Abstract
Background
While the impact of various treatments on myeloma patients’ health-related quality of life (HRQL) has been reported, the impact of a treatment-free interval (TFI) is currently unclear. The aims of this study were to assess if (1) a TFI is associated with a better HRQL vs. other treatment phases and (2) the length of the TFI influences HRQL.
Methods
A cross-sectional postal survey was conducted in the UK. The survey was sent to 605 multiple myeloma patients via the charity Myeloma UK and asked patients to rate their HRQL using the European Organisation for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire Core 30 (QLQ-C30), EORTC QLQ-MY20 and the EQ-5D. The results were analysed using ordinary least squares regression.
Results
Surveys of 402 (67 %) were returned; 370 (61 %) were considered eligible for analysis. Results demonstrated that being in a first TFI relative to other treatment phases and experiencing a longer TFI were significantly associated with better HRQL as assessed by various domains of the QLQ-C30, MY20 and EQ-5D.
Conclusion
Patients enjoy better HRQL when in their first TFI, and the length of the TFI also positively impacts on HRQL This information may be important for patients and their physicians making treatment decisions and has implications for treatment protocols incorporating extended therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple myeloma (MM) is an incurable haematological cancer resulting from the accumulation of malignant plasma cells in the bone marrow and often associated with the production of a monoclonal protein. Clinical presentation includes bone pain, lytic lesions, fractures, renal failure, repeated infections, anaemia and hypercalcaemia [23, 24]. Although it is a rare condition, multiple myeloma is the second most common haematologic malignancy. In the UK, the incidence of multiple myeloma in 2007 was 4,040, with an overall incidence rate of 6.6 per 100,000 and a male/female ratio of 1.24:1; the crude rate of deaths and mortality in 2008 was 4.3 per 100,000 [5].
Multiple myeloma is associated with significant morbidity and mortality. Until the early 1980s, MM caused a slow progressive decline in health status until death, which, on average, was approximately 2 years following diagnosis [24]. In the last decade, the increased use of high-dose therapy, the recent introduction of novel therapies and improvement in patient care have translated into better outcomes for patients. A recent study of 2,981 patients diagnosed with MM, between 1971 and 2006 [16], found that those diagnosed in the last decade had a 50 % improvement in overall survival compared with patients diagnosed prior to this (44.8 vs. 29.9 months; P < 0.001). Because curative therapies are not yet available, the broad aims of treatment are to control disease, maximise quality of life and prolong survival. Thus, treatment is initiated only in patients with symptomatic disease, i.e. with MM-related organ or tissue impairment [20]. The incorporation of high-dose therapy (HDT) with autologous stem cell transplantation (ASCT) into a front-line treatment strategy remains standard of care in younger and fitter patients [4]. Such patients are initially treated using induction regimen of three to six cycles, followed by mobilisation of peripheral blood stem cells for use in HDT and ASCT. Current recommended induction regimens include at least one novel agent: thalidomide, bortezomib or lenalidomide. In the UK, this would generally be thalidomide, while patients entered on clinical trials may receive bortezomib or lenalidomide containing regimens. For older and/or less fit patients (due to comorbidities or poor performance status) in whom HDT is not planned, initial therapy should consist of thalidomide or bortezomib, usually in combination with an alkylating agent and a steroid. Ideally, treatment decisions should be reviewed in a multi-disciplinary team meeting and take into account individual patient factors and patient choice [3].
