Abstract
Purpose
This study examined the mediating effects of cancer type, treatment, and distress on health-related quality of life (HRQoL) for early diagnosis cancer patients. Results were interpreted with respect to established thresholds for clinical meaningfulness.
Methods
A cross-sectional design was used. Patients completed surveys collecting demographics, cancer type, treatment, comorbid conditions, distress (HADS), and HRQoL (FACT-G). Hierarchical multivariate regressions examined associations between cancer type, treatment, and distress on HRQoL. Established minimum differences were used to identify clinically meaningful changes in HRQoL.
Results
Of the 1183 patients surveyed, 21% were classified as having elevated anxiety and 13% had elevated depression. Our sample reported significantly lower physical and emotional well-being compared to population norms. Patients with prostate, melanoma, gynaecological, and urological cancers had higher HRQoL scores than those with colorectal cancer. However, when effects for treatment type and distress were considered, differences between cancer types became non-significant. Anxiety and depression were associated with lower HRQoL scores as was chemotherapy. Only depression, anxiety, and chemotherapy were associated with clinically meaningful decreases in HRQoL scores.
Conclusions
While statistically significant differences in HRQoL were found between different cancer types, only chemotherapy, anxiety, and depression produced clinically meaningful poorer HRQoL scores. In practice, clinically meaningful differences could promote a shift in resources toward interventions where a positive effect on patient well-being is appreciated by both the patient and health professional.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Patient-reported outcome measures (PROMs) are now generally accepted to be concomitant with more traditional assessments of clinical outcomes and are recommended for routine use in clinical trial [1, 2] and survivorship [3] settings. While the benefit of implementing PROMs in daily clinical practice may improve patient-physician communication, diagnosis, and supportive care, a systematic review has identified the need for considerable work in this field before a quantifiable effect on health outcomes can be appreciated [4].
In the oncology setting, PROMs regularly take the form of distress screening tools. However, it is argued that distress measures alone are not enough to target the gamut of symptoms associated with cancer which include physical and psychosocial factors relating to symptoms, diagnosis, and treatment [5]. Health-related quality of life measures offer a more holistic and multi-dimensional approach by investigating characteristics attributable to the patient as well as their environment and include assessment of physical, functional, emotional, and social well-being [6, 7]. There is evidence showing improvements in physicians’ general awareness of their patients’ quality of life when daily HRQoL assessments are incorporated in clinical oncology practice [8].
Systematic reviews have demonstrated the benefit of incorporating HRQoL assessment in clinical trials as both a means of evaluating the outcome of new therapeutic interventions and a mechanism to identify opportunities for intervention [9,10,11,12]. In a study investigating women with advanced breast cancer, HRQoL factors were shown to predict chemotherapy response and toxicity as well as survival [13]. Additionally, in one randomised controlled trial with brain cancer patients, results showed no negative effect on HRQoL in those patients receiving a more aggressive treatment combination compared to those receiving a single treatment regime [2].
While research has examined the impact on HRQoL of specific cancers and treatments, few studies have investigated HRQoL across the disease and treatment spectrum. Information relating to disease-specific differences in HRQoL can assist healthcare professionals to effectively identify and support patient populations susceptible to lower HRQoL as a function of their cancer type and/or treatment received.
Evidence regarding the impact of cancer type on HRQoL suggests time since diagnosis is important. Studies investigating HRQoL for patients within a year of diagnosis have reported differences in HRQoL by cancer type. For instance, work by Reeve and colleagues [14] suggested that cancer type is associated with different HRQoL scores when patients are investigated closer to the time of their diagnosis (around 12 months post-diagnosis), while Zebrack and colleagues [15] found no effect of cancer type on HRQoL for long-term survivors. The reason why cancer type effects may appear closer to the time of diagnosis is likely to be a reflection on treatment, symptoms, and distress experienced at this early stage as these factors contribute to a patient’s overall HRQoL and global health perceptions [6, 7]. A recent literature review suggested that, in early-stage cancer patient populations, cancer site, treatment type, and other sociodemographic features are related to at least one domain of HRQoL [16]. The authors did not, however, include distress in their investigation. Exploring the relationship between cancer type, treatment, and distress could provide insight into factors influencing HRQoL early in the cancer trajectory so they do not evolve into a larger problem in the survivorship phase.
