Abstract
Purpose
The aims of this study were to determine if quality of life (QOL) among Arab Muslim hematopoietic stem cell transplantation (HSCT) survivors differs from that of a healthy matched comparison group and to examine the relationships of demographic and medical variables and perceived social support with post-HSCT QOL.
Methods
HSCT survivors (n = 63) were recruited from the King Hussein Cancer Center outpatient clinic. A matched (age, gender, education), healthy comparison group (n = 63) was recruited through public advertisements. Participants completed the EORTC-30 QOL scale and the Medical Outcomes Study Social Support Survey.
Results
Differences were found between the Arab Muslim HSCT survivor and healthy comparison groups for physical functioning (p < .0001), role functioning (p < .01), social functioning (p < .0001) QOL domains, and an overall symptom score (p = .003) with the HSCT group reporting poorer status than the healthy comparison group. Effect sizes for the three QOL domains ranged from .50 (role functioning) to 1.20 (social functioning). No significant difference was noted between the Arab Muslim HSCT and comparison groups in emotional and cognitive QOL domains. Higher overall symptom scores were significantly associated with poorer QOL across all QOL domains.
Conclusion
Similar to prior research with HSCT survivors, results suggest that HSCT has a significant negative impact on QOL. However, despite this general similarity, results suggest that the needs and experience of Muslim Arab HSCT survivors might differ from those of Western HSCT survivors in the social and emotional QOL domains. Given growing numbers of Arab and Muslim cancer survivors in the USA and other Western countries, future research is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hematopoietic stem cell transplantation (HSCT) is the treatment of choice for a number of cancers including Hodgkin’s disease, non-Hodgkin’s lymphoma, and leukemia [1, 2]. With HSCT, cure is possible for a high percentage of patients [2]. The use of HSCT for malignant and non-malignant diseases has increased dramatically in recent years [3]. Although HSCT is largely successful, it may negatively influence quality of life (QOL) [4]. A better understanding of QOL in an HSCT population may help identify interventions that will improve patient care [5] and guide rehabilitation programs that assist survivors to overcome any negative consequences of HSCT.
Most of the research to date on the effect of HSCT on QOL has been conducted using Western patient populations, primarily those from the USA, Canada, and Europe. Generalization to patients from other cultures may not be appropriate. Culture helps individuals in dealing with situations that appear to be difficult and unpredictable [6]. Culturally specific information on QOL in HSCT survivors would help to identify effective interventions. A lack of understanding of the experience of HSCT survivors within the context of their culture can create barriers that interfere with survivors’ health outcomes.
The number of hematopoietic stem cell transplants performed in Jordan increased significantly following the opening of the King Hussein Cancer Center (KHCC) in 1997. Because the culture of Jordan differs from that of Western cultures in terms of social, economic, and religious dimensions, findings obtained in studies of Western HSCT survivors may not apply to Arab Muslim HSCT survivors. Jordan is characterized as an Arab, Islamic country; 95 % of its population is Muslim [7]. Specific characteristics of this population that may differ from other parts of the world include the existence of strong family ties, abiding faith, reticence to discuss personal matters, and strong community relations [8]. Islam, whether practiced in the USA or Jordan, can also have a major influence on an individual’s health and involvement with health care [6, 9, 10]. Therefore, coping and adjustment in Arab Muslim HSCT survivors may differ from HSCT survivors in Western nations. Unfortunately, no research has been conducted regarding the QOL of these Arab Muslim survivors.
In addition to improving the care of Arab Muslims who reside in their country of origin, the outcomes of this study may or may not have the potential to assist health care professionals to better understand the needs of a growing number of Arabs and Muslims who have cancer or have undergone HSCT in Western countries including the USA. The estimated number of Muslims in the USA currently is seven million, and they come from a variety of ethnic backgrounds and national origins [9, 10]. The major subgroups among Muslim Americans are Arabs, South Asians, and US-born African Americans [10]. It was estimated that the number of Muslims in Western Europe alone was 11.3 million in 2010 [11]. The number of Muslims is expected to increase in Europe, Canada, and the USA over the next two decades [12, 13].