Current front-line therapies produce durable disease responses in up to 80 % of patients. After treatment stops, patients enter a ‘plateau phase’, defined as a period of remission where parameters of disease may persist but are stable, and there is no clinical progression of organ damage. During plateau phase, many patients enjoy reasonable quality of life (QOL) and well-being, and several patients return to pre-morbid lifestyles including work. This suggests patient well-being, and QOL will increase with length of time off chemotherapy or treatment-free interval (TFI). This depends on several factors, including the chemotherapy regimen received, whether a maintenance therapy was administered subsequently and intrinsic disease-related factors, such as underlying genetics and disease stage. Disease relapse is often heralded by reappearance of, or rise in, the M-protein in serum or urine, whilst re-initiation of chemotherapy is often guided by clinical need as judged, for example, by the appearance of new bone lesions, progressive anaemia, increasing infections, rapidly rising serum paraprotein or significant Bence Jones proteinuria. The choice of treatment regimen at this stage is dictated as much by availability of costly drugs and clinical trials, as well as disease and patient-related factors, including timing of relapse, age and comorbidities, regimen-related toxicities, persisting toxicities from previous therapy and patient preference [3]. Disease response to salvage regimens at first relapse has improved with the use of novel agents, and overall response rates (ORR) of 40–82 % [22] are reported. Thalidomide, bortezomib and lenalidomide are the three most often used agents in treating relapsed patients in the UK [3]. Thus, around half of patients will enter a second plateau phase following therapy for first relapse, with the opportunity to enjoy a further period of TFI. Inevitably, subsequent relapses will occur, necessitating further lines of treatment, with lower likelihood of response and shorter plateau phases.
In evaluating the effectiveness of non-curative treatments, clearly, overall survival is not the only parameter of benefit. Toxicity profiles (and consequent need for supportive medications), mode of administration and depth of response are important, as are ORR, progression-free survival, time to next treatment and TFI. Many of these factors are important because of the impact on patient-reported outcomes or health-related quality of life (HRQL). This is particularly relevant as patients with MM are living longer, and cost-effectiveness analyses will include data on HRQL. Here, HRQL needs to be in the form of a utility (e.g. preference weighted) so that quality-adjusted life years can be estimated. The need for HRQL assessment in MM has been recognised in a number of clinical trials [17]; indeed, a specific MM HRQL questionnaire (the MY20) has been developed and validated by the European Organisation for Research and Treatment of Cancer (EORTC) [6, 25]. To the best of our knowledge, however, all MM HRQL data collected to date is treatment specific and does not reflect the whole treatment pathway [2, 9, 13, 17–19]. Importantly, we do not have information on HRQL in patients in their TFI and how this differs from the HRQL whilst on therapy. It would also be valuable to know if HRQL differs between first-line therapy and subsequent therapy, and if it continues to recover or improve with length of TFI. Such data would allow for a more accurate assessment of the benefits of different treatments for cost-effectiveness analyses and would enable patients and their physicians to make better informed treatment decisions together.
There is no published HRQL data which describe the treatment phases and TFIs of patients with MM in detail. Therefore, the present study was designed to explore HRQL in MM to address this need. More specifically, the study was designed to explore two key research questions: (1) Is HRQL better during a TFI relative to other treatment phases? (2) Is a longer TFI associated with better HRQL?
Materials and methods
Design and participants
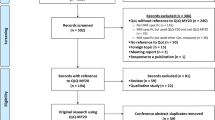
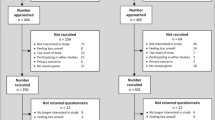
A cross-sectional postal survey was conducted in the UK. Potential participants were identified by Myeloma UK, the only MM specific charitable organisation in the UK, who sent copies of the survey and a return stamped addressed envelope to all patients listed in their database (n = 605). There was a 67 % response rate, with a total of 402 completed surveys returned. All patients with a self-reported diagnosis of multiple myeloma were eligible for inclusion; survey data was only excluded from analysis if the respondent failed to clearly identify their current treatment phase in the socio-demographic/clinical report form. Written informed consent was provided by all participants.
Survey
The survey included a socio-demographic/clinical report form and three quality of life measures: the EORTC Cancer Quality of Life Questionnaire Core 30 (QLQ-C30 [1]) and its associated multiple myeloma specific module (EORTC QLQ-MY20 [6, 25]) and the EQ-5D [10, 15].
