Abstract
Introduction
Cancer disease inducing an acquired hypercoagulable state is a well-established feature. Venous thromboembolism (VTE) occurs in 4% to 20% of the patients and is the second cause of mortality in cancer; VTE incidence is four to six times higher in cancer patients compared to other patients. In the last 10 years, important randomised clinical trials have clearly demonstrated that long-term use of daily subcutaneous low molecular weight heparin (LMWH) is more efficient than Vitamin K antagonists to treat VTE in cancer patients. First Italian, then American and more recently French national guidelines recommend the use of LMWH for 3 to 6 months for curative treatment of VTE in cancer patients with a clearly high level (A) of evidence. Despite convincing data, many physicians have not yet modified their clinical practice, doubting the tolerability of such a long period of subcutaneous injections. In fact, LMWH long-term use appears well tolerated and may also increase cancer patient survival.
Objectives
The aim of this review is to present the scientific rationale for long-term daily subcutaneous LMWH in cancer patients, and to reinforce the favourable benefit/tolerance tolerability ratio with this specific antithrombotic strategy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Venous thromboembolism (VTE), as defined by the presence of deep venous thrombosis (DVT) and/or pulmonary embolism (PE), occurs in 4% to 20% of cancer patients [49]. It is the second cause of mortality in these patients with approximately one death out of seven hospitalised cancer patients related to VTE [15]. The overall incidence of VTE is four to six times higher in cancer patients compared to the rest of the population [25]. The presence of cancer is an independent risk factor of VTE [5, 25, 43] and the onset of VTE during the course of active cancer also appears to be an independent prognostic factor for survival [43, 66]. Considering patients with the same type and degree of cancer extension, those with VTE have reduced overall survival rates [66]. Under chronic anticoagulant therapy, patients with active cancer are at a higher risk of bleeding complications and thromboembolic recurrences, which are both responsible for altered quality of life and increased health care expenses. In addition, cancer per se is an independent risk factor for bleeding during heparin and vitamin K antagonists (VKA) [30, 58] and the majority of treatment failures with VTE recurrences occur during VKA therapy.
The care of established venous thromboembolism in cancer patients has been dramatically changed over the last 10 years, given the results of comparisons between classical anticoagulation protocols using low molecular weight heparin (LMWH) and early VKA therapy [8] compared to the long-term use of LMWH for 3 to 6 months. Indeed, three important randomised clinical trials (CANTHANOX [50], CLOT [39] and LITE [28]) have clearly demonstrated that long-term use of LWMH is more efficient than VKA to treat VTE in cancer patients. These results led to the establishment of national guidelines in Italy [45], the US [44] and, more recently, France (www.sor-cancer.fr). These guidelines recommend the use of LMWH during 3 to 6 months for VTE treatment in cancer patients with a high level of evidence (grade A, level I). Despite these convincing data provided by the studies mentioned above, many practitioners have not yet modified their clinical practice and/or still have to doubt on the tolerability of daily subcutaneous LMWH for 6 months; however, few people would question the tolerability of subcutaneous insulin injections for treating diabetes in a cancer patient. Long-term use of LMWH appears to be well tolerated [53] in cancer patients and may prolong survival [40]. The aim of this review is to present the scientific rationale for long-term daily subcutaneous LMWH in cancer patients and to address the tolerability and consequences of this specific therapeutic approach.
Epidemiology
In the general population, cancer is associated with 16% to 20% of all VTEs [16, 41, 63]. In a large population-based North American case-control study comparing two groups of 625 patients with and without VTE, the risk of developing VTE related to cancer was estimated at 19.6% [24] and the risk of VTE was enhanced four to 6.5-fold in cancer cases [25]. In this series, several factors such as surgery (odds ratio [OR] = 21.7), hospitalisation (OR = 7.98), a central catheter (OR = 5.6) or chemotherapy (OR = 6.53) were also associated with an increased risk of DVT or PE [25]. The frequent coexistence of these independent risk factors in cancer patients contributes to the high rate of VTE. Similar figures were reported in Europe with the MEGA study, another large population-based case-control of VTE risk factors including 3,220 consecutive patients with a first thromboembolic episode and 2,131 controls [9], where the overall risk of VTE was increased sevenfold in patients with malignancy (OR, 6.7; 95%[CI], 5.2–8.6). In France, analysis of 458 VTE cases from the EPI-GETBO register in 2005 shows that 15% of the VTE were related to a cancer [54].
In cancer patients, the main risk factor for VTE occurs with surgery. In the @RISTOS study, 2.1% of the VTE events—including 0.8% of lethal PE—were noted among 2,773 patients despite adapted VTE prophylaxis in 81% of hospitalised patients and in 31% of ambulatory patients [1]. VTE risk varies depending on the type of surgery. Among 1,375 patients operated on for a gynaecological tumour, the frequency of postoperative VTE was about 4% in the case of major cancer surgery, 0.4% in case of minor cancer surgery and only 0.3% in non-cancer surgery [48]. The rate of VTE among 3,898 women with breast cancer surgery was 0.16% [7].
In hospitalised cancer patients, VTE prevalence was estimated at 2% among the 40,787,000 patients recruited in the National Hospital Discharge Survey from 1979 to 1999 [67] and at 4.5% in the University Health System Consortium data base collected between 1995 and 2003 [32]. These figures illustrate that the observed rate of VTE in cancer patients rose by approximately 30% between 1995 and 2003 [32].
