Abstract
Background
Achalasia has been reported to be associated with esophageal cancers (ECs). However, owing to the rarity of achalasia, details of achalasia-related ECs are not well investigated.
Method
The incidence of ECs in Japanese patients with achalasia and achalasia-related esophageal motility disorders (EMDs) was estimated, and risk factors for achalasia-related ECs were determined. Characteristics of ECs and treatment courses were also analyzed.
Results
Between 2010 and 2019, 2714 Japanese patients with achalasia and achalasia-related EMDs were recorded in 7 high-volume centers; 24 patients (21 men, 3 women) developed ECs. The incidence of ECs was estimated at 0.078 and 0.28 per 100 person-years from the onset and the diagnosis of disease, respectively. Kaplan–Meier estimate suggested that, in addition to a long history of achalasia, advanced age, male sex, and regular alcohol consumption were statistically significant risk factors for EC development. A prevalence of 40 ECs (12.5% multiple lesions, and 22.7% metachronal lesions) was also noted, predominantly distributed over the thoracic esophagus. All were histologically diagnosed as squamous cell carcinoma. Superficial ECs were successfully treated with endoscopic treatment in all cases, except one. Achalasia-related Barret esophagus was extremely rare, and Barret adenocarcinoma was not detected in our cohort.
Conclusion
The high relative risk of ECs was clarified in Japanese achalasia patients, although the absolute risk remained low. Therefore, surveillance endoscopy may be recommended in limited patients with several aforementioned risk factors determined. Superficial cancer can be treated with endoscopic treatment. Multiple and metachronal ECs should be screened.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Achalasia is a rare esophageal motility disorder with an unknown etiology despite being first noted more than 300 years ago [1]. Genetic inheritance, degenerative, autoimmune, and infectious factors have all been considered to play a part in the complex pathophysiology of achalasia [2,3,4]. On histopathology, achalasia is characterized by loss of the Auerbach plexus in the esophagus, and consequently, a relaxation of the lower esophageal sphincter and esophageal peristalsis are impaired [5]. The incidence of achalasia varies widely, ranging from 0.3 to 2.3 per 100,000 person-years, depending on the research design [6,7,8,9,10], but with the overall incidence considered to be almost the same over several decades [6, 11]. We previously investigated the incidence and prevalence of achalasia in Japan, which we estimated to be at 0.81–1.37 per 100,000 person-years, and 7.0 per 100,000 persons, respectively [12].
Patients with achalasia suffer from severe symptoms such as dysphagia, vomiting, and chest pain due to the mentioned abnormal esophageal motility [1, 2]. Furthermore, poor esophageal emptying causes chronic inflammation, which triggers inflammation-related carcinogenesis. Thus, achalasia is considered one of the risk factors of esophageal cancer [13]. However, the rarity of achalasia makes it difficult to estimate its real-world effect on the incidence of esophageal cancer. A meta-analysis estimated the risk of esophageal cancer in patients with achalasia and found that the absolute risk for squamous cell carcinoma (SCC) was 0.308 and that for adenocarcinoma was 0.018 per 100 person-years in these patients [14]. Esophageal adenocarcinoma risk is also considered to increase in achalasia, though the risk is substantially lower than that of SCC [15]. Overall, the incidence of esophageal cancer has ranged from 0.04 to 0.58 per patient-years of follow-up, and most studies have found an increased cancer risk of 7–33-fold in achalasia patients compared to that in the general population [16]. In summary, while the relative risk for esophageal cancer is considered markedly higher in achalasia patients, the absolute risk is still low. Hence, both the American College of Gastroenterology and the American Society for Gastrointestinal Endoscopy do not recommend routine surveillance endoscopy for esophageal cancer in patients with achalasia [16, 17]. European guidelines on achalasia likewise advise against routinely screening for dysplasia and cancer in these patients [18]. However, these studies are weighted toward the Caucasian population, and there are no large reports regarding risks to the Asian population.