Despite the increasing interest in applying HRQoL measures in the clinical setting, a challenge remains in the interpretation and application of results from these measures. Meaningful change is defined as the magnitude of change required in HRQoL measures which leads to a perceivable impact on patients’ lives (i.e. whether the patient has noticeably improved or deteriorated) [17]. Therefore, a ‘change’ reported by a patient or clinician does not necessarily coincide with statistically significant differences between groups of patients noted in research studies. In their systematic review, Bedard and colleagues highlighted that large sample sizes regularly generated statistically significant differences in HRQoL scores many of which may not necessarily lead to a meaningful outcome for the cancer patient [17]. Change scores between 2 and 14 points have been suggested as necessary to obtain a clinically meaningful change, with the size of the change dependent on the individual, the scale used, and the disease [17,18,19,20,21,22,23,24].
In this paper, we employ an analytical approach to explore the mediating effects of cancer type, treatment type, and psychological distress on separate HRQoL subscales using the FACT-G measurement tool for a range of cancer patients using hierarchical (stepped) regression modelling. We also explore clinically meaningful change by utilising established minimum thresholds reported for the FACT-G measurement tool [17, 25, 26] to assess the significance of differences found.
Methods
Participants
Participants were registered with the Victorian Cancer Registry (VCR); a population-based cancer registry for Australia’s second most populous state. Those who met the following eligibility criteria were invited to participate in the study: (1) confirmed diagnosis of invasive cancer, (2) aged 18–79 years of age, (3) registered with the VCR within 4 months of diagnosis, and (4) spoke English. People with a previous diagnosis of cancer or who were judged unsuitable to participate (e.g. due to cognitive impairment) by their treating clinician were excluded.
Procedures
The VCR identified a consecutive sample of people meeting the eligibility criteria and contacted each person’s notifying clinician to confirm eligibility. Clinicians were asked to inform the VCR within 4 weeks if they were aware of any reason why the person should not be approached for the study.
The VCR contacted eligible patients by mail and informed them of the study and asked if they agreed to the research team contacting them about study participation. After obtaining written consent for the VCR to release their contact details to the research team, a survey was sent along with a study information sheet and reply-paid envelope to participants. Return of the survey was considered consent. Up to two reminder letters were sent to non-responders.
Measures
Demographics
Participants reported demographic details including age, sex, marital status, and postcode (see Table 1). Marital status was coded to reflect ‘living with a partner’ vs ‘not living with a partner’, taking into account de facto, same sex relationships, and divorced and widowed individuals. Socioeconomic status was determined by substituting postcode values with an index score of relative socioeconomic disadvantage, as stipulated by the Australian Bureau of Statistics [27]. This score was recoded to represent which category (out of three) the individual was classed (1 = 0–40%— highest disadvantage, 2 = 41–80%—moderate disadvantage, and 3 = 81–100%— least disadvantage).
Comorbid conditions
Participants were asked to indicate if they had any existing health problems other than cancer. The list of conditions to choose from included heart disease, arthritis, diabetes, asthma, existing depression, existing anxiety, and chronic pain.
Diagnoses and treatment
Information on participant cancer type and date of diagnosis was obtained from the VCR. Specific cancer diagnoses were classified into broader cancer types: breast, prostate, colorectal, melanoma, lung, gynaecological, haematological, head and neck, urological, upper gastro-intestinal (GI), and other (see Table 1).
Participants were asked to indicate what treatment, if any, they had received. Responses were dummy-coded into three separate variables (chemotherapy, surgery, and radiotherapy), allowing for cases where more than one form of treatment was received. Other forms of treatment including adjuvant/alternative therapy were not recorded.