There may be negative physical, emotional, role, and/or social consequences associated with HSCT [14–17]. These consequences may be related to the toxicity of the procedure, social isolation throughout the transplant period, uncertainty regarding treatment outcomes, changes in usual role, threat to personal and future goals, and short- and long-term side effects [18]. Results of possible outcomes of the HSCT include difficulties in daily activities, irritability, fears and anxiety related to health concerns, depression, financial problems, and fatigue [16, 18]. Overall, QOL can be adversely influenced.
Several studies evaluating HSCT survivors’ QOL have used a healthy comparison group or general population normative data. Findings suggest that HSCT treatment can impact one or more QOL domains. In comparison with normative US and European population references, several studies found that HSCT negatively influences physical and role functioning [15, 16, 19] and may lead to emotional impairment [15, 19]. HSCT also has a negative impact on one or more domains of social functioning [14, 15, 19, 20]. Survivors frequently experience both short- and long-term physical symptoms [19, 21], and fatigue was found to interfere with daily activities [14, 16].
Social support has been found to decrease mortality [22], contribute to healthy lifestyles [23], and improve QOL [24]. In relation to HSCT, social support was positively associated with improved psychological and cognitive functioning following transplant [25, 26]. Greater social support was associated with less depression and anxiety and better cognitive functioning. Bush et al. [27] reported that inadequate social support was the most distressing hardship during long-term survival. The specific aims of this study were to (a) determine if QOL among Arab Muslim HSCT survivors differs from that of a healthy comparison group matched on age, sex, and education and (b) examine the relationships of demographic and medical variables and perceived social support with post-HSCT QOL.
Methods
Design and Sample
A cross-sectional comparative study was conducted with HSCT survivors (n = 63) and healthy participants (n = 63). KHCC is the only specialized cancer center in Jordan. Inclusion criteria for survivors were (a) age 18 years or older, (b) at least 3 months post-HSCT with no evidence of disease, (c) not hospitalized during the study, (d) not known to have a chronic disease (e.g., heart failure, renal failure, and liver failure), (e) no known major psychiatric problems (e.g., schizophrenia and major depression) prior to the HSCT procedure, and (f) able to read and write Arabic. The healthy comparison group was recruited through advertisements placed in public areas. Inclusion criteria for the comparison group were the same as those for the survivors excluding the HSCT experience. Participants in the comparison group were matched with survivors on age (5 ± years), sex, and level of education.
Instruments
European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30 (EORTC QLQ-C30)
This instrument is a 30-item, self-report multidimensional measure and consists of scales measuring functioning in five QOL domains: physical, role, emotional, cognitive, and social [28]. It also includes multi-item symptom scales and two items to measure overall QOL and health. The first 28 items are answered on a four-point Likert scale ranging from 1, “not at all,” to 4, “very much.” The last two items (overall QOL and overall health) are rated on a seven-point Likert scale ranging from 1, “very poor,” to 7, “excellent.” All of the functional scales and single-item measures are transformed to a 0–100 scale. Higher scores indicate a higher level of functioning and higher level of QOL except for the symptom scales where higher scores indicate greater problems. This measure has been translated into and validated in 38 languages including Arabic. It has satisfactory psychometric properties when tested with culturally diverse groups [29]. An overall symptom score was obtained by calculating the mean of the transformed scores for the fatigue, nausea and vomiting, and pain subscales and all other symptom item scores except for the financial difficulties item score [30].
Medical Outcomes Study Social Support Survey (MOS-SSS)
MOS-SSS is a 19-item self-report questionnaire that assesses perceived functional support [31]. It has four social support subscale scores (emotional/informational, affectionate, tangible, and positive social interaction) and an overall social support index. All subscale and overall support raw scores were standardized by transforming them to a 0–100 scale. Higher scores indicate a higher level of support [31]. The MOS-SSS was translated into Arabic by the investigator. Cronbach’s alpha for the overall social support scale was .93. Cronbach’s alphas for the subscales were .79 for tangible support, .87 for emotional-informational support, .82 for affectionate support, and .86 for positive social interaction support. The inter-correlations among the four subscales in this study ranged from .55 to .70.
Demographics and medical characteristics.