To adequately estimate the cancer risk in patients with achalasia, several other factors must be considered. In recent years, the development of high-resolution manometry (HRM) has made it the gold standard test for the diagnosis of achalasia, achalasia-related esophageal motility disorders (EMDs), and its differentials, including other EMDs. At present, the Chicago classification criteria, which is based on HRM findings, are used for the diagnosis of achalasia [19]. Currently, though, there are still no established data on the relationship between HRM-diagnosed achalasia, or achalasia-related EMDs, and the risk of esophageal cancer. Furthermore, a recent new understanding of the underlying pathophysiology and the development of novel treatment for achalasia, such as per oral endoscopic myotomy (POEM) [20], enabled earlier diagnosis and early curative treatment, which may have reduced the risk of esophageal cancer.
Taking all these into account, this study aimed to estimate the current incidence and risk factors of esophageal cancer in Japanese achalasia patients using a clinical database based on medical records. We also investigated the characteristics of esophageal cancer as well as the clinical courses of patients with achalasia-related esophageal cancer.
Methods
Patients
This study was conducted at seven high-volume EMD centers in Japan. Facilities included in the study were those with more than 50 patients with achalasia during a 10-year period, from 2010 to 2019.
Patients with EMDs who were diagnosed using standard methods (HRM, esophagogram, and esophagogastroscopy), and who were treated during the study period, were recruited. Among them, patients with achalasia and achalasia-related EMDs, including esophagogastric junction outflow obstruction (EGJ-OO), as well as major disorders of peristalsis, such as Jackhammer esophagus (JE) and diffuse esophageal spasm (DES), were analyzed in this study. HRM diagnosis was based on the Chicago classification criteria v3.0 [19].
This study was part of a more extensive retrospective clinical study in patients with EMDs, including achalasia. The study was approved by the ethics committee of the respective institution (Approval Number of our facility 2019–0401) and was conducted according to the tenets set by the Declaration of Helsinki. Informed consent was obtained in the form of an opt-out system on a website. All authors had access to the study data and reviewed and approved the final manuscript.
Data retrieval and analysis
The following clinical data were retrieved from computerized medical records: patient’s sex, the onset of EMD symptoms, age at EMD diagnosis, body mass index, smoking frequency, alcohol consumption, HRM diagnosis, presence of Barret esophagus on endoscopy, and follow-up information, including patient survival. Barret esophagus [21] was classified into long-segment Barrett esophagus (LSBE) and short-segment Barrett esophagus (SSBE), defined as ≥ 3 cm or < 3 cm of columnar metaplasia that circumferentially extends above the gastroesophageal junction, respectively, according to the Japanese classification [22].
In cases of achalasia with esophageal cancer, the age at cancer diagnosis, tumor macroscopic type, tumor location (cervical; upper, middle, and lower thoracic; abdominal), treatment strategy of esophageal cancer, final histopathologic diagnosis (SCC or adenocarcinoma), and treatment course were investigated. Histological diagnosis was performed based on the Japanese classification of esophageal carcinoma [23], which categorizes neoplastic lesions confined within the epithelial layer as “carcinoma.” In contrast, these are defined as “high-grade dysplasia (HGD)/carcinoma in situ” in Western classification systems [24, 25]. SM1 (superficial invasion into the submucosa) was defined as an invasion of ≤ 200 μm below the muscularis mucosa into the submucosa in the endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD) specimen, or up to one-third in the surgical specimen. The deeper submucosal invasion was defined as SM2–3.
Analysis of esophageal cancer incidence in achalasia and achalasia-related disorders
Incidence of esophageal cancer was calculated using the formulas below, which were based on the date of onset of symptoms, diagnosis of achalasia and achalasia-related EMDs, and last follow-up date.
The numerator included the number of patients diagnosed with esophageal cancer after a diagnosis of achalasia or achalasia-related EMDs; the denominator included the period from the onset of symptoms (pattern A) or from the diagnosis of achalasia or achalasia-related EMDs (pattern B) to the last follow-up date or to the time of occurrence of esophageal cancer among the patients. Pattern A and B analyses were performed in patients with achalasia (1) and patients with achalasia and achalasia-related EMDs (2) separately. In total, the incidence of esophageal cancer was calculated using four different methods.
