Abstract
Objective
Recently, guidelines for the treatment and prevention of ulcers induced by non-steroidal anti-inflammatory drugs (NSAIDs) were established. This study investigated the association between the current adherence to the guidelines and the incidence of gastric mucosal lesions caused by NSAIDs.
Methods
This study included 254 NSAIDs users (128 regular and 126 on-demand users) who had undergone upper gastrointestinal endoscopy. The patients were characterized as high risk based on the following: age 65 years or older, history of peptic ulcers, concurrent use of corticosteroids or anticoagulants, and high-dose NSAIDs use. Adherence was defined as the prescription of NSAIDs with proton pump inhibitors, prostaglandin analogues, or high-dose histamine 2 receptor antagonists in high-risk NSAIDs user. The severity of gastric mucosal lesions was evaluated using the modified LANZA score (MLS).
Results
Seventy-nine (61.7%) of the regular NSAIDs users and 65 (51.6%) of the on-demand NSAIDs users met our definition of high-risk patients. Adherence in the regular NSAIDs users and on-demand NSAIDs users was 25 (31.7%) and 16 (24.6%), respectively. The incidence of gastric mucosal lesions (MLS ≧ 1) was significantly higher in the nonadherence group than in the adherence group for both regular NSAIDs users (59.3 vs. 28.0%, P = 0.01) and on-demand NSAIDs users (63.3 vs. 25.0%, P = 0.01). Gastric ulcers in the regular NSAIDs users were more frequently observed in the nonadherence group than in the adherence group (29.6 vs. 4.0%, P < 0.01).
Conclusion
Nonadherence was associated with a high prevalence of NSAIDs-induced gastric mucosal lesions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-steroidal anti-inflammatory drugs (NSAIDs) are some of the most frequently prescribed drugs [1]. It was reported that gastroduodenal mucosal damage can be seen on endoscopy in 20–40% of people who take NSAIDs [2]. In the US, it is estimated that 100000 or more people per year are admitted to the hospital because of gastric mucosal lesions caused by NSAIDs, with 15000 or more cases resulting in mortality [3]. A survey by the Japan Rheumatic Foundation demonstrated that 15% of NSAIDs-using rheumatoid patients had some sort of upper gastrointestinal mucosal injury [4]. In a large meta-analysis, the overall relative risk for NSAIDs-induced gastric events in patients taking NSAIDs was approximately 2.4 [5]. However, this relative risk was markedly increased among patients who fell into various high-risk categories [5–7]. Physicians prescribing NSAIDs are therefore presented with two problems: (1) the identification of high-risk patients and (2) the selection of appropriate strategies to prevent peptic ulcer and its complications [8].
Strategies to minimize NSAIDs-related upper gastrointestinal events have been outlined in evidenced-based guidelines [9–11], which have consistently identified certain characteristics of high-risk NSAIDs users based on data from observational studies [12]. Elderly age, prior upper gastrointestinal events, and concurrent use of warfarin have been identified as markers of risk in each of these guidelines based on consistent findings from epidemiologic studies [5]. Some observational studies have identified concurrent corticosteroid use as a risk factor [5, 13], and high-dose NSAIDs use has also been indicated as a risk factor [14–16]. The most common strategy for reducing the occurrence of NSAIDs-related upper gastrointestinal complications is the co-prescription of drugs that protect the gastrointestinal mucosa [17]. Misoprostol [prostaglandin analogues (PAs)] was the first agent approved for the prevention of NSAIDs-related ulceration. Early studies in normal volunteers showed a marked reduction in the incidence of gastroduodenal ulcers in patients receiving NSAIDs in combination with misoprostol compared with those who received NSAIDs and placebo [18–20]. Both high-dose histamine 2 receptor antagonists (H2RAs) and proton pump inhibitors (PPIs) have been shown to be effective in reducing upper gastrointestinal symptoms and preventing new and recurrent endoscopic peptic ulcers [17, 21–24].
In our previous study, orthopedists in Japan were found to prescribe several types of drugs to prevent NSAIDs-associated gastrointestinal events, but only 28.2% of prescriptions followed the guidelines [25]. This study investigate the association between the current adherence to the guidelines for the prescription of NSAIDs based on the medical records of NSAIDs users and the incidence of gastric mucosal lesions caused by NSAIDs.