During chemotherapy, the rate of VTE is quite heterogeneous according to the studied populations and the drugs used to treat the underlying cancer. It varied from 2.2% in a prospective study including more than 4,000 patients [33] to 7.3% (15/206) among patients presenting various types of cancer [56] and 8.4% (15/179) in patients with germinal tumors [72]. More recently, Khorana et al [33], using a North American prospective observational cohort of 2,701 cancer outpatients, developed a simple model for predicting chemotherapy-associated VTE risk using five baseline clinical and laboratory variables: site of cancer (two points for very high risk site, one point for high-risk site), platelet count > 350,000/mm3, haemoglobin < 10 g/dl and or use of erythropoietin, leucocyte count > 11,000/mm3, and body mass index (BMI) > 35 (one point each). Patients at low risk (score = 0) had a VTE rate of 0.3% to 0.8%, at intermediate risk (score = 1 or 2) had a VTE rate of 1.8 to 2.2% and those at high risk (score > 2) had a VTE rate of 6.7% over a median of 2.5 months [33]. Validity of this scoring system in the European population, with lower BMI values, will have to be evaluated.
Venous thromboembolism: an independent prognostic factor of decreased overall survival in cancer patients
The presence of VTE has emerged as an independent risk factor of reduced survival in cancer patients. Using multivariate analysis of various prognostic factors associated with decreased survival in cancer patients, several studies have found that cancer patients without VTE live longer than those with VTE. Three different register studies have shown significant differences in survival rates in cancer patients with or without VTE. In the Medicare Claims registry data with a large number of 211,944 cancer patients gathered from 1988 to 1990, the overall survival rate was only 6% in cancer patients with VTE compared to 58% in those without [43]. In the Danish cancer registry, Sorensen et al. reported a 1-year survival of 12% in 668 cancer patients with VTE compared to 36% in 5,371 matched control patients with comparable cancer stage but no thrombosis [66]. More recently, analysis of the 235,149 cancer patients in the Californian registry showed that VTE (hazard ratio [HR] = 1.3 to 14.4) was the second most important predictor of death after metastasis extension (HR = 1.8 to 49) [15].
Decreased survival rate in cancer patients with VTE has been shown in various types of tumours, but its impact varies according to the tumor extension and the timing of VTE occurrence. Among 68,142 patients with colorectal cancer, the risk of death was 1.2-fold higher in patients presenting VTE. This difference was significant only in cases with extensive local and regional disease, with respectively 1.8- and 1.5-fold increased risk of death and was not found among metastatic patients [4]. Among 12,835 ovarian cancer patients, the survival rate at 1-year was 63% in those without VTE, 54% in case of VTE diagnosed more than 4 months prior to ovarian cancer diagnosis and 44% in patients with VTE occurrence within the 4 months preceding cancer diagnosis [69]. In patients operated for non-small-cell lung cancers, the survival rate at 18 months was also higher in cases without thrombosis (44% versus 18%) [47].
Treatment of established VTE in cancer patients
Unfractionated heparin (UH) or low molecular weight heparins (LMWH) with early introduction of vitamin K antagonist (VKA)
Three retrospective studies [12, 13, 17] and the control arm of a randomised multicentre study [28] show that unfractionated heparin (UFH) followed by long-term VKA therapy is associated with an unacceptable rate of recurrence (10% to 30%) and severe bleeding. As observed in the general population, the use of LMWH to start anticoagulation allowed significant progress in treating DVT and PE in cancer patients. In the absence of a specific randomised trial in cancer patients to compare the efficacy of LMWH to UFH in the initial treatment for VTE, one may learn from the results reported by non-specific meta-analyses in the general population, which included 10 to 15% of cancer patients [19, 22, 27, 42, 51, 60, 61, 65]. All these studies favour the use of LMWH compared to UFH in the initial treatment of VTE. In the general population, the incidence of major bleeding events and the rate of VTE recurrence was significantly reduced (five of the eight meta-analyses) under early treatment by LMWH compared with UFH. However, these meta-analyses rarely present any subgroup analysis, therefore limiting any conclusions for the cancer patients. Only, the meta-analysis by Hettiarachi included an analysis of efficacy for the subgroup of cancer patients, showing that LMWH was associated with a decrease in the recurrence rate of VTE [27]. A few other studies were specifically designed in the cancer population, with one retrospective [29] and four prospective studies [10, 57, 58, 70] plus the respective control arms of three randomised multicentre studies [18, 39, 50] using LMWH and early introduction of VKA. All results reported in the “cancer” population were similar with an increased risk of recurrence (2% to 16.9% according to the study) and of major bleeding complications (2.7% to 16%) during VTE treatment by LMWH with an early start of VKA. Therefore, other therapeutic protocols were proposed.
Prolonged use of LMWH for three to 6 months
The results of the long-term use of LMWH after initial treatment by heparin were evaluated by one meta-analysis [21] and four specific randomised trials in cancer patients comparing LMWH during 3 to 6 months with LMWH plus early introduction of VKA in the treatment of established VTE [18, 27, 39, 50].
The CANTHANOX trial evaluated enoxaparin in one daily sc injection of 150 UI/kg for 3 months in 67 patients and compared it to LMWH with early introduction of warfarin in 71 patients [50]. The main outcome in the CANTHANOX trial was a combined criterion, aggregating the recurrence and bleeding complications rates, for which a trend (p = 0.09) but no significant difference was shown (21% in the VKA group compared to 10% in the LMWH group) [50]. Nevertheless, the analysis of time passed to event (recurrence of VTE or major bleeding) revealed a statistically significant difference in favour of the long-term use of enoxaparin (p = 0.04). It is likely that the aggregated outcome would have shown a significant difference in favour of LMWH, but the trial was stopped prematurely because the inclusion period was considered too long.
The CLOT trial evaluated dalteparin administered at 200 UI/Kg once a day during 1 month followed by 150 UI/kg once a day for 5 months versus LMWH with early introduction of warfarin in good performance cancer patients (336 patients in each group) [39]. Confirmed diagnosis of symptomatic VTE recurrence during the 6-month treatment was statistically less frequent in cancer patients treated by LMWH (8%) versus classical anticoagulation (16%) [39]. In a further pharmacoeconomic analysis of the CLOT study, compliance was significantly better in the LMWH arm (98%) than in the VKA arm (89%, p < 0.001) [20].