Statistical analysis
Patient age and period of observation were presented as mean ± standard deviation. The number and incidence of esophageal cancer per 100 patient-years were also shown. We constructed Kaplan–Meier survival curves for esophageal cancer incidence by subgroups for sex, alcohol consumption, history of smoking, and age at baseline. We performed log-rank tests to compare the curves. We did not adjust the statistical significance level in multiple comparisons for the secondary analysis. Because there was a relatively small number of esophageal cancer developments, we did not calculate hazard ratios in Cox proportional multivariate regression. The number of patients followed for over 40 years was, similarly, relatively small. We considered that the very long follow-up data used in this study could not tolerate assumptions of any data missing at random points that were necessary for survival analysis. Thus, in the survival analysis of this study, we limited the follow-up duration to 40 years. Statistical analyses were performed using SAS statistical software version 9.4 (SAS Institute, Cary, NC, USA). All reported p values were two-sided, with p < 0.05 being considered significant.
Results
Incidence of esophageal cancer with achalasia
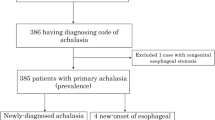
In this multicenter study, a total of 2,775 patients with EMDs were enrolled. Among them, 40 non-Japanese patients and 21 patients with other EMDs were excluded. Therefore, the final analysis included 2,714 patients with achalasia and achalasia-related EMDs (EGJ-OO, JE, and DES) and 2,523 patients with achalasia alone (Fig. 1). The details of patients’ characteristics are summarized and shown in Table 1.
Flowchart of the study analysis. Initially, 2,775 patients with esophageal motility disorders were recorded, with 40 non-Japanese patients, and 21 patients with absent contractility and minor esophageal motility disorders being excluded. A final cohort of 2,714 patients (2,523 with achalasia and 191 with achalasia-related esophageal motility disorders) were included in the final analysis
Out of 2,714 patients with achalasia and achalasia-related EMDs, esophageal cancer was identified in 24 patients (male to female ratio 21:3). During the period of observation from the onset of achalasia and achalasia-related EMDs (mean 11.3 ± 20.6 years), the annual incidence rate of esophageal cancer was 0.078 per 100 person-years; for the 1,339 men and 1,375 women, the annual incidences were 0.14 and 0.019, respectively. For all patients, from the time of diagnosis (period of observation: mean 3.1 ± 18.0 years), the annual incidence rate of esophageal cancer was 0.28 per 100 person-years. Separately, the annual incidences in men and women were 0.58 and 0.06, respectively.
The incidence of esophageal cancer in 2,523 patients with achalasia was 0.080 from the onset, and 0.28 from the diagnosis of achalasia (Table 2).
Risk factors for esophageal cancer with achalasia
In patients with achalasia and achalasia-related EMDs, risk factor analysis of esophageal cancer, controlling for sex (Fig. 2a), alcohol drinking habit (Fig. 2b), history of smoking (Fig. 2c), and age at disease onset (Fig. 2d), showed that men had a significantly increased risk of esophageal cancer over time (p = 0.0008), and that frequent alcohol intake significantly increased the risk of esophageal cancer after around 30 years (p = 0.0041). Smoking was not found to have a significant effect on esophageal cancer risk (p = 0.42). Finally, patients with elderly onset of achalasia carried an earlier and higher incidence of esophageal cancer than their younger counterparts.
Cumulative incidence of esophageal cancer in patients with achalasia and achalasia-related esophageal motility disorders. a Sex: men had a greater incidence than women; b Alcohol: daily or heavy drinkers (> 50 g per day) had a greater incidence than those who never drank or drank several times per week; c Smoking: current or previous smoking generated a higher risk, but this was not significant; d Elderly age at achalasia onset was weakly associated with esophageal cancer, both earlier on and at a higher rate
Characteristics of esophageal cancer and treatment course
Of the 24 patients with esophageal cancer following a diagnosis of achalasia and achalasia-related EMDs (Achalasia: 23, JE: 1), three (12.5%) had multiple lesions and five (20.8%) had metachronal lesions (median 24.6 months follow-up period from the initial cancer diagnosis). A total of 40 achalasia-related esophageal cancers were diagnosed (Table 3).
