Abstract
Background
The significance of HBV reactivation during immunosuppressive therapy was evaluated in three nationwide cohorts including patients with previously resolved HBV (prHBV) infection.
Methods
The clinical features of 1061 patients with acute liver failure (ALF) or late-onset hepatic failure (LOHF) were retrospectively examined, focusing on those who experienced HBV reactivation. Additionally, 420 patients with prHBV infection were prospectively enrolled: 203 received immunosuppressive therapies immediately after enrollment, while the remaining 217 were enrolled after having received immunosuppressive therapies without the occurrence of HBV reactivation. The serum HBV-DNA levels were prospectively monitored every month, and the incidences of HBV reactivation, defined as a serum HBV-DNA level of 1.3 log IU/ml or more, were evaluated.
Results
In the retrospective study, persistent HBV infection was found in 90 patients, and HBV reactivation was responsible for liver injuries in 50 patients including 23 receiving immunosuppressive therapies (26 with HBs-antigen positivity, 7 with prHBV infection). None of seven patients with prHBV infection were rescued. In the prospective studies, HBV reactivation occurred in ten patients, but preemptive entecavir administration prevented liver injury. The cumulative reactivation rate was 3.2 % at 6 months, and the increase of the rate compared to that at 6 months was +1.5 % at 48 months.
Conclusions
HBV reactivation during immunosuppression was responsible for liver injuries in a quarter of the ALF/LOHF patients with persistent HBV infection. Early serum HBV-DNA monitoring may improve patient prognosis, since HBV reactivation typically occurs within 6 months of the start of immunosuppressive therapies in patients with prHBV infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatitis B virus (HBV) infection is a global health problem; an estimated 2 billion people worldwide have either persistent or previously resolved infection, including 240 million individuals with serum HBs-antigen positivity [1]. Furthermore, approximately 1 million deaths per year are attributed to cirrhosis and/or hepatocellular carcinoma (HCC) caused by HBV infection [1, 2]. HBV infection is an important problem in Japan as well; the number of HBV carriers nationwide is estimated to exceed 1 million [3], and more than 20 % of the population over 50 years of age has a history of transient HBV infection [4], defined as serum anti-HBs and/or anti-HBc positivity despite a negative serum HBs-antigen status. These data suggest that more than 10 million Japanese people have either a persistent or previously resolved HBV (prHBV) infection. Such individuals have an increased risk of developing liver injuries because of HBV reactivation during and after immunosuppressive therapies and antineoplastic chemotherapies, since the covalently closed circular DNA (cccDNA) of the HBV genome inevitably persists in the nuclei of hepatocytes even in patients with a history of a transient HBV infection.
HBV reactivation in patients with prHBV infection was originally documented in 1975 by Wands et al. [5]; they reported that hepatitis with reverse seroconversion from negative to positive for serum HBs-antigen developed in patients who were positive for serum anti-HBs after chemotherapies for myeloproliferative and lymphoproliferative disorders. Their observations were prospectively confirmed by Loc et al. in 1991 [6]. Much attention has been paid to HBV reactivation since 1998, when Uemoto et al. demonstrated that HBV can be transmitted to recipients when living-related liver transplantations were performed using transplants from donors who were positive for serum anti-HBc, despite having a negative HBs-antigen status [7]. Liver injuries as a result of HBV reactivation in patients with prHBV infection, so-called “de novo hepatitis B,” are a serious problem, especially in those receiving chemotherapies for hematological malignancies [5, 6]. Rituximab, a molecularly targeted drug for CD20, is recognized as a high-risk factor for provoking de novo hepatitis B and/or HBV reactivation in patients with prHBV infection [8].
Controversy still exists, however, as to whether HBV reactivation can occur during immunosuppressive therapies in patients with prHBV infection. Recently, Barone et al. reported that HBV reactivation did not occur during long-term therapies with biologic agents in rheumatologic patients with prHBV infection [9]. In contrast, numerous studies performed in Japan have shown the development of de novo hepatitis B and/or HBV reactivation during immunosuppressive therapies in rheumatologic patients with prHBV infection [10–12].
Thus, to clarify the significance of HBV reactivation during immunosuppressive therapies in patients with prHBV infection, three nationwide cohorts were examined. First, the recent status of patients with severe de novo hepatitis B was examined through a nationwide survey of patients with acute liver failure (ALF) or late-onset hepatic failure (LOHF) in Japan (part 1). Second, the incidences of HBV reactivation during immunosuppressive therapies in patients with prHBV infection were prospectively evaluated in two cohorts (parts 2 and 3). In addition, the usefulness of the Japanese guideline for the prevention of liver injuries caused by HBV reactivation [13, 14] was assessed.