Data were collected on age, sex, education, annual income, employment status, and marital status. For HSCT survivors, medical records were used to obtain data on type of transplant and number of months post-HSCT.
Procedure
This study received approval from the University of Kentucky Institutional Medical Review Board and the KHCC Institutional Review Board. The ethical standards of the Declaration of Helsinki were followed in conducting this study. Seventy-six HSCT survivors were identified from the KHCC patient list as potential participants. Of these survivors, 10 lived outside Jordan, 1 was hospitalized at the time of data collection, 1 survivor refused to participate, and 1 did not provide a correct address. HSCT recipients who met the inclusion criteria were contacted by the investigator or the Bone Marrow Transplant coordinator at KHCC during their visit to the clinic or by phone. The study was explained, and those who agreed to participate were consented and given a detailed explanation about the study including the purpose, risks, benefits, and procedures. Following recruitment of the HSCT group, the healthy comparison group was recruited through advertisements.
The data were analyzed using SPSS (version 22.0; SPSS Inc., Chicago, IL). Alpha was set at p < .05. Descriptive statistics were used to describe participants’ responses to all scales and subscales. To assess differences in QOL, symptom severity, and perceived social support between the HSCT survivors and the comparison group, one-way analysis of covariance (ANCOVA) was used. The effect sizes were calculated for each outcome to evaluate the clinical significance of results. An effect size greater than .50 was considered clinically important [32].
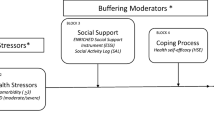
Hierarchical regression was used to examine the association of demographic, clinical, and social support variables with the five EORTC QOL domain scores of the HSCT survivors. For each domain score, a set of demographic variables was entered at step 1 (age, sex, education, marital status), the MOS overall support index score was entered at step 2, and clinical variables (overall symptom score, months post-HSCT, type of transplant) were entered at step 3. To identify the possibility of multicollinearity among the independent variables, the variance inflation factor (VIF) and tolerance statistics were computed. Multicollinearity was not a problem since the VIF values were less than 3.
Results
The mean age was 35.4 years (range, 19–63) for the HSCT group and 35.3 years (range, 18–62) for the healthy comparison group. The two groups did not differ on mean age. The mean number of months post-HSCT was 20.2 (range, 4–60). Among HSCT survivors, 31 (49 %) were diagnosed with leukemia, 18 (29 %) were diagnosed with lymphoma, 10 (16 %) were diagnosed with multiple myeloma, and the remaining four had other cancer diagnoses. Most survivors (n = 37; 59 %) had allogeneic transplants and 26 (41 %) had autologous transplants. Additional demographic characteristics of the participants are presented in Table 1. The survivor group was more likely to have poor economic status (p = 0.043) and be unemployed (p < .0001) relative to the healthy comparison group.
Table 2 shows a comparison of the HSCT and healthy comparison groups on QOL, symptoms, and perceived social support. ANCOVA was used to compare the groups. Because the two groups differed on economic status, this variable was included as a covariate. Significant differences were found for physical functioning, role functioning, and social functioning; the HSCT group reported poorer health status than the healthy comparison group. Effect sizes for these three QOL domains ranged from .50 (role functioning) to 1.20 (social functioning).
The HSCT and healthy comparison groups were significantly different on 8 of the 10 symptom indices examined (all p values < .05). Scores for all symptom indices, except for insomnia and constipation, were significantly higher in the HSCT group than in the healthy comparison group. Effect sizes for the eight symptom indices for which significant group differences were found ranged from 0.44 (fatigue) to 1.44 (financial difficulties). The effect size for the overall symptom index was 0.60. On the MOS social support scales, the HSCT group reported greater tangible and affectionate support and had a higher overall support index. Effect sizes for these three social support indices ranged from 0.32 (overall support index) to 0.52 (tangible support).