The interval from the onset of EMDs and the diagnosis of initial esophageal cancer was 20.2 ± 16.2 years, and the age at diagnosis of initial esophageal cancer was 64.1 ± 13.0. The ratio of men-to-women was 21:3. In cases of esophageal cancer with achalasia (n = 23), 52.2% were sigmoid (n = 6) or advanced sigmoid type [20] (n = 6) on esophagography, more common compared to that of all the cases of achalasia, which has 436 sigmoid and 146 advanced sigmoid type (23.1%) among 2,523 cases.
All 40 cancers were in the thoracic esophagus (Ce: 0, Ut: 3, Mt: 23, Lt: 14, Ae: 0). Out of the 40 cancers, 39 were macroscopically diagnosed at early stages on endoscopy. The macroscopic appearance of these 39 cancers was dominantly flat and slightly depressed (0-IIa: 1, 0-IIb: 21, 0-IIc: 17), and 37 were treated via endoscopy (EMR: 1, ESD: 36) (Fig. 3). All cancers except for one were treated successfully (complete resection rate 97.3%) without any adverse event. One was suspected to have severe fibrosis, interrupting endoscopic en-bloc removal, and was subsequently treated via esophagectomy for the en-bloc resection, with severe fibrosis visible in the postoperative histology. One other patient was elderly with poor general condition that only allowed for follow-up endoscopy without any treatment; no progression to cancer was detected during the observation period of this study. The one case not detected at an early stage was a type 2 advanced cancer detected as a metachronal cancer during closed surveillance endoscopy (interval 6 months). This advanced cancer was treated with neoadjuvant therapy, followed by esophagectomy.
Representative case of early esophageal cancer in achalasia. a High-resolution manometry showing type II achalasia. b An esophagogram revealed a dilated esophagus with remnant barium. c A reddish flat lesion (yellow triangles) is observed within the dilated middle thoracic esophagus. The biopsy revealed SCC. d Narrow band imaging showing a brownish area with a clear demarcation line. e Chromoendoscopy with iodine staining showing early esophageal cancer. f ESD was performed, and early esophageal cancer was successfully removed. SCC squamous cell carcinoma, ESD endoscopic submucosal dissection
All cancers, except for one, were treated curatively by endoscopy or surgery, and all patients, including the patient without treatment due to a poor general condition, remained alive during the study period. However, the untreated patient with submucosal invasion in histology died 5 months later due to cancer metastasis.
All 40 esophageal cancers were histologically investigated (using the en-bloc specimen 39, biopsy 1), and all were classified as SCC (one with basaloid component). Among the 2,714 patients with achalasia and achalasia-related EMDs, Barret esophagus was seen in only one patient, which was classified as SSBE (supplemental file 1). Esophageal adenocarcinoma was not present in our cohort.
Discussion
In this study, we investigated 2,714 Japanese patients with achalasia and achalasia-related EMDs for the recent 10-year period using practical medical records. This is the largest study among the cancer survey studies using medical records, although equivalent scale studies using health care databases, which are unable to provide information on histological type and treatment course, are present.
In Japan, the incidence of esophageal cancer in 2016 was reported at 0.0347 per person-year in men, and 0.0068 in women [26]. Compared to the incidence data on the general population, the incidence in patients with achalasia and achalasia-related EMDs was found to be much higher in this study (men 16.7 fold, women 8.8 fold; calculated based on the number diagnosed with achalasia and achalasia-related EMDs), meaning that achalasia and achalasia-related EMDs remain a risk factor for esophageal cancer, despite recent advancements in EMD diagnosis and treatment. However, the incidence in this current study was lower than that in a previous US study, which was similarly based on practical medical records [27] (Table 4). Several explanations may be considered: (1) the observation period from the diagnosis of achalasia and achalasia-related EMDs was shorter than that of the US study; and (2) our study was conducted with a more recent observation period, and the diagnostic skills and treatment of achalasia have improved over time owing to development and spread of HRM, endoscopic treatments like POEM, and improved awareness of the disorder. This may have possibly reduced the risk of esophageal cancer in patients with achalasia and achalasia-related EMDs. Reports based on practical medical records, including our study, had a higher incidence of esophageal cancer [27] than those using databases for healthcare purposes [8, 28], which may underestimate the incidence due to several limitations, such as a decreased database quality, since medical record data is extracted to produce healthcare databases.
