Abstract
Background
Most studies evaluating visceral sensation measure visceromotor response (VMR) to colorectal distention (CRD). However, CRD itself induces visceral sensitization, and little is known about the detailed characteristics of this response. The present study tried to clarify this question.
Methods
VMR was determined by measuring abdominal muscle contractions as a response to CRD in rats. The CRD set consisted of two isobaric distentions (60 mmHg for 10 min twice, with a 30-min rest), and the CRD set was performed on two separate days, i.e., days 1 and 3, 8.
Results
On day 1, VMR to the second CRD was increased as compared with that to the first CRD, which is the acute sensitization. VMR to the first CRD on day 3 returned to the same level as that to the first CRD on day 1, and total VMR, i.e., the whole response to the CRD set, was not different between day 1 and day 3. However, total VMR was significantly increased on day 8 as compared with that on day 1, suggesting CRD induced the delayed sensitization. Intraperitoneally administered astressin (200 µg/kg), a corticotropin-releasing factor receptor antagonist, at the end of the first CRD blocked the acute sensitization, but anakinra (20 mg/kg, intraperitoneally), an interleukin-1 receptor antagonist, did not modify it. Astressin (200 µg/kg, twice before CRD on day 8) did not alter the delayed sensitization, but anakinra (20 mg/kg, twice) abolished it.
Conclusions
CRD induced both acute sensitization and delayed sensitization, which were mediated through peripheral corticotropin-releasing factor and interleukin-1 pathways, respectively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Irritable bowel syndrome (IBS) is characterized by chronic abdominal pain or discomfort with altered defecation, and abnormality of gut motility and visceral sensation play an important role in the generation of symptoms [1]. Stress has been recognized as an important factor in the pathophysiology. Namely, it alters the colonic functions [2] and frequently exacerbates the symptoms of IBS [3]. Corticotropin-releasing factor (CRF) is a main mediator of the stress responses [4], and central and peripheral CRF receptors are involved in the stress-induced alterations of colonic functions [2].
Many studies have been conducted to evaluate the visceral sensation in order to explore the pathogenesis of IBS. The method adopted by the most of these studies relies on monitoring visceromotor response (VMR) to colorectal distention (CRD). However, CRD itself alters VMR [5–7], even though it is performed for the purpose of measuring VMR. A lot of studies demonstrated that stress such as restraint and water avoidance stress modifies VMR [8, 9], but it is important to note that the changes in VMR detected in these stress models may include those induced by CRD itself.
Therefore, knowledge of the precise mechanisms and characteristics of CRD-induced altered visceral sensation is fundamental for conducting experiments measuring VMR to CRD. Although it was reported that repetitive CRD induces enhanced VMR, which is mediated through peripheral CRF receptors [6, 10], little is known about the precise mechanisms, and it is not clear how long it continues.
In the present study, first we tried to determine the duration of CRD-induced hypersensitivity in rats. CRD was applied to the same rats on two separate days, i.e., days 1 and 3, 8, or 15 in order to clarify the duration of CRD-induced hypersensitivity. In these experiments, we obtained another new finding that CRD also induced delayed onset of hypersensitivity. In other words, CRD induced two different types of sensitization: acute sensitization and delayed sensitization. Then we tried to determine the mechanisms of these responses.
As described above, CRD may activate peripheral CRF signaling. Several studies demonstrated that peripheral CRF increases colonic permeability [11, 12], thereby contributing to the development of inflammatory processes [13]. Circulating levels of proinflammatory cytokines, including interleukin (IL)-1β, are increased in IBS patients [14], and peripheral administration of IL-1β induces visceral allodynia in rats [15]. Therefore, peripheral CRF and IL-1 signaling may contribute to visceral sensitization and the pathophysiology of IBS. In this context, we evaluated the role of peripheral CRF and IL-1 signaling in these responses.
Materials and methods
Animals
Experiments were conducted in adult male Sprague Dawley rats weighing about 250 g. Rats were housed in group cages (three to four rats per cage) in a temperature-regulated room (23–25 °C) under controlled light/dark conditions (lights on from 7 a.m. to 7 p.m.) with free access to standard rat chow (solid rat chow, Oriental Yeast, Tokyo, Japan) and tap water. Experiments started between 8 a.m. and 3 p.m., and finished no later than 4 p.m.