Patients and methods
Study designs
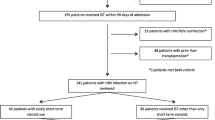
Three nationwide cohorts were studied (Fig. 1). Part 1 was performed as a project by the Intractable Hepato-Biliary Diseases Study Group of Japan (Ministry of Health, Labour and Welfare). Patients diagnosed as having ALF or LOHF were retrospectively enrolled, and the clinical features and outcomes of patients with HBV reactivation, in particular, were examined. In Parts 2 and 3, patients with prHBV infection were enrolled in a project conducted by the Study Groups for Research on Hepatitis and BSE of Japan (Ministry of Health, Labour and Welfare), and the incidences of HBV reactivation during various types of immunosuppressive therapies were prospectively evaluated.
Study designs for three nationwide studies. In Part 1, 1061 patients with acute liver disease (ALF) or late-onset hepatic failure (LOHF) treated between 2010 and 2013 were retrospectively enrolled from 1007 institutes through annual surveys. In contrast, in Parts 2 and 3, a total of 578 patients were enrolled from 197 institutes, and 420 patients scheduled to receive immunosuppressive therapies were analyzed in a prospective survey to clarify the incidence of HBV reactivation, defined as an increase in the serum HBV-DNA level of 1.3 log IU/ml or more; 158 patients scheduled to receive antineoplastic chemotherapy were analyzed as a reference group
Part 1 was performed with the approval of the Institutional Review Board of Saitama Medical University, and Parts 2 and 3 were conducted with the approval of the Institutional Review Board of each hospital at which the patients were enrolled as well as that of Saitama Medical University; written informed consent was obtained from all the participants (UMIN Clinical Trials Registry IDs: UMIN 000002859 for Part 2 and UMIN000008875 for Part 3).
Nationwide survey of patients with ALF or LOHF because of HBV reactivation in Japan (Part 1)
Patients diagnosed as having ALF or LOHF between 1 January 2010 and 31 December 2013 were enrolled from 1007 institutes with specialists in the fields of hepatology, gastroenterology, and/or acute medicine. All the patients had prothrombin time values (international normalization ratio: INR) of 1.5 or more according to the diagnostic criteria for ALF established by the Intractable Hepato-Biliary Diseases Study Group of Japan [15, 16].
The survey was performed in two steps: first, a questionnaire was sent annually to specialists at each institute asking whether any patients with ALF or LOHF had been treated in the previous year; then, a second questionnaire was sent to the institutes that had responded positively to obtain further details regarding the demographic and clinical features, the therapies that were used, and the outcomes of the patients. The etiologies of the liver diseases were determined according to the classification criteria of the Intractable Hepato-Biliary Diseases Study Group of Japan [17].
Prospective studies to evaluate the incidence of HBV reactivation during immunosuppressive therapies in patients with PrHBV infection (Parts 2 and 3)
In both Part 2 and Part 3, the subjects were patients with prHBV infections who tested positive for serum anti-HBs and/or anti-HBc despite having a negative serum HBs-antigen status. In Part 2, the patients were enrolled from 101 institutes with staff specializing in rheumatology (19 institutes), nephrology (16 institutes), hematology (47 institutes), or oncology (19 institutes); all the patients were enrolled between 1 January 2010 and 31 March 2012 and immediately received immunosuppressive therapy and/or antineoplastic chemotherapy without rituximab. In contrast, in Part 3, patients with prHBV infection were enrolled from 96 institutes with staff specializing in rheumatology (32 institutes), gastroenterology (35 institutes), dermatology (16 institutes), or ophthalmology (13 institutes) between 1 April 2012 and 31 March 2014. In this study, patients who had already been given immunosuppressive therapies at the time of enrollment, but HBV reactivation had not yet been observed, were included as well as those receiving the therapies after the enrollment. The inclusion criteria for the immunosuppressive therapies and antineoplastic chemotherapies permitted in Parts 2 and 3 are shown in Table 1.
In both studies, the serum HBV-DNA levels were measured every month during and after immunosuppressive therapy using the COBAS AmpliPrep/COBAS TaqMan HBV Test, v2.0 (Roche Diagnostics, K.K., Tokyo, Japan), which is based on a real-time polymerase chain reaction (PCR) assay [18]. Monitoring of the serum HBV-DNA levels was continued until 12 months after the discontinuation of the therapies. The cumulative incidences of HBV reactivation, defined as an increase in the serum HBV-DNA levels of 1.3 log IU/ml or more, during the immunosuppressive therapies were evaluated using the Kaplan-Meier method. The cumulative incidence within 6 months after the initiation of therapy was calculated for the patients enrolled in Part 2, and the cumulative incidence after 6 months of therapy was calculated for the patients enrolled in Parts 2 and 3. Regarding Part 2, patients with rheumatoid and renal diseases were included in the analysis, while those with myeloproliferative and lymphoproliferative diseases and malignancies of solid organs were excluded, although their data were assessed as a reference for patients receiving immunosuppressive therapies.