Hierarchical multiple regression was performed to examine how demographic and clinical variables, along with perceived social support and symptom scores, contributed to variance in the five EORTC QOL domain scores in the HSCT survivor group (see Table 3). The eight predictor variables accounted for a significant proportion of variance in each of the five QOL domain scores with the proportion of variance accounted for ranging from 34.6 % (cognitive domain) to 55.6 % (physical domain). For the most part, demographic variables did not show a consistent pattern of association with any of the five EORTC QOL domain scores. However, there was some evidence suggesting that the MOS overall social support score was associated with variance in emotional and cognitive domain scores; greater social support was associated with better QOL in these domains. In contrast, clinical variables were significantly associated with all five QOL domain scores, with the increment in variance accounted for by addition of clinical variables ranging from 16.6 % (cognitive domain) to 38.5 % (physical domain). Higher overall symptom scores were significantly associated with poorer QOL across all five QOL domains while longer time post-HSCT was significantly associated with better QOL in the Social domain.
Discussion
This study showed that HSCT has a distinct negative impact on physical, role, and social functioning of Muslim Arab survivors. The sizes of the deficits in these three areas were all clinically important as the effect size for all three exceeded .50—a criterion often used to indicate a clinically significant difference [32]. The effect sizes for physical and social functioning are particularly noteworthy as both exceeded 1.00. Deficit in role functioning indicated that Arab Muslim survivors had difficulty in performing their work, carrying out daily activities and enjoying their leisure time activities. In addition, the negative impact of HSCT was also seen in the symptom domain. The HSCT group reported significantly more symptoms for seven of the nine EORTC symptom items. Not surprisingly, they also scored significantly higher on the overall symptom index with the effect size for the symptom index being .60—again, a clinically important difference. These differences in physical, role, and social function as well as symptoms are not surprising and have been frequently demonstrated in studies of Western HSCT survivors’ QOL [14, 15, 19, 20].
Surprisingly, the HSCT and healthy comparison groups did not differ in the emotional QOL domain. Many studies of Western HSCT survivors have found a significant difference in distress and emotional QOL when comparing survivors to controls or norms [14, 15, 33]. The lack of a difference in the emotional QOL domain between the two groups in this study may be related to social desirability bias. People in the Arabic and Islamic culture may attempt to hide their weakness to maintain their traditional role in the community. The Arab Muslim community values discourage expressions of depression, anxiety, or other mental health issues [34, 35]. Using a self-report instrument like the EORTC to assess these issues may place cultural pressure on survivors to not admit to difficulties in emotional functioning. Health care providers need to be aware of this and take steps to ensure that Arab Muslim survivors have the opportunity to express their feelings and identify their needs in the emotional domain. Alternatively, Muslim Arab survivors may indeed experience fewer emotional difficulties and dysfunction due to the protective influence of Islamic beliefs on coping with illness. Muslims believe that God is the only healer for their diseases. They believe that being more connected with God allows them to feel more secure and keeps them away from the stressors of life [8, 36]. Consequently, these religious beliefs may foster better coping with the stresses of HSCT survivorship and result in less distress among Arab Muslim survivors.
Finally, the lack of difference in the emotional QOL domain between the HSCT group and the healthy comparison group may be due to the moderate to high social support perceived by the Arab Muslim survivors which stems from the strong community relations and family ties. HSCT survivors reported significantly greater social support than the comparison group. Survivors who perceived greater social support reported better emotional functioning. The lack of differences in the emotional QOL domain between survivors and the healthy comparison group has implications for the clinical management of Arab Muslim cancer survivors. Similar to Arab Muslim survivors, Western HSCT survivors perceived moderate to high social support [37, 38]. Further study is needed to explore the emotional impact of HSCT in Arab Muslim HSCT survivors and to identify why they may appear to report better emotional QOL than Western survivors of HSCT.
There was a huge, clinically important (effect size = 1.2) difference between the survivors and healthy comparison group in the social functioning QOL domain. This finding indicates that HSCT interfered markedly with family life and social activities. Several comparative studies conducted in the Western culture found only a small to moderate difference in social QOL domain between the two groups [14, 20, 33]. The large difference in social functioning in this current study may be related to the misconception and misunderstanding of cancer in the Arab Muslim community. Arab Muslim survivors may attempt to avoid possible negative perceptions of their condition within their community. Cancer patients and their families avoid talking about cancer diagnosis in public for fear that people will view this condition as a sign of death [39]. Consequently, Arab Muslim survivors may avoid interacting with people in the community to hide their physical symptoms and general appearance that may show their disease. Therefore, social functioning needs to be addressed before and after transplantation. Community education about cancer and patients’ needs is critical to change community opinions about cancer.
