Abstract
Background
Not only obesity but also sarcopenia is associated with NAFLD. The influence of altered body composition on the pathophysiology of NAFLD has not been fully elucidated. The aim of this study is to determine whether skeletal muscle mass to visceral fat area ratio (SV ratio) affects NAFLD pathophysiology.
Methods
A total of 472 subjects were enrolled. The association between SV ratio and NAFLD pathophysiological factors was assessed in a cross-sectional nature by stratification analysis.
Results
When the SV ratio was stratified by quartiles (Q 1–Q 4), the SV ratio showed a negative relationship with the degree of body mass index, HOMA-IR, and liver stiffness (Q 1, 8.9 ± 7.5 kPa, mean ± standard deviation; Q 2, 7.5 ± 6.2; Q 3, 5.8 ± 3.7; Q 4, 5.0 ± 1.9) and steatosis (Q 1, 282 ± 57 dB/m; Q 2, 278 ± 58; Q 3, 253 ± 57; Q 4, 200 ± 42) measured by transient elastography. Levels of leptin and biochemical markers of liver cell damage, liver fibrosis, inflammation and oxidative stress, and hepatocyte apoptosis were significantly higher in subjects in Q 1 than in those in Q 2, Q 3, or Q 4. Moreover, fat contents in femoral muscles were significantly higher in subjects in Q 1 and the change was associated with weakened muscle strength. In logistic regression analysis, NAFLD subjects with the decreased SV ratio were likely to have an increased risk of moderate-to-severe steatosis and that of advanced fibrosis.
Conclusions
Decreased muscle mass coupled with increased visceral fat mass is closely associated with an increased risk for exacerbating NAFLD pathophysiology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In Japan, national obesity trends have been adversely affected by Westernized dietary habits and chronic physical inactivity. The prevalence of obesity among the adult population is about 30%, and has increased by about 1.5-fold over the last 30 years among men [1]. Consequently, the incidences of lifestyle disease-associated conditions such as hypertension, high cholesterol, and impaired glucose tolerance are steadily increasing [2]. In particular, the occurrence of abnormal hepatic function is especially high, with the underlying cause possibly being an increase in the prevalence of non-alcoholic fatty liver disease (NAFLD) [2]. NAFLD is a chronic disease characterized by the accumulation of fat deposits in the liver and is considered to be the hepatic phenotype of metabolic syndrome [3].
Concerning the etiology of NAFLD, there have been complex cross-talks of diverse disturbing factors related to the pathological linkage between the liver and other organs, as proposed in the “multiple parallel hit hypothesis” [4]. That is, a principal role seems to be played by insulin resistance induced by the increased production of pro-inflammatory substances such as adipokines secreted from expanded visceral fat tissues in obese conditions and endotoxins, enterobacteria-related molecules. In addition to insulin resistance, various other factors such as oxidative stress, dietary factors, and genetic factors, etc., act on the liver in parallel and are thus involved in the pathogenesis of NAFLD. Because insulin resistance is frequently seen in patients with NAFLD even at an early stage of the disease, it has been considered as an important factor associated with the onset of NAFLD. Insulin resistance is induced by the combination of hepatic disorders with disorders of other organs or tissues, e.g., visceral fat and skeletal muscles. These organs or tissues play a central role in glucose and lipid metabolism. Abnormal body composition arising from obesity-related increase in visceral fat and reduced skeletal muscle mass, known as ‘sarcopenia’, aggravates insulin resistance, and thus it seems to be closely related to the onset and progression of NAFLD mediated by the abnormal metabolism of glucose and lipids.
It was recently reported that abnormal body composition, e.g., obesity and reduced skeletal muscles, is a factor affecting the pathophysiology of chronic liver disease [5]. The association of reduced skeletal muscles with the survival prognosis of patients with chronic liver disease has also been reported [6]. That is, reduction in exercise tolerability arising from reduced skeletal muscles affects the prognosis of chronic liver disease (liver cirrhosis) [6]. Reduced skeletal muscles serve as an independent prognostic factor for hepatocellular carcinoma [7, 8]. This also increases the risk for the onset of NAFLD [9,10,11] and the risk for liver fibrosis [11]. On the basis of these findings, changes in the body composition arising from an obesity-related increase in visceral fat and reduction in skeletal muscles (due to muscular protein degradation in the presence of obesity-related chronic inflammation) are estimated to be factors associated with the onset and progression of chronic liver diseases including NAFLD as well as with the survival prognosis of patients with such a condition. Thus, abnormal body composition in patients with chronic liver disease has been increasingly shown to serve as an important factor affecting the pathophysiology and survival prognosis of chronic liver disease.
This study was undertaken to evaluate the influence of abnormal body composition, e.g., reduced skeletal muscle mass and increased visceral fat mass, on the pathophysiology of NAFLD.