Methods
Patients
This study included 254 NSAIDs users who had undergone upper gastrointestinal endoscopy in Yodogawa Christian Hospital from April in 2006 to March in 2007. The outpatients who had been prescribed NSAIDs registered in the hospital during the investigation period, and those who had undergone upper gastrointestinal endoscopy were selected using the medical treatment fee database of the hospital. In this study, since we focused on NSAIDs used as analgesics, aspirin that had been prescribed as an anti-platelet was not included among the NSAIDs investigated. Therefore, use of the term “NSAIDs” in this study refers to non-aspirin NSAIDs. The prescribed duration of NSAIDs was not taken into consideration in the selection of candidates. The patients who did not undergo endoscopy during the NSAIDs treatment period were excluded. When endoscopy was conducted within 1 month after the last prescription of NSAIDs, it was considered as endoscopy during the treatment period. The NSAIDs were mainly prescribed by physicians and orthopedists. One hundred patients underwent endoscopy because of their symptoms, and the others underwent endoscopy for screening. We examined the medical records of the patients and investigated the patients’ clinical characteristics, including age, sex, symptoms, the types and the duration of NSAIDs, Helicobacter pylori (HP) infection evaluated by rapid urease test, and histopathological examination using biopsy specimens, past history of peptic ulcer, underlying disease, co-prescription of gastric agents, anti-platelets (low dose aspirin, cilostazol, ticlopidine hydrochloride, ethyl icosapentate, beraprost sodium), anti-coagulants (warfarin sodium), and corticosteroids, and the findings of upper gastrointestinal endoscopy. Drug compliance with NSAIDs was not always confirmed using medical records because this study was retrospective.
Definition
The patients were separated into regular NSAIDs users, i.e., patients who were prescribed NSAIDs to be taken regularly, and on-demand NSAIDs users, i.e., patients who were prescribed NSAIDs to be taken only when they had symptoms. We classified the patients into regular NSAIDs users and on-demand NSAIDs users according to how the prescription for NSAIDs was provided before endoscopy. Patients were classified as regular users regardless of the duration of NSAIDs prescription if they received NSAIDs regularly. Patients whose NSAIDs prescription was changed during the investigation period were classified according to the prescription nearest to the endoscopic examination.
Any drugs that were prescribed regularly during the NSAIDs treatment period were defined as co-prescribed drugs. In the on-demand NSAIDs users, the gastric agents prescribed simultaneously with NSAIDs were considered as co-prescription drugs. The patients were divided into five groups according to the prescribed gastric agents: PPIs users, PAs users, H2RAs users, gastroprotective drugs users, and the no gastric agents group.
Patients were characterized as high risk if they fulfilled any of the following criteria: age of 65 years or older, history of peptic ulcers, concurrent use of corticosteroids or anticoagulants, and high-dose NSAIDs use (more than twice the normal dose including the use of two or more kinds or different administration routes of NSAIDs) [10, 16]. In this study, risk factors were taken from evidence-based guidelines issued for Japan [16, 26]. The evidence-based guidelines produced so far vary slightly in their definition of high-risk users [12]; however, history of upper gastrointestinal events, concurrent use of anticoagulants, and advancing age were identified as risk factors in all guidelines [9, 10, 27]. High-dose use of NSAIDs was shown to be an important risk factor [10]. Co-administration of anti-platelets was not regarded as a risk factor although it has been reported that concurrent use of anti-platelet drugs was a risk factor for gastrointestinal bleeding in low-dose aspirin users [28]. Serious systemic disorder was excluded as a risk factor because of its ambiguous definition. Adherence was defined as the prescription of NSAIDs with PPIs, PAs, or high-dose H2RAs in high-risk NSAIDs users.
Endoscopic findings
All endoscopic examinations were digitally recorded. The extent of gastric mucosal injury was expressed in terms of Kobayashi-Mizushima’s modified Lanza score (MLS) [29–32]. We excluded the patients who were suffering from gastric cancer or had undergone a stomach operation. We validated the gastric mucosal lesions and gastric ulcers in the adherence and nonadherence groups. Gastric ulcer was defined as a lesion ≧3 mm in diameter with significant depth [33]. All endoscopic findings were evaluated by the first author’s review in a blind manner after having collected all patient data.