Emotional distress
Participants completed the Hospital Anxiety and Depression Scale (HADS), a 14-item scale comprising both an anxiety and depression subscale [28] that is widely used in oncology [29]. The scale has high internal consistency (α = .80 anxiety subscale, α = .81 depression subscale) and high test-retest reliability (correlation coefficients > .85) [30]. Higher scores reflect greater anxiety and depression. Participants rate how often they have experienced several different symptoms over the past 2 weeks on a 4-point scale. Responses to the seven items for each of the two scales are summed. If a response for a single item was missing for a respondent, the score was inferred using the mean of the remaining six items. If more than one item was missing, then the subscale was judged invalid for that participant. Scores above 11 have been identified as indicating clinically significant levels of anxiety or depression, while scores between 8 and 10 indicate borderline levels [28]. Based on findings that lower cut-off scores are needed for cancer patients [31, 32], a score of 8 was used in this paper to identify participants as having ‘elevated’ distress.
Health-related quality of life
The Functional Assessment of Cancer Therapy-General (FACT-G) version 4 assessed HRQoL. The FACT-G has shown to be a popular and effective scale used to assess HRQoL in the oncology setting [33]. This 27-item scale has been developed and validated for use with cancer patients and displays high internal consistency (overall scale α = .89) [33]. The measure comprises four domains of health-related quality of life (physical well-being (seven items, α = .82), social/family well-being (seven items, α = .69), emotional well-being (six items, α = .74), functional well-being (seven items, α = .80)), and an overall HRQoL score. Higher scores reflect higher HRQoL in each domain.
Meaningful change for the FACT-G scale has been investigated previously and reported as equal to or greater than two points for each of the subscales and five points for the FACT-G total score [17, 25, 26]. At least 80% of all items were required to be completed for the FACT-G to be considered valid. For those cases considered valid, any missing values were pro-rated similar to the HADS measure.
Analytic strategy
Analyses were conducted using the R statistical package, Version 3.4 (R Core Team, 2018). Descriptive statistics such as means, frequencies, and percentages were computed for patient demographics (Table 1) and HADS and FACT-G scales (not shown). Australian normative scores for a modified version of the FACT-G scale (FACT-GP, [26]) were also compared to results from this study.
Five hierarchical multivariate regressions were used for the FACT-G measure to create predictive models for each HRQoL subscale and the FACT-G total score (Table 2). Unstandardised estimates for beta values were reported to investigate absolute changes in subscale scores attributed to an increase of one unit in each predictor when the effects of all other predictors were held constant. Cancer type was included in Step 1 followed by distress (HADS) and treatment type predictors in Step 2. The colorectal sample was used as the reference group for multivariate analyses as it is a common cancer which affects both sexes equally. Model fit was calculated using R2 and F-ratios for each step.
Age, sex, marital status, socioeconomic status, and self-reported comorbid conditions (see Table 1) were included as covariates in all regression analyses (see Supplementary Table 1 for full model with all covariates shown).
Results from regression analyses were also interpreted with reference to established minimum differences previously reported for the FACT-G scales for any change in HRQoL to be detected by the patient or clinician [17, 25, 26].
Results
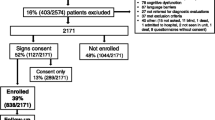
Of the 3713 eligible participants identified by the VCR, 1201 (32%) people consented to participate in the study and returned completed surveys via post. Eighteen cases were excluded from analyses due to high percentage of missing data. Therefore, the results in this study were based on survey data from 1183 participants.
Descriptives
Table 1 presents the main characteristics of the sample. Average age of participants was 60.5 years (SD = 10.9) and the mean time since diagnosis was 5.3 months (SD = 1.4).
Most participants reported living with a partner (78%) and residing in areas of highest socioeconomic disadvantage (44%). The most common comorbid condition reported was heart disease (20%). Breast (24%) was the largest cancer group in the sample, and 83% of all participants received surgical intervention for their cancer.
Overall, 21% of participants were classified as having elevated anxiety and 13% as having elevated depression. Breast, melanoma, head and neck, urological, and upper GI cancers had the highest prevalence of elevated anxiety. Although a small group, 42% of people with other cancers were also classified as having elevated anxiety.
The prevalence of elevated depression was highest among participants with upper GI (28%) and lung (24%) cancers. Prostate cancer had the lowest prevalence of elevated anxiety (10%) and depression (9%) in the sample.