Results
Patients with ALF or LOHF caused by HBV reactivation (Part 1)
As shown in Fig. 1, a total of 1061 patients with ALF or LOHF (1021 and 40 patients, respectively) were enrolled (554 males and 507 females; median age, 54 years; age range, 1–94 years). The subjects consisted of 512 patients without hepatic coma and 549 patients with hepatic coma; the patients with hepatic coma consisted of 283 patients with acute hepatic coma (acute type), 226 with subacute hepatic coma (subacute type), and 40 with LOHF, among whom hepatic encephalopathy of grade II or more developed within 10 days, between 11 and 56 days, and after 56 days, respectively, of the onset of disease symptoms according to the criteria of the Intractable Hepato-Biliary Diseases Study Group of Japan [15, 16]. The disease etiologies were diagnosed as viral infection in 319 patients (30.1 %), drug-induced liver injury in 145 patients (13.7 %), autoimmune hepatitis in 103 patients (9.7 %), liver injuries without hepatitis (such as circulatory failure) in 184 patients (17.3 %), and indeterminate in 282 patients (26.6 %). Among the patients whose injuries were caused by viral infection, HBV infection was found in 225 patients (70.5 %): 88 without hepatic coma, 74 with acute hepatic coma, 52 with subacute hepatic coma, and 11 with LOHF.
In addition, the 225 patients with HBV infection were classified into 127 patients who experienced a transient infection immediately before the onset of liver failure (56.4 %) and 90 patients with persistent HBV infection (40.0 %); 65 asymptomatic or inactive HBV carriers who exhibited an acute exacerbation of hepatitis (28.9 %) and 25 patients with prHBV infection who developed HBV reactivation (11.1 %); the infection pattern was indeterminate in the remaining 8 patients (3.6 %) (Fig. 1). Immunosuppressive therapies and/or antineoplastic chemotherapies were responsible for liver failure in 26 HBV carriers (40.0 %) and 24 patients with prHBV infection (96.0 %). The therapies that caused HBV reactivation are summarized in Fig. 2. Antineoplastic chemotherapies containing rituximab were responsible for HBV reactivation in 1 HBV carrier (3.8 %) and in 13 patients with prHBV infection (54.2 %), while antineoplastic chemotherapies without rituximab contributed to HBV reactivation in 9 patients (34.6 %) in the former group and 4 (16.7 %) in the latter group; immunosuppressive therapies contributed to HBV reactivation in 16 patients (61.5 %) and 7 patients (29.2 %), respectively.
Causative therapies responsible for the development of HBV reactivation in patients with acute liver failure or late-onset hepatic failure. a HBs-antigen-positive carriers (n = 26); b HBs-antigen-negative subjects with previously resolved HBV (prHBV) infection (n = 24). Antineoplastic chemotherapies including rituximab were responsible for HBV reactivation in 1 HBV carrier and 13 patients with prHBV infection. The antineoplastic chemotherapies without rituximab and immunosuppressive therapies that induced HBV reactivation are summarized in the lower tables
The outcomes of the patients with ALF or LOHF were unfavorable. Among the 39 HBV carriers in whom liver injuries occurred spontaneously without immunosuppressive therapies and/or antineoplastic chemotherapies, 13 patients (33.3 %) were rescued without requiring a liver transplantation. Among the patients who developed iatrogenic HBV reactivation, 5 of 26 HBV carriers (19.2 %) and 1 of 24 patients with prHBV infection (4.2 %) were rescued using only medical care; the survival rate of the latter patients was significantly lower than that of the HBV carriers who had not undergone immunosuppressive therapies (p < 0.05, Fisher's exact test). Regarding the patients who received immunosuppressive therapies, none of the seven patients with prHBV infection were rescued. In all the patients who developed ALF or LOHF as a result of HBV reactivation, the immunosuppressive therapies and/or antineoplastic chemotherapies that had been performed did not comply with the JSH Guidelines [13, 14]: HBV carriers did not receive nucleoside/nucleotide analogs preemptively, and monitoring of the serum HBV-DNA levels had not been performed in patients with prHBV infection.
Viral reactivation during and after immunosuppressive therapies and/or antineoplastic chemotherapies in patients with PrHBV infection (Part 2)
A total of 289 patients with prHBV infection were enrolled; 209 patients (72.3 %) were positive for both serum anti-HBc and anti-HBs, while 59 (20.4 %) and 21 (7.3 %) were positive for either serum anti-HBc or anti-HBs, respectively, even though the latter patients had not received an HBs-antigen vaccination. Among them, 131 patients received immunosuppressive therapies for rheumatoid and renal diseases, and 158 patients were given antineoplastic chemotherapies for hematological diseases and solid organ cancers. The drugs administered to these patients are summarized in Table 2.