Chemicals
The recombinant human IL-1 receptor antagonist anakinra (Swedish Orphan Biovitrum, Stockholm, Sweden) and IL-1β (Wako Pure Chemical Industries, Osaka, Japan) were dissolved in normal saline. Astressin, a CRF receptor antagonist (Sigma-Aldrich, St Louis, MO, USA), was dissolved in double-distilled water. All drugs were administered though the intraperitoneal route. Girard et al. [16] reported that lipopolysaccharide (LPS)-induced cytokine expression in rat placenta was dose-dependently inhibited by intraperitoneally administered anakinra at doses of 2–20 mg/kg. Moreover, we previously showed that intraperitoneally administered anakinra (20 mg/kg) blocked LPS-induced suppressed gastric contractility in rats [17]. In addition, we demonstrated that astressin (200 µg/kg, intraperitoneally) successfully blocked CRD-induced visceral sensitization, and IL-1β (10 µg/kg, intraperitoneally administered) is known to induce visceral allodynia in rats [15]. The doses of the chemicals used in the present study were selected according to the above-mentioned evidence.
Measurement of visceral sensation
Visceral pain in response to CRD was assessed by abdominal muscle contractions in conscious rats. The electrodes for measuring the muscle contractions electrophysiologically were acutely implanted on the day of the experiment.
Implantation of electrodes and balloon placement
The rats were trained to the experimental conditions by placing them singly in Bollmann cages for 3 h per day for three consecutive days before the study. On the day of the experiment, under brief ether anesthesia, skin incision about 5 mm in length was made in nonfasted rats. Then the electrodes (Teflon-coated stainless steel, 0.05-mm diameter, MT Giken, Tokyo, Japan) were inserted approximately 2 mm into the left side external oblique musculature through the incision and secured by cyanoacrylate instant adhesive (Aron Alpha, TOAGOSEI, Tokyo, Japan) together with the incised skin. The electrode leads were externalized through this closed incision and threaded through a urethane tube. The distension balloon [a 6-cm-long latex balloon tied around a 4-Fr poly(vinyl chloride) catheter, Atom, Tokyo, Japan] was inserted through the anus with the distal end positioned 1 cm proximal to the anus. The balloon was fixed in place by taping the catheter to the tail.
CRD and monitoring VMR
After completion of the manipulation for electrode implantation and balloon placement, the rats were put in Bollmann cages. Then, electrode leads were connected to a custom-made electromyogram (EMG) amplifier. EMG signals were amplified, filtered (3000 Hz), and digitized by a PowerLab system (AD Instruments, Colorado Springs, CO, USA), and stored by computer software (LabChart 7, AD Instruments). The distention balloon catheter was connected to a pressure amplifier (AP-641G, Nihon Kohden, Tokyo, Japan) via a pressure transducer (TP-400T, Nihon Kohden), and balloon pressure signals were digitized by a PowerLab system. The balloon catheter was also connected to an air-filled 50-ml syringe. After a 60-min period for recovery and stabilization in the cages, the rats were submitted to isobaric CRD caused by inflation of the balloon using the syringe manually. Such an acute preparation was previously validated to study visceral hyperalgesia induced by CRD in rats [6, 10, 18]. The basal area under the curve (AUC) was determined by calculating the AUC of the EMG signal trace for the 10-min period immediately preceding each CRD using LabChart 7. The VMR (µV min) was calculated by subtracting the basal AUC from the AUC during the distension period.
Experimental protocol
We adopted the distention protocol as follows (Fig. 1). A single CRD set consisted of two isobaric distentions (60 mmHg for 10 min twice, with a 30-min rest), which was shown to induce visceral sensitization [5, 6], i.e., VMR to the second CRD is increased as compared with that to the first CRD.
The rats were submitted to colorectal distention (CRD), which consisted of two isobaric distentions (60 mmHg for 10 min twice, with a 30-min rest) on two separate days, such as days 1 and 3, 8, or 15. The abdominal contractions were measured electrophysiologically, and visceromotor response (VMR) was determined by calculating the area under the curve of the trace of the electromyogram (EMG). Total VMR, i.e., the sum of the VMR to the first CRD and the second CRD, was also calculated
First, we determined how long this acute sensitization continues and whether delayed onset of sensitization occurs. In this experiment, the same rats were submitted to the CRD set on two separate days, i.e., days 1 and 3, 8 or 15, and VMR on each day was compared. Next, the effect of drugs on CRD-induced sensitization was determined in order to elucidate the response mechanisms.
