Abstract
Background and aims
Interferon and nucleotide/nucleoside analogues are the main treatments for chronic hepatitis B. These drugs effectively reduce serum hepatitis B virus (HBV) DNA titers but fail to sufficiently reduce hepatitis B surface antigen (HBsAg) levels. Following the recent identification of sodium taurocholate cotransporting polypeptide as a receptor for HBV entry, inhibition of HBV entry has become an attractive therapeutic target for chronic hepatitis B treatment. We therefore evaluated the antiviral effects of antibody to HBsAg (anti-HBs) immunoglobulin (HBIG), which can inhibit HBV entry, by in an vivo study and a clinical trial.
Methods
In the in vivo study, HBV-infected mice were generated from human hepatocyte chimeric mice and treated with HBIG. A clinical trial evaluating HBIG therapy in patients was also performed.
Results
In the mouse study, HBV DNA titers were reduced and serum HBsAg titers decreased to undetectable levels following high-dose HBIG injection. On the basis of this result, eight chronic hepatitis B patients, who had received long-term nucleotide analogue treatment, were treated with monthly HBIG injections as an additional treatment. After 1 year of treatment, an HBsAg level reduction of more than 1 log IU/mL was observed in four patients, and three patients became anti-HBs positive. No adverse events occurred during HBIG therapy.
Conclusion
These results suggest that monthly HBIG injection might benefit patients with chronic hepatitis B whose HBsAg titer becomes lower following long-term nucleotide/nucleoside analogue treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatitis B virus (HBV) infection is a serious global health problem. Chronic HBV infection often leads to chronic hepatitis, liver cirrhosis, and hepatocellular carcinoma, and more than 500,000 people die of liver-related diseases each year [1]. To prevent the progression of liver diseases by reducing inflammation, antiviral therapies that use interferon and nucleotide/nucleoside analogues (NAs) have been developed [2–4]. Current antiviral therapies strongly suppress viral replication; however, it is difficult to achieve complete HBV elimination from hepatocytes. The main obstacle to viral clearance is the long-term presence in the nucleus of HBV covalently closed circular DNA (cccDNA), which is a stable minichromosome composed of viral DNA in complex with histone and non-histone host proteins [5–10]. Therefore, antiviral therapies, especially those involving NAs, must be continued for long periods.
Hepatitis B surface antigen (HBsAg) loss is considered a clinical goal of antiviral therapy for prevention of the development of liver cirrhosis and hepatocellular carcinoma in patients with chronic hepatitis B, and accurate HBsAg quantification systems have been developed for monitoring changes in HBsAg levels. To achieve HBsAg loss, several clinical trials using pegylated interferon and NAs have been performed, and some positive results have been reported [11–14]. One clinical trial using adefovir and pegylated interferon alfa-2a has been performed, and a small number of patients (3.3 %) were able to achieve HBsAg seroclearance with this combination therapy [13]. However, the HBsAg seroclearance rate was not sufficient, and it is necessary to improve the treatment of chronic hepatitis B.
Recently, sodium taurocholate cotransporting polypeptide (NTCP) has been identified as the HBV receptor [15] and Myrcludex-B, an HBV entry inhibitor targeting NTCP, has been developed [16]. Myrcludex-B is a synthetic lipopeptide that inactivates NTCP function and inhibits HBV binding [17]. According to in vitro and in vivo studies, a very low dose of Myrcludex-B can inhibit HBV infection [16], and a phase Ib/IIa clinical study has been started [18]. Therefore, we considered that inhibition of HBV entry or attachment of hepatocytes could be a therapeutic target to increase the HBsAg seroclearance rate. Antibody to HBsAg (Anti-HBs) immunoglobulin (HBIG) can bind to HBsAg or to the surface of HBV particles and neutralizes HBsAg or protects hepatocytes from HBV infection [19, 20]. To improve the HBsAg seroclearance or reduction rate, we analyzed the antiviral effects of NA plus HBIG combination therapy. We evaluated antiviral effects of HBIG using the human hepatocyte chimeric mouse model, in which primary human hepatocytes were engrafted into immunocompromised mice [21]. Following the success of the mouse experiment, we performed a clinical trial to evaluate the antiviral effects of NA plus HBIG combination therapy in patients with chronic hepatitis B.