The socio-demographic/clinical report form included questions related to age, gender, date of diagnosis, current treatment phase and current or last treatment with start and completion dates. As the correct identification of current treatment phase was essential to the main aim of the study, a glossary of treatment phase terms was provided. This glossary described the terms: ‘first-line treatment’, ‘second-line treatment’, ‘later stage’ and ‘first treatment-free interval’. First-line treatment was described as the first treatment received to treat myeloma, and it was further explained that, if the patient had changed treatments due to unresponsiveness or side effects, these additional treatments still counted as ‘first line’. Second-line treatment was described as the treatment received after the first relapse; this may be a repeat of the first line treatment if the response had been good or an alternative treatment. The first TFI was described as the first time a patient is classed as being in remission; the patient may be taking supportive treatments (e.g. painkillers or anaemia medication) but is not receiving any active myeloma or maintenance treatment during this time. Finally, later stage was described as the time from second remission onwards. In order to ensure that the glossary was comprehensive and aided patients classification of their treatment phase, a pilot study, including a patient cognitive debrief interview, was conducted with ten multiple myeloma patients during the development of the glossary. The patients were recruited by Myeloma UK through their support groups, and the interviews were conducted over the phone by a trained researcher. Initial interviews prompted the expansion of the first-line treatment description to include reference to changing treatments; the final version of the glossary was deemed clear, comprehensive and helpful in assisting the classification of their treatment phase by the patients.
The EORTC QLQ-C30 contains 30 items which include five functional scales (physical, role, cognitive, emotional and social), three symptom scales (fatigue, nausea and vomiting and pain) and six individual items (global quality of life, dyspnoea, sleep disturbance, appetite loss, constipation, diarrhoea and financial difficulties) [1]. Each is converted into a scale ranging from 0 to 100. For the functional scales and the global quality of life scale, higher scores represent a better health state, whereas for the symptom items/scales, lower scores represent a better health state.
The EORTC QLQ-MY20 was developed as an additional module for the QLQ-C30 and is composed of 20 multiple myeloma specific items [6, 25]. These items are scored as four independent sub-scales: two functional scales (body image and future perspective) and two symptom scales (disease symptoms and side effects of treatment). Each is converted into a scale ranging from 0 to 100. For the functional scales, higher scores represent a better health state, whereas for the symptom scales, lower scores represent a better health state.
The EQ-5D is a standardised instrument for use as a measure of health outcome, particularly in health economic evaluations. It is a three-level, five-dimensional questionnaire in which the domains include mobility, self-care, usual activity, pain/discomfort and anxiety/depression. Participants are asked to indicate their current level of health by checking one of three boxes for each domain ranging from no problems to extreme or severe problems. Responses to the five domains are used to derive health utilities, which represent preferences for different health states and, when combined with life duration information, enable the calculation of quality-adjusted life years for economic evaluations. In this study, health utilities were derived from the EQ-5D using the UK general population weights [8], which provide a potential range of scores from −0.59 to 1.0 (where a score of 1 represents full health, 0 represents dead and less than 0 represents worse than dead). In addition to the five domains, participants also rate their current health on a scale of 0 to 100 (100 = best health state) on a visual analogue scale (VAS).
The survey also included a cover letter from Myeloma UK which provided details of the study sponsor and explained that the aim of the study was to better understand the quality of life of patients with multiple myeloma. At the end of the information sheet, potential participants were asked to indicate their consent to participate and were instructed to return the consent form with the survey.
Statistical analyses
Descriptive statistics, for the sample as a whole and by treatment phase, were generated for each of the QLQ-C30 and MY20 scales, as well as the EQ-5D utility value and VAS rating. Missing data were treated in line with published scoring procedures for the QLQ-C30 and the MY20 [12]; however, it is not possible to derive a utility value from the EQ-5D when any domain scores are missing.
In order to explore the association between health-related quality of life and being in a treatment-free interval relative to other treatment phases, 11 ordinary least squares (OLS) multiple regression analyses were conducted with the five QLQ-C30 functional scales, the four MY20 scales and the EQ-5D utility index and VAS rating as dependent variables. The four different treatment phases of myeloma identified in the survey (first line, first treatment-free interval, second line and later phase) were dummy coded, with the first treatment-free interval group as the reference group, and included as predictors.