Methods
Patients
Between April 2011 and December 2016, 366 subjects (207 men and 159 women) presented at the outpatient department of the University of Tsukuba Hospital. The diagnosis of NAFLD was based on overeating or physical inactivity, elevated serum ALT levels, and the presence of at least two of three abnormal findings using abdominal ultrasonography diffusely increased liver echogenicity (‘bright’) that was greater than that for kidney, vascular blurring, and deep attenuation of the ultrasound signal according to the diagnostic guidelines for NAFLD in the Asia–Pacific region [12]. We excluded patients with alcohol consumption (>20 g/day). Patients with the following conditions were also excluded from this study (a) presence of other causes of liver disease, (b) psychiatric diseases, or (c) taking anti-diabetic agents or weight-loss agents. Of the above subjects, 337 subjects (197 men and 140 women) were diagnosed with NAFLD. In addition, 106 non-obese and normolipidemic participants (48 men and 58 women), who worked for the University Hospital, were enrolled in the study. To evaluate the effects of abnormal body composition on the pathophysiological factors of NAFLD, all study subjects were divided into four groups according to the quartiles into which their skeletal muscle mass to visceral fat area ratio (SV ratio) (g/cm2) belonged [1st quartile (Q 1 lowest group); 2nd quartile (Q 2); 3rd quartile (Q 3); 4th quartile (Q 4 highest group)]. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in prior approval by the Ethics Committee of the University of Tsukuba, School of Medicine. Written informed consent was obtained from each patient.
Anthropometric measurements
Body weight, composition, and abdominal visceral fat area were measured using InBody720 (Biospace Japan Inc., Tokyo, Japan). Standing height was measured by a wall-mounted stadiometer (Muratec-KDS Co., Kyoto, Japan) and used to calculate BMI (kg/m2).
Maximal strength of isometric contraction of knee extension at an angle of 90° in a seated position was measured using a hand-held dynamometer μ-TasF-1 (Anima Co., Tokyo, Japan). Isometric movement was conducted by exerting maximum effort for knee joint extension movement for approximately 5 s. The highest of the two values of knee extension strength was used for each subject. The results were normalized by body weight (kg) and expressed as percentage.
Clinical and laboratory measurements
Blood samples were drawn from the median cubital vein. Biochemical analysis for clinical and laboratory measurements was performed as described previously [13]. Surrogate markers were calculated from the biochemical data for insulin resistance by the homeostasis model assessment (HOMA-IR) [14], for NAFLD fibrosis score (NFS) [15], and for FIB4 index [16].
Ultrasonography
An ultrasound scanner Aplio-400 (Toshiba Co. Ltd., Tokyo) was used to evaluate liver steatosis. The grade of steatosis (G0, normal echogenicity; G1, slight, diffuse increase in fine echoes in liver parenchyma with normal visualization of diaphragm and intrahepatic vessel borders; G2, moderate, diffuse increase in fine echoes with slightly impaired visualization of intrahepatic vessels and diaphragm; G3, marked increase in fine echoes with poor or nonvisualization of the intrahepatic vessel borders, diaphragm, and posterior right lobe of the liver) was determined according to the criteria reported previously [17] by a clinical radiologist. A radiologist was blinded to the treatment allocation of the patients. The films were scored in random order without any clinical information.
Contrast-enhanced ultrasonography
The study of contrast-enhanced ultrasonography (CEUS) was conducted using an ultrasound contrast agent Sonazoid [18] as described previously [19].
Liver stiffness and steatosis
A clinical gastroenterologist assessed the liver stiffness (LS) by transient elastography, using a FibroScan® device (Echosens, Paris, France) with a 3.5-MHz standard probe or 2.5-MHz XL probe. The principle and examination procedures have been previously published [20]. We determined the quantity of hepatic fat accumulation with a controlled attenuation parameter (CAP) designed to measure liver ultrasonic attenuation (go and return path) at 3.5 MHz by using signals acquired by the device. The detailed descriptions of CAP have also been published previously [21].
Proton magnetic resonance spectroscopy
The tissue fat contents in the liver, i.e., intra-hepatic lipids (IHL), and the muscles, i.e., intra-myocellular lipids (IMCL) and extra-myocellular lipids (EMCL) in the bilateral quadriceps, were determined using 1H-MRS. A 3-T MR device Philips Achieva (Philips Electronics Japan, Ltd., Tokyo, Japan) as described previously [22].
Statistical analysis
Statistical analysis was performed using SPSS 23.0 (SPSS Inc., Chicago, IL, USA). Each measurement value was expressed as mean ± standard deviation. Quartile stratification analysis of SV ratio was analyzed for frequency of each disease and diseased conditions using Pearson’s χ 2 test. Each pathophysiological factor of NAFLD among the SV ratio quartile groups was compared using ANCOVA with/without adjustment for age and gender as covariates. The categorical variables were compared using the Chi-squared test. The association of each NAFLD pathophysiological factor with liver stiffness and liver fat content in the subjects were analyzed using univariate and multivariate analyses. Odds ratios (ORs) were obtained from logistic regression analysis, and the results were presented as ORs with a 95% confidence interval (CI). A P value of <0.05 was defined as statistically significant.
Results
Comparison of the prevalence rates of lifestyle-related diseases of study subjects in each quartile of skeletal muscle mass to visceral fat area ratio
As shown in Table 1, comparisons between Q 1, Q 2, Q 3, and Q 4 showed that when compared to the other three quartiles, Q 1 had higher prevalence rates of moderate and severe obesity, i.e., body mass index (BMI) ≥30, and each of the lifestyle-related diseases, including NAFLD, diabetes, and dyslipidemia, and hypertension. The mean age of the subjects in Q 1 was significantly greater than that of the subjects in Q 2, Q 3, or Q 4.
