Abstract
Purpose
Cancer survivors continue to experience issues that persist across the survivorship trajectory. This study aims to explore the relationship among survivorship care need, symptom experience, and quality of life (QoL) of multiethnic cancer survivors by using path analytic methods.
Methods
Participants were recruited from an academic medical center in Singapore that provides inpatient and outpatient oncology and hematology service. The Cancer Survivor Unmet Needs measure, physical effects subscale of the Cancer Survivors’ Survey of Needs tool, and a Global QoL 10-point Likert scale were used to identify survivorship care needs, symptom experience, and QoL. Descriptive statistics were used to compute sociodemographic information, total survivorship needs, symptom experienced, and quality of life scores. The symptom experience model was used as the hypothetical model. The Analysis of Moment Structure was used to conduct the path analysis to evaluate the relationship between survivorship care needs, symptom experience, and quality of life.
Results
Older cancer survivors were more likely to have spent a longer duration having cancer. Males were unlikely to suffer from solid tumor malignancies. Survivors with solid tumor malignancies were less likely to require supportive care. Survivors who require more supportive care were more likely to have a greater symptom burden. Cancer survivors with more symptoms have poorer QoL. The findings from this study partially supported the symptom experience model.
Conclusions
Our findings reveal that cancer survivors continue to experience symptoms across the survivorship trajectory. The results provide information for nurses during the planning and execution of survivorship care.
Similar content being viewed by others

Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The global burden of cancer continues to rise. The American Cancer Society [1] estimates that the USA would have approximately 20 million cancer survivors by 2026. Singapore also experiences a similar phenomenon; the local National Registry of Diseases Office [2] reported that, with the advances in treatment and early screening, patients with cancer are increasingly surviving for a longer period. As survivors live longer and beyond treatment, their survivorship experiences must be examined. Cancer survivorship is defined by Feuerstein [3] as “individuals with a diagnosis of cancer who have completed primary treatment for cancer.”
Mullan [4] stratifies survivorship into three phases: (1) acute survival, (2) extended survival, and (3) permanent survival. Acute survival extends from diagnosis to initial treatment, where an individual often experiences the consequences of the treatment, i.e., side effects, fear, and anxiety [4, 5]. Among acute survivors with colorectal and lung cancers, older patients have experienced severe and more symptoms [6, 7]. Younger survivors in the acute phase have experienced more survivorship care needs, including managing side effects, symptoms, concerns about cancer recurrence, and emotional support [8]. The effects of gender on symptom experiences varied among different cancer types [6, 7, 9], suggesting that the type of cancer significantly influences symptom experiences [9]. Management of care needs, as a result of treatment, is paramount in the acute phase [5, 10, 11] as poorer symptom control and management negatively affect quality of life (QoL) [6, 7, 12].
As survivors transit into the extended survival phase, they struggle to return to normalcy after treatment completion because of various reasons. The latent effects of platinum-based chemotherapy may lead to peripheral neuropathy, a condition that affects the ability to perform activities of daily living [5]. Survivors with gynecological cancers in the extended phase also reported physical symptoms that are less frequent but severe [12]. Psychological burden because of fear and physical strains resulting from the latent effects of the symptoms can increase the demand for supportive care needs [11, 13, 14]. Furthermore, patients with cancer endure periods of “watchful waiting” for disease recurrence, follow-ups while struggling to navigate the healthcare system, and dealing with finances [10, 15]. Apart from symptoms and frequent hospital visits, patients also reported information about the near future, nutrition, physical activity, and heredity of cancer as essential but lacking during the extended survival phase [16].