Statistical analysis
To evaluate the differences between the drugs prescribed for the prevention of NSAIDs-induced gastric events between the high-risk and low-risk patients, we used the χ 2 test. We compared the MLS of adherence with that of nonadherence using the Mann–Whitney test. To evaluate the differences between the incidences of gastric mucosal lesions and gastric ulcers in the adherence and nonadherence groups, we used the χ 2 test. Analyses were performed using the STATA/SE statistical software system.
Results
Patients’ background
Of the 254 patients enrolled in this study, 120 were male and 134 were female. The mean age was 60 (15–90). Thirty patients (11.8%) had a past history of gastric ulcers. One hundred twenty-one patients (47.6%) had underlying orthopedic disease. Regarding underlying painful diseases in the regular NSAIDs users, rheumatoid arthritis was present in 29 patients (22.7%), lumbago was observed in 14 cases (10.9%), cancer-related pain occurred in 11 cases (8.6%), and osteoarthritis was seen in 10 (7.8%). In the on-demand NSAIDs users, headache was seen in 34 cases (27.0%), postoperative pain was present in 13 cases (10.3%), osteoarthritis was observed in 12 cases (9.5%), and lumbago occurred in 7 cases (5.6%) (Table 1). Co-prescription of anti-platelets, anti-coagulants, bisphosphonates, and corticosteroids were observed in 22 patients (8.7%; low dose aspirin in 12, cilostazol in 3, low dose aspirin and ticlopidine hydrochloride in 3, ticlopidine hydrochloride in 1, low dose aspirin and cilostazol in 1, ethyl icosapentate in 1, beraprost sodium in 1), 11 patients (4.3%), 8 patients (3.1%), and 23 patients (9.1%), respectively. HP infections were evaluated in 51 patients (20.1%), and 37 of them (72.5%) were found to be positive. As for the kind of NSAIDs prescribed, 163 patients (64.2%) were prescribed loxoprofen sodium, 60 (23.6%) were given dicrofenac sodium, 10 (3.9%) were administered sulindac, and 21 (8.3%) were prescribed other drugs. The period of administration of NSAIDs in the regular use patients was as follows: the number of patients who were prescribed the drugs for less than 1 week was 5, the number of patients administered them for more than 1 week and less than 2 weeks was 9, the number of patients who were prescribed for more than 2 weeks and less than 1 month was 37, the number of patients administered them for more than 1 month and less than 1 year was 29, and the number of patients prescribed the drugs for more than 1 year was 48. Co-prescription of PPIs, regular and half-dose H2RAs, gastroprotective drugs, and PAs were observed in 61 patients (24.0%), 37 patients (14.6%; regular-dose in 32, half-dose in 5), 132 patients (52.0%), and 10 patients (3.9%), respectively. Single use of gastroprotective drugs was prescribed in 93 patients (36.6%). Twenty-four patients were co-prescribed PPIs and gastroprotective drugs, 14 were co-prescribed H2RAs and gastroprotective drugs, and 1 was co-prescribed PAs and gastroprotective drugs. Fifty-seven patients (22.4%) were not prescribed any drugs for NSAIDs-related gastric events. There were no patients who were prescribed high-dose H2RAs. Three patients were co-prescribed PPIs and PAs, and one PPIs and H2RAs; they were classified as PPIs users. All gastric agents had been prescribed for the same or longer periods as NSAIDs.
Regular NSAIDs users and on-demand NSAIDs users
There were 128 regular NSAIDs users (50.4%) and 126 on-demand NSAIDs users (49.6%). Sixty-two (48.4%) regular NSAIDs users and 53 (42.1%) on-demand NSAIDs users were over the age of 65. Fourteen (10.9%) regular NSAIDs users and 16 (12.7%) on-demand NSAIDs users had a history of upper gastrointestinal events. Four (3.1%) regular NSAIDs users and 7 (5.6%) on-demand NSAIDs users received concomitant anticoagulant therapy. Eighteen (14.1%) regular NSAIDs users and 5 (4.0%) on-demand NSAIDs users received concomitant corticosteroid treatment. Three patients (2.3%) took a high-dose of NSAIDs. Thirty-two (25.0%) regular NSAIDs users and 29 (23.0%) on-demand NSAIDs users were prescribed PPIs to prevent NSAIDs-induced gastric events. Six (4.7%) regular NSAIDs users and 1 (0.8%) on-demand user were prescribed PAs. In the regular NSAIDs and on-demand users, H2RAs were prescribed in 21 (16.4%) and 15 patients (11.9%), respectively. Gastroprotective drugs were prescribed in 49 (38.3%) regular NSAIDs users and 44 (34.9%) on-demand NSAIDs users. Twenty (16.6%) regular NSAIDs users and 37 (29.4%) on-demand NSAIDs users were not prescribed any drugs for the prevention of NSAIDs-induced gastric events (Table 2).