Comparison of anthropometric characteristics of study subjects in each quartile of skeletal muscle mass to visceral fat area ratio
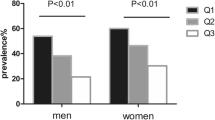
As shown in Table 1, the mean age and gender composition were significantly different between the SV ratio quartiles. Body weight and BMI in Q 1 were significantly higher than those in Q 2, Q 3, or Q 4. The proportions of subjects with moderate-to-severe obesity were 41.5% in Q 1, 26.3% in Q 2, 11.9% in Q 3, and 1.7% in Q 4, which were strongly negatively correlated with SV ratio in the respective quartiles (Fig. 1). Skeletal muscle mass and fat-free mass were significantly lower in Q 1 than in Q 4, while fat mass and visceral fat area were significantly higher in Q 1 than in Q 2, Q 3, or Q 4.
The comparisons of NAFLD pathophysiological factors and hepatic conditions such as BMI, HOMA-IR, ultrasonographic steatosis grade, CAP, LS, and Kupffer phase signal intensity in CEUS in study subjects, with quartile stratification according to the SV ratio. NAFLD non-alcoholic fatty liver disease, BMI body mass index, HOMA-IR homeostasis model assessment-insulin resistance, CAP controlled attenuation parameter, LS liver stiffness, CEUS contrast-enhanced ultrasonography, SV ratio skeletal muscle mass to visceral fat area ratio
Comparison of NAFLD-related hepatic conditions of study subjects in each quartile of skeletal muscle mass to visceral fat area ratio
As shown in Table 1, the comparison of hepatic conditions among the SV ratio quartiles showed that the CAP measurements by using a FibroScan device, which reflects the degree of hepatic fat accumulation, was significantly higher in Q 1 than in Q 3 or Q 4. Similar to the results seen with CAP, Q 1 had significantly higher IHL measurements by using MRS than Q 4. The LS measurements by using a FibroScan device, which reflects the degree of liver fibrosis and/or inflammation, was significantly higher in Q 1 than in Q 3 or Q 4. In addition, the Kupffer phase signal intensity in CEUS, which reflects Kupffer cell phagocytosis function of foreign bodies, were significantly lower in Q 1 than in Q 2, Q 3, or Q 4.
As shown in Fig. 1, a more detailed analysis of moderate-to-severe fat accumulation in the liver revealed the proportions of subjects with ultrasonographic evidence of steatosis grade 2 or 3 to be 72.1% in Q 1, 66.9% in Q 2, 55.0% in Q 3, and 17.8% in Q 4. In addition, the proportions of subjects with CAP measurements ≥260 dB/m were 66.7% in Q 1, 63.1% in Q 2, 46.1% in Q 3 and 12.9% in Q 4. A more detailed analysis of advanced liver fibrosis revealed the proportions of subjects with LS measurements ≥12 kPa were 20.3% in Q 1, 12.7% in Q 2, 5.1% in Q 3, and 1.7% in Q 4. The proportions of subjects with a severe decrease in the Kupffer phase signal intensity (<100 intensity) were 35.5% in Q 1, 22.7% in Q 2, 10.8% in Q 3, and 6.5% in Q 4 (Fig. 1). Each of these indicators of hepatic conditions worsened with a decrease in the SV ratio.
Comparison of skeletal muscle-related characteristics of study subjects in each quartile of skeletal muscle mass to visceral fat area ratio
As shown in Fig. 2, the analysis of the skeletal muscles of subjects in each of the SVR quartiles revealed grip strength to be 25.9 kg in Q 1, 31.0 kg in Q 2, 35.4 kg in Q 3, and 35.6 kg in Q 4. Knee extension muscle strength (normalized by body weight) was 44.5% in Q 1, 52.3% in Q 2, 60.8% in Q 3, and 66.5% in Q 4. Levels of intra-myocellular lipids (IMCL) were 5.83 mmol/body weight (kg) in Q 1, 4.89 mmol/kg in Q 2, 4.26 mmol/kg in Q 3, and 3.63 mmol/kg in Q 4. Levels of extra-myocellular lipids (EMCL) were 20.0 mmol/kg in Q 1, 14.1 mmol/kg in Q 2, 9.28 mmol/kg in Q 3, and 4.68 mmol/kg in Q 4. These results clearly indicated that a decrease in physical capacity and increases in levels of IMCL and EMCL occurred with a decrease in the SV ratio.
Comparisons of the skeletal muscle strength, grasping and isometric contraction of knee extension, and the skeletal fat accumulation, IMCL and EMCL in study subjects, with quartile stratification according to the SV ratio. IMCL intra-myocellular lipids, EMCL extra-myocellular lipids, SV ratio skeletal muscle mass to visceral fat area ratio. *P < 0.05, **P < 0.01; significantly different between the SV ratio quartiles
Comparison of insulin resistance status of study subjects in each quartile of skeletal muscle mass to visceral fat area ratio
As shown in Table 1, fasting plasma glucose (FPG), fasting insulin, homeostasis model assessment of insulin resistance (HOMA-IR), and hemoglobin A1c (HbA1c) levels were significantly higher in Q 1 than in Q 2, Q 3, or Q 4 and were associated with a higher rate of diabetes prevalence in Q 1. The proportions of subjects with insulin resistance (HOMA-IR ≥2.5) were 66.4% in Q 1, 42.5% in Q 2, 42.2% in Q 3, and 7.6% in Q 4, which were strongly negatively correlated with SV ratio in the respective quartiles (Fig. 1).
Comparison of biochemical characteristics of study subjects in each quartile of skeletal muscle mass to visceral fat area ratio
As shown in Table 1, the comparison of hepatic function parameters among the SV ratio quartiles showed that levels of aspartate aminotransferase (AST) and alanine aminotransferase (ALT), which are indicators of hepatocyte injury, were significantly higher in Q 1 than in Q 3 or Q 4. The comparison also showed that levels of gamma-glutamyltransferase (γ-GT) were significantly higher in Q 1 than in Q 4.