The serum HBV-DNA levels were less than 1.3 log IU/ml at baseline in all the patients, but were qualitatively detectable in six patients (2.1 %) (Table 3a). The serum HBV-DNA levels were measured every month during and after the therapies; the median observation period for patients receiving immunosuppressive therapies was 40 months, ranging from 1 to 62 months, while that for patients receiving antineoplastic chemotherapies was 14 months, ranging from 1 to 55 months. As shown in Table 3, serum HBV-DNA became detectable in 20 patients (6.9 %) following the initiation of therapy (9 patients receiving immunosuppressive therapies, 6.9 %; 11 patients receiving antineoplastic chemotherapies, 7.0 %). Among these patients, the serum HBV-DNA levels increased to 1.3 log IU/ml or more in 11 patients (3.8 %): at 2–32 months after the initiation of therapy in 5 patients who received immunosuppressive drugs and at 4–34 months after the initiation of antineoplastic chemotherapy in 6 patients. HBV reactivation was not correlated with the baseline serum anti-HBs or anti-HBc levels.
Among the 11 patients with serum HBV-DNA levels of 1.3 log IU/ml or more, entecavir (0.5 mg/day) was administered immediately after the diagnosis of HBV reactivation in ten patients; consequently, none of these patients developed an elevated serum ALT level. In a patient with rheumatoid arthritis, however, the serum HBV-DNA level increased to 1.4 log IU/ml at 32 months but then spontaneously decreased to less than 1.3 log IU/ml at 1 month thereafter, while preemptive entecavir administration was performed. In the remaining one patient with hypopharyngeal cancer, the serum HBV-DNA level increased to 1.5 log IU/ml at 34 months, but decreased to less than 1.3 log IU/ml at 1 month thereafter, so preemptive entecavir administration was not done. In contrast, among the six patients with detectable serum HBV-DNA at baseline, the serum HBV-DNA levels did not exceed 1.3 log IU/ml in three patients during immunosuppressive therapies and/or antineoplastic chemotherapies without entecavir administration. Also, in 12 patients with detectable serum HBV-DNA levels during therapy, neither de novo hepatitis B nor HBV reactivation developed even without preemptive entecavir administration.
Viral reactivation during immunosuppressive therapies in patients with PrHBV infection (Part 3)
A total of 289 patients with prHBV infection, consisting of 200 patients with rheumatoid diseases, 44 patients with skin diseases, 28 patients with intestinal diseases, and 17 patients with ophthalmological diseases, were enrolled. PrHBV infection was diagnosed before the initiation of immunosuppressive therapies in 187 patients (64.7 %) and during the therapies in 102 patients (35.3 %). Two hundred twelve patients (73.4 %) were positive for both serum anti-HBc and anti-HBs, and the remaining 77 patients were positive for either serum anti-HBc or anti-HBs despite not having received an HBs-antigen vaccination. Seventy-two patients were enrolled before the initiation of immunosuppressive therapies, but 52 patients were enrolled between 0 and 6 months after the initiation of immunosuppressive therapies, and 21 patients were enrolled between 6 and 12 months, 41 patients were enrolled 12–24 months, 24 patients were enrolled 24–36 months, and 79 patients were enrolled more than 36 months after the initiation of immunosuppressive therapy. In all the patients, the serum HBV-DNA levels were measured every month after enrollment. The durations between the initiation of immunosuppressive therapies and final monitoring of the serum HBV-DNA levels were as follows: <12 months in 4 patients (1.4 %), 12–23 months in 18 patients (6.2 %), 24–35 months in 69 patients (23.8 %), 36–47 months in 60 patients (20.8 %), 48–59 months in 47 patients (16.3 %), and ≥60 months in 91 patients (31.5 %).
Serum HBV-DNA became detectable in nine patients (3.1 %) at a median of 25 months after enrollment, ranging from 4 to 201 months after the initiation of immunosuppressive therapy, and the levels exceeded 1.3 log IU/ml in five patients (1.7 %) (Table 3b). Among these five patients with HBV reactivation, the serum HBV-DNA levels were further increased in only one patient at 1 month thereafter; in the remaining four patients, the serum HBV-DNA level remained unchanged or decreased spontaneously. Preemptive entecavir administration was not performed in one patient despite HBV reactivation, but the serum ALT level did not increase in any of the five patients who showed HBV reactivation during immunosuppressive therapy.