The ONCENOX trial was an open randomised trial with three arms, comparing two daily doses of 1.5 mg/kg and 1 mg/kg of enoxaparin sc with warfarin for 6 months in 102 patients [18]. In this study, major aims were to test feasibility and treatment compliance. Efficacy was judged on the rate of VTE recurrence and symptomatic extensions, which were identical under VKA and LMWH (3.3%).
In the LITE trial, tinzaparin at its usual therapeutic dose (175 UI/kg sc once a day) was compared to UFH with early introduction of warfarin for 3 months with 100 patients in each arm [28]. The main outcome was symptomatic VTE recurrence as evaluated three and 12 months after starting anticoagulation. After 3 months, recurrence rates were identical (6% for long-term LMWH vs 10% for UHF plus VKA); by 12 months, there was a significant difference with a 7% recurrence rate in long-term LMWH vs 16% in LMWH plus VKA. However, the control arm of the LITE trial may be controversial since the association UFH with early introduction of VKA is not the standard treatment for DTV and was inferior to the association LMWH with early introduction of VKA in the general population and in cancer patients [19, 27, 42, 51, 60, 61, 65].
None of these four randomised trials showed a significant statistical effect on the rate of bleeding complications under long-term use of LMWH as compared to their respective control arms.
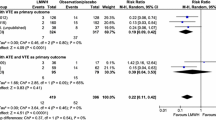
These four trials were included in a meta-analysis published in 2006 by Ferretti et al. on 2,907 patients from 11 randomised trials [21]. Analysis of the subgroup of 1,115 cancer patients showed a statistically significant lower rate of VTE recurrence when using LMWH alone for 3 to 6 months (RR = 0.52; IC 95: 0.359–0.769). Hull et al. published an update of Ferretti’s meta-analysis with all the data from the LITE trial [28] confirming the benefit in favour of long-term use of LMWH on the recurrence rate of VTE (RR = 0.5; IC95: 0.35–0.72). On the other hand, there was no significant difference concerning the rate of bleeding complications (RR = 0.80; IC95: 0.61–1.05).
Therefore, data in the literature reported for cancer patients in prospective randomised trials and the meta-analyses were coherent. In comparison with LMWH plus early VKA, long-term use of LMWH alone over 3 to 6 months in cancer patients with VTE is associated with a statistically significant 50% decrease in recurrence, without increase of major bleeding. These data finally led the authors of the Italian (AIOM) [45], North American (ACPP and ASCO) [11, 44] and French (FNCLCC, www.sor-cancer.fr) guidelines to recommend the use of 3 to 6 months of therapeutic dose sc LMWH for treating established VTE in cancer patients.
The cost of long-term use of LMWH in cancer patients
The cost effectiveness of the long-term use of LMWH in cancer patients has been studied in a Canadian post hoc analysis of the CLOT study performed by Dranitsaris et al [20]. When all the components were combined for the entire population (n = 676), patients in the dalteparin group had a significantly higher cost overrun of $Can 2,159. Drug acquisition contributed for 67% of the cost in the dalteparin group (vs 13% in the control), while VTE treatment and laboratory monitoring were the largest cost components in the oral anticoagulants group. A cost-utility analysis was then performed to estimate the incremental cost per quality-of-life adjusted year (QALY) gained. Indeed a $Can 50,000 cost per QALY has been suggested as a threshold, at or below, which new medical interventions should be considered by health care systems with an ‘acceptable’ economic value [37]. When differences in treatment preferences and health utilities were combined, the additional cost with dalteparin was associated well below the breakeven point mentioned.
The same medico-economic analysis had been previously performed in the non-cancer population using six trials comparing LMWH and long-term VKA [46]. The cost of a year of life with maintained quality of life was estimated at a cot of $6,583 per QALY based on the cost in Italy and $28,231 per QALY based on the costs in the United States. This figure is higher than noted in the cancer population by Dranitsakis [20]. However, LMWH appeared as a cost-effective drug for secondary prophylaxis of VTE, especially in patients at high risk of recurrence and in countries where the drug’s cost is lower.
Enhanced survival of cancer patients treated by long-term use of LMWH?
The experimental effects of LMWH on cancer progression have been previously reviewed [68] with several targets, including inhibition of coagulation, interaction with selectins, inhibition of heparanases and facilitation of apoptosis. The inhibiting effects of LMWH on metastatic tumor cells partly depend on previous activation of the coagulation by the tumor cell bound tissue factor and on the presence of fibrinogen as an important part of tissue stroma. Indeed, LMWH can inhibit the expression of L-selectin and P-selectin on platelets and endothelial cells, which facilitate the binding of glycoproteins in the plasma membrane of cancer cells and to the endothemium and platelets. LMWH do also inhibit the heparanase, which elevated levels in tumors have been shown to correlate with a more advanced cancer stage and a higher likelihood of metastasis. In addition, uptake of LMWH by the cancer cells could lead to enhanced apoptosis via interfering with a transcription factor and caspase activation [68].
Low molecular weight heparin may prolong survival in certain tumor types, apart from their effect on VTE. In a meta-analysis including 3,581 patients treated for VTE with LMWH or UFH followed by VKA relay, the 3-month mortality rate observed in the subgroup of 629 cancer patients was 15% in patients first treated by LMWH compared to 22% with UFH (odds ratio 0.61; confidence interval at 95% 0.40–0.93) [26]. To develop strategies potentially associated with a better life expectancy, recent studies have addressed the role of LMWH in cancer patient survival.