Levels of glycosylated Wisteria floribunda agglutinin-positive Mac-2 binding protein (WFA+-M2BP), which is a novel marker of liver fibrosis, were significantly higher in Q 1 than in Q 3 or Q 4. Levels of hyaluronic acid and type IV collagen, which are conventional markers of liver fibrosis, did not differ between the SV ratio quartiles. An analysis using the formula to predict liver fibrosis revealed that Q 1 had a significantly higher NAFLD fibrosis score than Q 2, Q 3, or Q 4, with the mean score above the low cutoff value of −1.455. There were no differences in the fibrosis-4 (FIB-4) index observed between the SV ratio quartiles. These results were consistent with a higher LS measurement and a decrease in the phagocytic function of Kupffer cells in Q 1, suggesting that subjects in Q 1 had hepatic conditions associated with progressive liver fibrosis.
As shown in Fig. 3, the comparison of inflammatory, oxidative stress, and apoptosis markers between the study subjects in each of the SV ratio quartiles showed that the levels of both high-sensitivity C-reactive protein (hs-CRP), which is an inflammatory marker, and 2-thiobarbituric acid reactive substances (TBARS), which is an oxidative stress marker, were significantly higher in Q 1 than in Q 3 or Q 4. In addition, levels of M30, which is a marker of hepatocyte apoptosis, were also higher in Q 1 than in Q 3 or Q 4. Moreover, Q 1 had significantly higher levels of LPS than Q 3, or Q 4. However, the levels of ferritin were not different between the SV ratio quartiles. These results indicated that Q 1 had hepatic conditions associated with aggravated inflammatory and oxidative stress pathophysiology, which are associated with increased hepatocyte apoptosis.
The comparisons of serum levels of inflammation, oxidative stress, and apoptosis markers, FFAs, and LPS in study subjects, with quartile stratification according to the SV ratio. hs-CRP high-sensitivity C-reactive protein, TBARS 2-thiobarbituric acid reactive substances, FFA free fatty acid, LPS lipopolysaccharide, SV ratio skeletal muscle mass to visceral fat area ratio. The comparisons between the SV ratio quartiles were made using an ANCOVA with adjustment for age and gender as covariates. *P < 0.05, **P < 0.01; significantly different between the quartiles
As shown in Fig. 4, the comparison of cytokines between the SV ratio quartiles showed that Q 1 had significantly higher levels of both leptin and interleukin-6 (IL-6) than Q 2, Q 3, or Q 4, while TNF-α levels were not different between the SV ratio quartiles. Leptin and IL-6 are inflammatory adipokines. On the other hand, Q 1 had a significantly lower level of adiponectin, which is an anti-inflammatory adipokine, than Q 3 or Q 4. For hepatokines, Q 1 had significantly higher levels of fetuin-A and fibroblast growth factor 21 (FGF21) than Q 4. However, the levels of Sep were not different between the SV ratio quartiles. For a myokine, Q 1 had significantly higher levels of myostatin (MSTN) than Q 2, Q 3, or Q 4. These results indicated a notably imbalanced production of adipokines, hepatokines, and a myokine in Q 1.
The comparisons of serum levels of adipokines, hepatokines, and a myokine in study subjects, with quartile stratification according to the SV ratio. IL-6 interleukin-6, TNF-α tumor necrosis factor-α, Sep selenoprotein-P, FGF21 fibroblast growth factor 21, MSTN myostatin, SV ratio skeletal muscle mass to visceral fat area ratio. The comparisons between the SV ratio quartiles were made using an ANCOVA with adjustment for age and gender as covariates. *P < 0.05, **P < 0.01; significantly different between the quartiles
As shown in Table 1, the comparison of serum lipids between the SV ratio quartiles showed that high-density lipoprotein-cholesterol (HDL-C) levels were significantly lower in Q 1 than in Q 3 or Q 4. On the other hand, the comparison showed that low-density lipoprotein-cholesterol (LDL-C) and triglyceride (TG) were significantly higher in Q 1 than in Q 4. Moreover, the levels of free fatty acids (FFAs) were significantly higher in Q 1 than in Q 4 (Fig. 3).
Analysis of NAFLD pathophysiological factors associated with hepatic steatosis and stiffness
A multiple regression analysis was performed with CAP measurements reflecting the degree of hepatic fat accumulation as dependent variables to determine the NAFLD pathophysiological factors. The SV ratio, amount of body fat, adiponectin, TG, and Kupffer phase signal intensity in CEUS were extracted as independent factors affecting CAP measurements (Table 2). In addition, multiple regression analysis was performed with LS measurements, which reflected the degree of liver fibrosis and/or inflammation as dependent variables to determine the NAFLD pathophysiological factors. The SV ratio, amount of body fat, leptin, hyaluronic acid, type IV collagen, and HOMA-IR were extracted as independent factors affecting LS measurements (Table 2). These results clearly indicated that SV ratio was an important factor affecting both fat accumulation and fibrosis in the liver.