In the experiment to reveal the acute sensitization mechanisms, a single CRD set was performed, and drug or vehicle was administered at the end of the first CRD. The percent change in VMR between the first and the second CRD [(VMR to the second CRD)/(VMR to the first CRD) × 100] was calculated, and the effect of the drug was determined.
In addition, in the experiment regarding the delayed sensitization, the CRD set was performed on two separate days. Total VMR, i.e., sum of the VMR to the first CRD and the second CRD in each CRD set and the percent change in total VMR to the CRD set between day 1 and the later day [(total VMR to the CRD set on the later day)/(total VMR to the CRD set on day 1) × 100] were calculated. Drug or vehicle was administered twice, 18 and 1 h prior to the later CRD set in order to reveal the mechanisms.
Colonic tissue damage assessment
To assess whether repeated CRD induces colonic tissue damage, four rats underwent two CRD sets on days 1 and 8, and control rats subjected to balloon placement but without CRD were prepared for the analysis. The rats underwent whole perfusion fixation before tissue sampling as described previously [19], with a minor modification. The rats were anesthetized with a ketamine–xylazine mixture, and the heart was exposed by thoracotomy. A perfusion needle was inserted into the ascending aorta through an apical left ventricle puncture, and the right atrium was incised. Then, 300 ml of 4 % paraformaldehyde phosphate buffer solution (Wako Pure Chemical Industries, Osaka, Japan) was perfused into the rats for about 15 min at room temperature. Next, the distal colon tissues were removed and further fixed by overnight immersion in the fixative at 4 °C. They were embedded in paraffin wax, sectioned (4 µm), stained with hematoxylin and eosin, and examined by light microscopy. The presence of colonic wall damage and inflammatory cells was assessed.
Statistical analysis
Data were expressed as the mean ± the standard error. Multiple comparison was performed by one-way repeated measures analysis of variance or one-way analysis of variance followed by Fisher’s least-significant-difference test. Comparison between two groups was performed using Student’s t or the paired t test. SYSTAT 13 (Systat Software, Chicago, IL, USA) was used throughout the study.
Ethical considerations
Approval by the Research and Development Committee and the Animal Care Committee of Asahikawa Medical University (no. 11042, approved on March 7, 2011) was obtained for all studies.
Results
CRD-induced acute sensitization was no longer observed after 48 h
On day 1, the initial CRD set was performed, and VMR to the second CRD was significantly higher than that to the first CRD (F = 8.2, p < 0.05, 67.8 ± 3.5 µV min for first CRD vs 98.0 ± 4.7 µV min for second CRD, n = 8, p < 0.05; Fig. 2a), which is consistent with previous studies demonstrating that CRD induces acute sensitization in rats [5, 6]. The same rats were submitted to the same CRD set on day 3, i.e., 48 h after the initial CRD set, and this acute sensitization was observed again (58.3 ± 8.2 µV min for the first CRD vs 85.3 ± 13.7 µV min for the second CRD, p < 0.05). However, VMR to the first CRD on day 3 was significantly reduced as compared with that to the second CRD on day 1, and returned to the same level as that to the first CRD on day 1. These results indicated that acute sensitization no longer continued after 48 h from the last CRD set.