The non-significant difference between the HSCT and the comparison groups in the overall QOL might be due to the hope gained by having this procedure. Most survivors feel that a cure is possible for a high percentage of patients who experience this treatment. Kopp et al. [20] found that the EORTC overall QOL was significantly associated with the helplessness/hopelessness subscale of the Mental Adjustment to Cancer (MAC) scale which supports this lack of a difference between the two groups.
This study also examined demographic and clinical variables associated with QOL in Arab Muslim HSCT survivors. Clinical variables were associated with variance in all QOL domains. The most interesting finding was that the level of symptoms was the strongest predictor of the overall QOL and its domains. Consistent with this finding, two studies [21, 40] examined Western survivors who had experienced a HSCT and found that higher levels of symptoms were highly correlated with lower overall QOL. This finding addresses the importance of assessing and using different pharmacological and non-pharmacological interventions to manage survivors’ symptoms to improve their QOL. In contrast, demographic variables were not consistently associated with QOL in this study. Other studies of Western HSCT survivors found that age and employment status [4, 19], gender [19, 40], family income [4], and educational level [40] are significantly associated with QOL.
The cross-sectional design of this study limits causal attributions and is a weakness in terms of understanding factors that influence HSCT survivors’ QOL over time. More longitudinal research among Arab Muslim survivors is recommended. Another limitation is the small sample size. Since this study focused on Arab Muslim survivors in Jordan, it is not known if similar results would be found with Arab Muslim patients treated in Western countries. The findings of this study are not generalizable to Arab Muslim survivors residing in Western countries. Patients who were diagnosed with solid tumors at the time of transplantation were underrepresented. Further research is needed to understand how the QOL of Muslim survivors of solid tumors might differ from their Western counterparts.
In conclusion, this is the first study to address the QOL of HSCT survivors from an Arabic and Muslim country. Therein lies its primary value. Similar to Western HSCT survivors, Arab Muslim HSCT survivors reported significant deficits in physical, role, and social functioning. However, the experience of Arab Muslim HSCT survivors may be different from that of Western HSCT survivors in the social and emotional domains. The social functioning of Arab Muslim HSCT survivors may be more negatively affected than that of Western HSCT survivors. Conversely, the emotional functioning of Arab Muslim survivors may be less negatively affected when compared to that of Western HSCT survivors. Both of these findings may be due to unique aspects of the Arab Muslim culture. It is also noteworthy to mention that Arab Muslim survivors are just one subset of Muslim cancer survivors. In general, Muslims come from different ethnic backgrounds and live in countries around the world with the majority residing in Asia-Pacific and the Middle East regions. Given the large and growing population of Muslims in the USA, further research is essential to examine the potential unique needs and experience of Muslim cancer survivors.
References
Corsten MF, Shah K (2008) Therapeutic stem-cells for cancer treatment: hopes and hurdles in tactical warfare. Lancet Oncol 9(4):376–384
Rischer J, Scherwath A, Zander AR, Koch U, Schulz-Kindermann F (2009) Sleep disturbances and emotional distress in the acute course of hematopoietic stem cell transplantation. Bone Marrow Transplant 44(2):121–128. doi:10.1038/bmt.2008.430
Gratwohl AMD, Baldomero HBMS, Aljurf MMD, Pasquini MCMD, Bouzas LFMD, Yoshimi AMD et al (2010) Hematopoietic stem cell transplantation: a global perspective. JAMA 303(16):1617–1624