Cumulative incidence of HBV reactivation during immunosuppressive therapies in patients with PrHBV infection (Parts 2 and 3)
Kaplan-Meier analyses were performed for the 131 patients who received immunosuppressive therapies after enrollment in Part 2 and the 289 patients who were enrolled in Part 3. Among the patients in Part 2 (Fig. 3a), the cumulative incidences of serum HBV-DNA detection were 3.8 % at baseline and 7.9 %, 8.7, 8.7, and 12.0 % at 6, 12, 24, and 48 months, respectively. The cumulative incidence of HBV reactivation, defined as a serum HBV-DNA level of 1.3 log IU/ml or more, was 3.2 % at 6 months after the initiation of immunosuppressive therapy, while the increase of cumulative incidences at time points after 6 months were relatively small. Thus, a Kaplan-Meier analysis was performed for patients enrolled in both Parts 2 and 3 to clarify the increase of cumulative incidences after 6 months of immunosuppressive therapy, and the percentages were found to be 0 % at 12 months and +0.5, +1.5, and +1.5 % at 24, 36, and 48 months, respectively (Fig. 3b).
Incidence of HBV reactivation during immunosuppressive therapies in patients with previously resolved HBV infection. a Incidence (%) of HBV reactivation evaluated in patients enrolled in Part 2 (n = 131). b Incidence (%) of HBV reactivation evaluated in patients enrolled in both Parts 2 and 3 (n = 420)
Discussion
A nationwide survey of patients with ALF or LOHF has been performed annually by the Intractable Hepato-Biliary Diseases Study Group of Japan, and a total of 1061 patients treated between 2010 and 2013 were enrolled in the present study (Part 1). These subjects consisted of 863 patients with hepatitis and 198 without hepatitis, including patients with circulatory disturbances and acetaminophen intoxication; HBV infection was responsible for liver injuries in 225 patients (26.1 % of the hepatitis patients). According to previous nationwide surveys performed in Japan, HBV infection was found in 462 patients (39.0 %) among 1,186 hepatitis patients with ALF or LOHF treated between 1998 and 2009 [19, 20]. Thus, the number of patients with ALF or LOHF as a result of HBV infection seems to be decreasing, possibly because of the use of nucleoside/nucleotide analogs for the treatment of severe hepatitis B. Of note, however, HBV reactivation because of immunosuppressive therapies and/or antineoplastic chemotherapies was responsible for liver injuries in 50 patients: 26 (40.0 %) of 65 HBV carriers and 24 (96.0 %) of 25 patients with prHBV infection. To our surprise, the drugs that were thought to have caused HBV reactivation were used for immunosuppressive therapies in 22 patients, including 7 patients with prHBV infection. As shown in Fig. 2, monotherapies or combination therapies with glucocorticoid, methotrexate, and cyclophosphamide as well as biologic therapies provoked ALF or LOHF in patients with prHBV infection, and all of these patients died without receiving liver transplantation. Recently, Barone et al. reported that HBV reactivation was not seen among 1218 rheumatologic patients receiving immunosuppressive therapies with biologic agents, including 179 patients with prHBV infection [9]. However, HBV reactivation caused by immunosuppressive therapies as well as antineoplastic chemotherapies is a crucial health problem in Asian countries where HBV infection is prevalent.
Since 2010, we have conducted two multicenter prospective studies to clarify the incidence of HBV reactivation during immunosuppressive therapies as a project by the study group of the Ministry of Health, Labour and Welfare. First, 289 patients with prHBV infection were enrolled from 101 institutes (Part 2). Among them, 131 patients were given immunosuppressive therapies for various diseases. The sample size was almost equivalent to that reported by Barone et al. [9]. In their study, however, all the patients received biologic agents such as rituximab and anti-TNF-α, while biologic agents were administered in only 74 patients (60.2 %) in our trial. Among these patients, the serum HBV-DNA levels were measured every month during the therapies, and the incidence of HBV reactivation, defined as a serum HBV-DNA level of 1.3 log IU/ml or more, was evaluated. The data obtained from the remaining 158 patients receiving antineoplastic chemotherapies were also assessed as a reference for those receiving immunosuppressive therapies.
In Part 2, HBV reactivation was observed in five patients receiving immunosuppressive therapies (3.8 %) and in six patients with antineoplastic chemotherapies (3.8 %). HBV reactivation occurred even in patients with a high serum anti-HBs titer and in those with a low serum anti-HBc titer; in these patients, a previous transient HBV infection was suspected as the infection pattern, as HBV carriers during the immunosurveillance stage were thought to be unlikely. Recently, the American Gastroenterological Association (AGA) published an institute guideline on the prevention and treatment of HBV reactivation [21] and suggested against using anti-HBs status to guide antiviral prophylaxis during immunosuppressive therapies; this statement is in line with our observations. Also, HBV reactivation developed in patients receiving monotherapies with glucocorticoid and methotrexate as well as combination therapies including biologic agents. Six patients had detectable serum HBV at a level of less than 1.3 log IU/ml at baseline. Among them, HBV reactivation only occurred in three patients. In contrast, serum HBV-DNA became detectable in 12 patients during immunosuppressive therapies and antineoplastic chemotherapies, but the levels did not exceed 1.3 log IU/ml even without entecavir administration. These data suggest that the preemptive administration of nucleoside/nucleotide analogs is required in patients with prHBV infection when the serum HBV-DNA level increases to 1.3 log IU/ml or more during immunosuppressive therapy or antineoplastic chemotherapy.