Materials and methods
Generation of HBV-infected human hepatocyte chimeric mice and administration of HBIG
Human hepatocyte chimeric mice (PXB mice, PhoenixBio, Hiroshima, Japan) were generated from uPA+/+/SCID+/+ mice and human hepatocytes were transplanted via spleen artery [21, 22]. Frozen human hepatocytes obtained from the same donor were transplanted into all the mice studied.
To generate HBV-infected mice, mice were inoculated with 50 μL of human serum containing a high titer of HBV DNA (1.2 × 108 copies per milliliter) via the tail vein. Every 2 weeks, mouse serum was collected, and HBV DNA and human albumin levels were evaluated. After HBV DNA levels had plateaued, we administered HBIG (Mitsubishi Pharma Corporation, Osaka, Japan) once. To evaluate the human hepatocyte repopulation rate of the mouse liver, human serum albumin levels in mouse serum were measured as described previously [21, 22].
Inoculation, extraction of mouse sera, and killing of mice were performed with the mice under ether anesthesia. The experimental protocol was approved by the Ethics Review Committee for Animal Experimentation of Graduate School of Biomedical Sciences, Hiroshima University. Human serum for inoculation was obtained from a patient with chronic hepatitis B who provided informed consent.
Detection of HBsAg and anti-HBs in mouse serum
HBsAg and anti-HBs were measured with commercial ELISA kits (BioChain Institute, Hayward, CA, USA) according to the manufacturer’s instructions.
Protocol of clinical trial
To verify antiviral effects of HBIG, a clinical trial was conducted. Eight chronic hepatitis B patients were enrolled on the basis of the following criteria: (1) chronic hepatitis B patients who have undergone long-term NA therapy; (2) HBsAg levels less than 500 IU/mL; (3) no coinfection with other viruses, such as human immunodeficiency virus or hepatitis C virus; (4) no other liver diseases such as alcoholic liver disease, autoimmune hepatitis, liver cirrhosis, or hepatic cancer; (5) no coexisting conditions such as poorly controlled diabetes mellitus, decompensated renal disease, preexisting psychiatric disease, seizure disorders, cardiovascular disease, hemophilia, autoimmune diseases, or posttransplant patients; (6) not pregnant. Reed et al. [23] administered HBIG at a high dose (560 mg/kg) to chronic hepatitis B patients, but HBsAg clearance occurred only in patients who had low HBsAg titers at the baseline. Consequently, it may be difficult to achieve HBsAg loss in patients with high baseline HBsAg levels, and therefore we focused on patients with low baseline HBsAg levels (500 IU/mL or less). The experimental protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki and was approved by the Hiroshima University Hospital Ethics Committee (University Hospital Medical Information Network Center Clinical Trials Registry ID UMIN000002568). All study patients provided written informed consent to participate in the study at Hiroshima University Hospital, Hiroshima, Japan.
After their enrollment in the study, all study participants were given 1000 IU of HBIG (Hebsbulin IH, Mitsubishi Tanabe Pharma, Tokyo, Japan) monthly together with ongoing NA therapy. When the HBsAg level reduction was poor, we increased the dose of HBIG up to 2000 IU. Serum HBV DNA, HBsAg, and anti-HBs levels were measured every month. When HBsAg was reduced to undetectable levels and the patient became anti-HBs positive, an additional treatment, monthly hepatitis B vaccination (Bimmugen, Kaketsuken, Kumamoto, Japan), was performed to maintain anti-HBs titers. After 6 months of therapy, patients whose HBsAg levels had reduced by less than 1 log IU/mL were judged as nonresponders, and HBIG therapy was discontinued. In patients who achieved a greater decline in HBsAg levels, we discontinued HBIG and hepatitis B vaccine combination therapy depending on the trend of anti-HBs production with vaccination. When anti-HBs was induced by hepatitis B vaccination, we discontinued antiviral treatment including HBIG and NA therapy.
