Summary
Background
Viral or bacterial upper respiratory infections are the most common cause of acute exacerbation of chronic obstructive pulmonary disease (AECOPD). Based on available data, no reliable parameter has been presented to distinguish between bacterial and nonbacterial exacerbations. Therefore, we compared the diagnostic value of procalcitonin (PCT) level, which is a newer marker for predicting bacterial infections in patients with AECOPD, to routine parameters such as C-reactive protein (CRP) levels and the neutrophil/lymphocyte (N/L) ratio.
Methods
This study included all consecutive patients who were admitted for a diagnosis of AECOPD between January 1 and March 31, 2014. PCT, CRP, and the N/L ratio were assessed in addition to cultures from tracheal aspirates or sputum on the first day of admission. Patients with a pneumonic infiltration on chest radiographs, or an extrapulmonary infection focus, or whose blood samples were not obtained for PCT and/or CRP at the same time as sputum culture were excluded from the study.
Results
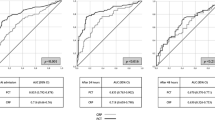
A total of 77 patients were included with a mean age of 71.7 ± 9.5 years. Bacteria were isolated in 37.4 % of the patients. Mean PCT levels were significantly higher in patients with positive sputum cultures than in patients with negative sputum cultures. The cut-off values for PCT, CRP, and the N/L ratio for predicting a bacterial infection were 0.40 ng/mL, 91.50 mg/L, and 11.5, respectively; sensitivity was 61, 54, and 61 % respectively; specificity was 67, 52, and 58 %, respectively; and the area under the curve (AUC) values were 0.64, 0.52, and 0.58, respectively. The AUC value of PCT was significantly better for predicting bacterial infection compared with the CRP level or the N/L ratio (p = 0.042).
Conclusion
PCT was better than CRP and the N/L ratio for predicting a bacterial infection in hospitalized patients with AECOPD. However, we find PCT not so reliable in predicting bacterial infection in AECOPD due to sensitivity and specificity of less than 80 % and a low AUC value.
Zusammenfassung
Hintergrund
Virale oder bakterielle Infektionen des oberen Respirationstraktes sind die häufigste Ursache einer akuten Exazerbation einer chronisch obstruktiven Lungenerkrankung (COPD). Bis jetzt ist kein verlässlicher Parameter bekannt, der in der Lage ist, zwischen bakteriellen und nicht-bakteriellen Exazerbationen zu unterscheiden. Wir haben daher den diagnostischen Wert der Konzentrationen von Procalcitonin (PCT), einem neueren Marker zur Vorhersage bakterieller Infektionen bei Patienten mit COPD, mit dem der herkömmlichen Routineparameter, wie dem C-reaktivem Protein (CRP) und dem Neutrophilen/Lymphozyten (N/L) Quotienten, verglichen.
Methoden
Diese Studie schloss alle konsekutiven Patienten ein, die mit der Diagnose einer COPD zwischen 1. Jänner und 31. März 2014 aufgenommen waren. PCT, CRP und die N/L Quotienten wurden zusätzlich zu Kulturen von Aspiraten aus der Trachea oder von Sputa am Aufnahmetag erhoben. Patienten mit einem Lungeninfiltrat oder einem extrapulmonalen Infektionsherd und/oder deren Blutproben nicht am selben Tag wie die Sputum Kulturen abgenommen waren, wurden aus der Studie ausgeschlossen.
Ergebnisse
Siebenundsiebzig Patienten mit einem mittlerem Alter von 71,7 ± 9,5 Jahren wurden in die Studie aufgenommen. Bei 37,4 % der Patienten konnten Bakterien isoliert werden. Die mittleren PCT Werte waren bei den Patienten mit positiven Sputum Kulturen signifikant höher als bei denen mit negativen Kulturen. Die Grenzwerte für die PCT, CRP und N/L Quotienten Werte zur Vorhersage eines bakteriellen Infektes lagen bei 0,40 ng/mL, 91,50 mg/L, und 11,5. Die Sensitivität war bei 61, 54, und 61 % – die Spezifität bei 67, 52, und 58 %, die Flächen unter der Kurve (AUC) 0,64, 0,52, and 0,58. Die AUC der PCT Werte war bei der Vorhersage von bakteriellen Infekten im Vergleich zu den CRP Werten und den N/L Quotienten signifikant besser (p = 0,042).