Although the percentages of patients who developed HBV reactivation did not differ between those receiving immunosuppressive therapy and those receiving antineoplastic chemotherapy, the periods from the initiation of therapy until HBV reactivation differed between the two groups. In patients receiving immunosuppressive drugs, HBV reactivation occurred within 3 months except in one patient with SLE in whom serum HBV-DNA became detectable after 4 months of therapy. In this patient, the serum HBV-DNA level increased to 1.4 log IU/ml at 32 months but then spontaneously decreased to less than 1.3 log IU/ml at 33 months. In contrast, in patients receiving antineoplastic chemotherapies, HBV reactivation occurred later than 6 months except in one patient with esophageal cancer. These observations prompted us to postulate that HBV reactivation may typically develop within 3 months in patients with preHBV infection who are undergoing immunosuppressive therapies. Thus, in Part 3, 289 patients with prHBV infection in whom HBV reactivation has not yet developed during immunosuppressive therapies were enrolled, and the incidence of HBV reactivation after at least 6 months of therapy was evaluated. In this study, HBV reactivation developed in five patients, but a further increase in the serum HBV-DNA levels at 1 month thereafter was only observed in one. Among the remaining four patients with HBV reactivation, preemptive entecavir administration was not performed in one in whom a further increase in the serum HBV-DNA level and an elevation in the ALT level were not observed for 26 months after HBV reactivation. These observations agreed with those in patients with HBV reactivation at 32 months of immunosuppressive therapy in Part 2.
To quantify the risk of HBV reactivation during immunosuppressive therapies in patients with preHBV infection, a Kaplan-Meier analysis was performed for patients enrolled in both Part 2 and Part 3. The cumulative incidence of HBV reactivation within 6 months was evaluated in 131 patients in Part 2, and an increase of the cumulative percentage at later than 6 months was assessed in the 420 patients enrolled in Parts 2 and 3. Consequently, the cumulative incidences of HBV reactivation were 0, 3.2, and 3.2 % at 1, 3, and 6 months, respectively, among patients receiving immunosuppressive therapies, and these percentages did not change until 12 months, with an increase of overall percentage of 1.5 % even at 48 months.
The risk of HBV reactivation in patients with prHBV infection differs depending on the type of therapy. Dickson et al. reported that HBV reactivation developed in 78 % of recipients receiving transplants from patients with a negative serum HBs-antigen status and a positive serum anti-HBc status during immunosuppressive therapies after liver transplantation [22]; the percentage was almost equivalent to that reported by Uemoto et al. [7]. In contrast, in patients receiving allogeneic hematopoietic stem cell transplantation, the risk of HBV reactivation has been controversial, with reported percentages ranging from nearly 100 [23] to 2.7 % [24]. Recently, Kusumoto et al. reported that HBV reactivation developed during or after chemotherapies including rituximab in 8.3 % of malignant lymphoma patients with prHBV infection [25]. The present study is the first report to describe the cumulative incidence of HBV reactivation during immunosuppressive therapies among patients with prHBV infection. The AGA guideline categorized immunosuppressive therapies into low-, moderate-, or high-risk groups [21], and patients with prHBV infection receiving monotherapies with methotrexate or prednisone at daily doses of 10 mg or less were classified to the low-risk group. In the present study, patients receiving prednisone at daily doses of 0.5 mg/kg body weight or more were enrolled, suggesting that the cumulative incidence shown in the manuscript corresponds mainly to that in the moderate-risk group in the AGA guideline. It should be noted, however, that HBV reactivation developed even in a patient receiving methotrexate monotherapy who was classified to the low-risk group. Factors associated with HBV reactivation should be clarified in the future.