It has been reported that anti-HBs can interact with HBsAg and form antigen–antibody complexes, and the accumulation of these complexes in the kidney might induce renal dysfunction [23]. Therefore, we monitored serum creatinine levels as a precaution.
Statistical analysis
Statistical analysis was performed by repeated measures analysis of variance and the Mann–Whitney U test. P values less than 0.05 were considered statistically significant.
Results
Antiviral effect of HBIG in vivo
Twelve human hepatocyte chimeric mice were prepared and inoculated with human serum containing HBV particles. All mice developed measurable viremia 2 weeks after inoculation, and viremia reached a plateau 8 weeks after inoculation. The 12 mice were divided into three groups. Seven mice were treated with HBIG at 100 or 500 IU for 9 weeks after inoculation, and the remaining five mice were treated with saline as a control group. As shown in Fig. 1, HBV DNA levels were not significantly reduced by saline injection (control). Although the low-dose (100-IU) HBIG injection did not decrease HBV DNA levels in mouse sera sufficiently, the high-dose (500-IU) HBIG injection significantly decreased HBV DNA titers. Furthermore, 24 h after high-dose HBIG injection, all mouse sera became transiently HBsAg negative and transiently anti-HBs positive. Therefore, repetitive HBIG injection was hypothesized to reduce serum HBV DNA and HBsAg levels and potentially induce anti-HBs seroconversion.
Hepatitis B virus (HBV) DNA level reduction caused by antibody to hepatitis B surface antigen immunoglobulin (HBIG) injection in vivo. Four mice received 100 IU of HBIG and three mice received 500 IU of HBIG by injection. Phosphate-buffered saline was injected into five mice as a control group (control). Changes in HBV DNA levels in mouse sera were compared among the three groups. Statistical analysis was performed with the Mann–Whitney U test
Clinical study of HBIG injection
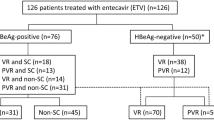
As it was assumed that sufficient antiviral effects could not be obtained in chronic hepatitis B patients with high viral loads and high HBsAg levels by HBIG therapy, we selected study patients whose HBV DNA titers had been reduced to unmeasurable levels and whose HBsAg levels were less than 500 IU/mL during NA therapy. Eight patients who fulfilled these criteria participated in the clinical study. The characteristics of these study participants are shown in Table 1. Five of the eight patients were male, and the mean age of the patients was 58 years. All patients were negative for hepatitis B e antigen (HBeAg) and HBV DNA was undetectable in all patients. Seven patients were being treated with entecavir at 0.5 mg/day , and the remaining patient was being treated with lamivudine at 100 mg/day. The mean duration of NA therapy was 91 months.
After written informed consent had been obtained, all patients were treated monthly with HBIG (median 22 injections; range 6–32 injections). The changes in HBsAg levels in each patient are shown in Fig. 2a. However, no differences in HBsAg level reduction were observed between responders and nonresponders after 3 months of HBIG therapy, and no association was observed between response to HBIG therapy and change in HBsAg titers during the year before therapy. At the end of HBIG therapy, HBsAg levels were significantly reduced, and the reduction was sustained at 6 months after the end of therapy (Fig. 2b). An HBsAg level reduction greater than 1 log IU/mL was observed in four of the eight patients. Three of these four patients became anti-HBs positive at the end of the therapy. At 6 months after the end of treatment, three patients were able to discontinue antiviral treatment including HBIG and NA therapy, and two patients achieved HBsAg loss and obtained anti-HBs. Although hepatitis B core antigen levels were also measured throughout the therapy, no significant changes in the levels were observed.