The FAMOUS and MALT studies aimed to assess the potential benefit of the prophylactic use of LMWH on survival with cancer but without VTE [31, 34]. One hundred ninety patients with various types of solid tumor at different stages were randomised in a group receiving dalteparin 5,000 UI daily sc for 1 year and 184 in the placebo group [31]. For all patients, survival at 1, 2 and 3 years did not differ (46%, 27% and 21% in the dalteparin group vs 41%, 18% and 12% in the placebo group). In patients with good prognosis (survival > 17 months), survival was improved at 2 and 3 years in the dalteparin group (78% vs 55% and 63% vs 36%). The MALT study [34] compared 148 patients treated with nadroparin (9,500 anti XA U/ml) versus 154 patients receiving placebo for 6 weeks. The median survival was higher with nadroparin (8 vs 6.6 months, p = 0.02) and the difference was more pronounced (p < 0.01) in patients with a life expectancy of more than 6 months at inclusion (15.4 vs 9.4 months).
In patients with localised cancer treated for VTE, an increased survival rate was also found with the long-term use of LMWH using an a posteriori analysis of the CLOT trial [40]: life expectancy was higher at 1 year in the long-term LMWH arm (80%) compared to LMWH with early introduction of VKA (64%). In an open randomised trial, dalteparin at 5,000 UI daily for 18 weeks together with chemotherapy in small-cell lung cancer patients without VTE was associated with a significant improvement in the mean survival (13 months with dalteparin vs 8 months in the control group (n = 42 in each group) [6]. In another controlled study performed on 138 cancer patients of various types to compare dalteparin, 5,000 UI sc daily vs placebo, no difference in mean survival was demonstrated (7.3 with dalteparin and 6.2 months with placebo, 70 patients in each group) [64]. The trial was stopped early for slow recruitment, which might explain the absence of significant difference in survival.
A systematic review with meta-analysis of these four randomised trials specifically evaluating the impact of LMWH on the survival of cancer patients without VTE has been performed [38]. In this review, LMWH appeared to improve the overall survival in cancer patients, (HR = 0.83, 95% CI 0.70–0.99; P = 0.03), even in those with advanced disease (HR = 0.86, 95% CI 0.74–0.99; P = 0.04). However, sensitivity analyses, according to tumor type, were not conducted, because of a lack of information.
Another meta-analysis included 11 studies with cancer patients without VTE treated with anticoagulant [35]. The relative risk for mortality was 0.877 (95% CI, 0.789–0.975; P = .015) for LMWH, compared with a relative risk of 0.942 (95% CI, 0.854–1.040; P = .239) for warfarin, resulting in an absolute risk difference (ARD) of 8% for LMWH. This meta-analysis suggested that improved survival with anticoagulation may depend on tumor type. A third meta-analysis included five randomised controlled trials (RCTs) comparing UFH or LMWH to no intervention or placebo in cancer patients without clinical evidence of VTE [2]. Overall, heparin therapy was associated with a statistically and clinically significant survival benefit (HR = 0.77; 95% CI 0.65 to 0.91). In the subgroup analysis, patients with limited small cell lung cancer clearly experienced a survival benefit (HR = 0.56; 95% CI 0.38 to 0.83). The survival benefit was not statistically significant for either patients with extensive small cell lung cancer (HR = 0.80; 95% CI 0.60 to 1.06) or patients with advanced cancer (HR = 0.84; 95%: 0.68 to 1.03). Many ongoing clinical studies at the European and North American levels will help to better elucidate the respective type of cancer patients who may benefit from LMWH and at which dosages, according to their specific VTE risks factors and cancer type and staging.
Tolerance of long-term use of LMWH in cancer patients (Table 1)
The major feared adverse effect keeping clinicians from prescribing daily subcutaneous injections of LMWH long term is the presumed intolerance and low acceptance by cancer patients. Indeed, many oncologists still do not prescribe LMWH for 3 or 6 months, fearing to impose additional constraint on their patients and, in consequence, to decrease their patients' quality of life.
Bleeding complications common to any type of anticoagulant treatment are identical in cancer patients with LMWH or VKA [28, 39, 50]. Theoretically, potential complications related to LMWH include heparin-induced thrombocytopenia, allergic reactions, pain and bruising linked to the subcutaneous injection and the risk of fractures due to induced osteoporosis.
In cancer patients, the various prospective studies did not report any cases of heparin-induced thrombocytopenia (HIT). The incidence of thrombopenia was identical with the long-term use of LMWH and VKA as assessed in the LITE [28], the CANTHANOX [50] and in the Sideras [64] studies. A retrospective study of patients treated with UFH found 55 episodes of HIT, including 11 in the cancer patients, but did not allow for an estimation of the prevalence of HIT in cancer patients [55]. From two prospectively evaluated groups of 598 patients treated with UFH and 1,754 patients under LMWH, extrapolation of the data estimated a HIT frequency of 1.5% (5/335) in the subgroup of cancer patients [59]. In the absence of specific studies and with a total of 16 HIT episodes reported (including five patients on LMWH), it was impossible to draw a firm conclusion on the real frequency of HIT in cancer patients. Nevertheless, it seems well established that thrombopenia is predominantly related to simultaneous use of chemotherapy and to bone marrow infiltration than heparin per se. In addition, thrombopenia related to heparin is less frequent with LMWH than with UFH [71]. Lastly, during prolonged use of LMWH, HIT is generally observed within the first month of treatment and infrequent thereafter.
Similarly, the risk of bone fractures was not increased with LMWH (no case in either arms in the CANTHANOX study [50], 5% with VKA and 3% with long-term LMWH in the LITE study [28] and appeared preferentially related to cancer than to LMWH. Allergic reactions were only documented in the MALT study and did not differ between the prophylactic use of LMWH and placebo [34].