a Visceromotor response (VMR) to the second colorectal distention (CRD) on day 1 was significantly higher than that to the first CRD on day 1, which was the acute sensitization. However, VMR to the first CRD on day 3 returned to the same level as that to the first CRD on day 1, indicating that this acute response disappeared within 2 days. The acute sensitization was also detected on days 3 and 8. Each column represents the mean ± the standard error. Asterisk p < 0.05 versus VMR to the respective first CRD, pound sign p < 0.05 versus VMR to the second CRD on day 1, cross p < 0.05 versus VMR to the first CRD on day 1. b Total VMR was not different between days 1 and 3, but it was increased on day 8. Since VMR to the first CRD on day 8 was significantly higher than that on day 1 (see a), increased total VMR on day 8 did not result from enhanced response of the acute sensitization, indicating that CRD induced delayed sensitization. This response was no longer observed on day 15. Asterisk p < 0.05 versus total VMR on day 1
In a separate experiment, VMR to the second CRD was significantly increased as compared with that to the first CRD on day 8 (F = 12.2, p < 0.05, 103.6 ± 10.4 µV min for the first CRD vs 134.0 ± 6.4 µV min for the second CRD, n = 12, p < 0.05). Moreover, VMR to the first CRD on day 8 was also greater than that to the first CRD on day 1 (vs 67.0 ± 12.3 µV min for the first CRD on day 1, p < 0.05). On the other hand, the acute sensitization was not detected on day 15 (83.1 ± 16.3 µV min for the first CRD vs 86.8 ± 15.7 µV min for the second CRD, n = 8, p > 0.05).
CRD induced the delayed sensitization 7 days after the last CRD
Total VMR was not different between days 1 and 3 (165.8 ± 8.3 µV min for day 1 vs 143.7 ± 21.8 µV min for day 3, p > 0.05; Fig. 2b). On the other hand, it was significantly increased on day 8 as compared with that on day 1 (157.1 ± 16.5 µV min for day 1 vs 237.6 ± 26.9 µV min for day 8, p < 0.05). Because VMR to the first CRD was significantly higher on day 8 than on day 1 as described earlier (Fig. 2a), increased total VMR on day 8 did not result from enhanced response of the acute sensitization, suggesting that CRD induced another type of visceral hypersensitivity response, such as delayed sensitization. We also determined VMR on days 1 and 15, and found total VMR was not different between these days (150.7 ± 24.7 µV min for day 1 vs 169.9 ± 31.7 µV min for day 15, p > 0.05), indicating that this response disappeared within 2 weeks.
Manipulation related to the measuring VMR did not induced the delayed sensitization
Next, to further confirm that CRD induces the delayed sensitization, the rats underwent manipulation only related to measuring VMR, i.e., anesthesia, skin incision, electrode implantation, and balloon insertion without CRD on day 1, and VMR was measured on day 8. These rats were placed in Bollmann cages for 3 h per day for three consecutive days before the manipulation on day 1 and measurement on day 8 as for controls. Controls underwent two CRD sets on days 1 and 8.
Total VMR of the manipulation-only rats was 136.2 ± 18.8 µV min (n = 6), which was significantly smaller than that of the respective controls on day 8 (F = 10.0, p < 0.05, 214.4 ± 12.8 µV min, n = 8, p < 0.05; Fig. 3) and comparable to that of controls on day 1 (140.9 ± 11.8 µV min). These results showed that the manipulation did not contribute to the delayed sensitization and that CRD definitely induced this response.
Manipulation related to measuring visceromotor response (VMR) to colorectal distention (CRD) on day 1 did not induce the delayed sensitization on day 8. Each column represents the mean ± the standard error. Asterisk p < 0.05 versus total VMR on day 1, pound sign p < 0.05 versus total VMR on day 8 in controls
The delayed sensitization was abolished by anakinra but not by astressin
Next, the delayed sensitization mechanism was evaluated. Astressin (200 µg/kg, twice before CRD on day 8) did not modify this response (change in total VMR between day 1 and day 8, 153.3 ± 18.2 % for vehicle, n = 7, vs 138.0 ± 6.5 % for astressin, n = 5, p > 0.05; Fig. 4).
Anakinra abolished the delayed sensitization but astressin did not modify the response. The same rats were submitted to the colorectal distention (CRD) set on days 1 and 8, and the percent change in total visceromotor response to the CRD set was determined. Vehicle or drug was administered twice, 18 and 1 h prior to the CRD set on day 8. Each column represents the mean ± the standard error.The number of rats examined is shown in parentheses. Asterisk p < 0.05 versus the vehicle-treated group
On the other hand, anakinra (20 mg/kg, twice before CRD on day 8) abolished the response (change in total VMR between day 1 and day 8, 147.8 ± 17.9 % for vehicle, n = 7, vs 102.1 ± 6.7 %, n = 7, p < 0.05), suggesting that IL-1 pathways contribute to the delayed sensitization.