Hepatitis B surface antigen (HBsAg) level reduction caused by antibody to HBsAg immunoglobulin (HBIG) therapy: a each subject, b median ± standard deviation. HBsAg level reductions before, at 3 months of HBIG therapy, and at the end of treatment (EOT) or 6 months after HBIG therapy were compared. Statistical analysis was performed with the Mann–Whitney U test
During HBIG treatment, no adverse events, including exacerbation of hepatitis (Fig. 3a), renal dysfunction (Fig. 3b), virological breakthrough, or gastrointestinal symptoms, were observed in any patient.
Change of serum alanine aminotransferase (ALT) and creatinine levels caused by antibody to hepatitis B surface antigen immunoglobulin (HBIG) therapy. To evaluate the safety of HBIG therapy, serum ALT and creatinine levels before and at the end of treatment (EOT) or 6 months after HBIG therapy were compared. Statistical analysis was performed with the Mann–Whitney U test
Clinical courses of the patients who achieved HBsAg loss and obtained anti-HBs
The clinical courses of four patients who achieved HBsAg loss and obtained anti-HBs are described below.
Case 1
A 58-year-old woman with HBeAg-negative chronic hepatitis B (HBV genotype C) had been treated with entecavir at 0.5 mg/day for 85 months. Her HBV DNA was undetectable and her HBsAg level was 20.7 IU/mL. The clinical course of this patient during HBIG therapy is shown in Fig. 4a. In February 2010, HBIG therapy was started. The HBsAg titer became undetectable after 13 months of this therapy, and the woman became anti-HBs positive at 20 months. Therefore, we started HBIG and hepatitis B vaccine combination therapy. Although the woman had remained anti-HBs positive for more than 6 months, we discontinued antiviral therapy. After discontinuation of antiviral therapy, the woman remained HBsAg negative. Although she became anti-HBs negative after discontinuation of antiviral therapy, the anti-HBs titer increased following hepatitis B vaccination, and HBsAg loss and low HBV DNA levels continued for more than 1 year.
Clinical courses of four patients who achieved hepatitis B surface antigen (HBsAg) loss. a A 58-year-old woman who had been treated with entecavir at 0.5 mg/day for 85 months before antibody to HBsAg (anti-HBs) immunoglobulin (HBIG) therapy was treated with HBIG for 13 months. After this therapy, HBsAg became undetectable and antiviral therapy was successfully discontinued. HBsAg loss has since been maintained for more than 1 year. b A 49-year-old woman who had been treated with lamivudine at 100 mg/day for 173 months was treated with HBIG for 19 months. After this therapy, the HBsAg titer became undetectable, and she had remained positive for anti-HBs for more than 1 year. c A 42-year-old man who had been treated with entecavir at 0.5 mg/day for 75 months was treated with HBIG for 13 months. During the HBIG therapy, the HBsAg titer gradually increased and he did not become anti-HBs positive. After discontinuation of the therapy, the HBsAg titer was maintained at the same level as before HBIG therapy. d A 55-year-old woman who had been treated with entecavir at 0.5 mg/day for 64 months was treated with HBIG. After 5 months of therapy, she became anti-HBs positive, and we started HBIG and hepatitis B vaccine (HB vaccine) combination therapy. However, she never became HBsAg negative, and HBIG and HB vaccine combination therapy was discontinued at 21 months. Six months after discontinuation of the combination therapy, HBsAg levels returned to pretreatment levels. ALT alanine aminotransferase, HBsAb antibody to HBsAg, HBV hepatitis B virus
Case 2
A 49-year-old woman with HBeAg-negative chronic hepatitis B had been treated with lamivudine at 100 mg/day for 173 months. Her HBV DNA was undetectable, and her HBsAg level was 0.4 IU/mL. The clinical course of this patient during HBIG therapy is shown in Fig. 4b. In October 2011, HBIG therapy was started. She became anti-HBs positive after 2 months of this therapy, and she became HBsAg negative at 5 months. Therefore, we started HBIG and hepatitis B vaccine combination therapy. Although she had remained anti-HBs positive for more than 1 year, we discontinued antiviral therapy. After discontinuation of antiviral therapy, she remained HBsAg negative. Although she became anti-HBs negative after discontinuation of antiviral therapy, the anti-HBs titer increased following hepatitis B vaccination, and HBsAg loss was maintained for more than 1 year.
