Abstract
Background
Endoscopic sphincterotomy (EST) is a standard procedure for the removal of bile duct stones. However, additional EST may increase the risk of bleeding and perforation in patients with prior EST. Endoscopic papillary large balloon dilation (EPLBD) can be an alternative method for removing recurrent common bile duct stones with lower risk of bleeding and perforation. The aim of this study was to evaluate the therapeutic outcomes and complications of EPLBD in patients with recurrent common duct stones who underwent EST previously.
Methods
Between January 2006 and August 2009, 70 patients with recurrent bile duct stones who had a history of EST were studied retrospectively. All patients underwent EPLBD without additional EST to enlarge the ampullary orifice. The size of the balloon for EPLBD was 12–18 mm and the duration of the balloon dilatation was 30–60 s.
Results
Of the 70 patients, there were 24 patients (34.3%) with periampullary diverticula, 18 patients (25.7%) with hypertension, 4 patients (5.7%) with ischemic heart diseases, 2 patients (2.9%) with liver cirrhosis, and 1 patient (1.4%) with chronic kidney disease. Mean diameter of the stones was 12.5 ± 5.5 mm. Complete clearance of the duct was achieved in all patients and mechanical lithotripsy was needed in 1 patient (1.4%). Sixty-eight cases (97.1%) required only 1 session of ERCP to achieve complete ductal clearance. Mild pancreatitis occurred in 1 patient (2.3%), but there was no bleeding or perforation.
Conclusion
EPLBD is an effective and safe method for the treatment of recurrent common duct stones in patients with prior EST.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the introduction of endoscopic sphincterotomy (EST) by Classen and Demling [1] in 1974, EST has become an established method of treatment for cholangiopancreatic diseases, and is most commonly performed to remove common bile duct (CBD) stones. There have been many studies involving the therapeutic benefits, complications, and long-term outcome of EST [2, 3]. The reported frequency of recurrence of choledocholithiasis after EST is 4–24% [3–6]; in most cases, the recurrent stones can be managed by re-EST. However, an endoscopic approach with repeat EST is associated with a higher risk of complications, such as bleeding and perforation [7, 8].
Endoscopic papillary balloon dilation (EPBD) was first introduced in 1983 as an alternative method to EST for the treatment of choledocholithiasis [9]. Although many studies have reported several advantages of EPBD over EST, such as preservation of the sphincter of Oddi function and less bleeding or perforation [10, 11], EPBD is not usually recommended because of the potential risk of severe pancreatitis.
Endoscopic papillary large balloon dilation (EPLBD), combined with limited EST, which was first introduced by Ersoz et al. [12] in 2003, has a lower risk of pancreatitis and encouraging outcomes for the treatment of patients with stones which are difficult to remove [12–16]. We postulated that EPLBD is also a safe and useful method of widening the ampullary orifice in patients with prior EST. No study has reported the therapeutic outcomes of EPLBD in these cases. The aim of this study was to evaluate the therapeutic outcomes, safety, and complications of EPLBD in patients with recurrent CBD stones who had previously undergone EST.
Methods
Between January 2006 and August 2009, 70 patients who underwent EPLBD because of recurrent CBD stones were studied retrospectively. All patients had previously undergone EST to remove CBD stones. Patients with stones smaller than the size of the ampullary opening were excluded in this study. The study protocol was approved by the institutional review board of our center. After conscious sedation with a combination of midazolam and meperidine, ERCP was performed by using a side-viewing endoscope (TJF-160 or TJF-140; Olympus Corp., Tokyo, Japan) by an experienced endoscopist who had performed EST in more than 1,000 cases over 10 years at a rate of more than 1 EST per week.
CBD stones greater than the size of the ampullary opening were identified during ERCP, and the guidewire (0.025–0.035 in. in diameter) was inserted into one of the intrahepatic ducts through a catheter under fluoroscopic guidance. The guidewire was maintained in the left proximal biliary tree, while the diagnostic catheter was removed and exchanged with a dilating balloon catheter (CRE balloon; Boston Scientific Microinvasive, Cork, Ireland). The dilating balloon was advanced over the guidewire and positioned in the mid-portion of the balloon across the major duodenal papilla. The balloon was then inflated gradually with diluted contrast media. In the initial 28 cases, we maintained ballooning for 1 min; in the subsequent 42 cases, the inflation was maintained for 10 s after the waist on the balloon disappeared.