Participants treated by surgery had a lower prevalence of elevated anxiety (20%) and depression (12%), while those not receiving any treatment had the highest prevalence of elevated anxiety (29%) and depression (20%); however, it should be acknowledged that this group comprised only 45 individuals (3.8% of total participant sample).
Overall, participants scored lower on the PWB and EWB subscales (all p < .01) but higher on the SWB and FWB subscales (all p < .05) compared to population norms. However, overall FACT-G total scores were similar to population norms (p = .55).
Regression models
Table 2 presents results from the hierarchical multivariate regression models for cancer, treatment type, and distress on each HRQoL scale (FACT-G subscales and total score) after adjusting for various demographic variables. All regression models were significant at each step (all p < .01).
Step 1 in each regression model shows the effects for cancer type, with colorectal cancer as the reference group. Significant increases in HRQoL scores were associated with prostate (b = 2.98, p < .01), melanoma (all b > 2.92, p < .01), gynaecological (all b > 2.72, p < .05), and urological (b = 3.21, p < .01) cancer types. However, compared to colorectal cancer patients, HRQoL scores were lower for lung (b = − 2.41, p < .05), upper GI (b = − 3.15, p < .05), and other cancer types (b = − 2.62, p < .01).
Except for PWB scale, the effects for cancer type on HRQoL subscales and overall became non-significant when treatment type and distress were introduced in step 2. Significant effects of cancer type remained in the PWB subscale (melanoma, b = 3.08, p < .01; gynaecological, b = 2.06, p < .05; urological, b = 3.02, p < .01). For the FACT-G total score, at Step 2, melanoma patients had higher scores than colorectal patients (b = 5.24, p < .01).
Distress was associated with lower HRQoL scores on all scales (anxiety, all b < − 1.37, p < .01; depression, all b < − 2.61, p < .01). However, for treatment, significant effects were only seen for chemotherapy, with lower HRQoL in the PWB, FWB, and FACT-G total scales (all b < − 2.34, p < .01).
Overall, results in Fig. 1 suggest that melanoma, urological, and gynaecological cancers were associated with the highest HRQoL scores, while anxiety, depression, and chemotherapy were associated with the lowest scores in the sample. Established minimum thresholds [17, 25, 26] for clinically meaningful differences in FACT-G scales are also illustrated in Fig. 1 by dashed vertical lines. When visually interpreted with respect to these thresholds, only depression, anxiety, and chemotherapy were suggestive of negatively influencing HRQoL scores by a clinically meaningful amount.
Coefficients reported in step 2 of Table 2, with 95% CIs for each HRQoL scale. Significant effects are identified in red. Dashed lines represent minimum reported thresholds for clinically meaningful differences for each FACT-G scale
Significant effects for melanoma, urological, and gynaecological cancers were associated with increases in PWB scores (including FACT-G total score for melanoma). However, their clinical meaningfulness could be considered borderline.
Discussion
In a sample of patients averaging 5 months post-diagnosis, we found significant differences in HRQoL across cancer types. However, these differences were mediated by treatment and distress levels suggesting that these factors, rather than cancer type per se, drive HRQoL in this early stage of survivorship. When clinically meaningful thresholds were considered, chemotherapy, anxiety, and depression, rather than cancer type, were associated with poorer HRQoL scores.
Cancer patients in our sample had, on average, significantly higher overall SWB and FWB scores than the general population, with PWB and EWB lower in our sample compared to population norms [26]. While the reasons behind these findings are not immediately apparent in our sample, it is likely that in some cases, additional support from friends and family provided to many people with cancer may translate to increases in SWB. Furthermore, frequent contact with nurses, allied health, and community-based services during their treatment may also add to the sense of social well-being. With respect to FWB, it is possible that some functional aspects of a patient’s life may have been restored or improved following their treatment intervention (our patient sample comprised cancer survivors, on average 5 months post-diagnosis). Research has shown some long-term improvements in function scales following treatment [34]; however, treatment intensity has shown to negatively affect this [35]. However, we note that the differences seen between our sample and population norms for FWB were largely statistical and are unlikely to translate to a perceptible difference between our patient sample and the general population.