Case 3
A 42-year-old man with HBeAg-negative chronic hepatitis B (HBV genotype C) had been treated with entecavir at 0.5 mg/day for 75 months. His HBV DNA was undetectable, and his HBsAg level was 32.09 IU/mL. The clinical course of this patient during HBIG therapy is shown in Fig. 4c. In January 2013, HBIG therapy was started. Although HBIG therapy was continued for 13 months, the HBsAg titer gradually increased, and he did not become anti-HBs positive. Therefore, we considered that the patient was a nonresponder to HBIG therapy and discontinued antiviral therapy. After discontinuation of the therapy, the HBsAg titer was maintained at the same level as before HBIG therapy.
Case 4
A 55-year-old woman with HBeAg-negative chronic hepatitis B (HBV genotype C) had been treated with entecavir at 0.5 mg/day for 64 months. Her HBV DNA was undetectable, and her HBsAg level was 3.78 IU/mL. The clinical course of this patient during HBIG therapy is shown in Fig. 4d. In March 2012, HBIG therapy was started. She became anti-HBs positive after 5 months of this therapy, and we started HBIG and hepatitis B vaccine combination therapy. Her anti-HBs level transiently increased to 64.9 IU/mL in November 2013; however, her anti-HBs level gradually decreased and she became anti-HBs negative in spite of HBIG and hepatitis B vaccine combination therapy. Although she never became HBsAg negative, we discontinued HBIG and hepatitis B vaccine combination therapy. Six months after discontinuation of the combination therapy, her HBsAg levels returned to the pretreatment levels.
Discussion
There are several steps in the life cycle of HBV, such as attachment and binding to hepatocytes, endocytosis, transcription of several HBV RNAs, replication of the HBV genome, formation of viral particles, and exocytosis, but recent antiviral therapies for chronic hepatitis B have mainly targeted transcription of HBV RNA or replication of the HBV genome. Although these antiviral therapies are able to strongly suppress HBV replication, it is difficult to reduce HBsAg levels or clear cccDNA from the nucleus because of recycling of HBV DNA and reinfection of hepatocytes with HBV particles. Therefore, we considered that protection from HBV reinfection could reduce cccDNA and HBsAg production. According to several reports, HBIG can block HBV entry [24–28] and enhances the response of T cells [29]. However, it is unclear whether HBIG can decrease viral load in chronic hepatitis B patients. To clarify this issue, we performed an in vivo analysis using HBV-infected human hepatocyte chimeric mice before starting a clinical study. As shown in Fig. 1, serum HBV DNA levels decreased significantly following HBIG injection, and the reduction was enhanced in a dose-dependent manner. Furthermore, serum HBsAg also transiently decreased to an undetectable level 24 h after HBIG injection (data not shown). According to these results, it was considered that repetitive HBIG therapy could inhibit HBV reinfection and could reduce intracellular cccDNA and HBsAg production.