Analysis of fat accumulation risk in study subjects in each quartile of skeletal muscle mass to visceral fat area ratio
After all the study subjects with NAFLD were divided into 4 quartiles based on their SV ratio, a logistic regression analysis was performed in order to estimate the relative risk of moderate-to-severe fat accumulation in the liver (CAP measurements ≥260 dB/m) in subjects in each quartile (Q 1–Q 4) (Table 3). As a result, with the risk of moderate-to-severe fat accumulation in the liver of subjects in Q 4 (highest SV ratio group) being 1, the relative risks were 1.37 in Q 3, 1.81 in Q 2, and 1.89 in Q 1. The results of analyses adjusted for cofounders were similar. These results indicated that a decreased SV ratio was a risk factor for moderate-to-severe fat accumulation in the liver.
Analysis of risk of advanced fibrosis in study subjects in each SV ratio quartile
After all study subjects with NAFLD were divided appropriately into the SV ratio quartiles, logistic regression analysis was performed in order to estimate the relative risk of advanced liver fibrosis (LS measurements ≥12 kPa) (Table 3). As a result, with the risk of liver fibrosis in Q 4 (highest SV ratio group) being 1, the relative risks were 1.00 in Q 3, 2.18 in Q 2, and 3.64 in Q 1. The results of analyses adjusted for cofounders were similar. These results indicated that a decreased SV ratio was a risk factor for advanced fibrosis in the liver.
Discussion
The results of this study are summarized as follows (1) The percentage of cases with moderate-to-severe obesity, insulin resistance, and moderate-to-severe fatty liver were higher in Q 1 of SV ratio than in Q 2, Q 3, and Q 4; (2) The percentage of cases with advanced liver fibrosis; (3) The accumulation of IMCL and EMCL in the bilateral quadriceps was more intense in Q 1 of SV ratio than in the other quartiles, accompanied by a reduction of grip and knee extensor muscle strength; and (4) The analysis of factors associated with the pathophysiology of NAFLD revealed a higher percentage of cases with aggravation of hepatic dysfunction, insulin resistance, inflammatory or oxidative stress, adipokine imbalance, liver fibrosis, and liver cell apoptosis, and cases with reduction of the phagocytic activity of Kupffer cells in Q 1 of SV ratio than in the other quartiles.
Multiple regression analysis revealed SV ratio, body fat mass, triglyceride, adiponectin, and Kupffer phase signal intensity in CEUS (Table 2) as independent factors affecting CAP values that reflect hepatic fat accumulation associated with NAFLD. Furthermore, SV ratio, body fat mass, HOMA-IR, leptin, hyaluronic acid, and type IV collagen were identified as independent factors affecting LS measurements that reflect hepatic inflammation and/or fibrosis associated with NAFLD (Table 2). These findings suggest that reduction in SV ratio is a factor directly associated with the aggravation of hepatic conditions such as fat accumulation and inflammation and/or fibrosis. The pathogenesis of NAFLD is therefore considered to involve not only primary abnormalities of the liver but also abnormalities of other organs or tissues such as skeletal muscles and visceral fat tissues.
In the regression analysis of the data from the entire NAFLD population studied (n = 337), the risk for moderate-to-severe steatosis (CAP ≥260 dB/m) was 1.89 times (unadjusted) higher for Q 1 of SV ratio than for Q 4 (Table 3). The risk for advanced fibrosis (LS ≥12 kPa) was 3.64 times (unadjusted) higher for Q 1 of SV ratio than for Q 4 (Table 3). Such differences in the risk for Q 1 of SV ratio remained even after correction for potential confounding factors. Furthermore, in the analysis of the clinical course of 48 patients with NAFLD, the LS after the survey period for 2–5 years was 134% higher than the pre-survey level in Q 1 of SV ratio, in contrast to the course seen in Q 2 and Q 3 (data not shown). In Q 1 of SV ratio, the pathophysiological factors associated with the progression of NAFLD-related liver fibrosis tended to aggravate, suggesting a more rapid progression of NAFLD-related liver fibrosis. It is estimated that reduction in SV ratio serves not only as a risk factor for the onset of NAFLD but also as a factor associated with the progression of such liver fibrosis.
The findings obtained in this study are consistent with those of previous reports showing that obesity is a factor associated with the aggravation of chronic liver disease [5]; reduction in skeletal muscles is a factor associated with the onset, progression, and survival prognosis of chronic liver disease [6,7,8,9,10,11]; and the magnitude of skeletal muscle reduction is a factor affecting the postsurgical outcome of patients undergoing liver transplantation [23].
Multiple definitions of sarcopenia have been proposed, each with advantages and disadvantages. The prevalence of sarcopenia varies widely, even within the same group of patients, depending on the definition adopted [24]. In overweight or obese subjects, decreased skeletal muscle mass, which may have some synergic effects on increased visceral fat, plays a critical role in the onset and progression of NAFLD. Relative ratio to body composition, not absolute amount of skeletal muscle mass, may be more important to the pathophysiology of NAFLD. It is likely that fat mass should be considered in evaluating sarcopenia in these subjects as reported previously [25].
Q 1 of SV ratio in this study was suggested to reflect a condition resembling sarcopenic obesity. An issue of combined skeletal muscle reduction and visceral fat increase is now discussed here. Evaluation of skeletal muscles solely based on muscle mass involves the problem of possibly overlooking muscle fiber decrease, increased fat accumulation, and other factors. In this study, measurement of muscle mass was combined with measurement of muscle strength and MRS measurement of muscle fat levels. Analysis of these results revealed the reduction of not only muscle mass but also muscle strength, as well as an increase in fat accumulation in muscles in Q 1 of SV ratio. In other words, it seems that Q 1 of SV ratio had reduced muscle fiber volume, resulting in contractility reduction, and qualitative deterioration due to increased fat accumulation inside and outside muscle cells and other factors. Furthermore, the severity of both intra-myocellular and extra-myocellular fat accumulation, measured with MRS (Fig. 2), correlated with the severity of liver steatosis (data not shown), suggesting that Q 1 of SV ratio represents a pathological condition characterized by stimulation of ectopic fat accumulation.