The current guidelines of both the American Association for the Study of Liver Diseases and the European Association for the Study of Liver recommend monitoring of the serum ALT levels as well as the HBV-DNA level in patients with preHBV infection who are being treated with immunosuppressive therapies and/or antineoplastic chemotherapies [26, 27]. Also, the Guideline of the Japan Society of Hepatology (JSH Guideline) has suggested that the serum HBV-DNA level should be measured every 1 to 3 months during immunosuppressive therapies and/or antineoplastic chemotherapies until at least 12 months after the discontinuation of treatment, and nucleoside/nucleotide analogs should be preemptively given in patients showing HBV-DNA levels of 1.3 log IU/ml or more [14]. In Parts 2 and 3, liver injuries did not occur in any of the patients with HBV reactivation when entecavir was administered when the serum HBV-DNA levels increased to 1.3 log IU/ml or more. In contrast, in Part 1, monitoring of the serum HBV-DNA levels was not performed in any of the patients with prHBV infection who developed ALF or LOHF. Considering these observations, the JSH guideline seems to be useful for preventing liver injuries in patients with prHBV infection who must undergo immunosuppressive therapy. The monitoring of serum HBV-DNA levels should be done especially during the early stage of immunosuppressive therapies, at least until 6 months of therapy, but the significance of monitoring during the late stage will require further evaluation since the risk of HBV reactivation decreased at time points beyond 6 months among the subjects enrolled in Parts 2 and 3.
In conclusion, HBV reactivation because of immunosuppressive therapy or antineoplastic chemotherapy without rituximab was not infrequent among Japanese patients with prHBV infection who developed fatal liver injuries, such as ALF or LOHF. The cumulative incidence of HBV reactivation in patients with prHBV infection was 3.2 % at 6 months after the initiation of immunosuppressive therapies, and the risk decreased at time points later than 6 months. Thus, the monitoring of serum HBV-DNA levels should be performed every month at least until 6 months after the initiation of immunosuppressive therapies, and nucleoside/nucleotide analogs should be administered to patients with serum HBV-DNA levels of 1.3 log IU/ml or more. The significance of monitoring more than 6 months of immunosuppressive therapies requires further investigation.
References
World Health Organization. Hepatitis: fact sheet N°204, July 2015. www.who.int/mediacentre/factsheets/fs204/en/.
Perz JF, Armstrong GL, Farrington LA, et al. The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer world wide. J Hepatol. 2006;45:529–38.
Tanaka J, Kumagai J, Katayama K, et al. Sex- and age-specific carriers of hepatitis B and C virus in Japan estimated by the prevalence in the 3,485,648 first-time blood donors during 1995–2000. Intervirol. 2004;47:32–40.
Kusumoto S, Tanaka Y, Mizokami M, et al. Reactivation of hepatitis B virus following systemic chemotherapy for malignant lymphoma. Int J Hematol. 2009;90:13–23.
Wands JR, Chura CM, Roll FJ, et al. Serial studies of hepatitis-associated antigen and antibody in patients receiving antitumor chemotherapy for myeloproliferative and lymphoproliferative disorders. Gastroenterology. 1975;68:105–12.
Lok AS, Liang RH, Chiu EK, et al. Todd D. Reactivation of hepatitis B virus replication in patients receiving cytotoxic therapy. Report of a prospective study. Gastroenterology. 1991;100:182–8.
Uemoto S, Sugiyama K, Marusawa H, et al. Transmission of hepatitis B virus from hepatitis B core antibody-positive donors in living related liver transplants. Transplantation. 1998;65:494–9.
Dervite I, Hober D, Morel P. Acute hepatitis B in a patient with antibodies to hepatitis B surface antigen who was receiving rituximab. N Engl J Med. 2001;344:68–9.
Barone M, Notarnicola A, Lopalco G, et al. Safety of long-term biologic therapy in rheumatologic patients with a previously resolved hepatitis B viral infection. Hepatology. 2015;62:40–6.
Urata Y, Uesato R, Tanaka D, et al. Prevalence of reactivation of hepatitis B virus replication in rheumatoid arthritis patients. Mod Rheumatol. 2011;21:16–23.
Mori S. Past hepatitis B infection in rheumatoid arthritis patients receiving biologic and/or nonbiologic disease-modifying antirheumatic drugs. Mod Rheumatol. 2011;21:621–7.
Tamori A, Koike T, Goto H, et al. Prospective study of reactivation of hepatitis B in patients with rheumatoid arthritis who received immunosuppressive therapy: evaluation of both HBsAg-positive and HBsAg-negative cohorts. J Gastroenterol. 2011;46:556–64.
Oketani M, Ido A, Uto H, et al. Prevention of hepatitis B virus reactivation in patients receiving immunosuppressive therapy or chemotherapy. Hepatol Res. 2012;42:627–36.
Drafting Committee for Hepatitis Management Guidelines and the Japan Society of Hepatology. JSH guidelines for the management of hepatitis B virus infection. Hepatol Res. 2014;44(Suppl S1):1–58.
Mochida S, Takikawa Y, Nakayama N, et al. Diagnostic criteria of acute liver failure: a report by the intractable hepato-biliary diseases study group of Japan. Hepatol Res. 2011;41:805–12.
Sugawara K, Nakayama N, Mochida S. Acute liver failure in Japan: definition, classification, and prediction of the outcome. J Gastroenterol. 2012;47:849–61.