Risk factors for esophageal cancer in patients with achalasia were also independently investigated in this study. Similar to findings in the general population [29], this study also found a higher risk of esophageal cancer in men than in women. Frequent alcohol consumption and smoking are known risk factors for esophageal cancer. However, the long time to carcinogenesis, and the low absolute incidence rate of esophageal cancer in our study might have led to the discrepancies in statistical significance seen. Long disease duration and aging both increase the incidence of esophageal cancer, but the influence of these two factors, which can be clarified by comparing the incidence data of esophageal cancer with and without achalasia in the same population, could not be stratified in this study. Our follow-up study will attempt to investigate the individual effects of the two factors. Although sigmoid and advanced sigmoid type on esophagography had more esophageal cancers, we also need to pay attention to straight type achalasia.
In this study, the histological classification of esophageal cancer for all cases was SCC, with no adenocarcinomas detected. In Western studies, the incidence of adenocarcinoma from LSBE and SSBE were estimated at 0.33–0.56%, and 0.19%, respectively [30, 31], with the incidence of esophageal adenocarcinoma and SCC being almost equal. [32] Notably, regarding the background of achalasia studies in Caucasian populations, Barret esophagus and subsequent adenocarcinoma were more common, and are particularly related to post-treatment reflux [33]. In Japan, the prevalence of SSBE is reported at 10–43%, which is relatively higher than in Western studies [34, 35]; LSBE prevalence is extremely low (< 1.0% of all Barrett esophagus patients). Furthermore, the incidence of adenocarcinoma may be influenced by race or ethnicity. In East Asia, the reported rate of SCC is nine times greater than adenocarcinoma [32]. Likewise, in Asians with achalasia, the incidence of adenocarcinoma appears to be much less and may account for the identification of only SCC in our cohort.
Based on the lower incidence of esophageal cancer in our study compared with a previous Western study [27], routine endoscopic surveillance for esophageal cancer may not be recommended for Japanese patients with achalasia. We also found that patients with achalasia-related esophageal cancer had common clinical characteristics to those in the overall esophageal cancer population, such as older age, male sex dominance, and a history of alcohol consumption [36]. Based on this study’s result, we may recommend surveillance endoscopy for the following high-risk patients with achalasia: male, > 40 years of age, long history of achalasia over 30 years, and a history of frequent alcohol intake. Finally, due to the ever-evolving nature of medical technology and better disease understanding, earlier diagnosis and subsequent treatment may be conducted for patients with achalasia, with subsequent improvements in longevity. This further necessitates proper cancer surveillance in high-risk patients.
To our knowledge, this is the first study to widely review the characteristics of esophageal cancer in achalasia other than using histological classification, including its treatment course and paying particular attention to endoscopic treatment. Achalasia-related SCC was located predominantly in the thoracic area, was macroscopically 0-IIb and 0-IIc dominant, and reflected common characteristics of esophageal SCC [37]. In this study, macroscopical early cancer was successfully removed endoscopically in patients with achalasia despite the duration of symptoms of achalasia exceeding up to 49 years. Our results indicate that achalasia-related early esophageal cancer is amenable to endoscopic treatment such as EMR/ESD. It must be noted though, that after endoscopic treatment, the risk of metachronal esophageal cancer may be higher, since achalasia triggers mucosal inflammation in all areas of the esophagus, promoting carcinogenesis. This study was performed by high-volume EMD centers, and all the clinicians involved were all endoscopic experts, which may have affected the high early esophageal cancer rate and high complete resection rate.