It has been suggested that insulin resistance, inflammation, and leptin resistance play important roles in the background of qualitative deterioration of muscles associated with sarcopenic obesity. Moreover, in this study, aggravation of these pathogenic factors was observed in Q 1 of SV ratio (Table 1). Insulin resistance stimulates glycogenesis and accelerates muscular protein degradation and is also associated with a reduction of leg muscle and grip strength [26]. Sarcopenic obesity involves inflammation. The inflammatory cytokines produced by adipocytes act on skeletal muscles, possibly reducing muscle mass and strength. A negative correlation has been shown between blood inflammatory cytokine level and skeletal muscle mass [27]. Particularly concerning IL-6 and its soluble IL-6 receptor, high levels have been reported in patients with sarcopenic obesity [28]. An increase of IL-6 reduces muscle strength and the capability for movement of elderly persons, accompanied by the inhibition of muscle anabolic activity of insulin-like growth factor-1, leading to the stimulation of muscle protein degradation and aggravation of insulin resistance.
Serum leptin levels have been reported to be higher in patients with sarcopenic obesity than in those with sarcopenia or visceral fat accumulation [29]. Leptin resistance is considered to underlie such hyperleptinemia [29]. Leptin is known to stimulate fat degradation in skeletal muscles while improving insulin sensitivity [30]. Leptin resistance in patients with sarcopenic obesity leads, through a shortage of leptin activity, to reduction in muscle mass, and is considered to stimulate fat accumulation in muscles through the reduction of fatty acid oxidation in muscles mediated by the AMPK pathway. In both men and women, serum leptin levels have been reported to have a negative correlation with the cross-sectional area of femoral muscles [29]. Leptin resistance is considered an important condition for sarcopenic obesity. The results of the analysis in this study suggest that a body composition change in the SV ratio is associated with changes in adipokines, myokines, and hepatokines. These cytokines may be involved in the induction of insulin resistance [31] as well as in the onset and progression of NAFLD-related hepatic conditions mediated by cross-talks among adipocytes, myocytes, and hepatocytes.
In Q 1 of SV ratio, high levels of liver stiffness, liver fibrosis markers in blood (WFA+-M2BP), and predicted fibrosis levels (NAFLD fibrosis score and Fib4 index) are all considered to predict the progression of liver fibrosis. Furthermore, as the elevation of M30, i.e., a metabolite of soluble cytokeratin (CK-18), in blood [32] and elevation of both CK-18 and FGF21 [33] are known to be useful biomarkers in the diagnosis of NASH, it can be estimated that Q 1 of SV ratio includes many cases with NASH.
Although the association between sarcopenia and liver fibrosis was reported in a previous study [11], the background has not been clarified sufficiently. In this study, Q 1 of SV ratio often had hyperleptinemia, as mentioned above, and aggravation of leptin resistance has been considered to underlie such cases [30]. For many years, it has been shown that leptin acts as a factor that stimulates liver fibrosis [34]. Hyperleptinemia in Q 1 of SV ratio seems to play an important role in the formation of liver fibrosis. As a molecular mechanism for the stimulation of liver fibrosis by leptin, it has been pointed out that leptin induces the formation of transforming growth factor-β in sinusoidal endothelial cells and Kupffer cells [35].
The results of this study suggest that the Kupffer phase signal intensity in CEUS was significantly lower in Q 1 of SV ratio, and therefore, the phagocytic activity of Kupffer cells is probably low in this quartile. Sonazoid is a contrast agent phagocytosed by Kupffer cells [19, 20] and has been used for the diagnosis of liver function. Contrast-enhanced ultrasonography is a useful means of screening for NASH [18]. Although the bacterial toxins, e.g., lipopolysaccharide (LPS), play an important role in the onset of NASH and the progression of liver fibrosis, the in vivo capability to dispose LPS is also important. In Q 1 of SV ratio, the phagocytic activity of Kupffer cells was low and the liver stiffness had aggravated. This condition probably involves prolonged inflammatory disorders due to the activation of innate immunity, which is induced by the increased levels of LPS (associated with the reduction of the phagocytic activity of Kupffer cells) coupled with the increased levels of leptin, free fatty acids (FFAs), and fetuin-A. LPS is recognized by the Toll-like receptor (TLR) of Kupffer cells and activates the inflammatory signals. Hyperleptinemia increases the sensitivity of the TLR to LPS of Kupffer cells [36]. Furthermore, fetuin-A physically interacts with both FFAs and TLR [37], and it plays a key role in FFA-induced TLR activation and thus in inflammatory reactions. These pathological conditions probably lead to the progression of hepatic conditions associated with NAFLD.
When a retrospective analysis of our previous studies on weight loss intervention through exercise in middle-aged obese men [13] was conducted, the increase of SV ratio after the exercise intervention compared with the pre-intervention level led to alleviation of hepatic fat accumulation, accompanied by alleviation of hepatic inflammation and fibrosis. On the other hand, among patients receiving diet therapy, a decrease of SV ratio compared with the pre-intervention level was observed after the intervention. When exercise therapy was compared with diet therapy, there was no significant difference in the alleviation of adipokine imbalance; however, exercise therapy induced a decrease of selenoprotein-P (involved in insulin resistance) [38] and an increase of FGF21 (exhibiting anti-obesity activity) in hepatokines [39]. Furthermore, among the myokines, MSTN (involved in muscle atrophy) [40] was reduced by exercise therapy.
