Summary
Objective
The aim of this study was to describe real world extravascular lung water index (EVLWI) measurements obtained by pulse index continuous cardiac output (PiCCO) on the day of admission. These were then related to a radiologic score for lung edema, Halperin score and both the Halperin score and EVLWI were assessed for prediction of in-hospital mortality in critically ill patients.
Methods and results
A total of 311 patients admitted to a tertiary medical university hospital between February 2004 and December 2010 were included in this retrospective analysis and of these 177 patients were intubated. In-hospital mortality was assessed by logistic regression. In the overall cohort, EVLWI and the Halperin score correlated poorly (r = 0.17; p = 0.02). In intubated patients, EVLWI and Halperin score did not correlate (r = 0.09; p = 0.39), whereas in patients who were not intubated there was a moderate association (r = 0.30; p = 0.007).
In the overall cohort, (a) EVLWI (hazard ratio [HR] 1.10, 95% confidence interval [CI] 1.02–1.19; p = 0.01; area under the curve [AUC] 0.63, 95% CI 0.54–0.71) but not (b) Halperin score (HR 1.00, 95% CI 0.996–1.004; p = 0.94; AUC 0.52, 95% CI 0.45–0.58) was associated with in-hospital mortality There was a robust association of EVLWI (HR 1.12, 95% CI 1.01–1.25; p = 0.03) but not Halperin score (HR 1.003, 95% CI 0.997–1.009; p = 0.30) with mortality in non-intubated patients. In intubated patients, neither EVLWI (HR 0.997 95% CI 0.990–1.003; p = 0.33) nor Halperin score (HR 1.08; 95% CI 0.88–1.32; p = 0.47) was associated with mortality.
Conclusion
The EVLWI correlated moderately with a radiologic score for lung edema, the Halperin score, in non-intubated but not in intubated patients. The EVLWI at admission was associated with in-hospital mortality in our patient collective of critically ill patients and might constitute not only a tool for risk stratification but most importantly a valuable treatment goal.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Although pulmonary arterial catheter (PAC) has been considered the gold standard for cardiac output measurement for the last 40 years, pulse index continuous cardiac output (PiCCO) has been used recently to determine hemodynamic key parameters in critically ill patients [1,2,3,4]. The PiCCO is based on transpulmonary thermodilution and pulse contour analysis [5, 6]. Via a central venous catheter, a cold liquid bolus, which passes through various thoracic compartments is applied in transpulmonary thermodilution. Using a peripheral arterial thermodilution catheter, cardiac output is calculated using the modified Steward-Hamilton equation based on a temperature curve. Information on cardiac index (CI), cardiac output (CO) and stroke volume variation (SVV) is thereby obtained by arterial pulse contour analysis [7].
The extravascular lung water index (EVLWI), thought to reflect pulmonary edema, was described to be predictive for mortality and in critically ill patients suffering from acute lung injury or septic shock [8,9,10,11]. Although PiCCO is certainly less invasive compared to methods like PAC, a procedural risk still remains [12]. Therefore, other measurements of pulmonary edema are of utmost interest. Chest roentgenograms are routinely done in critically ill patients but interpretation is usually not standardized and therefore difficult to compare and to evaluate against objective measurements such as EVLWI. Halperin et al. proposed a score (ranging from 0–390) to objectify lung edema seen on a chest roentgenogram in critically ill patients, which was shown to be correlated to measurements of extravascular lung water by a thermal dye indicator technique [13]. In the original study, only intubated critically ill patients were investigated and an evaluation of the Halperin score in non-intubated patients is lacking.
In our study, we aimed (i) to describe and relate real world EVLWI measurements and Halperin scores and (ii) evaluate both for association with in-hospital mortality.
Material and methods
Study subjects
A total of 311 patients admitted to the tertiary medical University Hospital in Jena between February 2004 and December 2010 were included in this retrospective analysis. Halperin scores were available for all patients and 177 patients were intubated. Data on in-hospital mortality, which was the primary endpoint, was assessed by the χ2-test and logistic regression and was available in 242 patients. Out of 311 patients, 174 were monitored by PiCCO in the ICU. Decisions concerning which patients were monitored by PiCCO depended on the clinical state and available laboratory values in relation to individual clinical experience of the treating physician. There was no predefined treatment algorithm.
Approval for the study was given by the local ethics committee of the Medical Faculty of the Friedrich Schiller University of Jena.
Laboratory analyses
Blood samples were obtained using standard clinical procedures. Laboratory parameters were tested at the Department of Clinical Chemistry at the University Hospital Jena. We report the maximum value of laboratory values that were measured repeatedly on the day of admission depending on the clinical relevance.