Mochida S, Takikawa Y, Nakayama N, et al. Classification of the etiologies of acute liver failure in Japan: a report by the intractable hepato-biliary diseases study group of Japan. Hepatol Res. 2014;44:365–7.
Allice T, Cerutti F, Pittaluga F, et al. COBAS AmpliPrep-COBAS TaqMan hepatitis B virus (HBV) test: a novel automated real-time PCR assay for quantification of HBV DNA in plasma. J Clin Microbiol. 2007;45:828–34.
Fujiwara K, Mochida S, Matsui A, et al. Intractable liver diseases study group of Japan. Fulminant hepatitis and late onset hepatic failure in Japan: summary of 698 patients between 1998 and 2003 analyzed by the annual nationwide survey. Hepatol Res. 2008;38:646–57.
Oketani M, Ide A, Nakayama N, et al. Etiology and prognosis of fulminant hepatitis and late-onset hepatic failure in Japan: summary of the annual nationwide survey between 2004 and 2009. Hepatol Res. 2013;43:97–105.
Reddy KR, Beavers KL, Hammond SP, et al. American gastroenterological association institute guideline on the prevention and treatment of hepatitis B virus reactivation during immunosuppressive drug therapy. Gastroenterology. 2015;148:215–9.
Dickson RC, Terrault NA, Ishitani M, et al. Protective antibody levels and dose requirements for IV 5 % Nabi hepatitis B immune globulin combined with lamivudine in liver transplantation for hepatitis B-induced end stage liver disease. Liver Transpl. 2006;12:124–33.
Knöll A, Boehm S, Hahn J, et al. Long-term surveillance of haematopoietic stem cell recipients with resolved hepatitis B: high risk of viral reactivation even in a recipient with a vaccinated donor. J Viral Hepat. 2007;14:478–83.
Nakamoto S, Kanda T, Nakaseko C, et al. Reactivation of hepatitis B virus in hematopoietic stem cell transplant recipients in Japan: efficacy of nucleos(t)ide analogues for prevention and treatment. Int J Mol Sci. 2014;15:21455–67.
Kusumoto S, Tanaka Y, Suzuki R, et al. Monitoring of hepatitis B virus (HBV) DNA and risk of HBV reactivation in B-Cell lymphoma: a prospective observational study. Clin Infect Dis. 2015;61:719–29.
Lok AS, McMahon BJ. Chronic hepatitis B: update 2009. Hepatology. 2009;50:661–2.
European Association for the Study of Liver. EASL clinical practical guidelines: management of alcoholic liver disease. J Hepatol. 2012;57:399–420.
Acknowledgments
We thank the doctors for their cooperation in enrolling patients to Parts 2 and 3 (Supplementary Table). This study was performed with the support of the Ministry of Health, Labour and Welfare as an official project by the Intractable Hepato-biliary Diseases Study Group of Japan and by the Research on Hepatitis and BSE.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Satoshi Mochida has received research grants, speaking fees, or honoraria from Bristol Myers Squibb, Chugai Pharmaceutical Co. Ltd., Dainippon, Mitsubishi Tanabe Pharma Co., MSD K.K., Toray Medical Co. Ltd., Ajinomoto Pharmaceuticals Co. Ltd., and Eisai Co. Ltd. Satoshi Mochida and Yoshihito Uchida have received patent royalties from SRL Inc. Masayoshi Harigai has received research grants from Abbvie Japan Co. Ltd., Astellas Pharma Inc., Chugai Pharmaceutical Co. Ltd., Eisai Co. Ltd., Mitsubishi Tanabe Pharma Co., Ono Pharmaceuticals, Takeda Pharmaceutical Co. Ltd., and UCB Japan. Kenji Ikeda has received speaking fees or honoraria from Sumitomo Dainippon Pharma Co. Ltd. and Eisai Co. Ltd. Masamitsu Nakao, Nobuaki Nakayama, Sumiko Nagoshi, Akio Ido, Toshihide Mimura, Hiroshi Kaneko, Tetsuya Tsuchida, Hiromichi Suzuki, Nobuyuki Ura, Yuichi Nakamura, Masami Bessho, Kazuo Dan, Shigeo Kusumoto, Yasutsuna Sasaki, Hirofumi Fujii, Fumitaka Suzuki, Hiroko Kobayashi, Kazuhiko Yamamoto, Hajime Takikawa, and Hirohito Tsubouchi have no conflict of interest directly relevant to the content of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mochida, S., Nakao, M., Nakayama, N. et al. Nationwide prospective and retrospective surveys for hepatitis B virus reactivation during immunosuppressive therapies. J Gastroenterol 51, 999–1010 (2016). https://doi.org/10.1007/s00535-016-1168-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-016-1168-2