The impact of the length of a TFI on HRQL was also explored using OLS regressions with TFI length (measured in days) as the predictor and the same dependent variables as listed above. The TFI length was calculated based on the date the survey was completed minus the last treatment date, for all those patients who classified themselves as currently experiencing their first TFI.
Age and gender were also included as potential covariates; however, no significant associations were identified, and they were removed from the reported analysis. Given the exploratory nature of this study, an uncorrected critical alpha of 0.05 was adopted throughout. All regression analyses were screened for violation of regression assumptions, and none were identified. All analyses were conducted using SPSS version 17.
Results
Of the 402 surveys received, 32 cases were excluded due to lack of a self-reported MM diagnosis (n = 9) or failure to clearly identify treatment phase (n = 23), giving a total for analysis of 370 patients. Within the TFI group, 18 patients did not provide sufficient date information to conduct the TFI length analysis; thus, 159 out of the total 177 TFI patients were included in the analysis.
The demographic and treatment details, for the sample as a whole and by current treatment phase, are provided in Table 1. In terms of age and gender, all groups display similar distributions. With regard to treatment phase distribution, the first-line treatment group is small (n = 12), which should be considered when evaluating any comparisons involving this group. It is also worth noting that 70 % of the ‘TFI’ group stated that ‘stem cell transplant’ was their last treatment, whereas the second-line treatment and later stage groups have a more equal ‘last therapy’ spread.
Treatment phase analysis
Descriptive statistics, for the sample as a whole and by treatment phase, were generated for each of the QLQ-C30 and MY20 scales, as well as the EQ-5D utility value and VAS rating. As illustrated in Fig. 1, in all functional domains of the EORTC QLQ-C30 and MY20, the mean scores of the first treatment-free interval group track above all other treatment phases, indicative of higher functioning and thus better HRQL. Similarly, in Fig. 2, the first treatment-free interval group means track below all other treatment phases, indicative of lower symptomology and thus better HRQL, with the exception of the QLQ-C30 ‘appetite loss’ and ‘financial difficulties’, and MY20 ‘disease symptoms’. The EQ-5D results, presented in Table 2, also demonstrated a superior HRQL profile amongst those in their first treatment-free interval compared to other treatment phases.
The OLS multiple regression analyses largely supported this pattern of results (Table 3). The EORTC QLQ-C30 physical, role, emotional and social functioning; MY20 future perspectives; side effects; body image; EQ-5D utility and VAS scores all demonstrated significantly positive associations between better HRQL and being in the first TFI relative to one or more of the other treatment phases. There were no significant differences between treatment phases for the MY20 disease symptoms scale or the QLQ-C30 cognitive functioning scale. Most of the measures of HRQL reduced significantly when patients moved from the first TFI to second-line and later treatment phase, rather than first-line treatment. The reduction in HRQL between first TFI and later treatment phase was of a greater magnitude than those associated with second-line treatment.
TFI length analysis
Prior to conducting the regression analyses, the ‘length of TFI’ (measured in days) predictor was log transformed due to its positively skewed distribution (3–5,973 days, median 762 days). Significant associations between a longer log TFI and better HRQL were found for the MY20 future perspectives (R 2 = 0.041, p = 0.011) and body image (R 2 = 0.051, p = 0.005) scales, the QLQ-C30 physical functioning (R 2 = 0.028, p = 0.036) and role functioning (R 2 = 0.035, p = 0.018) scales and the EQ-5D utility value (R 2 = 0.045, p = 0.008). As these significant associations related to a log-transformed predictor, the significant relationship identified was non-linear, with a steep rise in HRQL over the first year, which starts to plateau after 1.5–2 years. However, as the variance explained in each case was relatively low, a linear relationship with non-transformed TFI data was also explored. The linear relationship was also significant (p = 0.05), with HRQL increasing with TFI length. A hierarchical regression found no significant contribution of the non-linear relationship over and above the linear relationship.