Health-related quality of life was initially found to vary by cancer type. However, type of treatment and anxiety and depression levels mediated this variation, consistent with previous findings [36]. When treatment and distress levels were not considered in analyses, patients with prostate, melanoma, gynaecological, and urological cancer generally had higher HRQoL compared to colorectal cancer patients. These findings are similar to those reported by Choi and colleagues [37] who showed higher HRQoL scores for prostate cancer patients compared to general cancer population. Other research has shown long-term HRQoL remains unaffected following treatment for prostate [38] and gynaecological [39] cancers. Likewise, higher HRQoL scores associated with melanomas could be attributable to their treatment, which is largely surgical with minimally invasive procedures, with little or sometimes no inpatient stay.
Previous research has pointed to the potential mediating role of treatment on HRQoL [17, 35, 40] suggesting that type of treatment might be responsible for much of the variation in HRQoL between cancer types. Our findings that the association between cancer type and HRQoL reduced to non-significant levels once treatment and distress were included in the models are in line with this suggestion. Our results suggest that patients with cancers requiring chemotherapy are at greater risk of lower HRQoL scores than those with cancers that do not require chemotherapy.
Around 20% of patients in our sample experienced elevated anxiety and 13% experienced elevated depression approximately 5 months post-diagnosis. Our results showed a strong inverse relationship between distress and HRQoL for our sample of cancer patients. While distress is commonly investigated in isolation to HRQoL measures, it is important to consider its strong relationship with HRQoL, and the potentially causal influence it has on HRQoL [5,6,7]. As these studies suggest, future investigations could assess these measures together to gain a more holistic understanding on the factors affecting patient well-being.
Many of the significant effects of cancer type and treatment on HRQoL we identified (red lines in Fig. 1) were not clinically meaningful. Interestingly, only chemotherapy, anxiety, and depression were associated with decreases in HRQoL that were clinically meaningful. Differences in HRQoL for melanoma, urological, and gynaecological cancers were of borderline clinical significance, which may be due to the relative small number of these cases in our sample. These results, therefore, suggest that interventions targeting anxiety and depression, especially in patients receiving chemotherapy, are more likely to demonstrate stronger improvements in patient HRQoL which are clinically meaningful and appreciated by both the patient and health professional.
Several limitations of our study need to be noted. We could not control for stage of disease, as this information was not captured. As other studies have found disease stage influences HRQoL [41], our findings may be altered if we were able to include disease stage in the model. Likewise, we did not assess treatment side effects and cancer-related fatigue which are known to exist in large proportions of cancer patients and can negatively impact HRQoL [42, 43]. Some strengths of the study also need to be noted. Our large sample size and population approach to recruitment ensured that we captured a representative dataset which can help in the generalisability of these findings. A further strength of this study was the use of a validated measure of HRQoL and our attempt to identify and understand the clinical significance of differences in HRQoL.
Despite these limitations, our study suggests that anxiety, depression, and chemotherapy were associated with clinical meaningful deficits in cancer patients’ HRQoL, at least in the first year post-diagnosis. This highlights the importance of screening for these two conditions, especially in chemotherapy patient populations, where this work can contribute toward the future translation and application of these findings in real-world settings.