High-risk patients, adherence patients
In the regular NSAIDs users, 61 patients (47.7%) had 1 risk factor, 14 patients (10.9%) had 2, and 4 patients (3.1%) had 3. Forty-nine patients (38.3%) had no risk factors. In the on-demand NSAIDs users, 51 patients (40.5%) had 1 risk factor, 12 patients (9.5%) had 2, and 2 patients (1.6%) had 3. Sixty-one patients (48.4%) had no risk factors (Table 3). Seventy-nine patients (61.7%) in the regular NSAIDs users and 65 patients (51.6%) in the on-demand NSAIDs users met our criteria for high-risk patients. High-dose H2RAs were not prescribed in any case. There were no significant differences between the high-risk and low-risk patients with regard to the drugs prescribed for the prevention of NSAIDs-induced gastric events both in the regular NSAIDs (P = 0.64) and on-demand NSAIDs users (P = 0.85) (χ2 test). The adherence rate in the regular NSAIDs and on-demand NSAIDs users was 25 (31.7%) and 16 (24.6%), respectively (Table 4).
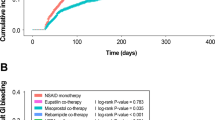
MLS
The MLS of the patients who were co-prescribed PPIs and PAs tended to be low in both the high-risk and low-risk regular NSAIDs users. Similar results were obtained for the on-demand NSAIDs users (Table 5). In a comparison of MLS between adherence and nonadherence, there were significant differences in both the regular NSAIDs users (0.72 vs. 2.33, P < 0.01) and the on-demand NSAIDs users (0.63 vs. 2.02, P < 0.01) (Mann–Whitney test) (Table 6). The incidence of gastric mucosal lesions (MLS ≧ 1) was significantly higher in nonadherence than that in adherence in both regular NSAIDs users [32/54 (59.3%) vs. 7/25 (28.0%), P = 0.01] and on-demand NSAIDs users [31/49 (63.3%) vs. 4/16 (25.0%), P = 0.01]. The incidence of gastric ulcers (MLS = 5) was significantly higher in the nonadherence group than in the adherence group in the regular NSAIDs users [16/54 (29.6%) vs. 1/25 (4.0%), P < 0.01; χ2 test; Fischer’s test] (Table 7). Non-adherent regular NSAIDs users with more than two risk factors had more gastric ulcers (MLS = 5) than those with only one risk factor; however, the difference was not significant [5/13 (38.5%) vs. 11/41 (26.8%), P = 0.32; Fischer’s test].
Discussion
Given the high prevalence of NSAIDs use, particularly among elderly and other high-risk populations, preventing NSAIDs-related gastropathy continues to be an important public health objective [34]. Several sets of guidelines have been published in the US that recommend misoprostol or PPIs and high-dose H2RAs as prophylactic agents for the prevention of NSAIDs-induced ulcers and identified the following risk factors: elderly age, prior upper gastrointestinal events, and concurrent use of warfarin or corticosteroids [9, 10, 27]. In Japan, guidelines for gastric ulcers were also published in 2003 [26] that stated the same risk factors and prophylactic agents. In order to investigate the association between the current adherence to the evidence-based guidelines for the prescription of NSAIDs and the incidence of gastric mucosal lesions caused by NSAIDs, we retrospectively examined the medical records of NSAIDs users who underwent upper gastrointestinal endoscopy. The patients were characterized as high risk if they met any of above risk factors. Adherence was defined as the prescription of NSAIDs with PPIs, PAs, or high-dose H2RAs in high-risk NSAIDs users.