Our study had several limitations. First, this was a retrospective study; therefore, the interval of surveillance endoscopy was not fixed between the cases. Second, the follow-up period after the treatment for achalasia was not sufficient to estimate how much and which interventions decreased the risk of esophageal cancer in patients with achalasia. Besides, achalasia itself is not a malignant disorder, which made it difficult to perform long-term follow up. Third, HRM diagnosis and pathological diagnosis were performed by different expert clinicians and pathologists in each hospital, which may have resulted in some inter-hospital discrepancy regarding the diagnosis. Fourth, the number of esophageal cancers detected in this study was too small to conduct a multivariate analysis of risk factors. Finally, the patient’s recollection of the time of achalasia onset might not have been entirely accurate, and any potential misrepresentations might have affected our findings and interpretations.
In conclusion, the relative risk of esophageal SCC is higher in Japanese patients with achalasia, although the absolute risk remains relatively low. Cancer surveillance is recommended in a limited subset of patients with a high risk of SCC. Barrett esophagus and adenocarcinoma are rare in Japan.
References
Richter JE. Oesophageal motility disorders. Lancet. 2001;358:823–8.
Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. Lancet. 2014;383:83–93.
Francis DL, Katzka DA. Achalasia: update on the disease and its treatment. Gastroenterology. 2010;139:369–74.
Park W, Vaezi MF. Etiology and pathogenesis of achalasia: the current understanding. Am J Gastroenterol. 2005;100:1404–14.
Sato H, Takahashi K, Mizuno KI, et al. Esophageal motility disorders: new perspectives from high-resolution manometry and histopathology. J Gastroenterol. 2018;53:484–93.
Duffield JA, Hamer PW, Heddle R, et al. Incidence of achalasia in South Australia based on esophageal manometry findings. Clin Gastroenterol Hepatol. 2017;15:360–5.
Samo S, Carlson DA, Gregory DL, et al. Incidence and prevalence of achalasia in central Chicago, 2004–2014, since the widespread use of high-resolution manometry. Clin Gastroenterol Hepatol. 2017;15:366–73.
Harvey PR, Thomas T, Chandan JS, et al. Incidence, morbidity and mortality of patients with achalasia in England: findings from a study of nationwide hospital and primary care data. Gut. 2019;68:790–5.
van Hoeij FB, Ponds FA, Smout AJ, et al. (2018) Incidence and costs of achalasia in The Netherlands. Neurogastroenterol Motil 30.
Kim E, Lee H, Jung HK, et al. Achalasia in Korea: an epidemiologic study using a national healthcare database. J Korean Med Sci. 2014;29:576–80.
Booy JD, Takata J, Tomlinson G, et al. The prevalence of autoimmune disease in patients with esophageal achalasia. Dis Esophagus. 2012;25:209–13.
Sato H, Yokomichi H, Takahashi K, et al. Epidemiological analysis of achalasia in Japan using a large-scale claims database. J Gastroenterol. 2019;54:621–7.
Torres-Aguilera M, Remes Troche JM. Achalasia and esophageal cancer: risks and links. Clin Exp Gastroenterol. 2018;11:309–16.
Tustumi F, Bernardo WM, da Rocha JRM, et al. Esophageal achalasia: a risk factor for carcinoma. A systematic review and meta-analysis. Dis Esophagus. 2017;30:1–8.
Vaezi MF, Pandolfino JE, Vela MF. ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol. 2013;108:1238–49.
Hirota WK, Zuckerman MJ, Adler DG, et al. ASGE guideline: the role of endoscopy in the surveillance of premalignant conditions of the upper GI tract. Gastrointest Endosc. 2006;63:570–80.
Vaezi MF, Pandolfino JE, Yadlapati RH, et al. ACG clinical guidelines: diagnosis and management of achalasia. Am J Gastroenterol. 2020;115:1393–411.