References
Saban KL, Penckofer SM, Androwich I, Bryant FB (2007) Health-related quality of life of patients following selected types of lumbar spinal surgery: a pilot study. Health Qual Life Outcomes 5:71. https://doi.org/10.1186/1477-7525-5-71
Taphoorn MJB, Stupp R, Coens C, Osoba D, Kortmann R, van den Bent MJ, Mason W, Mirimanoff RO, Baumert BG, Eisenhauer E, Forsyth P, Bottomley A, Ncic CTG (2005) Health-related quality of life in patients with glioblastoma: a randomised controlled trial. Lancet Oncol 6(12):937–944. https://doi.org/10.1016/s1470-2045(05)70432-0
Efficace F, Bottomley A, Smit EF, Lianes P, Legrand C, Debruyne C, Schramel F, Smit HJ, Gaafar R, Biesma B, Manegold C, Coens C, Giaccone G, Van Meerbeeck J, Grp ELC, Quality Life U (2006) Is a patient’s self-reported health-related quality of life a prognostic factor for survival in non-small-cell lung cancer patients? A multivariate analysis of prognostic factors of EORTC study 08975. Ann Oncol 17(11):1698–1704. https://doi.org/10.1093/annonc/mdl183
Valderas JM, Kotzeva A, Espallargues M, Guyatt G, Ferrans CE, Halyard MY, Revicki DA, Symonds T, Parada A, Alonso J (2008) The impact of measuring patient-reported outcomes in clinical practice: a systematic review of the literature. Qual Life Res 17(2):179–193. https://doi.org/10.1007/s11136-007-9295-0
Bultz BD, Carlson LE (2013) A commentary on ‘Effects of screening for psychological distress on patient outcomes in cancer: a systematic review’. J Psychosom Res 75(1):18–19. https://doi.org/10.1016/j.jpsychores.2013.04.002
Wilson IB, Cleary PD (1995) Linking clinical variables with health-related quality of life: a conceptual model of patient outcomes. J Am Med Assoc 273(1):59–65. https://doi.org/10.1001/jama.273.1.59
Ferrans CE, Zerwic JJ, Wilbur JE, Larson JL (2005) Conceptual model of health-related quality of life. J Nurs Scholarsh 37(4):336–342. https://doi.org/10.1111/j.1547-5069.2005.00058.x
Detmar SB, Muller MJ, Schornagel JH, Wever LDV, Aaronson NK (2002) Health-related quality-of-life assessments and patient-physician communication - a randomized controlled trial. Jama-Journal of the American Medical Association 288(23):3027–3034. https://doi.org/10.1001/jama.288.23.3027
Granger CL, McDonald CF, Berney S, Chao C, Denehy L (2011) Exercise intervention to improve exercise capacity and health-related quality of life for patients with non-small cell lung cancer: a systematic review. Lung Cancer 72(2):139–153. https://doi.org/10.1016/j.lungcan.2011.01.006
Jansen L, Koch L, Brenner H, Arndt V (2010) Quality of life among long-term (> = 5 years) colorectal cancer survivors - systematic review. Eur J Cancer 46(16):2879–2888. https://doi.org/10.1016/j.ejca.2010.06.010
Mols F, Vingerhoets A, Coebergh JW, van de Poll-Franse LV (2005) Quality of life among long-term breast cancer survivors: a systematic review. Eur J Cancer 41(17):2613–2619. https://doi.org/10.1016/j.ejca.2005.05.017
Porter MP, Penson DF (2005) Health-related quality of life after radical cystectomy and urinary diversion for bladder cancer: a systematic review and critical analysis of the literature. J Urol 173(4):1318–1322. https://doi.org/10.1097/01.ju.0000149080.82697.65
Lee CK, Stockler MR, Coates AS, Gebski V, Lord SJ, Simes RJ, Australian New Zealand Breast C (2010) Self-reported health-related quality of life is an independent predictor of chemotherapy treatment benefit and toxicity in women with advanced breast cancer. Br J Cancer 102(9):1341–1347. https://doi.org/10.1038/sj.bjc.6605649
Reeve BB, Potosky AL, Smith AW, Han PK, Hays RD, Davis WW, Arora NK, Haffer SC, Clauser SB (2009) Impact of cancer on health-related quality of life of older Americans. J Natl Cancer Inst 101(12):860–868. https://doi.org/10.1093/jnci/djp123
Zebrack BJ, Yi J, Petersen L, Ganz PA (2008) The impact of cancer and quality of life for long-term survivors. Psycho-Oncology 17(9):891–900. https://doi.org/10.1002/pon.1300