Discussion
This study provided a cross-sectional view of the MM treatment pathway, with the aim of exploring the impact of the first TFI on MM patients’ HRQL. Overall, the results demonstrated that being in the first TFI was associated with better HRQL compared to other treatment phases, and that longer TFIs were largely associated with better HRQL. Gaining a better understanding of the relationship between HRQL and the first TFI could provide information for potential HRQL endpoints in randomised controlled trials [24], be a valuable aid to cost-effectiveness analyses and help inform clinical practice. In clinical practice, some treatments are used until disease progression [7, 20, 27, 28], while others are used for a set number of cycles allowing patients to benefit from a TFI prior to relapse [11, 14, 21]. A TFI resulting in an improvement in HRQL may be an important treatment benefit for patients. This study provides, for the first time, evidence for this relationship. While HRQL data has been published in relation to specific MM treatments, to our knowledge, this is the first study to report the impact of the first TFI on HRQL.
The survey response rate was high, and respondents represented the MM treatment pathway from first-line to later treatment phases. The gender and age distributions in all treatment phases were very similar, which is likely to account for the lack of any significant age or gender relationships with the HRQL-dependent variables. The descriptive statistics for the EORTC QLQ-C30 and MY20 all suggested that being in a TFI, relative to the other phases of MM assessed, was associated with better HRQL, with the exception of the MY20 disease symptom scale and QLQ-C30 cognitive scale. Given the small mean differences in some instances, this may reflect chance variation; however, it may also reflect the contribution of age rather than MM to the bone pain assessed in the MY20 symptom scale and cognitive functioning. The EQ-5D demonstrated the same pattern of results, with the TFI group reporting a utility value 0.053–0.093 higher than the other treatment groups; however, the standard deviations were relatively large. This is likely to be due to within group variability, which will be considered later.
In the regression analyses, the self-rated EQ-5D VAS was significantly higher amongst patients in the first TFI group, indicative of better HRQL, relative to all other treatment phases. Most of the measures of HRQL reduced significantly when patients moved from the first TFI to second-line and later treatment phases (Table 3). The lack of significant differences between first TFI and first line treatment groups may be due to the small sample size in the latter group (n = 12). The reduction in HRQL between first TFI and later treatment phase were of a greater magnitude than those associated with second-line treatment. This may, in part, be due to the smaller sample size in the second-line treatment group; however, it is also likely to reflect the HRQL decline associated with subsequent relapses in MM progression. As the precise treatment phase represented by the later phase group is unknown (patients could be in their third, fourth or higher treatment or TFI phase), it is not possible to extrapolate on this. However, these findings do suggest that longitudinal clinical research of HRQL amongst MM patients would be worthwhile.
Similar conclusions can also be drawn from the analysis of the relationship between HRQL and TFI length. A significant relationship between a longer log TFI and better HRQL was found on two domains of the QLQ-C30 (physical and role functioning) and MY20 (future perspectives and body image) and the EQ-5D utility value. Thus, longer TFI appears to particularly benefit patients in terms of social functioning and outlook. This significant result on log transformed data suggested a non-linear relationship in line with previous assumptions [26], with a steep incline in HRQL in the first year which then begins to plateau around 1.5–2 years. However, as the variance in HRQL explained by TFI length was relatively low, a linear relationship was also explored and found to be significant. Further data collection using a longitudinal design or sampling heavily throughout the TFI will be required to explore whether the exact nature of this relationship is linear or non-linear. We believe that these data would be valuable for cost-effectiveness analysis where much simpler assumptions about HRQL may be made.
Limitations
There are some important limitations in the current study design which should be considered. The study used a cross-sectional design to describe how people with MM may change over time based on the assumption that all of the study participants were representative of people with MM at each phase of the disease. Using these data, we have made some tentative conclusions regarding different influences on patients’ HRQL. A longitudinal design would have had greater rigour for the assessment of these changes over time, and we recommend that such a study be considered as a next step. This would also address the treatment phase sample size issue that was evident in the present study. Participants for this study were recruited from a patient advocacy group and so may not be fully representative of people with MM. The cross-sectional design also meant that there was likely to be a survivor bias and bias in favour of only including people who were well enough to complete the survey. In addition, it became necessary to exclude some cases from the analysis because it was not possible to determine with any certainty their current treatment phase. It should also be noted that patients' medical records were not reviewed to confirm diagnosis and treatment history. A pilot study was conducted to minimise error associated with patients' self-report of treatment phase.