Permanent survival is the transition from the extended disease-free survival to a low likelihood of disease return [4]. The change to the “new normal” begins with concerns regarding employment and health promotion [4, 11]. Fear of recurrence and fatigue are lasting concerns across the continuum of survivorship [9, 11]. Each phase of survivorship poses unique concerns based on individual experience and the outcome of initial treatment and subsequent screening [11, 15]. Taylor and Monterosso [15] found that the provision of survivorship care plan and treatment summary is essential in ensuring a smooth transition into survivorship. Survivorship care plans comprise information detailing follow-up care, available resources, and recommended screenings for recurrence. However, the literature exploring the survivorship care needs of patients with cancer in Singapore is inadequate. In addition, better understanding of the survivorship is warranted given the increasing emphasis from the Singapore Ministry of Health to provide quality cancer care.
Demographic variables (age and gender), disease characteristics (type of cancer and duration with cancer), and individual characteristics (survivorship needs) are closely related, can affect symptom experience [6, 7, 9, 13], and are factors in predicting QoL across cancer survivorship [12]. However, only a few studies explored the collective relationships between demographic, disease, and individual variables and symptom experience and QoL among individuals with different cancer types. Thus, this study aims to identify the relationship among demographic variables, survivorship care needs, symptom experience, and QoL of multiethnic cancer survivors by using a path analytic approach. The findings provide an understanding of survivorship needs and can be used in the development of a holistic survivorship care approach to address concerns unique to cancer survivors across their survivorship journey.
Conceptual model
Armstrong [17] describes symptoms as the guidepost for oncology nursing practice. As patients go through their survivorship trajectory, they experience numerous symptoms or concerns of various degrees [4, 10, 15]. Contemporary oncology practice mainly focuses on physical symptoms, particularly during the acute survivorship phase. Hence, the present study adopted Armstrong’s [17] definition of symptoms, that is, the “perception of frequency, intensity, distress, and meaning occurring as symptoms are produced” (p. 602). This definition enables a broader classification of symptoms beyond physical needs but from a meaning-based approach that encapsulates the symptoms experienced during the acute, extended, and permanent survival phases.
The symptom experience model (Fig. 1) is chosen because it takes multiple dimensions, such as (1) demographic (age, gender, race, etc.), (2) disease (type, stage, treatment, etc.), and (3) individual characteristics (knowledge, values, past experiences, sense of coherence, etc.) of an individual into account. The model also describes how patient demographics, disease, and characteristics (antecedents) influence the symptom experience and severity (symptom perception), ultimately affecting outcomes such as QoL. Patient age, ethnicity, and gender relating to disease type, stage, and treatment can influence an individual’s knowledge, values, experience, and sense of coherence. These factors can contribute to symptom experiences of the patients and ultimately affect their QoL. Hence, we proposed six hypotheses (H) according to the symptom experience model.
Hypotheses
-
H1: Patient age, gender, and ethnicity are related to disease characteristics.
-
H2: The type and years with cancer have an effect on a patient’s individual characteristics.
-
H3: The relationship, information, cancer care, QoL, and existential survivorship needs can predict a patient’s experienced symptoms.
-
H4: Patient age, gender, and ethnicity can be used to predict their experienced symptoms.
-
H5: The type and years of cancer can be used to predict a patient’s experienced symptoms.
-
H6: Experienced symptoms can predict patient QoL.
Methods
Study design and participants
A quantitative exploratory design was adopted to examine the survivorship care needs of patients with cancer. The study was conducted in an academic medical center in Singapore with both inpatient and outpatient units that provide chemotherapy, radiotherapy, hematopoietic stem cell transplant, survivorship, and psychosocial care. Participants above 21 years old with a definitive cancer diagnosis and who completed at least one cycle of cancer treatment as determined by their physician, can understand English or Mandarin, and agreed to participate were recruited. Patients with cognitive impairment or at the end of life were excluded. Participants were recruited from the outpatient and inpatient settings from August 2016 to June 2017.