On the basis of the in vivo analysis, we conducted a clinical trial involving treatment of chronic hepatitis B patients with HBIG. Because it was considered to be difficult to obtain adequate results with patients with high initial HBV DNA or HBsAg levels, the study focused only on chronic hepatitis B patients undergoing long-term nucleotide analogue therapy who had undetectable HBV DNA levels and HBsAg levels less than 500 IU/mL (Table 1). After more than 1 year of HBIG therapy, a greater than 1 log reduction of HBsAg levels was observed in four of the eight patients, and two of these four patients achieved sustained HBsAg loss and were able to discontinue antiviral therapy (Fig. 4a, b). Although the clinical trial was conducted with a small number of patients, the HBsAg level reduction rate was high, and 25 % of patients achieved HBsAg loss. Furthermore, these results suggest that HBIG therapy might be a trigger for HBsAg level reduction, because in some cases HBsAg levels began to reduce after discontinuation of HBIG therapy (Fig. 4c). Considering the low HBsAg loss rate over the natural course or during antiviral therapy (0.6–11 %) [30–35], the HBsAg loss rate observed in this study appears quite high and suggests that HBIG combination therapy might induce additional HBsAg level reduction in patients with low HBsAg titers.
Furthermore, several interesting characteristics were observed in the two most successful clinical courses. Although anti-HBs titers gradually decreased after discontinuation of antiviral therapy, they rebounded following additional hepatitis B vaccination (Fig. 4a, b). Anti-HBs levels generally do not increase in chronic hepatitis B patients after additional hepatitis B vaccination, but these two patients reliably responded to the additional vaccination. The clinical results suggest that these patients might have been able to successfully eliminate HBV and that their immune responses to HBV were restored by the NA and HBIG combination therapy. However, transient HBV DNA elevation (2.1 log copies per milliliter or less) occurred despite HBsAg loss in these two patients, indicating that HBV cccDNA still remained in the nuclei of hepatocytes. Therefore, it is important to maintain anti-HBs levels at a higher titer to prevent HBV recurrence.
According to the Japanese Prescribing Information, the use of HBIG in HBsAg-positive HBV carriers is contraindicated because of concern about acute renal failure due to immune complex or anaphylaxis by activation of immune complement. However, the use of HBIG in HBV carriers is not contraindicated in other countries, and HBIG can be used safely to protect against HBV reinfection in patients who underwent liver transplantation for HBV-related liver failure. Furthermore, Reed et al. [23] reported that no severe adverse events were observed in six HBV carriers who received a high dose of HBIG. To verify the safety of the present study, we closely monitored monthly laboratory data. As shown in Fig. 3b, serum creatinine levels did not increase during HBIG therapy, and no other adverse events occurred. Although it is important to analyze a larger number of patients, these results suggest that HBIG therapy for chronic hepatitis B patients can be performed safely.
In conclusion, we demonstrated through both basic and clinical studies that blocking HBV reinfection with HBIG could promote reduction of HBV DNA and HBsAg levels. This study provides evidence that additional HBIG injection during antiviral therapy could be a useful option to induce HBsAg loss, potentially leading to discontinuation of long-term antiviral therapies.
Abbreviations
- Anti-HBs:
-
Antibody to hepatitis B surface antigen
- cccDNA:
-
Covalently closed circular DNA
- HBeAg:
-
Hepatitis B e antigen
- HBIG:
-
Antibody to hepatitis B surface antigen immunoglobulin
- HBsAg:
-
Hepatitis B surface antigen
- HBV:
-
Hepatitis B virus
- NA:
-
Nucleotide/nucleoside analogue
- NTCP:
-
Sodium taurocholate cotransporting polypeptide
References
Bruix J, Llovet JM. Hepatitis B virus and hepatocellular carcinoma. J Hepatol. 2003;39(Suppl 1):S59–63.
Conjeevaram HS, Lok AS. Management of chronic hepatitis B. J Hepatol. 2003;38(Suppl 1):S90–103.
Lee YS, Suh DJ, Lim YS, et al. Increased risk of adefovir resistance in patients with lamivudine-resistant chronic hepatitis B after 48 weeks of adefovir dipivoxil monotherapy. Hepatology. 2006;43:1385–91.