IL-1β increased VMR
We also tested the effect of IL-1β on VMR to CRD. IL-1β (10 µg/kg) or vehicle was injected 1 h prior to the CRD set. Total VMR was significantly increased as compared with that of the vehicle-treated group (144.2 ± 13.0 µV min for vehicle, n = 11, vs 199.8 ± 16.9 µV min for IL-1β, n = 8, p < 0.05; Fig. 5).
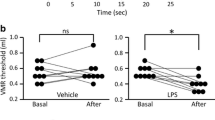
The acute sensitization was blocked by astressin but not by anakinra
Finally, we determined the role of CRF and IL-1 signaling in the acute sensitization. Astressin (200 µg/kg) administered at the end of the first CRD abolished the acute sensitization (change in VMR between the first CRD and the second CRD, 120.1 ± 7.3 % for vehicle, n = 6, vs 95.9 ± 13.2 % for astressin, n = 5, p < 0.05; Fig. 6), which is consistent with our previous study [6].
Astressin abolished the acute sensitization but anakinra did not modify it. A single colorectal distention (CRD) set was performed and vehicle or drug was administered at the end of the first CRD. The percent change in visceromotor response between the first CRD and the second CRD was determined. Each column represents the mean ± the standard error. The number of rats examined is shown in parentheses. Asterisk p < 0.05 versus the vehicle-treated group
Anakinra (20 mg/kg) administered at the end of first CRD did not alter the sensitization (change in VMR between the first CRD and the second CRD, 122.7 ± 7.9 % for vehicle, n = 6, vs 121.4 ± 4.6 % for anakinra, n = 9, p > 0.05). Moreover, anakinra at the same dose twice 18 and 1 h prior to the CRD set did not alter the response either (change in VMR between the first CRD and the second CRD, 132.0 ± 8.1 % for vehicle, n = 9, vs 128.2 ± 9.0 % for anakinra, n = 10, p > 0.05). Total VMR was not different between the anakinra and vehicle groups (159.0 ± 12.2 µV min for vehicle vs 153.7 ± 20.0 µV min for anakinra, p > 0.05).
Repeated CRD did not produce colonic tissue damage
Histological analysis did not detect any differences in colonic wall structure and the presence of inflammatory cells (Fig. 7).
Discussion
We reconfirmed the finding that CRD induces the acute sensitization and showed that it disappeared within 48 h. It is of interest that VMR was enhanced again after 7 days from the last CRD set, i.e., delayed sensitization. Since manipulation associated with the placement of EMG electrodes did not induce this sensitization, this response was thought to result from CRD itself. We measured VMR only on days 1 and 3, 8, or 15, and therefore additional experiments to determine more accurately the onset or duration of the delayed sensitization are needed. In any event, to our knowledge, this is the first report showing CRD induces delayed visceral hypersensitivity. Several studies have adopted experimental protocols involving several CRD sets on different days in order to evaluate the mechanisms of chronic or repeated stress-induced altered visceral sensation [20, 21]. Our results may raise caution in interpreting the results obtained by these experiments, because CRD itself may induce the delayed hypersensitivity.
The present finding that intraperitoneally administered astressin poorly penetrating the brain [22] blocked the acute sensitization strongly suggested that CRD activates peripheral CRF signaling to induce this response. A couple of studies have shown that peripheral injection of cortagine, which is a CRF receptor subtype 1 agonist, induces visceral hyperalgesia within 30 min of injection of this peptide in rats [6, 12], indicating stimulating peripheral CRF pathways displays a rapid response, which is consistent with the notion above. With regard to the mechanisms, peripheral CRF signaling is thought to modulate visceral sensation directly through acting visceral afferent neurons [23] and/or indirectly through stimulating the release of mediators such as serotonin from enterochromaffin cells [24] and mast cells [25], leading to activation of afferents to induce acute sensitization. As described above, astressin does not penetrate the brain, but it may affect the brain through circumventricular organs, which are relatively unprotected by the blood–brain barrier. In this context, the contribution of central CRF signaling to CRD-induced visceral sensitization cannot be denied completely.
The present study also showed that the acute sensitization occurred not only on day 1, but also on days 3 and 8, but it was not detected on day 15, the reason for which is not known. Aging of rats may alter responsiveness to stress [26], which may be a possible explanation.