Data collection
Potential patients were identified by their primary physicians or nurses and referred to the researcher who was not a member of a healthcare team that provided direct care; this was done to reduce social desirability bias. The researcher then explained the purpose, nature, and process of the study and obtained written informed consent prior to administering the questionnaires. Participants who refused to participate were also asked for their reasons, which were recorded. Sample size calculation was based on multiple regression and correlation analysis to examine the predictors of unmet needs based on eight variables (age, gender, education, cancer type, treatment type, number of reported symptoms, severity of symptoms, and ethnicity). For a power of 0.80, significance of 0.01, and medium effect size, the sample size needed was 147 [18].
Measures
The patient questionnaire consisted of (1) demographic (age, gender, and marital status) and disease information (cancer diagnosis, years with cancer, type of treatment received), (2) the Cancer Survivor Unmet Needs (CaSUN) measure [19], (3) the physical effects subscale of the Cancer Survivors’ Survey of Needs (CSSN) tool [20], and (4) self-rated Global QoL 10-point Likert scale. The CaSUN aims to directly assess unmet needs of cancer survivors [19] and includes 35 total need items with five subscales. The scale has a 5-point Likert scale that scores an individual’s perception of the need. Items are rated from no unmet need (no need, have need but need is being met) or unmet needs (weak, moderate, or strong). This study measured the total needs of cancer survivors. No need is coded 0, whereas having met need or strength of need is coded 1. The score ranges from 0 to 35, with higher scores indicating greater needs. The scale has good acceptability, internal consistency (Cronbach’s alpha of 0.96), and construct validity [19]. The internal consistency coefficient of the total CaSUN had a Cronbach’s alpha of 0.97. A methodological review of unmet need scales suggested that the CaSUN measure performs well or better than any other measures [21]. The physical effect subscale of CSSN was used to complement the CaSUN in the patient survey [20]. The physical effect subscale consists of a numeric analog scale (0 = no concern, 5 = extreme concern). The CSSN demonstrated good internal reliability with a Cronbach’s alpha of 0.96. Participants were asked to assess their concerns among the 19 physical symptoms on the day of completing the survey. The scores were summed, and a higher score represented a greater concern for that symptom. The Cronbach’s alpha of the scale study was 0.947. A separate QoL 10-point Likert scale, a part of the CSSN tool, was used to understand participants’ perception of their QoL. Participants were asked to rate their QoL on the day of the survey from 0 (poor) to 10 (best), with a higher score indicating better QoL. Ethical approval was obtained from the Singapore National Healthcare Group-Domain Specific Review Board (2016-01023). All participants received study information and provided verbal and written consent.
Statistical analysis
The IBM Statistical Package for Social Sciences (SPSS) version 25.0 (IBM Corporation, Armonk, NY, USA) was used for data analysis. Internal consistencies were used to test the reliability of all scales. Missing data were replaced by expectation-maximization technique in SPSS. Descriptive analysis was performed for demographic and socioeconomic variables. Path analysis was used to test the directional relationships among study variables according to our hypothetical model. Analysis of Moment Structures (AMOS) software version 25.0 was used to perform path analysis for examining the hypothetical path model [22]. The AMOS program tested whether or not the hypothetical model is suitable for the constructs (demographic, disease, individual characteristic, total supportive care need, symptom perception, and QoL), with path diagrams to verify the intensity of effects according to symptom experience model [23]. A correlation matrix for all constructs was developed. Path analysis is a multivariate technique to concede a simultaneous calculation of parameter estimates for intensity of fitting with supposed relations among preliminary hypotheses [24]. Normally distributed data are specifically required when applying full information maximum likelihood in path analysis [24]. The path coefficient estimated the intensity of the causal linkage between two study variables and was analyzed using standardized regression coefficients, i.e., β weight. The full information maximum likelihood estimation method was used to assess parameters to signify population values [23]. The criteria for goodness-of-fit were the following: chi-square (χ2)/degree of freedom (d/f) was < 3, incremental fit index (IFI) > 0.95, comparative fit index (CFI) > 0.95, and root mean square error of approximation (RMSEA) < 0.06 [25, 26].