In conclusion, a reduction in skeletal muscle mass and an increase of visceral fat mass are considered to increase the risk for the onset of NAFLD and to serve as an important factor involved in the progression of liver fibrosis. In the management of NAFLD, it seems necessary to implement an intervention for preventing the reduction of muscle mass in addition to maintaining skeletal muscle mass as well as to implement nutritional management. An important issue is to promote hepatic rehabilitation, accompanied by measures for alleviating and preventing abnormal body composition through active support by medical teams by using diet and exercise therapies.
Abbreviations
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- BMI:
-
Body mass index
- CAP:
-
Controlled attenuation parameter
- CEUS:
-
Contrast-enhanced ultrasonography
- EMCL:
-
Extra-myocellular lipid
- FFA:
-
Free fatty acid
- FGF21:
-
Fibroblast growth factor 21
- FPG:
-
Fasting plasma glucose
- HDL-C:
-
High-density lipoprotein-cholesterol
- HOMA-IR:
-
Homeostasis model assessment-insulin resistance
- hs-CRP:
-
High-sensitivity C-reactive protein
- IHL:
-
Intrahepatic lipid
- IL-6:
-
Interleukin-6
- IMCL:
-
Intra-myocellular lipid
- LDL-C:
-
Low-density lipoprotein-cholesterol
- LPS:
-
Lipopolysaccharide
- LS:
-
Liver stiffness
- 1H-MRS:
-
Proton magnetic resonance spectroscopy
- MSTN:
-
Myostatin
- NAFLD:
-
Non-alcoholic fatty liver disease
- NASH:
-
Non-alcoholic steatohepatitis
- Sep:
-
Selenoprotein-P
- SV ratio:
-
Skeletal muscle mass to visceral fat area ratio
- TBARS:
-
2-Thiobarbituric acid reactive substances
- TG:
-
Triglyceride
- TNF-α:
-
Tumor necrosis factor-α
- γ-GT:
-
gamma-Glutamyltransferase
- VFA:
-
Visceral fat area
- VLDL:
-
Very low density lipoprotein
- WFA+-M2BP:
-
Wisteria floribunda agglutinin-positive Mac-2 binding protein
References
Eguchi E, Iso H, Tanabe N, et al. Healthy lifestyle behaviours and cardiovascular mortality among Japanese men and women: the Japan collaborative cohort study. Eur Heart J. 2012;33:467–77.
Survey in Japan Society of Ningen doc in 2012 Japan Society of Ningen Doc. http://www.ningen-dock.jp/wp/common/data/other/ release/dock-genkyou_h24.pdf.
Targher G. Non-alcoholic fatty liver disease, the metabolic syndrome and the risk of cardiovascular disease: the plot thickens. Diabet Med. 2007;24:1–6.
Tilg H, Moschen AR. Evolution of inflammation in nonalcoholic fatty liver disease: the multiple parallel hits hypothesis. Hepatology. 2010;52:1836–46.
Berzigotti A, Garcia-Tsao G, Bosch J, the Portal Hypertension Collaborative Group, et al. Obesity is an independent risk factor for clinical decompensation in patients with cirrhosis. Hepatology. 2011;54:555–61.
Alameri HF, Sanai FM, Dukhayll MA, et al. Six-minute walk test to assess functional capacity in chronic liver disease patients. World J Gastoenterol. 2007;13:3996–4001.
Iritani S, Imai K, Takai K, et al. Skeletal muscle depletion is an independent prognostic factor for hepatocellular carcinoma. J Gastoenterol. 2015;50:323–32.
Fujiwara N, Nakagawa H, Kudo Y, et al. Sarcopenia, intramuscular fat deposition, and visceral adiposity independently predict the outcomes of hepatocellular carcinoma. J Hepatol. 2015;63:131–40.
Hong HC, Hwang SY, Choi HY, et al. Relationship between sarcopenia and nonalcoholic fatty liver disease: the Korean sarcopenic obesity study. Hepatology. 2014;59:1772–8.
Lee Y-H, Jung KS, Kim SU, et al. Sarcopaenia is associated with NAFLD independently of obesity and insulin resistance: nationwide surveys (KNHANES 2008–2011). J Hepatol. 2015;63:486–93.
Lee Y-H, Kim SU, Song K, et al. Sarcopenia is associated with significant liver fibrosis independently of obesity and insulin resistance in nonalcoholic fatty liver disease: nationwide surveys (KNHANES 2008–2011). Hepatology. 2016;63:776–86.
Farrell GC, Chitturi S, Lau GK, et al. Guidelines for the assessment and management of non-alcoholic fatty liver disease in the Asia-Pacific region: executive summary. J Gastroenterol Hepatol. 2007;22:775–7.
Sechang Oh, Shida T, Yamagishi K, et al. Moderate to vigorous physical activity volume is an important factor for managing nonalcoholic fatty liver disease: a retrospective study. Hepatology. 2015;61:1205–15.
Matthews DR, Hosker JP, Rudenski AS, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Angulo P, Hui JM, Marchesini G, et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology. 2007;45:846–54.
Vallet-Pichard A, Mallet V, Nalpas B, et al. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection. Comparison with liver biopsy and fibrotest. Hepatology. 2007;46:32–6.