Calculation of the Halperin score
For the radiologic calculation of the score proposed by Halperin et al., both lungs were divided on the chest radiographs into a total of six regions, consisting of two upper, two perihilar, and two lower regions. Each of the six regions was scored by using the following scoring system ranging from 0 to 65 points: 0, normal; 10, mild pulmonary vascular congestion; 20, moderate pulmonary vascular congestion; 30, severe pulmonary vascular congestion; 40, interstitial edema without septal lines; 45, interstitial edema with septal lines; 50, mixed interstitial and alveolar edema, with some sparing of pulmonary regions; 55, mixed interstitial and alveolar edema, involving entire regions; 60, alveolar edema, with sparing; 65, alveolar edema involving the entire pulmonary region. Thus, the final radiographic score with a summation of the six regions ranges from 0 to 390 points [13].
Calculation of SAPS2 and APACHE score
Calculations of admission acute physiology and chronic health evaluation (APACHE) scores and simplified acute physiology score II (SAPS2) were performed within 24 h after admission by the treating physician as previously reported [14, 15].
Statistical analysis
Statistical analysis was conducted using SPSS (IBM SPSS Statistics for Mac, Version 24.0. Armonk, NY, USA) and MedCalc (Version 17.4.4 MedCalc, Ostend, Belgium). Normally distributed data are given as mean ± standard error of the mean and compared by Student’s t‑test. Non-normally distributed data are given as median ± interquartile range and compared by the Mann-Whitney U‑test. The χ2-test was applied to calculate differences between groups. Univariate and multivariate logistic regression analyses were used to compare survival data. For the multivariate regression model, cofounders with a p-value < 0.10 in the univariate analysis were included, then a backward variable elimination was performed. Elimination criterion was a p-value of more than 0.10. Receiver operating curve (ROC) analysis was done and area under the curve (AUC) was calculated. Correlation between continuous parameters was assessed by Pearson’s correlation coefficient. An optimal statistical cut-off was assessed by means of the Youden Index.
Results
Baseline characteristics
Baseline characteristics of patients are shown in Table 1 and admission diagnosis in Table 2. The median Halperin score was 120. Median ELVWI was 8.9 ml/kg body weight (BW). Patients (age 63 ± 1 year) included in this analysis were severely ill as represented by both high SAPS2 (42 ± 2) and APACHE2 scores (23 ± 1). Patients were split into above and below median Halperin scores: patients showing Halperin score above 120 were older (65 ± 1 years vs. 61 ± 1 years) but neither SAPS2 (42 ± 2 vs. 43 ± 3; p = 0.65) nor APACHE2 (22 ± 1 vs. 23 ± 1; p = 0.89) differed. Patients were split in above and below median EVLWI: patients evidencing EVLWI above 8.9 were of similar age (66 ± 1 years vs. 63 ± 2 years; p = 0.15) and similarly ill as expressed by equal APACHE2 (23 ± 2 vs. 21 ± 2; p = 0.30) and SAPS2 (44 ± 3 vs. 41 ± 3; p = 0.62) scores.
Correlation of EVLWI and Halperin score
In the overall cohort, EVLWI and Halperin score correlated poorly (r = 0.17; p = 0.02; Fig. 1). Halperin score was moderately predictive for EVLWI > 8.9 (AUC 0.55, 95% CI 0.47–0.64). Similarly, EVLWI was a poor predictor for Halperin score > 120 (AUC 0.57, 95% CI 0.49–0.66). In intubated patients, EVLWI and Halperin score did not correlate (r = 0.09; p = 0.39), whereas in patients not intubated there was some association (r = 0.30; p = 0.007). Still, in non-intubated patients EVLWI was moderately discriminative for a Halperin score > 120 (AUC 0.60; 95%CI 0.48–0.73) and likewise Halperin score moderately predictive for EVLWI > 8.9 (AUC 0.63, 95% CI 0.50–0.75). This weak correlation between EVLWI and Halperin score could be verified in both patients with Halperin score ≤ 120 (r = 0.09; p = 0.04), and patients with Halperin score > 120 (r = −0.11; p = 0.003).
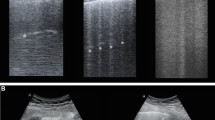
Survival analysis
In the overall cohort EVLWI (HR 1.10, 95% CI 1.02–1.19; p = 0.01; AUC 0.63, 95% CI 0.54–0.71, Fig. 2a) but not Halperin score (HR 1.00, 95% CI 0.996–1.004; p = 0.94; AUC 0.52, 95% CI 0.45–0.58; Fig. 2b) was associated with in-hospital mortality. This remained true after correction for both SAPS2 or APACHE2 in multivariate analysis (Table 3). A statistically optimal cut-off was calculated with EVLWI 8.6 ml/kg BW. Patients with ELVWI > 8.6 suffered from increased in-hospital mortality (24% vs. 6%; p = 0.04). To exclude concomitant pneumonia as confounder, we assessed the association of both EVLWI (1.11, 95% CI 1.01–1.23; p = 0.03) and Halperin score (0.998, 95% CI 0.993–1.003; p = 0.47) in those patients not suffering from pneumonia, showing similar results.