Results
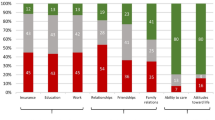
A total of 200 out of 283 eligible patients consented to participate in the study. The response rate was 67.6%. Lack of interest (N = 19), no time (N = 32), and unwell (N = 45) were the reasons of the non-participants. Among 200 participants, 122 (61%) were female, and the mean age was 55.03 (SD = 12.8). Chinese made up the majority of the sample at 131 (66%). Sixty-nine (34.5%) were diagnosed with breast cancer, and majority of them (89%) had chemotherapy. The survivors were mostly within the first to third year of cancer survivorship (59%). The participants reported having survivorship needs based on the CaSUN measure (mean = 8.56, SD = 9.26) and subscales: existential survivorship (mean = 4.24, SD = 4.96), comprehensive cancer care (mean = 1.91, SD = 2.23), information (mean = 0.96, SD = 1.28), relationship (mean = 0.69, SD = 1.07), and QoL (mean = 0.76, SD = 0.91). Participants generally reported good QoL (mean = 7.22, SD = 1.85). The demographic information of the participants is presented in Table 1.
Table 2 shows the skewness and kurtosis results of CaSUN, CSSN, and QoL scores ranging from − 0.12 to − 0.88 and − 0.36 to − 0.47, indicating that the study variables were normally distributed and fulfilled the use of complete information maximum likelihood in path analysis [24]. The results of the correlation matrix for all constructs are presented in Table 3. Patient age was significantly correlated to the years with cancer, whereas gender was significantly correlated to cancer type. The CaSUN scores were significantly correlated to year of cancer and CSSN. The QoL scores were significantly correlated to age, gender, ethnicity, and CSSN. Figure 2 shows the path analytic model to examine the structural relationships among the study variables. Age has a significant positive effect on years with cancer (β = 0.214, P = 0.002); gender (male) has a significant negative effect on type of cancer (solid tumor malignancies) (β = − 0.294, P < 0.001); type of cancer (solid tumor malignancies) has a significant negative effect on CaSUN scores (total supportive care need) (β = − 0.154, P = 0.033). The CaSUN scores (total supportive care need) revealed a significant positive effect on the CSSN scores (experienced symptoms) (β = 0.343, P < 0.001), whereas the CSSN scores (experienced symptoms) had a significant negative effect on QoL scores (quality of life) (β = − 0.333, P < 0.001). The model statistics for path analysis model fitted well with our data (χ2/d/f = 1.337, IFI = 0.986, CFI = 0.982, and RMSEA = 0.041). This finding suggested that older cancer survivors were more likely to have spent more years with cancer and males were less likely to have oncological cancer. Cancer survivors with oncological cancer were less likely to have supportive care needs. The result also indicated that cancer survivors who required supportive care were more likely to experience physical symptoms. Cancer survivors with more physical symptoms may have poorer QoL. These findings partially supported the hypothetical relationships among study variables based on the symptom experience model in the path analysis.
Discussion
This study reported the relationship between the demographic and disease characteristics, unmet needs, experienced symptoms, and the QoL of patients who completed at least one cycle of cancer treatment and were either in the acute, extended, or permanent survivorship phase of their cancer trajectory. Majority of the participants had a diagnosis of breast cancer and were in the first to third year of survivorship. To our knowledge, this study is the first in Singapore to explore survivorship care needs among all cancer types in both inpatient and outpatient units. This study found that patients’ age was correlated to years with cancer, while patients’ gender was correlated to the type of cancer. CaSUN scores were significantly correlated to year of cancer and CSSN. QoL scores were significantly related to patients’ age, ethnicity, and CSSN. This partially supported the hypothetical model.