On the other hand, administration of astressin before the measurement of day 8 did not block the delayed sensitization, suggesting a CRF-independent mechanism for the delayed sensitization. The most important point of the present study is this delayed sensitization was completely blocked by pretreatment with anakinra before the CRD set on day 8. This result indicates that it may be mediated through IL-1 pathways, suggesting that inflammatory processes may engage in this phenomenon. We microscopically evaluated the colonic tissue of rats that underwent CRD, but neither tissue damage nor inflammatory changes were found. CRD with higher intensity (80 mmHg for 30 s with a 90-s rest for 2 h or 80 mmHg for 20 s with a 60-s rest, 15 times for six consecutive days) was reported to induce colonic plasma extravasation, or to increase the numbers of neutrophils, eosinophils, and intraepithelial lymphocytes in muscularis mucosae, suggesting colonic inflammation [7, 27]. This fact suggests that a significant CRD intensity is needed to induce histological changes, but even a lower intensity of CRD as in this study might induce minor inflammation without histological abnormalities, leading to activation of IL-1 signaling. Although the mechanisms involved in CRD-induced inflammatory processes remain unknown, repeated CRD might induce ischemia and reperfusion of colonic wall, which is known to increase the production of IL-1β [28]. That may be a possible explanation.
With regard to the mechanisms by which IL-1 signaling plays a role in the control of visceral sensation, increasing evidence has been reported as follows. Coelho et al. [15] demonstrated that intraperitoneally administered IL-1β induces rectal allodynia in rats, and we also showed in this study that it induces hyperalgesia. There are several studies suggesting possible mechanisms for IL-1-induced visceral sensitization. IL-1 immunoreactive nerve fiber afferents are located in the abdominal visceral organs and the celiac–superior mesenteric ganglion complex of rats [29]. In addition, peripheral administration of IL-1β stimulates abdominal visceral afferents [30]. It follows from these lines of evidence that peripheral IL-1 may activate visceral afferents, causing visceral sensitization.
Although peripheral administration of anakinra blocked the delayed sensitization, involvement of central IL-1 pathways cannot be denied for the following reasons. Several studies showed that anakinra can penetrate the brain [31, 32]. Greenhalgh et al. [31] demonstrated that a single subcutaneous injection of anakinra (100 mg/kg) increased the concentration of cerebrospinal fluid. It is also known that LPS induces rectal allodynia mediated through brain IL-1β, and moreover, intracerebroventricular administration of IL-1β induces rectal allodynia in rats [33]. Thus, not only peripheral but also central IL-1 may be involved in the control of visceral sensation.
Our study has several limitations. The barostat system with the high-compliance polyethylene bag which can provide a constant pressure is thought to be reliable to measure visceral sensitivity, but we used a latex balloon which was inflated by a syringe. There is a report indicating the different rectal thresholds between the bag and the balloon in humans [34]. This issue, therefore, might modify the main results presented in our study. Additionally, CRD did not induce significant tissue damage or inflammatory response, but hematoxylin and eosin staining may not be a perfect staining to detect immune activation. Moreover, the delayed sensitization was not blocked by astressin, but there is a possibility that the dose of the antagonist and the timing of its administration might be inappropriate for blocking CRF signaling. Further studies are warranted to clarify these issues.
There is growing evidence suggesting the importance of the gut immune system in the pathogenesis of IBS. In particular, recent clinical studies demonstrated that a subset of IBS patients display low-grade inflammation in the intestinal mucosa without macroscopic abnormal findings [35, 36]. Moreover, circulating levels of proinflammatory cytokines such as IL-1β, IL-6, and TNF-α are increased [14]. Therefore, the delayed hypersensitivity induced by CRD, which is IL-1 dependent without pathological abnormality of the colon, might be a new stress model mimicking IBS pathogenesis.
In summary, we demonstrated that CRD induced both acute and delayed visceral sensitization, which were mediated through peripheral CRF and IL-1 pathways, respectively. The delayed visceral sensitization without apparent pathological changes might help us understand the pathophysiology of postinfectious IBS patients with visceral hypersensitivity at late onset [37].