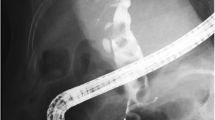
The size of the balloon for EPLBD was 12–18 mm in diameter. We determined the balloon according to the size of the stone, not exceeding 2 mm over the diameter of the distal CBD. CBD stone extraction after EPLBD was performed with either stone retrieval baskets or balloon-tipped catheters (Fig. 1). If the stone was too big to remove intact, mechanical lithotripsy was performed to crush the stone.
EPLBD for recurrent CBD stones. a Endoscopic retrograde cholangiography (ERC) showed several large filling defects in the common bile duct. b, c After the balloon was inflated with diluted contrast media, the waist of the balloon disappeared. d There was a small opening at the ampullary orifice due to previous EST. e Endoscopic view showed that the balloon is advanced over a guidewire and is inflated across the main duodenal papilla. f A widely opened ampullary orifice is observed after balloon dilation
To assess the efficacy and safety of EPLBD, the number and size of CBD stones, the number of sessions to achieve complete duct clearance, complications, and the hospital stay after initial ERCP were evaluated. The number and size of the stones were measured after optimum opacification of the biliary tree. Stone size was estimated based upon the ratio of the diameter of the stone and the shaft of the endoscope. When there were no stones on cholangiogram after stone extraction, we concluded that the stone had been removed completely. Post-ERCP pancreatitis was diagnosed when abdominal pain was present with elevation of serum amylase, and post-ERCP hyperamylasemia was diagnosed when the serum amylase level was elevated without abdominal pain. Post-ERCP bleeding was defined as a bleeding that required endoscopic therapy to control it.
The statistical analysis was performed by using SPSS, version 13.0 (SPSS, Inc., Chicago, IL, USA). All continuous variables were expressed as the mean ± standard deviation (SD).
Results
From January 2000 to August 2009, a total of 1,449 cases of EST were done to remove bile duct stones. Among 1,449 patients, the number of cases with recurrent bile duct stones was 141 cases (9.73%). Seventy cases of the recurrent choledocholithiasis underwent EPLBD between January 2006 and August 2009. Twenty-six cases underwent additional EST and the other 45 cases did not require additional EST or EPLBD for the removal of the recurrent bile duct stones.
Interval between the recurrence of the bile duct stones and previous EST was below 1 year in 20.0%, 1–2 years in 21.4%, 2–3 years in 24.3%, and more than 3 years in 34.3% of the cases (Table 1).
Of the 70 patients who underwent EPLBD, 41 patients were males and 29 patients were females, with mean age of 68.7 ± 12.0 years. Significant co-morbidities were hypertension in 18 patients (25.7%), ischemic heart disease in 4 patients (5.7%), liver cirrhosis in 2 patients (2.9%), and chronic kidney disease in 1 patient (1.4%). Twenty-four patients (34.3%) had periampullary diverticula.
The size of the CBD stones ranged from 5 to 30 mm, with a mean diameter of 12.5 ± 5.5 mm. Forty-two patients (60%) had single stones, and brown pigment stones were noted in 63 of 70 patients (90%; Table 1). The diameter of the balloon for EPLBD was 12 mm in 7 patients (10%), 15 mm in 21 patients (30%), and 18 mm in 42 patients (60%). The duration of balloon inflation was 20–30 s in 30 patients (42.9%) and 60 s in 40 patients (57.1%) including 12 patients who were maintained ballooning for 10 s after waist on the balloon disappeared. CBD stones were extracted with a balloon catheter in 25 patients (35.7%) and a stone retrieval basket in 19 patients (12.9%). In 24 patients (34.3%), both a balloon catheter and basket were necessary to remove the stones (Table 2). The stones were removed successfully during the initial attempt in 68 of 70 patients (97.1%). In 2 patients (2.9%), complete duct clearance was achieved during the second attempt of ERCP without additional EPLBD or EST. Only 1 patient (1.4%) with a concomitant distal CBD stricture required mechanical lithotripsy to remove CBD stones (Table 3).
Endoscopic nasobiliary drainage (ENBD) was performed for 1–3 days to prevent subsequent acute cholangitis in 5 patients who potentially had remnant stones or ampullary edema. The mean hospital stay after the initial ERCP was 6.0 ± 3.8 days.
No significant hemorrhage or perforation occurred after EPLBD, although there was some temporary oozing of blood, which stopped spontaneously. Hyperamylasemia was noted in 7 patients, but clinically apparent pancreatitis developed in only 1 patient; the pancreatitis was mild and improved promptly with conservative treatment (Table 4).