Again, there was a robust association of EVLWI (HR 1.12, 95% CI 1.01–1.25; p = 0.03) but not Halperin score (1.003, 95% CI 0.997–1.009; p = 0.30) with mortality in non-intubated patients. In intubated patients, neither EVLWI (HR 0.997, 95% CI 0.990–1.003; p = 0.33) nor Halperin score (HR 1.08, 95% CI 0.88–1.32; p = 0.47) was associated with mortality. Due to low patient numbers and missing values, multivariate analysis was not possible in the subgroup of non-intubated patients.
Discussion
In our study the Halperin score correlated with EVLWI in non-intubated but not intubated patients. Furthermore, Halperin score was not associated with mortality and was not useful for prediction of mortality in any subgroup of our study cohort. The EVLWI was associated with in-hospital mortality and might therefore be useful for risk stratification. Certainly, our study is underpowered for definite mortality analysis and our results are at this point descriptive, but generate an important thesis: As the EVLWI might also be influenced by physicians using diuretics, vasopressors or vasodilators, it might also constitute a potential treatment goal. In our study there was no predefined treatment algorithm taking either the Halperin score or EVLWI measurements into account in a standardized way, treatment decisions were done solely on the on-call physician’s discretion. Therefore, in a next step studies evaluating treatment, especially concerning fluid management, based on predefined treatment algorithms are necessary to assess the value of EVLWI as treatment goal in the critically ill as already proposed in sepsis, subarachnoid hemorrhage and acute respiratory distress syndrome [16].
Of note, there were differences between intubated and non-intubated patients concerning the correlation between EVLWI and Halperin score. Contrary to our anticipation, Halperin score and EVLWI showed no correlation at all in intubated patients in whom the score was originally evaluated by Halperin et al. in 1985 [13]. In non-intubated patients there was a moderate association of EVLWI and Halperin score. Due to the retrospective design of the study we do not have information on the respiratory parameters, but we speculate that Halperin score might have been influenced by mechanical respiration, in particular by (high) positive end-expiratory pressures, which might be necessary in critically ill patients at admission. Further, lung edema might be influenced by other pulmonary radiographic pathologies, e.g., pneumonic infiltrates, atelectasis, from which the lung edema is difficult to distinguish in patients both critically ill and intubated.
Our findings that a hemodynamic measurement but not a radiologic score was useful for prediction of in-hospital mortality warrant further studies comparing chest roentgenograms with PiCCO measurements. Scorings tools like the Halperin score might help objectify radiologic findings in future studies.
Conclusion
The EVLWI correlated moderately well with a radiologic score for lung edema, the Halperin score in non-intubated patients but not in intubated patients. The EVLWI at admission was associated with in-hospital mortality in our patient collective of critically ill patients and might constitute not only a tool for risk stratification but most importantly a valuable treatment goal. Targeting EVLWI might help further improve patient outcomes.
Abbreviations
- CO:
-
Cardiac output
- CVP:
-
Central venous pressure
- EVLWI:
-
Extravascular lung water index
- GEDVI:
-
Global end-diastolic volume index
- ICU:
-
Intensive care unit
- ITBVI:
-
Intrathoracic blood volume index
- PAC:
-
Pulmonary artery catheter
- PICCO:
-
Pulse index continuous cardiac output
- SVRI:
-
Systemic vascular resistance index
References
Swan HJ, Ganz W, Forrester J, Marcus H, Diamond G, Chonette D. Catheterization of the heart in man with use of a flow-directed balloon-tipped catheter. N Engl J Med. 1970;283(9):447–51. https://doi.org/10.1056/nejm197008272830902. Epub 1970/08/27.
Kirton OC, Calabrese RC, Staff I. Increasing use of less-invasive hemodynamic monitoring in 3 specialty surgical intensive care units: a 5-year experience at a tertiary medical center. J Intensive Care Med. 2015;30(1):30–6. https://doi.org/10.1177/0885066613498055. Epub 2013/08/14.
Wernly B, Lichtenauer M, Franz M, Fritzenwanger M, Kabisch B, Figulla HR, et al. Pulse contour cardiac output monitoring in acute heart failure patients : assessment of hemodynamic measurements. Wien Klin Wochenschr. 2016;128(23/24):864–9. https://doi.org/10.1007/s00508-016-1048-z. PubMed PMID: 27525745; PubMed Central PMCID: PMCPMC5161758.