Demographic and disease characteristics
This study found that older cancer survivors were more likely to live long with cancer. This finding is not surprising given that patients with cancer are living longer because of advancements in cancer detection and treatment modalities, with older patients making up a significant proportion of the population [27, 28]. In addition, majority of the participants suffered from breast cancer, which has relatively high 5-year survival rates [29]. The present study also found that males were less likely to have oncological malignancies. Again, this finding may be due to the over-representation of breast cancer in this study. The breast cancer population in this study did not comprise any males. In addition, 19.5% of the study population were individuals suffering from hematological malignancies, and majority of them were males. Fitzmaurice and colleagues [30] found that hematological malignancies were predominantly diagnosed in males than in females. However, such finding does not equate to males being less likely to have solid tumor malignancies. Nonetheless, these two probable reasons supported the finding that males were less likely to have oncological malignancies.
Individual characteristics
Individual characteristics comprised health knowledge, values, past experiences, and sense of coherence [17] and were measured using CaSUN. Needs surrounding QoL such as management of side effects and lifestyle changes are of utmost concern among the study population. These findings were comparable with a study by Thompson, Stan [31] of 329 survivors of breast cancer and an analysis by Campo, Leniek [32] of 3076 cancer survivors, which reported that symptom management (pain, distress, and neuropathy) was important to survivors whose needs were not totally met. Comprehensive cancer care and information were two other unmet needs. Access to comprehensive cancer care addresses the availability of healthcare services, communication between doctors, and accessibility of parking areas, which was highlighted. Participants who rated parking as highly unmet described a “lack of parking facilities” in the open-ended segment of the questionnaire. This concern was also found by a UK study by Morrison, Henderson [33], where patients were unable to locate parking facilities near treatment areas. In the current study, this finding can be due to the ongoing upgrading efforts in the study hospital, which resulted in a lack of visitor parking. This concern is common because majority of the participants were within the acute or extended survival phase of their cancer trajectory with more frequent visits and follow-ups in surveillance and survivorship clinics. Informational needs consisting of understandable and up-to-date information were met among the study population, possibly owing to the availability of nurse navigators (breast, colorectal, lymphoma, leukemia, myeloma, and bone marrow transplant) in our hospital. The role of nurse navigators includes being a resource person and following up with patient appointments. In addition, the hospital provides a home care and nurse-led cancer telephone hotline service for patients and their caregivers, which has been found useful to patients and their families for obtaining timely information to alleviate their immediate concerns and stress [34]. Studies showed that nurse-led services by advanced practice nurses offer patient-centered care in a coordinated and cohesive manner [35, 36]. Existential survivorship comprising personal elements such as stress management, concerns about recurring cancer, interpersonal relationships, and self-expectations was among the least concerns of the study population. However, Hodgkinson et al. [37] found that patients with breast cancer, which was also the predominant diagnosis in our study, have also reported existential survivorship as highly unmet. This difference could be due to the several protective factors for the survivors. First, survivorship programs using psychosocial interventions are readily available in our study hospital [38]. Second, Singapore citizens have basic insurance coverage from the government’s MediShield scheme to support their medical expenses [39], an important aspect especially when survivors who were not initially covered by medical insurance experience difficulties that add to their financial stress [31].
Symptom experience
Majority of the patients reported symptoms as minor except for fatigue, which was the most experienced physical symptom among the population with cancer. This finding was echoed by Russell et al. [40] and Burris et al. [41] in their studies, where survivors of colorectal and breast malignancies also reported high frequencies of fatigue. Survivors verbalized the presence of long-term fatigue even after completing chemotherapy and transition from “patient to survivor,” where they had to reassume their premorbid roles such as household matters, work, and follow-up visits to the hospital [34, 42]. Fertility was rated as the least concern among the participants, which was not unexpected given that fertility and sexual health issues are often experienced by young adult cancer survivors [43] as opposed to older adult survivors, which largely composed the subjects of our study. The present study also showed that cancer survivors with more physical symptoms were more likely to have poorer QoL, a finding that is similar to that of numerous studies, where the presence of physical symptoms negatively affected the QoL of cancer survivors [6, 7, 12]. In addition, Beck, Towsley, Caserta, LinDau, and Dudley [44] attributed this finding to the presence of comorbid diseases along with cancer survivorship symptoms that led to poorer QoL.