Wingard JR, Huang IC, Sobocinski KA, Andrykowski MA, Cella D, Rizzo JD et al (2010) Factors associated with self-reported physical and mental health after hematopoietic cell transplantation. Biol Blood Marrow Transplant 16(12):1682–1692. doi:10.1016/j.bbmt.2010.05.017
Pidala J, Anasetti C, Jim H (2010) Health-related quality of life following haematopoietic cell transplantation: patient education, evaluation and intervention. Br J Haematol 148(3):373–385. doi:10.1111/j.1365-2141.2009.07992.x
Silbermann M, Hassan EA (2011) Cultural perspectives in cancer care: impact of Islamic traditions and practices in Middle Eastern countries. J Pediatr Hematol Oncol 33(Suppl 2):S81–S86
U.S. Department of State (2005). Jordan: International Religious Freedom Report 2005. http://www.state.gov/j/drl/rls/irf/2005/51602.htm. Accessed 16 August 2013
Wehbe-Alamah H (2008) Bridging generic and professional care practices for Muslim patients through use of Leininger's culture care modes. Contemp Nurse 28(1–2):83–97
Padela AI, Gunter K, Killawi A, Heisler M (2012) Religious values and healthcare accommodations: voices from the American Muslim community. J Gen Intern Med 27(6):708–715
Padela AI, Killawi A, Forman J, DeMonner S, Heisler M (2012) American Muslim perceptions of healing: key agents in healing, and their roles. Qual Health Res 22(6):846–858
Pew Research (2011) Religion and Public Life Project: The Future of the Global Muslim Population. http://www.pewforum.org/2011/01/27/future-of-the-global-muslim-population-regional-europe/. Accessed 5 May 2014
Johnson T (2011) Muslims in the United States. Council on Foreign Relations. http://www.cfr.org/united-states/muslims-united-states/p25927. Accessed 13 May 2013
Ezenkwele UA, Roodsari GS (2013) Cultural competencies in emergency medicine: caring for Muslim-American patients from the Middle East. J Emerg Med 45(2):168–174
Andrykowski MA, Bishop MM, Hahn EA, Cella DF, Beaumont JL, Brady MJ et al (2005) Long-term health-related quality of life, growth, and spiritual well-being after hematopoietic stem-cell transplantation. J Clin Oncol 23(3):599–608. doi:10.1200/JCO.2005.03.189
Syrjala KL, Langer SL, Abrams JR, Storer BE, Martin PJ (2005) Late effects of hematopoietic cell transplantation among 10-year adult survivors compared with case-matched controls. J Clin Oncol 23(27):6596–6606. doi:10.1200/JCO.2005.12.674
Wettergren L, Sprangers M, Bjorkholm M, Langius-Eklof A (2008) Quality of life before and one year following stem cell transplantation using an individualized and a standardized instrument. Psychooncology 17(4):338–346. doi:10.1002/pon.1240
Saleh US, Brockopp DY (2001) Quality of life one year following bone marrow transplantation: psychometric evaluation of the quality of life in bone marrow transplant survivors tool. Oncol Nurs Forum 28(9):1457–1464
Mosher CE, Redd WH, Rini CM, Burkhalter JE, DuHamel KN (2009) Physical, psychological, and social sequelae following hematopoietic stem cell transplantation: a review of the literature. Psychooncology 18(2):113–127
Bieri S, Roosnek E, Helg C, Verholen F, Robert D, Chapuis B et al (2008) Quality of life and social integration after allogeneic hematopoietic SCT. Bone Marrow Transplant 42(12):819–827. doi:10.1038/bmt.2008.253
Kopp M, Holzner B, Meraner V, Sperner-Unterweger B, Kemmler G, Nguyen-Van-Tam DP et al (2005) Quality of life in adult hematopoietic cell transplant patients at least 5 yr after treatment: a comparison with healthy controls. Eur J Haematol 74(4):304–308. doi:10.1111/j.1600-0609.2004.00402.x
Cohen MZ, Rozmus CL, Mendoza TR, Padhye NS, Neumann J, Gning I et al (2012) Symptoms and quality of life in diverse patients undergoing hematopoietic stem cell transplantation. J Pain Symptom Manag 44(2):168–180. doi:10.1016/j.jpainsymman.2011.08.011
Eng PM, Rimm EB, Fitzmaurice G, Kawachi I (2002) Social ties and change in social ties in relation to subsequent total and cause-specific mortality and coronary heart disease incidence in men. Am J Epidemiol 155(8):700–709