Popovic M, Lao N, Zeng L, Zhang L, Cella D, Beaumont JL, Chow R, Chiu N, Chiu L, Lam H, Poon M, Chow E (2013) The impact of clinical and sociodemographic features on quality of life in patients with early stage cancers using the functional assessment of cancer therapy-general assessment tool. Support Care Cancer 21(8):2267–2277. https://doi.org/10.1007/s00520-013-1789-4
Bedard G, Zeng L, Lam H, Cella D, Zhang LY, Lauzon N, Chow E (2012) Meaningful change in oncology quality-of-life instruments: a systematic literature review. Expert Review of Pharmacoeconomics & Outcomes Research 12(4):475–483. https://doi.org/10.1586/erp.12.34
Askew RL, Xing Y, Palmer JL, Cella D, Moye LA, Cormier JN (2009) Evaluating minimal important differences for the FACT-melanoma quality of life questionnaire. Value Health 12(8):1144–1150. https://doi.org/10.1111/j.1524-4733.2009.00570.x
Eton DT, Cella D, Bacik J, Motzer RJ (2006) A brief symptom index for advanced renal cell carcinoma. Health Qual Life Outcomes 4:68. https://doi.org/10.1186/1477-7525-4-68
Eton DT, Cella D, Yount SE, Davis KM (2007) Validation of the functional assessment of cancer therapy - lung symptom index-12 (FLSI-12). Lung Cancer 57(3):339–347. https://doi.org/10.1016/j.lungcan.2007.03.021
Osoba D, Rodrigues G, Myles J, Zee B, Pater J (1998) Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol 16(1):139–144
Maringwa J, Quinten C, King M, Ringash J, Osoba D, Coens C, Martinelli F, Reeve BB, Gotay C, Greimel E, Flechtner H, Cleeland CS, Schmucker-Von Koch J, Weis J, Van Den Bent MJ, Stupp R, Taphoorn MJ, Bottomley A, Project EP, Brain C (2011) Minimal clinically meaningful differences for the EORTC QLQ-C30 and EORTC QLQ-BN20 scales in brain cancer patients. Ann Oncol 22(9):2107–2112. https://doi.org/10.1093/annonc/mdq726
Maringwa JT, Quinten C, King M, Ringash J, Osoba D, Coens C, Martinelli F, Vercauteren J, Cleeland CS, Flechtner H, Gotay C, Greimel E, Taphoorn MJ, Reeve BB, Schmucker-Von Koch J, Weis J, Smit EF, van Meerbeeck JP, Bottomley A, Project EP, Lung Canc G (2011) Minimal important differences for interpreting health-related quality of life scores from the EORTC QLQ-C30 in lung cancer patients participating in randomized controlled trials. Support Care Cancer 19(11):1753–1760. https://doi.org/10.1007/s00520-010-1016-5
Deyo RA, Battie M, Beurskens A, Bombardier C, Croft P, Koes B, Malmivaara A, Roland M, Von Korff M, Waddell G (1998) Outcome measures for low back pain research - a proposal for standardized use. Spine 23(18):2003–2013. https://doi.org/10.1097/00007632-199809150-00018
Cella D, Hahn EA, Dineen K (2002) Meaningful change in cancer-specific quality of life scores: differences between improvement and worsening. Qual Life Res 11(3):207–221. https://doi.org/10.1023/a:1015276414526
Janda M, DiSipio T, Hurst C, Cella D, Newman B (2009) The Queensland cancer risk study: general population norms for the functional assessment of cancer therapy-general (FACT-G). Psycho-Oncology 18(6):606–614. https://doi.org/10.1002/pon.1428
ABS (2013) Socio-economic indexes for areas (SEIFA), 2011. vol 2033.0.55.001. Australia Bureau of Statistics, Canberra
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67(6):361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
Sellick SM, Crooks DL (1999) Depression and cancer: an appraisal of the literature for prevalence, detection, and practice guideline development for psychological interventions. Psycho-Oncology 8(4):315–333. https://doi.org/10.1002/(sici)1099-1611(199907/08)8:4<315::aid-pon391>3.0.co;2-g
Quintana JM, Padierna A, Esteban C, Arostegui I, Bilbao A, Ruiz I (2003) Evaluation of the psychometric characteristics of the Spanish version of the hospital anxiety and depression scale. Acta Psychiatr Scand 107(3):216–221