Strengths and limitations
This paper contributed to the understanding of survivorship care needs among a multiethnic group of cancer survivors. With the use of path analysis method, the relationships between demographic, disease, and individual characteristics, symptom experience, and QoL were explored. Given that recruitment was not limited to any specific cancer group, this study provided an overview of the survivorship needs among a multiethnic population. However, this study adopted a cross-sectional, convenience sampling approach in a single site with a possibility of selection bias [45]. Breast cancer survivors were also overrepresented, which possibly limited the generalizability of the findings to all cancer survivors receiving care from other settings. In addition, the use of a self-administered questionnaire may have affected the results because of social desirability bias [46]. Despite the limitation, this study is the first to obtain baseline information about survivorship care needs that are unique to a multiethnic population, thereby informing the policy and planning activities in Singapore. In addition, the response rate was high at 67.7%, and many of the participants were diagnosed with solid tumors (breast, lung, and colorectal) and were receiving chemotherapy in an outpatient unit. The patients with hematological cancers or in an inpatient unit were limited. However, the recruited solid tumor groups were representative of the top three male and female cancers in Singapore [47].
In conclusion, cancer survivors continue to live longer due to technological and pharmacological advancement in managing cancer. However, survivors continue to report long-term side effects, fears of recurrence, uncertainty, financial difficulties, and comorbidities that affect the older population. Continued care with a focus on symptom management beyond acute treatment is essential to ensure the concerns are appropriately managed to ensure good survivorship outcomes. This study provided valuable information regarding met and unmet survivorship care needs among Singaporean patients with cancer that could provide valuable information on the most appropriate survivorship care plan approach for healthcare professionals. Moving forward, oncology care with special attention to geriatric oncology patients, management of side effects, and lifestyle changes should be incorporated into the acute treatment phase in anticipation of patient’s future survivorship needs. The essential components amid difficulties in providing complex survivorship care and addressing patient QoL were highlighted for policy implications.
References
Simon S (2016) ACS report: number of US cancer survivors expected to exceed 20 million by 2026. American Cancer Society, Atlanta
Office, N.R.o.D. (2017) Singapore Cancer Registry Annual Registry Report 2015, Health Promotion Board Singapore
Feuerstein M (2007) Defining cancer survivorship. J Cancer Surviv 1(1):5–7
Mullan F (1985) Seasons of survival: reflections of a physician with cancer, Mass Med Soc
den Bakker C et al (2018) Cancer survivors’ needs during various treatment phases after multimodal treatment for colon cancer-is there a role for eHealth? BMC Cancer 18(1):1207
Zhang M-f et al (2015) The influence of demographics, psychological factors and self-efficacy on symptom distress in colorectal cancer patients undergoing post-surgical adjuvant chemotherapy. Eur J Oncol Nurs 19(1):89–96
Hung HY, Wu LM, Chen KP (2018) Determinants of quality of life in lung cancer patients. J Nurs Scholarsh 50(3):257–264
Giuliani M, McQuestion M, Jones J, Papadakos J, le LW, Alkazaz N, Cheng T, Waldron J, Catton P, Ringash J (2016) Prevalence and nature of survivorship needs in patients with head and neck cancer. Head Neck 38(7):1097–1103