Saadeh S, Younossi ZM, Remer EM, et al. The utility of radiological imaging in nonalcoholic fatty liver disease. Gastroenterology. 2002;123:745–50.
Watanabe R, Matsumura M, Munemasa T, et al. Mechanism of hepatic parenchyma-specific contrast of microbubble-based contrast agent for ultrasonography. Invest Radiol. 2007;42:643–51.
Iijima H, Moriyasu F, Tsuchiya K, et al. Decrease in accumulation of ultrasound contrast microbubbles in non-alcoholic steatohepatitis. Hepatol Res. 2007;37:722–30.
Sandrin L, Fourquet B, Hasquenoph JM, et al. Transient elastography: a new noninvasive method for assessment of hepatic fibrosis. Ultrasound Med Biol. 2003;29:1705–13.
Sasso M, Beaugrand M, de Ledinghen V, et al. Controlled attenuation parameter (CAP): a novel VCTE guided ultrasonic attenuation measurement for the evaluation of hepatic steatosis: preliminary study and validation in a cohort of patients with chronic liver disease from various causes. Ultrasound Med Biol. 2010;36:1825–35.
Oh S, Shida T, Onozuka T, et al. Acceleration training for management of non-alcoholic fatty liver disease: a pilot study. Ther Clin Risk Manag. 2014;10:925–36.
Kaido T, Ogawa K, Fujimoto Y, et al. Impact of sarcopenia on survival in patients undergoing living donor liver transplantation. Am J Transplant. 2013;13:1549–56.
Kim H, Hirano H, Edahiro A, et al. Sarcopenia: prevalence and associated factors based on different suggested definitions in community-dwelling older adults. Geriatr Gerontol Int. 2016;16(supple 1):110–22.
Newman AB, Kupelian V, Visser M, et al. Sarcopenia: alternative definitions and associations with lower extremity function. J Am Geriatr Soc. 2003;51:1602–9.
Abbatecola AM, Ferrucci L, Ceda G, et al. Insulin resistance and muscle strength in older persons. J Gerontol A Biol Sci Med Sci. 2005;60A:1278–82.
Cesari M, Kritchevsky SB, Baumgartner RN, et al. Sarcopenia, obesity, and inflammation—results from the trial of angiotensin converting enzyme inhibition and novel cardiovascular risk factors study. Am J Clin Nutr. 2005;82:428–34.
Schrager ME, Metter EJ, Simonsick E, et al. Sarcopenic obesity and inflammation in the InCHIANTI study. J Appl Physiol. 2007;102:919–25.
Kohara K, OchiM Tabara Y, et al. Leptin in sarcopenic visceral obesity: possible link between adipocytes and myocytes. PLoS One. 2011;6:e24633.
Dyck DJ. Adipokines as regulators of muscle metabolism and insulin sensitivity. Appl Physiol Nutr Metab. 2009;34:396–402.
Sell H, Dietze-Schroeder D, Eckel J. The adipocyte-myocyte axis in insulin resistance. Trends Endocrinol Metab. 2006;17:416–22.
Feldstein AE, Wieckowska A, Lopez AR, et al. Cytokeratin-18 fragment levels as noninvasive biomarkers for nonalcoholic steatohepatitis: a multicenter validation study. Hepatology. 2009;50:1072–8.
She J, Chan HL-Y, Wong GL-H, et al. Non-invasive diagnosis of non-alcoholic steatohepatitis by combined serum biomarkers. J Hepatol. 2012;56:1363–70.
Ikejima K, Honda H, Yoshikawa M, et al. Leptin augments inflammatory and profibrogenic responses in the murine liver induced by hepatotoxic chemicals. Hepatology. 2001;34:288–97.
Ikejima K, Takei Y, Honda H, et al. Leptin receptor-mediated signaling regulates hepatic fibrogenesis and remodeling of extracellular matrix in the rat. Gastroenterology. 2002;122:1399–410.
Imajo K, Fujita K, Yoneda M, et al. Hyperresponsivity to low-dose endotoxin during progression to nonalcoholic steatohepatitis is regulated by leptin-mediated signaling. Cell Metab. 2012;16:44–54.
Pal D, Dasgupta S, Kundu R, et al. Fetuin-A acts an endogenous ligand of TLR4 to promote lipid-induced insulin resistance. Nat Med. 2012;18:1279–85.
Misu H, Takamura T, Takayama H, et al. A liver-derived secretory protein, selenoprotein-P, causes insulin resistance. Cell Meta. 2010;12:483–95.
Kharitonenkov A, Larsen P. FGF21 reloaded: challenges of a rapidly growing field. Trends Endocrinol Metab. 2011;22:81–6.
Yarasheski KE, Bhasin S, Sinha-Hikim I, et al. Serum myostatin-immunoreactive protein is increased in 60–92 year old women and men with muscle wasting. J Nutr Health Aging. 2002;6:343–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Funding
This work was supported by in part by Grants-in-Aids for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology, Japan (Nos. 25282212, 26282191, 26293284, 26293297, 26670109, 15K15037, 15K15488, and 16K15188).
Rights and permissions
About this article
Cite this article
Shida, T., Akiyama, K., Oh, S. et al. Skeletal muscle mass to visceral fat area ratio is an important determinant affecting hepatic conditions of non-alcoholic fatty liver disease. J Gastroenterol 53, 535–547 (2018). https://doi.org/10.1007/s00535-017-1377-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-017-1377-3