Morse R, Kendell K, Barton S (2005) Screening for depression in people with cancer: the accuracy of the hospital anxiety and depression scale. Clin Eff Nurs 9(3–4):188–196. https://doi.org/10.1016/j.cein.2006.08.012
Singer S, Kuhnt S, Gotze H, Hauss J, Hinz A, Liebmann A, Krauss O, Lehmann A, Schwarz R (2009) Hospital anxiety and depression scale cutoff scores for cancer patients in acute care. Br J Cancer 100(6):908–912. https://doi.org/10.1038/sj.bjc.6604952
Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, Silberman M, Yellen SB, Winicour P, Brannon J, Eckberg K, Lloyd S, Purl S, Blendowski C, Goodman M, Barnicle M, Stewart I, McHale M, Bonomi P, Kaplan E, Taylor S, Thomas CR, Harris J (1993) The functional assessment of cancer-therapy scale - delevopment and validation of the general measure. J Clin Oncol 11(3):570–579
Kwon IG, Ryu E, Noh GO, Sung YH (2012) Health-related quality of life in cancer patients between baseline and a three-year follow-up. Eur J Oncol Nurs 16(2):131–136. https://doi.org/10.1016/j.ejon.2011.05.004
Petrick JL, Reeve BB, Kucharska-Newton AM, Foraker RE, Platz EA, Stearns SC, Han XS, Windham BG, Irwin DE (2014) Functional status declines among cancer survivors: trajectory and contributing factors. J Geriatr Oncol 5(4):359–367. https://doi.org/10.1016/j.jgo.2014.06.002
Linden W, Vodermaier A, MacKenzie R, Greig D (2012) Anxiety and depression after cancer diagnosis: prevalence rates by cancer type, gender, and age. J Affect Disord 141(2–3):343–351. https://doi.org/10.1016/j.jad.2012.03.025
Choi EP, Wong CK, Tsu JH, Chin WY, Kung K, Wong CK, Yiu MK (2016) Health-related quality of life of Chinese patients with prostate cancer in comparison to general population and other cancer populations. Support Care Cancer 24(4):1849–1856. https://doi.org/10.1007/s00520-015-2980-6
Davis JW, Kuban DA, Lynch DF, Schellhammer PF (2001) Quality of life after treatment for localized prostate cancer: differences based on treatment modality. J Urol 166(3):947–952. https://doi.org/10.1016/s0022-5347(05)65870-3
Rannestad T, Skjeldestad FE, Platou TF, Hagen B (2008) Quality of life among long-term gynaecological cancer survivors. Scand J Caring Sci 22(3):472–477. https://doi.org/10.1111/j.1471-6712.2007.00557.x
World Health Organization (1990) Cancer pain relief and palliative care. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser 804:1–75
The ACTION Study Group (2017) Health-related quality of life and psychological distress among cancer survivors in Southeast Asia: results from a longitudinal study in eight low- and middle-income countries. BMC Med 15(1):10. https://doi.org/10.1186/s12916-016-0768-2
Cheville AL (2009) Cancer-related fatigue. Phys Med Rehabil Clin N Am 20(2):405−+. https://doi.org/10.1016/j.pmr.2008.12.005
Jefford M, Ward AC, Lisy K, Lacey K, Emery JD, Glaser AW, Cross H, Krishnasamy M, McLachlan SA, Bishop J (2017) Patient-reported outcomes in cancer survivors: a population-wide cross-sectional study. Support Care Cancer 22(22):3171–3179. https://doi.org/10.1007/s00520-017-3725-5
Acknowledgements
We would like to acknowledge contributions from Dr. Mariko Carey and Dr. Sandra Ieropoli for developing the survey tool and overseeing data collection. We would also like to acknowledge the contribution of Ms. Helen Farrugia, Head of the Victorian Cancer Registry. We give our thanks and respect to the time and effort our survey participants gave to the project.
Funding
Funding for this study was provided by the Cancer Council Victoria (institutional funding).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 32.8 kb)
Rights and permissions
About this article
Cite this article
Marco, D.J.T., White, V.M. The impact of cancer type, treatment, and distress on health-related quality of life: cross-sectional findings from a study of Australian cancer patients. Support Care Cancer 27, 3421–3429 (2019). https://doi.org/10.1007/s00520-018-4625-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4625-z