Pain and skin hematoma at the injection sites are common adverse side effects in daily practise, which may occur in 30 to 90% of subjects with sc administration [23]. However, these side effects have not been evaluated in randomised trials. They were only mentioned by Sideras, who reported a significant difference between the placebo (19%) and the LMWH group (50%) [64]. These side effects can be the source of discomfort for patients with prolonged treatment and could limit the number of available injection sites. Nonetheless, they can be reduced by a change in subcutaneous injection techniques of LMWH. In a series of subjects with chronic obstructive pulmonary disease, a prolonged 30-s injection or a 10-s wait before pulling the needle compared to an injection performed within 10 s allowed to observe less frequent (61% or 64% vs 89%) and less pronounced indurations (55 mm and 35 mm vs 110 mm) [3]. In two studies performed among 34 patients with stroke [14] and 50 hospitalised medical patients [73], an injection of LMWH performed over 30 s compared to 10 s reduced the pain (10 and 14 vs 23 and 21 on the Visual Analogic Scale) and the incidence of bruising (30% and 42% vs 53% and 54%).
A lot of data on the influence of the needle size exists too, but results are non-conclusive. Ice application after injecting the LMWH does not reduce the frequency and the size of skin induration [36, 62], although if it may have an analgesic effect.
Overall, the long-term use of LMWH to treat VTE is well accepted in cancer patients and their use does not appear more detrimental than daily subcutaneous injections for other life-long therapies, such as diabetes treatment. Two studies in palliative care performed by Noble reported the results of semi-directive 30-min interviews with cancer patients treated with long-term LMWH [52, 53]. In the first study, 37 out of 40 indications for the use of LMWH were secondary to the impossibility to adequately maintain oral anticoagulation with VKA, i.e. the impossibility to achieve therapeutic ranges of INR, VTE recurrence under VKA or the impossibility to achieve oral absorption of VKA [52]. LMWH were well accepted and were even acknowledged to have a positive impact on the quality of life of patients. Constraints under LMWH were considered insignificant as compared with those occurring under chemotherapy or radiotherapy. Most patients, who were once treated by VKA, preferred LMWH, which allowed far less biological surveillance and therapeutic adaptation [52]. LMWH were also preferred to compression stockings, which patients found too difficult to wear [53]. This finding was not limited to palliative care patients and analysis of the CLOT study also showed improved quality of life in patients treated by LMWH (score of 0.66 for LMWH and 3.4 for VKA) [20].
Conclusion
Analysis of data available in the literature shows that low weight molecular heparins are the gold standard therapy for VTE in cancer patients. They are more efficient than VKA in preventing recurrence without increased bleeding risk in comparison. The higher costs of LMWH appear acceptable in consideration of the gain in quality of life. Among classical complications that may occur with LMWH, allergies, fractures and HIT were not more frequent compared to VKA and were linked to the cancer and other treatments. Skin indurations at injection sites can be minimised by changing the injection techniques. Long-term LMWH was equally or even better tolerated than VKA even in palliative care situations. The potential longer term benefit with increased survival in cancer patients treated by LMWH will have to be confirmed by ongoing prospective trials.
References
Agnelli G, Bolis G, Capussotti L, Scarpa RM, Tonelli F, Bonizzoni E et al (2006) A clinical outcome-based prospective study on venous thromboembolism after cancer surgery: the @RISTOS project. Ann Surg 243(1):89–95 doi:10.1097/01.sla.0000193959.44677.48
Akl EA, van Doormaal FF, Barba M, Kamath G, Kim SY, Kuipers S et al (2007) Parenteral anticoagulation for prolonging survival in patients with cancer who have no other indication for anticoagulation. Cochrane Database Syst Rev 3:CD006652
Balci Akpinar R, Celebioglu A (2008) Effect of injection duration on bruising associated with subcutaneous heparin: a quasi-experimental within-subject design. Int J Nurs Stud 45(6):812–817, Jun
Alcalay A, Wun T, Khatri V, Chew HK, Harvey D, Zhou H et al (2006) Venous thromboembolism in patients with colorectal cancer: incidence and effect on survival. J Clin Oncol 24(7):1112–1118 doi:10.1200/JCO.2005.04.2150
Alikhan R, Cohen AT, Combe S, Samama MM, Desjardins L, Eldor A et al (2004) Risk factors for venous thromboembolism in hospitalized patients with acute medical illness: analysis of the MEDENOX Study. Arch Intern Med 164(9):963–968 doi:10.1001/archinte.164.9.963
Altinbas M, Coskun HS, Er O, Ozkan M, Eser B, Unal A et al (2004) A randomized clinical trial of combination chemotherapy with and without low-molecular-weight heparin in small cell lung cancer. J Thromb Haemost 2(8):1266–1271 doi:10.1111/j.1538-7836.2004.00871.x