References
Lee YJ, Park KS. Irritable bowel syndrome: emerging paradigm in pathophysiology. World J Gastroenterol. 2014;20:2456–69.
Taché Y, Martínez V, Wang L, et al. CRF1 receptor signaling pathways are involved in stress-related alterations of colonic function and viscerosensitivity: implications for irritable bowel syndrome. Br J Pharmacol. 2004;141:1321–30.
Tanaka Y, Kanazawa M, Fukudo S, et al. Biopsychosocial model of irritable bowel syndrome. J Neurogastroenterol Motil. 2011;17:131–9.
Owens MJ, Nemeroff CB. Physiology and pharmacology of corticotropin-releasing factor. Pharmacol Rev. 1991;43:425–73.
Million M, Zhao JF, Luckey A, et al. The newly developed CRF1-receptor antagonists, NGD 98-2 and NGD 9002, suppress acute stress-induced stimulation of colonic motor function and visceral hypersensitivity in rats. PLoS One. 2013;8:e73749.
Nozu T, Takakusaki K, Okumura T. A balance theory of peripheral corticotropin-releasing factor receptor type 1 and type 2 signaling to induce colonic contractions and visceral hyperalgesia in rats. Endocrinology. 2014;155:4655–64.
Saito-Nakaya K, Hasegawa R, Nagura Y, et al. Corticotropin-releasing hormone receptor 1 antagonist blocks colonic hypersensitivity induced by a combination of inflammation and repetitive colorectal distension. Neurogastroenterol Motil. 2008;20:1147–56.
Ait-Belgnaoui A, Bradesi S, Fioramonti J, et al. Acute stress-induced hypersensitivity to colonic distension depends upon increase in paracellular permeability: role of myosin light chain kinase. Pain. 2005;113:141–7.
Schwetz I, Bradesi S, McRoberts JA, et al. Delayed stress-induced colonic hypersensitivity in male Wistar rats: role of neurokinin-1 and corticotropin-releasing factor-1 receptors. Am J Physiol Gastrointest Liver Physiol. 2004;286:G683–91.
Million M, Maillot C, Adelson DA, et al. Peripheral injection of sauvagine prevents repeated colorectal distension-induced visceral pain in female rats. Peptides. 2005;26:1188–95.
Santos J, Saunders PR, Hanssen NP, et al. Corticotropin-releasing hormone mimics stress-induced colonic epithelial pathophysiology in the rat. Am J Physiol Gastrointest Liver Physiol. 1999;277:G391–9.
Larauche M, Gourcerol G, Wang L, et al. Cortagine, a CRF1 agonist, induces stresslike alterations of colonic function and visceral hypersensitivity in rodents primarily through peripheral pathways. Am J Physiol Gastrointest Liver Physiol. 2009;297:G215–27.
Larauche M, Kiank C, Taché Y. Corticotropin releasing factor signaling in colon and ileum: regulation by stress and pathophysiological implications. J Physiol Pharmacol. 2009;60(Suppl 7):33–46.
Liebregts T, Adam B, Bredack C, et al. Immune activation in patients with irritable bowel syndrome. Gastroenterology. 2007;132:913–20.
Coelho AM, Fioramonti J, Bueno L. Systemic lipopolysaccharide influences rectal sensitivity in rats: role of mast cells, cytokines, and vagus nerve. Am J Physiol Gastrointest Liver Physiol. 2000;279:G781–90.
Girard S, Tremblay L, Lepage M, et al. IL-1 receptor antagonist protects against placental and neurodevelopmental defects induced by maternal inflammation. J Immunol. 2010;184:3997–4005.
Tsuchiya Y, Nozu T, Kumei S, et al. IL-1 receptor antagonist blocks the lipopolysaccharide-induced inhibition of gastric motility in freely moving conscious rats. Dig Dis Sci. 2012;57:2555–61.
Gaudreau GA, Plourde V. Involvement of N-methyl-d-aspartate (NMDA) receptors in a rat model of visceral hypersensitivity. Behav Brain Res. 2004;150:185–9.
Gage GJ, Kipke DR, Shain W. Whole animal perfusion fixation for rodents. J Vis Exp. 2012;(65):e3564. doi:10.3791/3564.
