et al. Sex differences in gut microbiota. World J Mens Health. 2020;38:48–60.
Fransen F, van Beek AA, Borghuis T, et al. The impact of gut microbiota on gender-specific differences in immunity. Front Immunol. 2017;8:754.
Chen JJ, Zheng P, Liu YY, et al. Sex differences in gut microbiota in patients with major depressive disorder. Neuropsychiatr Dis Treat. 2018;14:647–55.
Kim SE, Park HK, Kim N, et al. Prevalence and risk factors of functional dyspepsia: a nationwide multicenter prospective study in Korea. J Clin Gastroenterol. 2014;48:e12–8.
Kang SJ, Park B, Shin CM. Helicobacter pylori eradication therapy for functional dyspepsia: a meta-analysis by region and H. pylori prevalence. J Clin Med. 2019;8:1324.
von Wulffen M, Talley NJ, Hammer J, et al. Overlap of irritable bowel syndrome and functional dyspepsia in the clinical setting: prevalence and risk factors. Dig Dis Sci. 2019;64:480–6.
Yao X, Yang Y, Zhang S, et al. The impact of overlapping functional dyspepsia, belching disorders and functional heartburn on anxiety, depression and quality of life of Chinese patients with irritable bowel syndrome. BMC Gastroenterol. 2020;20:209.
Lee JY. Park KS [Gender difference in functional gastrointestinal disorders]. Korean J Gastroenterol. 2018;72:163–9.
Chang L, Toner BB, Fukudo S, et al. Gender, age, society, culture, and the patient’s perspective in the functional gastrointestinal disorders. Gastroenterology. 2006;130:1435–46.
Aziz I, Palsson OS, Törnblom H, et al. Epidemiology, clinical characteristics, and associations for symptom-based Rome IV functional dyspepsia in adults in the USA, Canada, and the UK: a cross-sectional population-based study. Lancet Gastroenterol Hepatol. 2018;3:252–62.
Choi YJ, Park YS, Kim N, et al. Gender differences in ghrelin, nociception genes, psychological factors and quality of life in functional dyspepsia. World J Gastroenterol. 2017;23:8053–61.
Le Pluart D, Sabate JM, Bouchoucha M, et al. Functional gastrointestinal disorders in 35,447 adults and their association with body mass index. Aliment Pharmacol Ther. 2015;41:758–67.
Balboa A, Mearin F, Badía X, et al. Impact of upper digestive symptoms in patients with irritable bowel syndrome. Eur J Gastroenterol Hepatol. 2006;18:1271–7.
Hwang SW, Kim N, Jung HK, et al. Association of SLC6A4 5-HTTLPR and TRPV1 945G>C with functional dyspepsia in Korea. J Gastroenterol Hepatol. 2014;29:1770–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nam, K., Kim, N., Song, H.J. et al. Gender difference in the overlap of irritable bowel syndrome and functional dyspepsia: a prospective nationwide multicenter study in Korea. J Gastroenterol 56, 537–546 (2021). https://doi.org/10.1007/s00535-021-01775-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-021-01775-2