Horick NK, Muzikansky A, Gutierrez HL, Boyd KL, Finkelstein DM (2018) Physical symptoms in long-term survivors of rare cancer. J Cancer Surviv 12(6):835–842
Ness S, et al. (2013) Concerns across the survivorship trajectory: results from a survey of cancer survivors. in Oncol Nurs Forum
Mayer DK, Nasso SF, Earp JA (2017) Defining cancer survivors, their needs, and perspectives on survivorship health care in the USA. Lancet Oncol 18(1):e11–e18
Wu S-F, Tong HY, kan YY, Su SH, Lee MC, Kao CC, Lin YH (2017) The exploration of health-related quality of life: factors influencing quality of life in gynecologic cancer patients. Clin Nurs Res 26(1):114–131
Bernat JK, Wittman DA, Hawley ST, Hamstra DA, Helfand AM, Haggstrom DA, Darwish-Yassine M, Skolarus TA (2016) Symptom burden and information needs in prostate cancer survivors: a case for tailored long-term survivorship care. BJU Int 118(3):372–378
Reed SC, Bell JF, Whitney R, Lash R, Kim KK, Bold RJ, Joseph JG (2018) Psychosocial outcomes in active treatment through survivorship. Psycho-oncology 27(1):279–285
Taylor K, DipOnc G, Monterosso L (2015) Survivorship care plans and treatment summaries in adult patients with hematologic cancer: an integrative literature review. in Oncol Nurs Forum
Wieldraaijer T, Duineveld LAM, Bemelman WA, van Weert HCPM, Wind J (2019) Information needs and information seeking behaviour of patients during follow-up of colorectal cancer in the Netherlands. J Cancer Surviv 13(4):603–610
Armstrong TS (2003) Symptoms experience: a concept analysis. In Oncology Nursing Forum. Oncol Nurs Soc
Cohen J (1992) Quantitative methods in psychology: a power primer. Psychol Bull 112:1155–1159
Hodgkinson K, Butow P, Hunt GE, Pendlebury S, Hobbs KM, Lo SK, Wain G (2007) The development and evaluation of a measure to assess cancer survivors’ unmet supportive care needs: the CaSUN (Cancer Survivors’ Unmet Needs measure). Psychooncology 16(9):796–804
Schlairet MC, Heddon MA, Martha Griffis R (2010) Piloting a needs assessment to guide development of a survivorship program for a community cancer center. In Oncology Nursing Forum. Oncol Nurs Soc
Pearce NJ, Sanson-Fisher R, Campbell HS (2008) Measuring quality of life in cancer survivors: a methodological review of existing scales. Psychooncology 17(7):629–640
Arbuckle JL (2017) IBM SPSS AMOS 25 User’s guide, United States: IBM Development Corporation
Byrne BM (2016) Structural Equation Modeling With AMOS: Basic Concepts, Applications, and Programming (Third Edition). Routledge, New York
Kline RB (2015) Principles and practice of structural equation modeling (fourth edition). Guilford publication, New York
Schermelleh-Engel K, Moosbrugger H, Müller H (2003) Evaluating the fit of structural equation models: tests of significance and descriptive goodness-of-fit measures. Methods Psychol Res Online 8(2):23–74
Hu Lt, Bentler PM (1999) Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model Multidiscip J 6(1):1–55
Parry C, Kent EE, Mariotto AB, Alfano CM, Rowland JH (2011) Cancer survivors: a booming population. Cancer Epidemiol Prev Biomarkers 20(10):1996–2005
Mangoni AA et al. (2016) Chronic conditions and cancer in older adults, in Cancer and chronic conditions, Springer. p. 421–454
Runowicz CD, Leach CR, Henry NL, Henry KS, Mackey HT, Cowens-Alvarado RL, Cannady RS, Pratt-Chapman ML, Edge SB, Jacobs LA, Hurria A, Marks LB, LaMonte S, Warner E, Lyman GH, Ganz PA (2016) American Cancer Society/American Society of Clinical Oncology breast cancer survivorship care guideline. CA Cancer J Clin 66(1):43–73
Fitzmaurice C et al (2017) Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA Oncol 3(4):524–548