In this study, 61.7% of regular NSAIDs users and 51.6% of on-demand NSAIDs users were shown to be at high risk of developing upper gastrointestinal events. Among these groups, only 31.7% of regular NSAIDs users and 24.6% of on-demand NSAIDs users were prescribed PPIs or PAs. In our previous study using a questionnaire given to orthopedists, we found that PPIs and PAs were prescribed by 10.8 and 17.4% of the orthopedists, respectively, for the prevention of NSAIDs-induced gastrointestinal events [25], which were similar to the results of this study. Recently, it has been reported that adherence to the evidence-based guidelines for the prescription of NSAIDs is low. Suh et al. [34] reported that of 16344 chronic NSAIDs users, 1586 (10%) received at least one PPIs prescription during follow-up. Abraham et al. [12] reported that among the high-risk group only 27.2% received NSAIDs prescriptions that were adherent to the evidenced-based guidelines. Our results were consistent with these reports. In Arakawa’s report, which used a questionnaire in East Asian countries, the most common drugs of first choice for comedication were PPIs (49%) followed by mucoprotective drugs (29%), H2RAs (3%), and PAs (3%) [35].
We evaluated NSAIDs-induced gastric mucosal injury by endoscopic findings using MLS. In a comparison of MLS between the adherence and nonadherence groups, there were significant differences both in the regular NSAIDs (P < 0.01) and the on-demand NSAIDs users (P < 0.01). In both the regular NSAIDs and on-demand NSAIDs users, nonadherence was more strongly associated with gastric mucosal lesions than adherence (P = 0.01, P = 0.01). Moreover, in the regular NSAIDs users, those in the nonadherence group had more gastric ulcers than those in the adherence group (P < 0.01). These results suggest that adherence to evidence-based guidelines is important for the safe prescription of NSAIDs.
However, this study does have limitations because the data were collected retrospectively from NSAIDs users who had undergone upper gastrointestinal endoscopy. In addition, the investigated co-prescribed drugs were limited to co-prescription in Yodogawa Christian Hospital. Some patients might have received co-prescribed drugs in the other hospitals. In this retrospective study, we could not investigate NSAIDs user’s drug compliance. Prospective studies are therefore required to clarify the consequences of nonadherence.
Both HP infection and NSAIDs use independently and significantly increase the risk of peptic ulcer and ulcer bleeding [36]. It is likely that HP infection affected the results in this study; however, HP infection was examined in only 51 patients (20.1%). Therefore, we were not able to consider the involvement of HP infection.
Coté et al. [37] reported that the combination of a computer alert and a brief physician education course improved the use of gastroprotection among high-risk NSAIDs users. It is very important to improve physician awareness of the risk factors for NSAIDs-related gastric events and the necessity of adherence to the guidelines. In the future, construction of an electronic alert system may contribute to an increase in adherence.
In summary, adherence to evidenced-based guidelines for the prevention of NSAIDs-induced gastric mucosal events was found to be low among NSAIDs users who had undergone endoscopy, which corresponded with the results of past studies. Nonadherence was found to be associated with a high prevalence of NSAIDs-induced gastric mucosal lesions. The construction of a system for increasing adherence might be required.
References
Clinard Francois, Bardou Marc, Sgro Catherine, Lefevre Nathalie, Raphael Francis, Paille Francois, et al. Non-steroidal anti-inflammatory and cytoprotective drug co-prescription in general practice. Eur J Clin Pharmacol. 2001;57:737–43.
Taha AS, Hudson N, Hawkey CJ, Swannell AJ, Trye PN, Cottrell J, et al. Famotidine for the prevention of gastric and duodenal ulcers caused by nonsteroidal anti-inflammatory drugs. N Engl J Med. 1996;334:1435–9.
Weil J, Langman MJ, Wainwright P, Lawson DH, Rawlins M, Logan RF, et al. Peptic ulcer bleeding: accessory risk factors and interactions with non-steroidal anti-inflammatory drugs. Gut. 2000;46:27–31.
Shiokawa Y, Nobenaga T, Saitoh T, Asaji S, Ogawa A. Epidemiological study on upper digestive injuries by non-steroidal anti-inflammatory drugs. J Jpn Rheum Assoc. 1991;31:96–111 (in Japanese).
Gabriel SE, Jaakkinmainen L, Bombardier C. Risk for serious gastrointestinal complications related to use of nonsteroidal anti-inflammatory drugs: a meta-analysis. Ann Intern Med. 1991;115:787–96.