Suzuki Y, Kumada H, Ikeda K, et al. Histological changes in liver biopsies after one year of lamivudine treatment in patients with chronic hepatitis B infection. J Hepatol. 1999;30:743–8.
Belloni L, Allweiss L, Guerrieri F, et al. IFN-α inhibits HBV transcription and replication in cell culture and in humanized mice by targeting the epigenetic regulation of the nuclear cccDNA minichromosome. J Clin Investig. 2012;122:529–37.
Belloni L, Pollicino T, De Nicola F, et al. Nuclear HBx binds the HBV minichromosome and modifies the epigenetic regulation of cccDNA function. Proc Natl Acad Sci U S A. 2009;106:19975–9.
Brechot C, Gozuacik D, Murakami Y, et al. Molecular bases for the development of hepatitis B virus (HBV)-related hepatocellular carcinoma (HCC). Semin Cancer Biol. 2000;10:211–31.
Murakami Y, Saigo K, Takashima H, et al. Large scaled analysis of hepatitis B virus (HBV) DNA integration in HBV related hepatocellular carcinomas. Gut. 2005;54:1162–8.
Nagaya T, Nakamura T, Tokino T, et al. The mode of hepatitis B virus DNA integration in chromosomes of human hepatocellular carcinoma. Genes Dev. 1987;1:773–82.
Yaginuma K, Kobayashi H, Kobayashi M, et al. Multiple integration site of hepatitis B virus DNA in hepatocellular carcinoma and chronic active hepatitis tissues from children. J Virol. 1987;61:1808–13.
Lau GK, Piratvisuth T, Luo KX, et al. Peginterferon alfa-2a, lamivudine, and the combination for HBeAg-positive chronic hepatitis B. N Engl J Med. 2005;352:2682–95.
Marcellin P, Lau GK, Bonino F, et al. Peginterferon alfa-2a alone, lamivudine alone, and the two in combination in patients with HBeAg-negative chronic hepatitis B. N Engl J Med. 2004;351:1206–17.
Piccolo P, Lenci I, Demelia L, et al. A randomized controlled trial of pegylated interferon-alpha2a plus adefovir dipivoxil for hepatitis B e antigen-negative chronic hepatitis B. Antivir Ther. 2009;14:1165–74.
Takkenberg B, Terpstra V, Zaaijer H, et al. Intrahepatic response markers in chronic hepatitis B patients treated with peginterferon alpha-2a and adefovir. J Gastroenterol Hepatol. 2011;26:1527–35.
Yan H, Zhong G, Xu G, et al. Sodium taurocholate cotransporting polypeptide is a functional receptor for human hepatitis B and D virus. Elife. 2012;1:e00049.
Petersen J, Dandri M, Mier W, et al. Prevention of hepatitis B virus infection in vivo by entry inhibitors derived from the large envelope protein. Nat Biotechnol. 2008;26:335–41.
Ni Y, Lempp FA, Mehrle S, et al. Hepatitis B and D viruses exploit sodium taurocholate co-transporting polypeptide for species-specific entry into hepatocytes. Gastroenterology. 2014;146:1070–83.
Warner N, Locarnini S. The new front-line in hepatitis B/D research: identification and blocking of a functional receptor. Hepatology. 2013;58:9–12.
Krugman S, Giles JP, Hammond J. Viral hepatitis, type B (MS-2 strain) prevention with specific hepatitis B immune serum globulin. JAMA. 1971;218:1665–70.
Szmuness W, Prince AM, Goodman M, et al. Hepatitis B immune serum globulin in prevention of nonparenterally transmitted hepatitis B. N Engl J Med. 1974;290:701–6.
Tateno C, Yoshizane Y, Saito N, et al. Near completely humanized liver in mice shows human-type metabolic responses to drugs. Am J Pathol. 2004;165:901–12.
Tsuge M, Hiraga N, Takaishi H, et al. Infection of human hepatocyte chimeric mouse with genetically engineered hepatitis B virus. Hepatology. 2005;42:1046–54.