Bradesi S, Schwetz I, Ennes HS, et al. Repeated exposure to water avoidance stress in rats: a new model for sustained visceral hyperalgesia. Am J Physiol Gastrointest Liver Physiol. 2005;289:G42–53.
Larauche M, Mulak A, Kim YS, et al. Visceral analgesia induced by acute and repeated water avoidance stress in rats: sex difference in opioid involvement. Neurogastroenterol Motil. 2012;24:1031-e547.
Stengel A, Taché Y. Neuroendocrine control of the gut during stress: corticotropin-releasing factor signaling pathways in the spotlight. Annu Rev Physiol. 2009;71:219–39.
Million M, Wang L, Wang Y, et al. CRF2 receptor activation prevents colorectal distension induced visceral pain and spinal ERK1/2 phosphorylation in rats. Gut. 2006;55:172–81.
Wu SV, Yuan PQ, Lai J, et al. Activation of Type 1 CRH receptor isoforms induces serotonin release from human carcinoid BON-1N cells: an enterochromaffin cell model. Endocrinology. 2011;152:126–37.
Overman EL, Rivier JE, Moeser AJ. CRF induces intestinal epithelial barrier injury via the release of mast cell proteases and TNF-α. PLoS One. 2012;7:e39935.
Chaloner A, Greenwood-Van Meerveld B. Genetic diversity contributes to abnormalities in pain behaviors between young and old rats. Age (Dordr). 2013;35:1–10.
Zhai QZ, Traub RJ. The NMDA receptor antagonist MK-801 attenuates c-Fos expression in the lumbosacral spinal cord following repetitive noxious and non-noxious colorectal distention. Pain. 1999;83:321–9.
Vlachakis IK, Pitoulias GA, Kontopoulou KE, et al. Semapimod a new pretreatment modality of acute intestinal ischemia-reperfusion syndrome: experimental study in rabbits. Int Angiol. 2011;30:35–42.
Schultzberg M, Svenson SB, Unden A, et al. Interleukin-1-like immunoreactivity in peripheral tissues. J Neurosci Res. 1987;18:184–9.
Fu LW, Longhurst JC. Interleukin-1β sensitizes abdominal visceral afferents of cats to ischaemia and histamine. J Physiol. 1999;521(1):249–60.
Greenhalgh AD, Galea J, Denes A, et al. Rapid brain penetration of interleukin-1 receptor antagonist in rat cerebral ischaemia: pharmacokinetics, distribution, protection. Br J Pharmacol. 2010;160:153–9.
Galea J, Ogungbenro K, Hulme S, et al. Intravenous anakinra can achieve experimentally effective concentrations in the central nervous system within a therapeutic time window: results of a dose-ranging study. J Cereb Blood Flow Metab. 2011;31:439–47.
Coelho A, Fioramonti J, Bueno L. Brain interleukin-1β and tumor necrosis factor-α are involved in lipopolysaccharide-induced delayed rectal allodynia in awake rats. Brain Res Bull. 2000;52:223–8.
Sloots CE, Felt-Bersma RJ, Cuesta MA, et al. Rectal visceral sensitivity in healthy volunteers: influences of gender, age and methods. Neurogastroenterol Motil. 2000;12:361–8.
De Giorgio R, Barbara G. Is irritable bowel syndrome an inflammatory disorder? Curr Gastroenterol Rep. 2008;10:385–90.
Kindt S, Van Oudenhove L, Broekaert D, et al. Immune dysfunction in patients with functional gastrointestinal disorders. Neurogastroenterol Motil. 2009;21:389–98.
Beatty JK, Bhargava A, Buret AG. Post-infectious irritable bowel syndrome: mechanistic insights into chronic disturbances following enteric infection. World J Gastroenterol. 2014;20:3976–85.
Acknowledgments
This work was supported in part by Grants-in-Aid from the Ministry of Education, Culture, Sports, Science, and Technology of Japan [C-23590252 (TN), and C-22590753 (TO)].
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nozu, T., Kumei, S., Miyagishi, S. et al. Colorectal distention induces acute and delayed visceral hypersensitivity: role of peripheral corticotropin-releasing factor and interleukin-1 in rats. J Gastroenterol 50, 1153–1161 (2015). https://doi.org/10.1007/s00535-015-1070-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-015-1070-3