Andtbacka RH, Babiera G, Singletary SE, Hunt KK, Meric-Bernstam F, Feig BW et al (2006) Incidence and prevention of venous thromboembolism in patients undergoing breast cancer surgery and treated according to clinical pathways. Ann Surg 243(1):96–101 doi:10.1097/01.sla.0000193832.40178.0a
Baron JA, Gridley G, Weiderpass E, Nyren O, Linet M (1998) Venous thromboembolism and cancer. Lancet 351(9109):1077–1080 doi:10.1016/S0140-6736(97)10018-6
Blom JW, Doggen CJ, Osanto S, Rosendaal FR (2005) Malignancies, prothrombotic mutations, and the risk of venous thrombosis. JAMA 293(6):715–722 doi:10.1001/jama.293.6.715
Bona RD, Hickey AD, Wallace DM (2000) Warfarin is safe as secondary prophylaxis in patients with cancer and a previous episode of venous thrombosis. Am J Clin Oncol 23(1):71–73 doi:10.1097/00000421-200002000-00020
Buller HR, Agnelli G, Hull RD, Hyers TM, Prins MH, Raskob GE (2004) Antithrombotic therapy for venous thromboembolic disease: the Seventh ACCP Conference on antithrombotic and thrombolytic therapy. Chest 126(Suppl 3):401S–428S doi:10.1378/chest.126.3_suppl.401S
Calligaro KD, Bergen WS, Haut MJ, Savarese RP, DeLaurentis DA (1991) Thromboembolic complications in patients with advanced cancer: anticoagulation versus Greenfield filter placement. Ann Vasc Surg 5(2):186–189 doi:10.1007/BF02016754
Chan A, Woodruff RK (1992) Complications and failure of anticoagulation therapy in the treatment of venous thromboembolism in patients with disseminated malignancy. Aust N Z J Med 22(2):119–122
Chan H (2001) Effects of injection duration on site-pain intensity and bruising associated with subcutaneous heparin. J Adv Nurs 35(6):882–892 doi:10.1046/j.1365-2648.2001.01925.x
Chew HK, Wun T, Harvey D, Zhou H, White RH (2006) Incidence of venous thromboembolism and its effect on survival among patients with common cancers. Arch Intern Med 166(4):458–464 doi:10.1001/.458
Cohen AT, Davidson BL, Gallus AS, Lassen MR, Prins MH, Tomkowski W et al (2006) Efficacy and safety of fondaparinux for the prevention of venous thromboembolism in older acute medical patients: randomised placebo controlled trial. BMJ 332(7537):325–329 doi:10.1136/bmj.38733.466748.7C
Debourdeau P, Meyer G, Sayeg H, Marjanovic Z, Bastit L, Cabane J et al (1996) Classical anticoagulant treatment of venous thromboembolic disease in cancer patients. Apropos of a retrospective study of 71 patients. Rev Med Intern 17(3):207–212 doi:10.1016/0248-8663(96)81247-1
Deitcher SR, Kessler CM, Merli G, Rigas JR, Lyons RM, Fareed J (2006) Secondary prevention of venous thromboembolic events in patients with active cancer: enoxaparin alone versus initial enoxaparin followed by warfarin for a 180-day period. Clin Appl Thromb Hemost 12(4):389–396 doi:10.1177/1076029606293692
Dolovich LR, Ginsberg JS, Douketis JD, Holbrook AM, Cheah G (2000) A meta-analysis comparing low-molecular-weight heparins with unfractionated heparin in the treatment of venous thromboembolism: examining some unanswered questions regarding location of treatment, product type, and dosing frequency. Arch Intern Med 160(2):181–188 doi:10.1001/archinte.160.2.181
Dranitsaris G, Vincent M, Crowther M (2006) Dalteparin versus warfarin for the prevention of recurrent venous thromboembolic events in cancer patients: a pharmacoeconomic analysis. Pharmacoeconomics 24(6):593–607 doi:10.2165/00019053-200624060-00006
Ferretti G, Bria E, Giannarelli D, Carlini P, Felici A, Mandala M et al (2006) Is recurrent venous thromboembolism after therapy reduced by low-molecular-weight heparin compared with oral anticoagulants? Chest 130(6):1808–1816 doi:10.1378/chest.130.6.1808
Gould MK, Dembitzer AD, Doyle RL, Hastie TJ, Garber AM (1999) Low-molecular-weight heparins compared with unfractionated heparin for treatment of acute deep venous thrombosis. A meta-analysis of randomized, controlled trials. Ann Intern Med 130(10):800–809
Hadley SA, Chang M, Rogers K (1996) Effect of syringe size on bruising following subcutaneous heparin injection. Am J Crit Care 5(4):271–276
Heit JA (2005) Cancer and venous thromboembolism: scope of the problem. Cancer Control 12(Suppl 1):5–10
Heit JA, Silverstein MD, Mohr DN, Petterson TM, O’Fallon WM, Melton LJ 3rd (2000) Risk factors for deep vein thrombosis and pulmonary embolism: a population-based case-control study. Arch Intern Med 160(6):809–815 doi:10.1001/archinte.160.6.809
Hettiarachchi RJ, Smorenburg SM, Ginsberg J, Levine M, Prins MH, Buller HR (1999) Do heparins do more than just treat thrombosis? The influence of heparins on cancer spread. Thromb Haemost 82(2):947–952
Hettiarachchi RJ, Prins MH, Lensing AW, Buller HR (1998) Low molecular weight heparin versus unfractionated heparin in the initial treatment of venous thromboembolism. Curr Opin Pulm Med 4(4):220–225 doi:10.1097/00063198-199807000-00007
Hull RD, Pineo GF, Brant RF, Mah AF, Burke N, Dear R et al (2006) Long-term low-molecular-weight heparin versus usual care in proximal-vein thrombosis patients with cancer. Am J Med 119(12):1062–1072 doi:10.1016/j.amjmed.2006.02.022
Hutten BA, Prins MH, Gent M, Ginsberg J, Tijssen JG, Buller HR (2000) Incidence of recurrent thromboembolic and bleeding complications among patients with venous thromboembolism in relation to both malignancy and achieved international normalized ratio: a retrospective analysis. J Clin Oncol 18(17):3078–3083