Discussion
EST has been used widely for the non-surgical treatment of choledocholithiasis. Although EST has many advantages, various complications associated with EST have been reported. Acute pancreatitis, hemorrhage, perforation, and acute cholangitis are known to be early complications, and recurrence of stones and papillary stenosis are late complications of EST [2, 17].
EPBD was first described in 1983 as an alternative to EST for facilitation of CBD stone removal [1]. Complications, such as hemorrhage and perforation, are less frequent in EPBD compared with EST. EPBD appears to be effective in patients with coagulopathies or those presenting technical difficulties for EST, such as a Billroth II gastrectomy or a periampullary diverticulum. The incidence of late complications, such as recurrence of choledocholithiasis or papillary stenosis, is expected to be reduced because the function of sphincter of Oddi is likely to be preserved [10, 18]. In spite of these advantages of EPBD over EST, EPBD is not usually recommended for the treatment of choledocholithiasis because there is a potential risk of life-threatening pancreatitis. According to one report, a significant rise in the mortality due to pancreatitis after EPBD was noted [19]. It is presumably associated with impairment of pancreatic flow or damage to the pancreas due to balloon compression.
Recently, there have been reports that EPLBD combined with limited EST has encouraging therapeutic outcomes and safety with a lower risk of complications, including pancreatitis, for the treatment of difficult CBD stones [12–14]. The mechanisms for the decreased incidence of acute pancreatitis after EPLBD in EST are not clear. Obstruction of pancreatic flow may be alleviated because the radial force of balloon inflation is likely to direct toward the CBD which is weaker point because of loss of sphincter muscle rather than toward pancreatic orifice. In addition, pancreatic ductal damage can be decreased because unnecessary selective pancreatic cannulation can be avoided in EST.
There are many reports about the recurrence of CBD stones after EST with a wide range of frequency (4–24%) [3, 4, 6, 20–27]. Most of the recurrent stones are known to be brown pigment stones [28]. Important factors for the pathogenesis of stone recurrence after EST are biliary stasis and bacterial superinfection of the bile. In cases of EST, loss of sphincter function or subsequent papillary stenosis may facilitate ascending infections or bile stasis [29]. This pathogenesis explains why most of the recurrent stones in our study were brown pigment stones. Additional ampullary widening is probably unnecessary to remove recurrent stones after EST because the majority of the stones are brown pigment stones with soft consistency and are easily crushed. However, the procedure time is likely to be prolonged and there is a possibility of remnant stone fragments, which may serve as a nidus for recurrent stones, if mechanical lithotripsy is applied to remove the stones. Therefore, it might be better to remove the stone without fragmentation.
Recurrent bile duct stones are usually managed by repeat EST. Although EST is a safe and feasible method of treatment [27, 30, 31], repeat EST may increase the risk of hemorrhage and perforation. We postulated that the presence of a previous EST was similar to the situation with a limited EST, and EPLBD of this site was safe and effective for the removal of recurrent stones. There are many studies comparing EPLBD with EST, but no data are available about the efficacy of EPLBD in patients with recurrent stones after EST. In our study, endoscopic removal of choledocholithiasis with EPLBD was successful in all patients with no serious complications, and 97.1% of cases required only 1 session of ERCP to achieve complete duct clearance. Ampullary widening with EPLBD was sufficient to remove the stones so that fragmentation of the stones was not necessary in all cases, except 1 patient with a complication (a bile duct stricture).
Although hyperamylasemia developed in 7 patients, there was only 1 case of mild acute pancreatitis, which improved with conservative treatment.
Theoretically, EPLBD is associated with a potential risk of complications, such as bleeding and perforation, especially in cases with a periampullary diverticulum or coagulopathy. However, even though 34.3% of the patients had periampullary diverticula and 10% had a high risk of bleeding, such as liver cirrhosis or chronic kidney disease, EPLBD can be performed safely with no development of bleeding or perforation.
Ballooning exerts radial force on the ampullary area and may cause tearing of weak points, but the junction between the CBD and duodenum may be strong enough not to be injured by ballooning of an appropriate size, so tearing is likely to stop at this point and distension of the ampullary area occurs. Bleeding is another potential complication of EPLBD. Dilation of the ampullary area may injure small blood vessels, but large vessels can be displaced or distended because of their elastic property and can be protected from injury because of the radial force of balloon dilation. In a previous study involving EPLBD combined with a limited EST, and in our study there was very little risk of bleeding or perforation. However, excessive dilatation increased the risk of perforation of the ampullary area and trauma to the large vessels that leads to severe hemorrhage.