Ritter S, Rudiger A, Maggiorini M. Transpulmonary thermodilution-derived cardiac function index identifies cardiac dysfunction in acute heart failure and septic patients: an observational study. Crit Care. 2009;13(4):R133. https://doi.org/10.1186/cc7994. Epub 2009/08/13.
Oren-Grinberg A. The PiCCO Monitor. Int Anesthesiol Clin. 2010;48(1):57–85. https://doi.org/10.1097/AIA.0b013e3181c3dc11. Epub 2010/01/13.
Litton E, Morgan M. The PiCCO monitor: a review. Anaesth Intensive Care. 2012;40(3):393–409. Epub 2012/05/15.
Cottis R, Magee N, Higgins DJ. Haemodynamic monitoring with pulse-induced contour cardiac output (PiCCO) in critical care. Intensive Crit Care Nurs. 2003;19(5):301–7. Epub 2003/10/01.
Jozwiak M, Silva S, Persichini R, Anguel N, Osman D, Richard C, et al. Extravascular lung water is an independent prognostic factor in patients with acute respiratory distress syndrome. Crit Care Med. 2013;41(2):472–80. https://doi.org/10.1097/CCM.0b013e31826ab377. Epub 2012/12/25.
Kuzkov VV, Kirov MY, Sovershaev MA, Kuklin VN, Suborov EV, Waerhaug K, et al. Extravascular lung water determined with single transpulmonary thermodilution correlates with the severity of sepsis-induced acute lung injury. Crit Care Med. 2006;34(6):1647–53. https://doi.org/10.1097/01.ccm.0000218817.24208.2e. Epub 2006/04/21.
Wang ZY, Bai Y. Extravascular lung water and pulmonary vascular permeability index may inadvertently delay the identification of acute respiratory distress syndrome. Crit Care. 2013;17(2):420. https://doi.org/10.1186/cc12542. PubMed PMID: 23522053; PubMed Central PMCID: PMCPMC3672491.
Wang H, Cui N, Su L, Long Y, Wang X, Zhou X, et al. Prognostic value of extravascular lung water and its potential role in guiding fluid therapy in septic shock after initial resuscitation. J Crit Care. 2016;33:106–13. https://doi.org/10.1016/j.jcrc.2016.02.011. PubMed PMID: 27021852.
Gassanov N, Caglayan E, Nia A, Erdmann E, Er F. Hemodynamic monitoring in the intensive care unit: pulmonary artery catheter versus PiCCO. Dtsch Med Wochenschr. 2011;136(8):376–80. https://doi.org/10.1055/s-0031-1272539. PubMed PMID: 21332037.
Halperin BD, Feeley TW, Mihm FG, Chiles C, Guthaner DF, Blank NE. Evaluation of the portable chest roentgenogram for quantitating extravascular lung water in critically ill adults. Chest. 1985;88(5):649–52. PubMed PMID: 3902385.
Knaus WA, Zimmerman JE, Wagner DP, Draper EA, Lawrence DE. APACHE-acute physiology and chronic health evaluation: a physiologically based classification system. Crit Care Med. 1981;9(8):591–7. Epub 1981/08/01.
Le Gall JR, Lemeshow S, Saulnier F. A new simplified acute physiology score (SAPS II) based on a European/north American multicenter study. J Am Med Assoc. 1993;270(24):2957–63. Epub 1993/12/22.
Mutoh T, Kazumata K, Ajiki M, Ushikoshi S, Terasaka S. Goal-directed fluid management by bedside transpulmonary hemodynamic monitoring after subarachnoid hemorrhage. Stroke. 2007;38(12):3218–24. https://doi.org/10.1161/strokeaha.107.484634. Epub 2007/11/10.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
B. Wernly, S. Haumann, M. Masyuk, J. Muessig, M. Lichtenauer, L. Bäz, M. Franz, A. Pfeil, A. Lauten, P.C. Schulze, U.C. Hoppe, M. Kelm, R. Westenfeld, C. Jung, and D. Renz declare that they have no competing interests.
Ethical standards
The study was approved by the local ethics committee of Jena University Hospital and the Medical Faculty of the Friedrich Schiller University of Jena. The local ethics committee of Jena University Hospital waived the need to obtain written informed consent to participate from the patients involved in this study, as the data were collected retrospectively.
Additional information
Availability of supporting data
All data relevant for this study will be given by the authors upon specific request without restriction.
Rights and permissions
About this article
Cite this article
Wernly, B., Haumann, S., Masyuk, M. et al. Extravascular lung water index and Halperin score to predict outcome in critically ill patients. Wien Klin Wochenschr 130, 505–510 (2018). https://doi.org/10.1007/s00508-018-1370-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-018-1370-8