Pirie PL, Rooney BL, Pechacek TF, Lando HA, Schmid LA (1997) Incorporating social support into a community-wide smoking-cessation contest. Addict Behav 22(1):131–137
Sammarco A, Konecny LM (2010) Quality of life, social support, and uncertainty among Latina breast cancer survivors. Oncol Nurs Forum 35(5):844–849
Hochhausen N, Altmaier EM, McQuellon R, Davies SM, Papadopolous E, Carter S et al (2007) Social support, optimism, and self-efficacy predict physical and emotional well-being after bone marrow transplantation. J Psychosoc Oncol 25(1):87–101
Rini C, Redd WH, Austin J, Mosher CE, Meschian YM, Isola L et al (2011) Effectiveness of partner social support predicts enduring psychological distress after hematopoietic stem cell transplantation. J Consult Clin Psychol 79(1):64–74. doi:10.1037/a0022199
Bush NE, Haberman M, Donaldson G, Sullivan KM (1995) Quality of life of 125 adults surviving 6-18 years after bone marrow transplantation. Soc Sci Med 40(4):479–490
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85(5):365–376
Osoba D, Aaronson N, Zee B, Sprangers M, te Velde A (1997) Modification of the EORTC QLQ-C30 (version 2.0) based on content validity and reliability testing in large samples of patients with cancer. The Study Group on Quality of Life of the EORTC and the Symptom Control and Quality of Life Committees of the NCI of Canada Clinical Trials Group. Qual Life Res 6(2):103–108
Jeppe CY, Becker P, Smith MD (2013) Post-Frey procedure quality of life in South African patients with painful chronic pancreatitis. JOP: J Pancreas 14(1):21–30. doi:10.6092/1590-8577/933
Sherbourne CD, Stewart AL (1991) The MOS Social Support Survey. Soc Sci Med 32(6):705–714
Norman GR, Sloan JA, Wyrwich KW (2003) Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care 41(5):582–592. doi:10.1097/01.MLR.0000062554.74615.4C
Sutherland HJ, Fyles GM, Adams G, Hao Y, Lipton JH, Minden MD et al (1997) Quality of life following bone marrow transplantation: a comparison of patient reports with population norms. Bone Marrow Transplant 19(11):1129–1136. doi:10.1038/sj.bmt.1700806
Weatherhead S, Daiches A (2010) Muslim views on mental health and psychotherapy. Psychol Psychother: Theory Res Pract 83(Pt 1):75–89
Ciftci A, Jones N, Corrigan PW (2013) Mental health stigma in the Muslim community. J Muslim Ment Health 7 (1):17-32. http://hdl.handle.net/2027/spo.10381607.0007.102
Ahmad F, Muhammad M, Abdullah AA (2011) Religion and spirituality in coping with advanced breast cancer: perspectives from Malaysian Muslim women. J Relig Health 50(1):36–45
Jenks Kettmann JD, Altmaier EM (2008) Social support and depression among bone marrow transplant patients. J Health Psychol 13(1):39–46
Nenova M, DuHamel K, Zemon V, Rini C, Redd WH (2013) Posttraumatic growth, social support, and social constraint in hematopoietic stem cell transplant survivors. Psychooncology 22(1):195–202
Mellon S, Gauthier J, Cichon M, Hammad A, Simon MS (2013) Knowledge, attitudes, and beliefs of Arab-American women regarding inherited cancer risk. J Genet Couns 22(2):268–276. doi:10.1007/s10897-012-9546-2
Prieto JM, Saez R, Carreras E, Atala J, Sierra J, Rovira M et al (1996) Physical and psychosocial functioning of 117 survivors of bone marrow transplantation. Bone Marrow Transplant 17(6):1133–1142
Acknowledgments
The authors would like to thank the King Hussein Cancer Center in Jordan for their assistance in conducting this study. Financial support for this research was provided by the American Oncology Nursing Society.
Conflicts of interest
We declare that all authors have no conflicts of interest to disclose. We have full control of all primary data and agree to allow the Journal to review our data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alaloul, F., Brockopp, D.Y., Andrykowski, M.A. et al. Quality of life in Arab Muslim cancer survivors following hematopoietic stem cell transplantation: comparison with matched healthy group. Support Care Cancer 23, 2157–2164 (2015). https://doi.org/10.1007/s00520-014-2583-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-014-2583-7