In cases with periampullary diverticulum, the high possibility of perforation and bleeding was of concern because the ampullary area is composed of thin mucosa and there is no sphincter muscle in the diverticulum. However, our study demonstrated that EPLBD could be performed safely, even in cases in which the ampulla is located within the large diverticulum.
According to several trials, the bile duct clearance rate of EPLBD is different, ranging from 80 to 100% [9, 32, 33]. Various clearance rates may be due to the difference in the dilating effect of the balloon and characteristics of the stones.
The size of the balloon is the most important factor for achieving adequate ampullary dilatation, as well as preventing complications. The larger the ampullary widening, the easier it is to remove the stones. However, the endoscopist must exercise caution since oversized balloons may cause perforation or vessel injury. In our study, we used various balloon diameters; indeed, an 18-mm balloon was used safely in 65% of the cases. This relatively large ballooning was thought to be safe because we chose the balloon according to the size of the CBD stone and the diameter of the distal part of the CBD, and balloon dilatation was performed under conditions in which the ducts were already dilated over the size of the balloon. There was 1 case that needed mechanical lithotripsy where enough ballooning was not possible because of common bile duct strictures. It is better to avoid excessive dilatation in cases of bile duct strictures to reduce the risk of duct injury.
The duration of balloon inflation for ampullary widening is another factor to consider during EPLBD. Initially, we performed ballooning for about 1 min, but we found that it was sufficient to perform ballooning until notching of the balloon disappeared. It usually took 20–60 s and the ampullary area was adequately enlarged.
In conclusion, we suggest that EPLBD is an effective and safe alternative to EST in patients with recurrent choledocholithiasis after EST. EPLBD might be useful, especially in patients who have a high risk of complications associated with EST, such as diverticuli or bleeding tendencies.
References
Classen ML, Demling L. Endoscopic sphincterotomy of the papilla of the vater and extraction of stones from the choledochal duct. Dtsch Med Wochenschr. 1974;99:496–7.
Cotton PB, Lehman G, Vennes J, Geenen JE, Russel RC, Meyers WC, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383–93.
Ikeda S, Tnanka M, Matsumoto S, Yoshimoto H, Itoh H. Endoscopic sphincterotomy: long-term results in 408 patients with complete follow–up. Endoscopy. 1988;20:13–7.
Bergmann JJ, van der Mey S, Rauws EA, Tijssen JG, Gouma DJ, Tytpat GN, et al. Long-term follow-up after endoscopic sphincteritomy for bile duct stones in patients younger than 60 years of age. Gastrointest Endosc. 1996;44:643–9.
Prat F, Malak NA, Pelletiet G, Buffet C, Fritsch J, Choury AD, et al. Biliary symptoms and complications more than 8 years after endoscopic sphincterotomy for choledocholithiasis. Gastroenterology. 1996;110:894–9.
Tanaka M, Takahata S, Konomi H, Matsunaga H, Yokohata K, Takeda T, et al. Long-term consequence of endoscopic sphincterotomy for bile duct stones. Gastrointest Endosc. 1998;48:465–9.
Leung JWC, Chan FKL, Sung JJY, Chung SCS. Endoscopic sphincterotomy-induced hemorrhage: a study of risk factors and the role of epinephrine injection. Gastrointest Endosc. 1995;42:550–4.
Geenen J, Vennes JA, Silvis SE. Resume of a seminar on endoscopic retrograde sphincterotomy. Gastrointest Endosc. 1981;27:31–8.
Staritz M, Ewe K, Meyer zum Buschenfelde KH. Endoscopic papillary dilatation (EPD) for the treatment of common bile duct stones and papillary stenosis. Endoscopy. 1983;15:197–8.
Sato H, Kodama T, Takaaki J, Tatsumi Y, Maeda T, Fujita S, et al. Endoscopic papillary balloon dilatation may preserve sphincter of Oddi function after common bile duct stone management: evaluation from the viewpoint of endoscopic manometry. Gut. 1997;41:541–4.
Komatsu Y, Kawabe T, Toda N, Ohashi M, Isayama M, Tateishi K, et al. Endoscopic papillary balloon dilatation for the management of common bile duct stones: experience of 226 cases. Endoscopy. 1998;30:12–7.
Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilatation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003;57:156–9.
Meydeo A, Bhandari S. Balloon sphincteropalsty for removing difficult bile duct stones. Endoscopy. 2007;39:958–61.