Bellary SV, Isaacs PE, Lee FI. Upper gastrointestinal lesions in elderly patients presenting for endoscopy; relevance of NSAID usage. Am J Gastroenterol. 1991;86:961–4.
Fries JF, Williams CA, Bloch DA, Michel DA. Nonsteroidal anti-inflammatory drug-associated gastropathy: incidence and risk factor models. Am J Med. 1991;91:213–22.
Lanza FL, Chan FK, Quigley EM. Guidelines for prevention of NSAID-related ulcer complications. Am J Gastroenterol. 2009;104:728–38.
Recommendation for the medical management of osteoarthritis of the hip and knee. 2000 update. American College of Rheumatology Subcommittee on Osteoarthritis Guidelines. Arthritis Rheum 2000;43:1905–15.
Lanza FL. A guideline for the treatment and prevention of NSAID-induced ulcers: members of the ad hoc committee on practice parameters of the American college of gastroenterology. Am J Gastroenterol. 1998;93(11):2037–46.
MacLean CH. Quality indicators for the management of osteoarthritis in vulnerable elders. Ann Intern Med. 2001;135:711–21.
Abrahama NS, El-Serag HB, Johnson ML, Hartman C, Richardson P, Ray WA, et al. National adherence to evidence-based guidelines for the prescription of nonsteroidal anti-inflammatory drugs. Gastroenterology. 2005;129(4):1171–8.
Smalley WE, Griffin MR. The risks and costs of upper gastrointestinal disease attributable to NSAIDs. Gastroenterol Clin North Am. 1996;25(2):373–96.
Hernandez-Diaz S, Rodriguez LA. Association between nonsteroidal anti-inflammatory drugs and upper gastrointestinal tract bleeding/perforation. Arch Intern Med. 2000;160:2093–9.
Moens HJ, Van Croonenborg JJ, Al MJ, van den Bemt PM, Lourens J, Numans ME, et al. Guideline: ‘NSAID use and the prevention of gastric damage’. Ned Tijdschr Geneeskd. 2003;148:604–8.
Wofe MM, Lichtenstein DR, Singh G. Gastrointestinal toxicity of nonsteroidal anti-inflammatory drugs. N Eng J Med. 1999;340:1888–99.
van Soest EM, Sturkenboom MC, Dieleman JP, Verhamme KM, Siersema PD, Kuipers EJ. Adherence to gastroprotection and the risk of NSAID-related upper gastrointestinal ulcers and haemorrhage. Aliment Pharmacol Ther. 2007;26(2):265–75.
Lanza FL, Fakouhi D, Rubin A, Davis RE, Rack MF, Nissen C, et al. A double-blind placebo-controlled comparison of the efficacy and safety of 50, 100, and 200 micrograms of misoprostol q.i.d. in the prevention of ibuprofen-induced gastric and duodenal mucosal lesions and symptoms. Am J Gastroenterol. 1989;84:633–6.
Targownik LE, Metge CJ, Leung S, Chateau DG. The relative efficacies of gastroprotective strategies in chronic users of nonsteroidal anti-inflammatory drugs. Gastroenterology. 2008;134:937–44.
Lanza FL. A double-blind study of prophylactic effect of misoprostol on lesions of gastric and duodenal mucosa induced by oral administration of tolmetin in healthy subjects. Dig Dis Sci. 1986;31:131–6.
Hawkey C, Talley NJ, Yeomans ND, Jones R, Sung JJ, Langstrom G, et al. Improvements with esomeprazole in patients with upper gastrointestinal symptoms taking non-steroidal anti-inflammatory drugs, including selective COX-2 inhibitors. Am J Gastroenterol. 2005;100:1028–36.
Hooper L, Brown TJ, Elliott R, Payne K, Roberts C, Symmons D. The effectiveness of five strategies for the prevention of gastrointestinal toxicity induced by non-steroidal anti-inflammatory drugs: systematic review. BMJ. 2004;329:948.
Rostom A, Dube C, Wells G, Tugwell P, Welch V, Jolicoeur E, et al. Prevention of NSAID-induced gastroduodenal ulcers. Cochrane Database Syst Rev. 2002;(4):CD002296.