Thompson CA, Stan DL, Solberg Nes L, Jenkins SM, Lackore KA, Pruthi S (2014) Breast cancer survivors’ self-reported needs and preferences of survivorship care. Breast J 20(1):107–109
Campo RA, Leniek KL, Gaylord-Scott N, Faurot KR, Smith S, Asher G, Porterfield D, Gaylord SA (2016) Weathering the seasons of cancer survivorship: mind-body therapy use and reported reasons and outcomes by stages of cancer survivorship. Support Care Cancer 24(9):3783–3791
Morrison V, Henderson BJ, Zinovieff F, Davies G, Cartmell R, Hall A, Gollins S (2012) Common, important, and unmet needs of cancer outpatients. Eur J Oncol Nurs 16(2):115–123
Ang WHD, Lang SP, Ang E, Lopez V (2016) Transition journey from hospital to home in patients with cancer and their caregivers: a qualitative study. Support Care Cancer 24(10):4319–4326
Gates P, Krishnasamy M (2009) Nurse-led survivorship care. In Cancer Forum. The Cancer Council Australia
Lipscomb J, Gotay CC, Snyder CF (2007) Patient-reported outcomes in cancer: a review of recent research and policy initiatives. CA Cancer J Clin 57(5):278–300
Hodgkinson K, Butow P, Hunt GE, Pendlebury S, Hobbs KM, Wain G (2007) Breast cancer survivors’ supportive care needs 2–10 years after diagnosis. Support Care Cancer 15(5):515–523
Mahendran R, Lim HA, Tan JYS, Ng HY, Chua J, Lim SE, Kua EH, Griva K (2017) Evaluation of a brief pilot psychoeducational support group intervention for family caregivers of cancer patients: a quasi-experimental mixed-methods study. Health Qual Life Outcomes 15(1):17
Lim J (2017) Sustainable health care financing: the Singapore experience. Glob Policy 8:103–109
Russell L, Gough K, Drosdowsky A, Schofield P, Aranda S, Butow PN, Westwood JA, Krishnasamy M, Young JM, Phipps-Nelson J, King D, Jefford M (2015) Psychological distress, quality of life, symptoms and unmet needs of colorectal cancer survivors near the end of treatment. J Cancer Surviv 9(3):462–470
Burris JL, Armeson K, Sterba KR (2015) A closer look at unmet needs at the end of primary treatment for breast cancer: a longitudinal pilot study. Behav Med 41(2):69–76
Zebrack BJ, Mills J, Weitzman TS (2007) Health and supportive care needs of young adult cancer patients and survivors. J Cancer Surviv 1(2):137–145
Bober SL, Fine E, Recklitis C (2019) Sexual health and rehabilitation after ovarian suppression treatment (SHARE-OS): a clinical intervention for young breast cancer survivors. J Cancer Surviv: p. 1–5
Beck SL, Towsley GL, Caserta MS, Lindau K, Dudley WN (2009) Symptom experiences and quality of life of rural and urban older adult cancer survivors. Cancer Nurs 32(5):359–369
Etikan I, Musa SA, Alkassim RS (2016) Comparison of convenience sampling and purposive sampling. Am J Theor Appl Stat 5(1):1–4
Van de Mortel TF (2008) Faking it: social desirability response bias in self-report research. Aust J Adv Nurs 25(4):40
Teo MC, Soo KC (2013) Cancer trends and incidences in Singapore. Jpn J Clin Oncol 43(3):219–224
Acknowledgments
The authors would like to thank all survivors for participating in this study. The authors would also like to thank Professor Alex Molasiotis of Hong Kong Polytechnic University and Professor Raymond Chan of Queensland University of Technology for their inclusion into the STEP study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval was obtained from the Singapore National Healthcare Group-Domain Specific Review Board (2016-01023). All participants received study information and provided verbal and written consent.
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ang, W.H.D., Lau, Y., Ngo, L.P.E. et al. Path analysis of survivorship care needs, symptom experience, and quality of life among multiethnic cancer survivors. Support Care Cancer 29, 1433–1441 (2021). https://doi.org/10.1007/s00520-020-05631-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05631-6