Minami A, Hirose S, Nomoto T, Hayakawa S. Small sphincterotomy combined with papillary dilation with large balloon permits retrieval of large stones without mechanical lithotripsy. World J Gastroenterol. 2007;13:2179–82.
Kim GH, Kang DH, Song GA, Heo J, Park CH, Ha TI, et al. Endoscopic removal of bile-duct stones by using a rotatable papillotome and a large-balloon dilator. Gastrointest Endosoc. 2008;67:1134–8.
Espinel J, Pinedo E, Olcoz JL. Large hydrostatic balloon for choledocholithiasis. Rev Esp Enferm Dig. 2007;99:33–8.
Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Darsher PJ, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909–18.
Minami A, Nakatsu T, Uchida N, et al. Papillary dilatation vs sphincterotomy in endoscopic removal of bile duct stonesa randomized trial with manometric function. Dig Dis Sci. 1995;40:2550–4.
Disario JA, Freeman ML, Bjorkman DJ. Endoscopic balloon dilatation comparedwith sphincterotomy for extraction of bile duct stones. Gastroenterology. 2004;127:1291–9.
Rösch W, Rienmann JF, Lux G, Linder HG. Long-term follow-up after endoscopic sphincterotomy. Endoscopy. 1981;13:152–3.
Riemann JF, Lux G, Förster P, Altendorf A. Long-term results after endoscopic papillotomy. Endoscopy. 1983;15:165–8.
Escourrou J, Cordova JA, Lazorthes F, Frexinos J, Ribet A. Early and late complications after endoscopic sphincterotomy for biliary lithiasis with and without the gall bladder “in situ”. Gut. 1984;25:598–602.
Jacobsen O, Matzen P. Long-term follow-up study of patients after endoscopic sphincterotomy for choledocholithiasis. Scand J Gastroenterol. 1987;22:903–6.
Seifert E. Long-term follow-up after endoscopic sphincterotomy (EST). Endoscopy. 1988;20:232–5.
Ingoldby CJ, El-Saadi J, Hall RI, Denyer ME. Late results of endoscopic sphincterotomy for bile duct stones in elderly patients with gall bladders in situ. Gut. 1989;30:1129–31.
Hawes RH, Cotton PB, Vallon AG. Follow-up 6 to 11 years after duodenoscopic sphincterotomy for stones in patients with prior cholecystectomy. Gastroenterology. 1990;98:1008–12.
Pereira-Lima JC, Jakobs R, Winter UH, Benz C, Martin WR, Admek HE, et al. Long-term results (7 to 10 years) of endoscopic papillotomy for choledocholithiasis. Multivariate analysis of prognostic factors for the recurrence of biliary symptoms. Gastrointest Endosc. 1998;48:457–64.
Kim DI, Kim MH, Lee SK, Seo DW, Choi WB, Park HJ, et al. Risk factors for recurrence of primary bile duct stones after endoscopic biliary sphincterotomy. Gastrointest Endosc. 2001;54:42–8.
Gregg JA, De Girolami P, Carr-Locke DL. Effects of sphincteroplasty and endoscopic sphincterotomy on the bacteriologic characteristics of the common bile duct. Am J Surg. 1985;149:668–71.
Sugiyama M, Atomi Y. Risk factors predictive of late complications after endoscopic sphincterotomy for bile duct stones: long-term (more than 10 years) follow-up study. Am J Gastroenterol. 2002;97:2763–7.
Mavrogiannis C, Liatsos C, Papanikolaou IS, Psilopoulous DI, Goulas SS, Romanos A, et al. Safety of extension of a previous endoscopic sphincterotomy: a prospective study. Am J Gastroenterol. 2003;98:72–6.
Mathuna PM, White P, Clarke E, Merriman R, Lenon JR, Growe J. Endoscopic balloon sphincteriplasty (papillary dilatation) for bile duct stones: efficact, sagety, and follow-up in 100 patients. Gastrointest Endosc. 1995;42:468–74.
Bergman JJ, Rauws EA, Fockens P, van Berkel AM, Bossuyt PM, Tijssen JG, et al. Randomized trials of endoscopic balloon dislatation versus endoscopic sphincterotomy for removal of bileduct stones. Lancet. 1997;349:1124–9.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, K.O., Kim, T.N. & Lee, S.H. Endoscopic papillary large balloon dilation for the treatment of recurrent bile duct stones in patients with prior sphincterotomy. J Gastroenterol 45, 1283–1288 (2010). https://doi.org/10.1007/s00535-010-0284-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-010-0284-7