Conclusion
These results on patients with MM provide, for the first time, evidence that a first TFI is associated with better HRQL when compared to other treatment phases. The data also indicate that the length of the first TFI is associated with better patient-reported HRQL. These findings lend support to and may justify treatment approaches that employ more aggressive front-line protocols so as to achieve longer first remissions. A longitudinal clinical study would provide valuable information to assist the evaluation of future MM therapies, including cost-effectiveness analyses.
References
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, de Haes JCJM, Kaasa S, Klee MC, Osoba D, Razavi D, Rofe PB, Schraub S, Sneeuw KCA, Sullivan M, Takeda F (1993) The European Organisation for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85:365–376
Adam Z, Pour L, Svobodník A, Scudla V, Salajka F, Vytrasová M, Bacovský J, Schützová M, Koza V, Sumná E, Franková H, Lehanka F, Gumulec J, Stavarová Y, Cahová S, Vránová M, Dostálová V, Kessler P, Walterová L, Meluzínová I, Seifertová N, Sláma O, Büchler T, Krejcí M, Bencíková V, Nykodýmová V, Dusek L, Hájek R, Czech Myeloma Group (2002) Quality of life and tolerance of maintenance treatment in patients with multiple myeloma. [Czech]. Vnitr Lek 48:216–229
Bird JM, Owen RG, D'Sa S, Snowden JA, Pratt G, Ashcroft J, Yong K, Cook G, Feyler S, Davies F, Morgan G, Cavenagh J, Low E, Behrens J, Haemato-oncology Task Force of the British Committee for Standards in Haematology (BCSH) and UK Myeloma Forum (2011) Guidelines for the diagnosis and management of multiple myeloma 2011. Br J Haematol 154:32–75
Bladé J, Cibeira MT, Fernández de Larrea C, Rosiñol L (2010) Multiple myeloma. Ann Oncol: Official Journal of the European Society for Medical Oncology/ESMO 21(Suppl 7):vii313–vii319
Cancer Research UK (2007) http://www.cancerresearchuk.org/. Accessed 20 Dec 2010
Cocks K, Cohen D, Wisløff F, Sezer O, Lee S, Hippe E, Gimsing P, Turesson I, Hajek R, Smith A, Graham L, Phillips A, Stead M, Velikova G, Brown J, EORTC Quality of Life Group (2007) An international field study of the reliability and validity of a disease-specific questionnaire module (the QLQ-MY20) in assessing the quality of life of patients with multiple myeloma. Eur J Cancer 43:1670–1678
Dimopoulos M, Spencer A, Attal M, Prince HM, Harousseau JL, Dmoszynska A, San Miguel J, Hellman A, Facon T, Foà R, Corso A, Masliak Z, Olesnyckj M, Yu Z, Patin J, Zeldis JB, Knight RD, Multiple Myeloma (010) Study Investigators (2007) Lenalidomide plus dexamethasone for relapsed or refractory multiple myeloma. N Engl J Med 357:2123–2132
Dolan P (1997) Modelling valuations for EuroQol Health States. Med Care 35:1095–1108
Dubois D, Dhawan R, van de Velde H, Esseltine D, Gupta S, Viala M, de la Loge C (2006) Descriptive and prognostic value of patient-reported outcomes: the bortezomib experience in relapsed and refractory multiple myeloma. J Clin Oncol 24:976–982
EuroQol Group (1990) EuroQol—a new facility for the measurement of health-related quality of life. Health Policy 16:199–208