Ihnat DM, Mills JL, Hughes JD, Gentile AT, Berman SS, Westerband A (1998) Treatment of patients with venous thromboembolism and malignant disease: should vena cava filter placement be routine? J Vasc Surg 28(5):800–807 doi:10.1016/S0741-5214(98)70054-0
Kakkar AK, Levine MN, Kadziola Z, Lemoine NR, Low V, Patel HK et al (2004) Low molecular weight heparin, therapy with dalteparin, and survival in advanced cancer: the fragmin advanced malignancy outcome study (FAMOUS). J Clin Oncol 22(10):1944–1948 doi:10.1200/JCO.2004.10.002
Khorana AA, Francis CW, Culakova E, Kuderer NM, Lyman GH (2007) Frequency, risk factors, and trends for venous thromboembolism among hospitalized cancer patients. Cancer 110(10):2339–2346 doi:10.1002/cncr.23062
Khorana AA, Kuderer NM, Culakova E, Lyman GH, Francis CW (2008) Development and validation of a predictive model for chemotherapy-associated thrombosis. Blood 111:4902–4907
Klerk CP, Smorenburg SM, Otten HM, Lensing AW, Prins MH, Piovella F et al (2005) The effect of low molecular weight heparin on survival in patients with advanced malignancy. J Clin Oncol 23(10):2130–2135 doi:10.1200/JCO.2005.03.134
Kuderer NM, Khorana AA, Lyman GH, Francis CW (2007) A meta-analysis and systematic review of the efficacy and safety of anticoagulants as cancer treatment: impact on survival and bleeding complications. Cancer 110(5):1149–1161 doi:10.1002/cncr.22892
Kuzu N, Ucar H (2001) The effect of cold on the occurrence of bruising, haematoma and pain at the injection site in subcutaneous low molecular weight heparin. Int J Nurs Stud 38(1):51–59 doi:10.1016/S0020-7489(00)00061-4
Laupacis A, Feeny D, Detsky AS, Tugwell PX (1992) How attractive does a new technology have to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. CMAJ 146(4):473–481
Lazo-Langner A, Goss GD, Spaans JN, Rodger MA (2007) The effect of low-molecular-weight heparin on cancer survival. A systematic review and meta-analysis of randomized trials. J Thromb Haemost 4:729–737 doi:10.1111/j.1538-7836.2007.02427.x
Lee AY, Levine MN, Baker RI, Bowden C, Kakkar AK, Prins M et al (2003) Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med 349(2):146–153 doi:10.1056/NEJMoa025313
Lee AY, Rickles FR, Julian JA, Gent M, Baker RI, Bowden C et al (2005) Randomized comparison of low molecular weight heparin and coumarin derivatives on the survival of patients with cancer and venous thromboembolism. J Clin Oncol 23(10):2123–2129 doi:10.1200/JCO.2005.03.133
Leizorovicz A, Cohen AT, Turpie AG, Olsson CG, Vaitkus PT, Goldhaber SZ (2004) Randomized, placebo-controlled trial of dalteparin for the prevention of venous thromboembolism in acutely ill medical patients. Circulation 110(7):874–879 doi:10.1161/01.CIR.0000138928.83266.24
Lensing AW, Prins MH, Davidson BL, Hirsh J (1995) Treatment of deep venous thrombosis with low-molecular-weight heparins. A meta-analysis. Arch Intern Med 155(6):601–607 doi:10.1001/archinte.155.6.601
Levitan N, Dowlati A, Remick SC, Tahsildar HI, Sivinski LD, Beyth R et al (1999) Rates of initial and recurrent thromboembolic disease among patients with malignancy versus those without malignancy. Risk analysis using Medicare claims data. Medicine (Baltimore) 78(5):285–291 doi:10.1097/00005792-199909000-00001
Lyman GH, Khorana AA, Falanga A, Clarke-Pearson D, Flowers C, Jahanzeb M et al (2007) American Society of Clinical Oncology guideline: recommendations for venous thromboembolism prophylaxis and treatment in patients with cancer. J Clin Oncol 25(34):5490–5505 doi:10.1200/JCO.2007.14.1283
Mandala M, Falanga A, Piccioli A, Prandoni P, Pogliani EM, Labianca R et al (2006) Venous thromboembolism and cancer: guidelines of the Italian Association of Medical Oncology (AIOM). Crit Rev Oncol Hematol 59(3):194–204 doi:10.1016/j.critrevonc.2006.05.001
Marchetti M, Pistorio A, Barone M, Serafini S, Barosi G (2001) Low-molecular-weight heparin versus warfarin for secondary prophylaxis of venous thromboembolism: a cost-effectiveness analysis. Am J Med 111(2):130–139 doi:10.1016/S0002-9343(01)00793-8
Mason DP, Quader MA, Blackstone EH, Rajeswaran J, DeCamp MM, Murthy SC et al (2006) Thromboembolism after pneumonectomy for malignancy: an independent marker of poor outcome. J Thorac Cardiovasc Surg 131(3):711–718 doi:10.1016/j.jtcvs.2005.10.027
Martino MA, Borges E, Williamson E, Siegfried S, Cantor AB, Lancaster J et al (2006) Pulmonary embolism after major abdominal surgery in gynecologic oncology. Obstet Gynecol 107(3):666–671
Meyer G, Farge D, Sauvaget F, Diehl JL, Herve R, Rouffy J et al (1994) Thromboembolic disease and cancer. Presse Med 23(38):1767–1771
Meyer G, Marjanovic Z, Valcke J, Lorcerie B, Gruel Y, Solal-Celigny P et al (2002) Comparison of low-molecular-weight heparin and warfarin for the secondary prevention of venous thromboembolism in patients with cancer: a randomized controlled study. Arch Intern Med 162(15):1729–1735 doi:10.1001/archinte.162.15.1729
Mismetti P, Quenet S, Levine M, Merli G, Decousus H, Derobert E et al (2005) Enoxaparin in the treatment of deep vein thrombosis with or without pulmonary embolism: an individual patient data meta-analysis. Chest 128(4):2203–2210 doi:10.1378/chest.128.4.2203