Oude Nijhuis RAB, Zaninotto G, Roman S, et al. European guidelines on achalasia: United European Gastroenterology and European Society of Neurogastroenterology and motility recommendations. United Eur Gastroenterol J. 2020;8:13–33.
Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27(2):160–74.
Inoue H, Sato H, Ikeda H, et al. Per-oral endoscopic myotomy: a series of 500 patients. J Am Coll Surg. 2015;221:256–64.
Spechler SJ, Souza RF. Barrett’s esophagus. N Engl J Med. 2014;371:836–45.
The Japan Esophageal Society. Guidelines for the clinical and pathologic studies on carcinoma of the esophagus. 11th ed. Kanehara Co. Tokyo, Japan.
Japan ES. Japanese classification of esophageal cancer, 11th edition: part I. Esophagus. 2017;14:1–36.
Rice TW, Patil DT, Blackstone EH. 8th edition AJCC/UICC staging of cancers of the esophagus and esophagogastric junction: application to clinical practice. Ann Cardiothorac Surg. 2017;6:119–30.
Board WCoTE. WHO classification of tumours, 5th ed., Vol.1. 2019.
Statistics Bureau, Ministry of internal affairs and communications website (https://www.stat.go.jp/english/index.html).
Leeuwenburgh I, Scholten P, Alderliesten J, et al. Long-term esophageal cancer risk in patients with primary achalasia: a prospective study. Am J Gastroenterol. 2010;105:2144–9.
Zendehdel K, Nyren O, Edberg A, et al. Risk of esophageal adenocarcinoma in achalasia patients, a retrospective cohort study in Sweden. Am J Gastroenterol. 2011;106:57–61.
Ohashi S, Miyamoto S, Kikuchi O, et al. Recent advances from basic and clinical studies of esophageal squamous cell carcinoma. Gastroenterology. 2015;149:1700–15.
Sikkema M, de Jonge PJ, Steyerberg EW, et al. Risk of esophageal adenocarcinoma and mortality in patients with Barrett’s esophagus: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2010;8:235–44.
Desai TK, Krishnan K, Samala N, et al. The incidence of oesophageal adenocarcinoma in non-dysplastic Barrett’s oesophagus: a meta-analysis. Gut. 2012;61:970–6.
Hongo M, Nagasaki Y, Shoji T. Epidemiology of esophageal cancer: orient to occident. Effects of chronology, geography and ethnicity. J Gastroenterol Hepatol. 2009;24:729–35.
Ichkhanian Y, Benias P, Khashab MA. Case of early Barrett cancer following peroral endoscopic myotomy. Gut. 2019;68:2107–10.
Amano Y, Ishimura N, Furuta K, et al. Which landmark results in a more consistent diagnosis of Barrett’s esophagus, the gastric folds or the palisade vessels? Gastrointest Endosc. 2006;64:206–11.
Amano Y, Kinoshita Y. Barrett esophagus: perspectives on its diagnosis and management in asian populations. Gastroenterol Hepatol. 2008;4:45–53.
Lordick F, Mariette C, Haustermans K, et al. Oesophageal cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2016;27:v50–7.
Tachimori Y, Ozawa S, Numasaki H, et al. Comprehensive registry of esophageal cancer in Japan, 2012. Esophagus. 2019;16:221–45.
Ponds FA, Moonen A, Smout A, et al. Screening for dysplasia with Lugol chromoendoscopy in longstanding idiopathic achalasia. Am J Gastroenterol. 2018;113:855–62.
Markar SR, Wiggins T, MacKenzie H, et al. (2019) Incidence and risk factors for esophageal cancer following achalasia treatment: national population-based case-control study. Dis Esophagus 32.
Acknowledgements
We would like to thank Editage [http://www.editage.com] for editing and reviewing this manuscript for the English language.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Ethical approval
Hiroki Sato accepts official responsibility for the overall conduct of this study and the publication of this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sato, H., Terai, S., Shimamura, Y. et al. Achalasia and esophageal cancer: a large database analysis in Japan. J Gastroenterol 56, 360–370 (2021). https://doi.org/10.1007/s00535-021-01763-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-021-01763-6