Facon T, Mary JY, Hulin C, Benboubker L, Attal M, Pegourie B, Renaud M, Harousseau JL, Guillerm G, Chaleteix C, Dib M, Voillat L, Maisonneuve H, Troncy J, Dorvaux V, Monconduit M, Martin C, Casassus P, Jaubert J, Jardel H, Doyen C, Kolb B, Anglaret B, Grosbois B, Yakoub-Agha I, Mathiot C, Avet-Loiseau H (2007) Melphalan and prednisone plus thalidomide versus melphalan and prednisone alone or reduced-intensity autologous stem cell transplantation in elderly patients with multiple myeloma (IFM 99–06): a randomised trial. Lancet 370:1209–1218
Fayers P, Aaronson NK, Bjordal K, Curran D, Groenvold M, EORTC Quality of Life Study Group (2001) EORTC QLQ-C30 scoring manual, 3rd edn. EORTC Quality of Life Group, Brussels
Gulbrandsen N, Wisløff F, Brinch L, Carlson K, Dahl IM, Gimsing P, Hippe E, Hjorth M, Knudsen LM, Lamvik J, Lenhoff S, Lofvenberg E, Nesthus I, Nielsen JL, Turesson I, Westin J, Nordic Myeloma Study Group (2001) Health-related quality of life in multiple myeloma patients receiving high-dose chemotherapy with autologous blood stem-cell support. Med Oncol 18:65–77
Hulin C, Facon T, Rodon P, Pegourie B, Benboubker L, Doyen C, Dib M, Guillerm G, Salles B, Eschard JP, Lenain P, Casassus P, Azais I, Decaux O, Garderet L, Mathiot C, Fontan J, Lafon I, Virion JM, Moreau P (2009) Efficacy of melphalan and prednisone plus thalidomide in patients older than 75 years with newly diagnosed multiple myeloma: IFM 01/01 trial. J Clin Oncol 27:3664–3670
Kind P (1996) The EuroQoL instrument: An index of health-related quality of life. In: Spilker (ed) Quality of life and pharmacoeconomics in clinical trials, 2nd edn. Lippincott-Raven, Philadelphia
Kumar SK, Rajkumar SV, Dispenzieri A, Lacy MQ, Hayman SR, Buadi FK, Zeldenrust SR, Dingli D, Russell SJ, Lust JA, Greipp PR, Kyle RA, Gertz MA (2008) Improved survival in multiple myeloma and the impact of novel therapies. Blood 111:2516–2520
Kvam AK, Fayers P, Hjermstad M, Gulbrandsen N, Wisloff F (2009) Health-related quality of life assessment in randomised controlled trials in multiple myeloma: a critical review of methodology and impact on treatment recommendations. Eur J Haematol 83:279–289
Lee SJ, Richardson PG, Sonneveld P, Schuster MW, Irwin D, San Miguel JF, Crawford B, Massaro J, Dhawan R, Gupta S, Anderson KC (2008) Bortezomib is associated with better health-related quality of life than high-dose dexamethasone in patients with relapsed multiple myeloma: results from the APEX study. Br J Haematol 143:511–519
Palumbo A, Bringhen S, Caravita T, Merla E, Capparella V, Callea V, Cangialosi C, Grasso M, Rossini F, Galli M, Catalano L, Zamagni E, Petrucci MT, De Stefano V, Ceccarelli M, Ambrosini MT, Avonto I, Falco P, Ciccone G, Liberati AM, Musto P, Boccadoro M, Italian Multiple Myeloma Network GIMEMA (2006) Oral melphalan and prednisone chemotherapy plus thalidomide compared with melphalan and prednisone alone in elderly patients with multiple myeloma: randomized controlled trial. Lancet 367:825–831
Palumbo A, Sezer O, Kyle R, Miguel JS, Orlowski RZ, Moreau P, Niesvizky R, Morgan G, Comenzo R, Sonneveld P, Kumar S, Hajek R, Giralt S, Bringhen S, Anderson KS, Richardson PG, Cavo M, Davies F, Bladé J, Einsele H, Dimopoulos MA, Spencer A, Dispenzieri A, Reiman T, Shimizu K, Lee JH, Attal M, Boccadoro M, Mateos M, Chen W, Ludwig H, Joshua D, Chim J, Hungria V, Turesson I, Durie BG, Lonial S, IMWG (2009) International Myeloma Working Group guidelines for the management of multiple myeloma patients ineligible for standard high-dose chemotherapy with autologous stem cell transplantation. Leukemia 23:1716–1730