Noble SI, Finlay IG (2005) Is long-term low-molecular-weight heparin acceptable to palliative care patients in the treatment of cancer related venous thromboembolism? A qualitative study. Palliat Med 19(3):197–201 doi:10.1191/0269216305pm1008oa
Noble SI, Nelson A, Turner C, Finlay IG (2006) Acceptability of low molecular weight heparin thromboprophylaxis for inpatients receiving palliative care: qualitative study. BMJ 332(7541):577–580 doi:10.1136/bmj.38733.616065.802
Noboa S, Mottier D, Oger E (2006) Estimation of a potentially preventable fraction of venous thromboembolism: a community-based prospective study. J Thromb Haemost 4(12):2720–2722 doi:10.1111/j.1538-7836.2006.02196.x
Opatrny L, Warner MN (2004) Risk of thrombosis in patients with malignancy and heparin-induced thrombocytopenia. Am J Hematol 76(3):240–244 doi:10.1002/ajh.20098
Otten HM, Mathijssen J, ten Cate H, Soesan M, Inghels M, Richel DJ et al (2004) Symptomatic venous thromboembolism in cancer patients treated with chemotherapy: an underestimated phenomenon. Arch Intern Med 164(2):190–194 doi:10.1001/archinte.164.2.190
Palareti G, Legnani C, Lee A, Manotti C, Hirsh J, D’Angelo A et al (2000) A comparison of the safety and efficacy of oral anticoagulation for the treatment of venous thromboembolic disease in patients with or without malignancy. Thromb Haemost 84(5):805–810
Prandoni P, Lensing AW, Piccioli A, Bernardi E, Simioni P, Girolami B et al (2002) Recurrent venous thromboembolism and bleeding complications during anticoagulant treatment in patients with cancer and venous thrombosis. Blood 100(10):3484–3488 doi:10.1182/blood-2002-01-0108
Prandoni P, Falanga A, Piccioli A (2007) Cancer, thrombosis and heparin-induced thrombocytopenia. Thromb Res 120(Suppl 2):S137–S140 doi:10.1016/S0049-3848(07)70143-3
Quinlan DJ, McQuillan A, Eikelboom JW (2004) Low-molecular-weight heparin compared with intravenous unfractionated heparin for treatment of pulmonary embolism: a meta-analysis of randomized, controlled trials. Ann Intern Med 140(3):175–183
Rocha E, Martinez-Gonzalez MA, Montes R, Panizo C (2000) Do the low molecular weight heparins improve efficacy and safety of the treatment of deep venous thrombosis? A meta-analysis. Haematologica 85(9):935–942
Ross S, Soltes D (1995) Heparin and haematoma: does ice make a difference? J Adv Nurs 21(3):434–439 doi:10.1111/j.1365-2648.1995.tb02724.x
Samama MM, Cohen AT, Darmon JY, Desjardins L, Eldor A, Janbon C et al (1999) A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients. Prophylaxis in Medical Patients with Enoxaparin Study Group. N Engl J Med 341(11):793–800 doi:10.1056/NEJM199909093411103
Sideras K, Schaefer PL, Okuno SH, Sloan JA, Kutteh L, Fitch TR et al (2006) Low-molecular-weight heparin in patients with advanced cancer: a phase 3 clinical trial. Mayo Clin Proc 81(6):758–767
Siragusa S, Cosmi B, Piovella F, Hirsh J, Ginsberg JS (1996) Low-molecular-weight heparins and unfractionated heparin in the treatment of patients with acute venous thromboembolism: results of a meta-analysis. Am J Med 100(3):269–277 doi:10.1016/S0002-9343(97)89484-3
Sorensen HT, Mellemkjaer L, Olsen JH, Baron JA (2000) Prognosis of cancers associated with venous thromboembolism. N Engl J Med 343(25):1846–1850 doi:10.1056/NEJM200012213432504
Stein PD, Beemath A, Meyers FA, Skaf E, Sanchez J, Olson RE (2006) Incidence of venous thromboembolism in patients hospitalized with cancer. Am J Med 119(1):60–68 doi:10.1016/j.amjmed.2005.06.058
Ten Cate-Hoek AJ, Prins MH (2008) Low molecular weight heparins in cancer. Management and prevention of venous thromboembolism in patients with malignancies. Thromb Res (in press) doi:10.1016/j.thromres.2006.12.026
Tetsche MS, Norgaard M, Pedersen L, Lash TL, Sorensen HT (2006) Prognosis of ovarian cancer subsequent to venous thromboembolism: a nationwide Danish cohort study. BMC Cancer 6:189 doi:10.1186/1471-2407-6-189
Vucic N, Ostojic R, Svircic T (2002) Treatment of deep vein thrombosis with oral anticoagulants in patients with malignancy: prospective cohort study. Croat Med J 43(3):296–300
Warkentin TE (2004) Heparin-induced thrombocytopenia: diagnosis and management. Circulation 110(18):e454–e458 doi:10.1161/01.CIR.0000147537.72829.1B
Weijl NI, Rutten MF, Zwinderman AH, Keizer HJ, Nooy MA, Rosendaal FR et al (2000) Thromboembolic events during chemotherapy for germ cell cancer: a cohort study and review of the literature. J Clin Oncol 18(10):2169–2178
Zaybak A, Khorshid L (2008) A study on the effect of the duration of subcutaneous heparin injection on bruising and pain. J Clin Nurs 17(3):378–385
Acknowledgements
We wish to thank Mrs. Georgina Caspari for her precious help in editing the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Debourdeau, P., Elalamy, I., de Raignac, A. et al. Long-term use of daily subcutaneous low molecular weight heparin in cancer patients with venous thromboembolism: why hesitate any longer?. Support Care Cancer 16, 1333–1341 (2008). https://doi.org/10.1007/s00520-008-0491-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-008-0491-4