Scheiman JM, Yeomans ND, Talley NJ, Vakil N, Chan FK, Tulassay Z, et al. Prevention of ulcers by esomeprazole in at-risk patients using non-selective NSAIDs and COX-2 inhibitors. Am J Gastroenterol. 2006;101(4):701–10.
Tsumura H, Tamura I, Tanaka H, Chinzei R, Ishida T, Masuda A, et al. Prescription of non steroidal anti-inflammatory drugs and co-prescribed drugs for mucosal protection: analysis of the present status based on questionnaires obtained from orthopedists in Japan. Intern Med. 2007;46:927–31.
EBM ni motozuku ikaiyou shinnryou gaidolain dai2han. NSAID kaiyou yobou. in EBM ni motozuku ikaiyou shinnryou gaidolain. Jihou, 2007 (in Japanese).
Schnitzer TJ, American College of Rheumatology. Update of ACR guidelines for osteoarthritis: role of the coxibs. J Pain Symptom Manage. 2002;23(Suppl 4):S24–30.
Sorensen R, Hansen ML, Abildstrom SZ, Hvelplund A, Torp-Pedersen C, Gislason GH. Risk of bleeding in patients with acute myocardial infarction treated with different combinations of aspirin, clopidogrel, and vitamin K antagonists in Demark: a retrospective analysis of nationwide registry data. Lancet. 2009;374:1967–74.
Naito Y, Yoshikawa T, Iinuma S, Yagi N, Matsuyama K, Boku Y, et al. Rebamipide protects against indomethacin-induced gastric mucosal injury in healthy volunteers in a double-blind, placebo-controlled study. Dig Dis Sci. 1998;43:83–9.
Lanza FL, Royer GL, Nelson RS, Chen TT, Sechman CE, Rack MF. A comparative endoscopic evaluation of the damaging effects of nonsteroidal anti-inflammatory agents on the gastric and duodenal mucosa. Am J Gatroenterol. 1981;75:17–21.
Kobayashi K, Mizushima Y, Yanagawa A, Kasukawa R, Ito J, Koshino T, et al. Prophylactic effects ranitidine, a H2 receptor antagonist, on gastric and duodenal lesions induced by nonsteroidal anti-inflammatory agents. J Adult Dis. 1990;20:253–64 (in Japanese).
Robinson MG, Griffin JW, Bowers J, Kogan FJ, Kogut DG, Lanza FL, et al. Effect on ranitidine on gastroduodenal mucosal damage induced by nonsteroidal anti-inflammatory drugs. Dig Dis Sci. 1989;34:424–8.
Yeomans ND, Naesdal J. Systematic review: ulcer definition in NSAID ulcer prevention trials. Aliment Pharmacol Ther. 2008;27:465–72.
Suh D-C, Hunsche E, Shin H-C, Mavros P. Co-prescribing of proton pump inhibitors among chronic users of NSAIDs in the UK. Rheumatology. 2008;47:458–63.
Arakawa T, Fujiwara Y, Sollano JD, Ahu Q, Kachintorn U, Rani AA, et al. IGIS study group: a questionnaire-based survey on the prescription of non-steroidal anti-inflammatory drugs by physicians in East Asian countries in 2007. Digestion. 2009;79:177–85.
Huang JQ, Sridhar S, Hunt RH. Role of Helicobacter pylori infection and non-steroidal anti-inflammatory drugs in peptic-ulcer disease: a meta-analysis. Lancet. 2002;359:14–22.
Coté GA, Rice JP, Bulsiewicz W, Norvell JP, Christensen K, Bobb A, et al. Use of physician education and computer alert to improve targeted use of gastroprotection among NSAID users. Am J Gastroenterol. 2008;103:1097–103.
Acknowledgments
This study was supported by a grant for the Global COE Program “Global Center of Excellence for Education and Research on Signal Transduction Medicine in the Coming Generation” from the Ministry of Education, Culture, Sports, Science, and Technology of Japan (T.A.).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsumura, H., Fujita, T., Tamura, I. et al. Association between adherence to evidence-based guidelines for the prescription of non-steroidal anti-inflammatory drugs and the incidence of gastric mucosal lesions in Japanese patients. J Gastroenterol 45, 944–951 (2010). https://doi.org/10.1007/s00535-010-0236-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-010-0236-2