Richardson PG, Sonneveld P, Schuster MW, Irwin D, Stadtmauer EA, Facon T, Harousseau JL, Ben-Yehuda D, Lonial S, Goldschmidt H, Reece D, San-Miguel JF, Bladé J, Boccadoro M, Cavenagh J, Dalton WS, Boral AL, Esseltine DL, Porter JB, Schenkein D, Anderson KC, Assessment of Proteasome Inhibition for Extending Remissions (APEX) Investigators (2005) Bortezomib or high-dose dexamethasone for relapsed multiple myeloma. N Engl J Med 352:2487–2498
Shah N, Lonial S (2010) Evidence-based mini-review: treatment options for patients with relapsed/refractory myeloma previously treated with novel agents and high-dose chemotherapy and autologous stem-cell transplantation. Hematology/the Education Program of the American Society of Hematology. American Society of Hematology. Education Program 2010: 310–313
Singer CR (1997) ABC of clinical haematology. Multiple myeloma and related conditions. BMJ 314:960–963
Sirohi B, Powles R (2004) Multiple myeloma. Lancet 363:875–887
Stead ML, Brown JM, Velikova G, Kaasa S, Wisløff F, Child JA, Hippe E, Hjorth M, Sezer O, Selby P (1999) Development of an EORTC questionnaire module to be used in health-related quality-of-life assessment for patients with multiple myeloma. European organization for research and treatment of cancer study group on quality of life. Br J Haematol 104:605–611
van Agthoven M, Segeren CM, Buijt I, Uyl-De Groot CA, van der Holt B, Lokhorst HM, Sonneveld P (2004) A cost-utility analysis comparing intensive chemotherapy alone to intensive chemotherapy followed by myeloablative chemotherapy with autologous stem-cell rescue in newly diagnosed patients with stage II/III multiple myeloma; a prospective randomised phase III study. Eur J Cancer 40:1159–1169
Waage A, Gimsing P, Fayers P, Abildgaard N, Ahlberg L, Björkstrand B, Carlson K, Dahl IM, Forsberg K, Gulbrandsen N, Haukås E, Hjertner O, Hjorth M, Karlsson T, Knudsen LM, Nielsen JL, Linder O, Mellqvist UH, Nesthus I, Rolke J, Strandberg M, Sørbø JH, Wisløff F, Juliusson G, Turesson I, Nordic Myeloma Study Group (2010) Melphalan and prednisone plus thalidomide or placebo in elderly patients with multiple myeloma. Blood 116:1405–1412. doi:10.1182/blood-2009-08-237974
Wijermans P, Schaafsma M, Termorshuizen F, Ammerlaan R, Wittebol S, Sinnige H, Zweegman S, van Marwijk Kooy M, van der Griend R, Lokhorst H, Sonneveld P, Dutch-Belgium Cooperative Group HOVON (2010) Phase III study of the value of thalidomide added to melphalan plus prednisolone in elderly patients with newly diagnosed multiple myeloma: the HOVON 49 study. J Clin Oncol 28:3160–3166. doi:10.1200/JCO.2009.26.1610
Acknowledgments
The authors would like to thank Myeloma UK for their assistance in this study and all patients that participated.
Conflict of interest
This study and manuscript were sponsored by Janssen-Cilag Ltd., where the author Sabine Gaugris is an employee. All primary data is available for review if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Acaster, S., Gaugris, S., Velikova, G. et al. Impact of the treatment-free interval on health-related quality of life in patients with multiple myeloma: a UK cross-sectional survey. Support Care Cancer 21, 599–607 (2013). https://doi.org/10.1007/s00520-012-1548-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-012-1548-y