Reed WD, Eddleston AL, Cullens H, et al. Infusion of hepatitis-B antibody in antigen-positive active chronic hepatitis. Lancet. 1973;2:1347–51.
Itoh Y, Takai E, Ohnuma H, et al. A synthetic peptide vaccine involving the product of the pre-S(2) region of hepatitis B virus DNA: protective efficacy in chimpanzees. Proc Natl Acad Sci U S A. 1986;83:9174–8.
Iwarson S, Tabor E, Thomas HC, et al. Neutralization of hepatitis B virus infectivity by a murine monoclonal antibody: an experimental study in the chimpanzee. J Med Virol. 1985;16:89–96.
McAleer WJ, Buynak EB, Maigetter RZ, et al. Human hepatitis B vaccine from recombinant yeast. Nature. 1984;307:178–80.
Neurath AR, Kent SB, Strick N, et al. Genetic restriction of immune responsiveness to synthetic peptides corresponding to sequences in the pre-S region of the hepatitis B virus (HBV) envelope gene. J Med Virol. 1985;17:119–25.
Ogata N, Ostberg L, Ehrlich PH, et al. Markedly prolonged incubation period of hepatitis B in a chimpanzee passively immunized with a human monoclonal antibody to the a determinant of hepatitis B surface antigen. Proc Natl Acad Sci U S A. 1993;90:3014–8.
Celis E, Abraham KG, Miller RW. Modulation of the immunological response to hepatitis B virus by antibodies. Hepatology. 1987;7:563–8.
Buster EH, Flink HJ, Cakaloglu Y, et al. Sustained HBeAg and HBsAg loss after long-term follow-up of HBeAg-positive patients treated with peginterferon alpha-2b. Gastroenterology. 2008;135:459–67.
Chang TT, Lai CL, Kew Yoon S, et al. Entecavir treatment for up to 5 years in patients with hepatitis B e antigen-positive chronic hepatitis B. Hepatology. 2010;51:422–30.
Chu CM, Liaw YF. HBsAg seroclearance in asymptomatic carriers of high endemic areas: appreciably high rates during a long-term follow-up. Hepatology. 2007;45:1187–92.
Gish RG, Chang TT, Lai CL, et al. Loss of HBsAg antigen during treatment with entecavir or lamivudine in nucleoside-naive HBeAg-positive patients with chronic hepatitis B. J Viral Hepat. 2010;17:16–22.
Heathcote EJ, Marcellin P, Buti M, et al. Three-year efficacy and safety of tenofovir disoproxil fumarate treatment for chronic hepatitis B. Gastroenterology. 2011;140:132–43.
Zoutendijk R, Reijnders JG, Brown A, et al. Entecavir treatment for chronic hepatitis B: adaptation is not needed for the majority of naive patients with a partial virological response. Hepatology. 2011;54:443–51.
Acknowledgments
This study was supported in part by a Grant-in-Aid for Scientific Research from the Japanese Ministry of Labor, Health and Welfare. The authors thank Rie Akiyama and Yoko Matsumoto for excellent technical assistance and Akemi Sada, Chikako Kanehara, and Emi Nishio for clerical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Michio Imamura received honoraria from Bristol-Myers Squibb. Kazuaki Chayama received honoraria from Bristol-Myers Squibb and MSD. Masataka Tsuge and Michio Imamura received commercial research funding from Bristol-Myers Squibb. Kazuaki Chayama received commercial research funding from AbbVie, Dainippon Sumitomo Pharma, and RIKEN.
Rights and permissions
About this article
Cite this article
Tsuge, M., Hiraga, N., Uchida, T. et al. Antiviral effects of anti-HBs immunoglobulin and vaccine on HBs antigen seroclearance for chronic hepatitis B infection. J Gastroenterol 51, 1073–1080 (2016). https://doi.org/10.1007/s00535-016-1189-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-016-1189-x