Schlussfolgerung
Bei Patienten mit COPD war das PCT bei der Vorhersage von bakteriellen Infekten besser als das CRP beziehungsweise die N/L Quotienten. Wir sind allerdings der Meinung, dass PCT kein sehr verlässlicher Parameter in der Vorhersage von bakteriellen Infekten ist, da sowohl die Spezifität als auch die Sensitivität unter 80 % liegen, und da auch die AUC niedrig ist.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute exacerbation of chronic obstructive pulmonary disease (AECOPD) is defined as an event with an acute onset characterized by a change in a patient’s respiratory symptoms such as baseline dyspnea or cough and/or sputum beyond day-to-day changes, resulting in treatment modifications [1]. AECOPD is one of the most common reasons for presentation to a hospital particularly during the winter [2]. An increased number of severe exacerbations in patients with chronic obstructive pulmonary disease (COPD) are a negative prognostic factor [3]. The most common causes of exacerbations include factors such as viral or bacterial infections of the lower respiratory tract, air pollution, and cigarette smoking [1]. However, no etiology is found in 30 % of cases [4]. The clinical manifestations of systemic inflammation due to infectious and noninfectious causes are similar in patients with COPD [5]. Treatment of viral illnesses and noninfective causes of inflammation with antibiotics is ineffective and contributes to increased medical costs as well as the development of antibiotic resistance, toxicity, and allergic reactions [6]. The likelihood of having a positive sputum culture is higher in exacerbations with purulent sputum compared with exacerbations with a mucoid sputum [7]. C-reactive protein (CRP) is a sensitive acute-phase reactant and its serum levels increase with infection and chronic inflammatory diseases [8]. Serum CRP levels increase in patients with sputum purulence and a positive sputum culture [5, 9]. Counts of leukocytes and their subtypes are biomarkers of inflammatory diseases. The absolute neutrophil-to-lymphocyte count (N/L) ratio has potential prognostic and predictive value in systemic inflammatory diseases such as cardiovascular and kidney diseases [10]. Based on available data, more specific and reliable biomarkers are needed, as traditional diagnostic parameters such as CRP and leukocyte count have no specificity for distinguishing infectious from noninfectious causes of AECOPD [11]. Procalcitonin (PCT) is a precursor of calcitonin that is normally produced by thyroid C-cells. It was first used in 1993 by Assicot et al. [12] to distinguish bacterial meningitis from viral meningitis in children. PCT levels increase in the presence of systemic, bacterial, fungal, and parasitic infections but remain normal or slightly increased in viral infections [8].
Several studies on respiratory tract infections including AECOPD have shown that PCT can be used to identify a bacterial infection and reduce antibiotic use [4]. Simon et al. [13] performed a meta-analysis to evaluate the accuracy of PCT and CRP levels for diagnosing a bacterial infection. The diagnostic accuracy of PCT seemed to be higher than that of CRP among patients hospitalized with suspected bacterial infections [13].
Thus, we evaluated the correlation between positive sputum cultures and serum levels of PCT in addition to traditional parameters such as CRP and the N/L ratio in patients who were hospitalized for AECOPD.
Material and methods
Ethical approval was given by the ethics committee of our institution, and written informed consent was obtained from each patient.
All consecutive patients who were admitted to the Respiratory Intensive Care Unit and Chest Diseases Department of the Medical Faculty of Bülent Ecevit University between January 1 and March 31, 2014, with a diagnosis of AECOPD were included in the study. In addition to chest radiography and routine parameters (complete blood cell count, erythrocyte sedimentation rate, and CRP levels), cultures from tracheal aspirates or sputum and serum PCT levels were assessed on the first day of admission. Spontaneously expectorating sputum or tracheal aspirate samples were collected from patients. All respiratory samples (sputum or aspirate) were processed within 2 h for Gram stain and culture. Bacterial isolation and identification were performed using standard techniques. If there were < 10 epithelia in each field under 100 × magnification, and > 25 neutrophils in each field under 10 × magnification, the sputum sample was considered adequate and was processed. Growth of 105 cfu/mL was considered positive. All patients were started on standard bronchodilator therapy, controlled oxygen therapy, and empirical antibiotherapy, which were modified according to the culture results. Serum PCT levels were measured with the Mini VIDAS immunoassay analyser (BioMérieux, Inc., Cicero NY, USA) using an enzyme-linked fluorescent immunoassay. The upper and lower detection limits were 200 and 0.05 ng/mL, respectively. CRP levels were measured with a Beckman Coulter Image 800 instrument (Beckman Coulter, Inc., Brea, CA, USA) using a nephelometric assay. Patients were divided into groups based on their culture results: positive and negative groups. Variables such as age, sex, length of stay, PCT, CRP, and N/L ratio were compared between the two groups. Patients who failed to provide an adequate sputum sample on the first day of admission, or with a pneumonic infiltration on chest radiographs, or whose blood samples were not obtained for PCT and/or CRP at the same time as sputum culture were excluded from the study. Furthermore, patients with an extrapulmonary focus of infection and those who failed to provide written consent were excluded. The diagnosis of COPD was made according to the spirometric GOLD criteria [1]. Clinical and radiological compatibility and a history of COPD diagnosed by a physician were essential in patients who were unable to undergo spirometry. We used SPSS ver. 17.5 software for statistical analyses. The intergroup comparisons of frequencies and percentages were made using the χ2 test and Fisher’s exact test. Student’s t-test or the nonparametric Mann–Whitney U-test was used to compare the means of variables were appropriate. The significance level was set at p < 0.05 for interpretations. A receiver operator characteristic (ROC) curve analysis was used to evaluate the predictive performance of PCT, CRP, and the N/L ratio for culture positivity, providing the best cut-off value and the area under the ROC curve (AUC) values for culture positivity as well as sensitivity and specificity values.
Results
Among the 102 patients, we excluded 12 patients due to the lack of a sputum sample, 5 patients due to chest radiography showing pneumonic infiltrate, 9 patients due to lack of PCT and/or CRP at the same time as sputum culture, and 1 patient due to a concurrent urinary tract infection. Hence, the study included 77 patients: 56 men (72.2 %) and 21 women (27.8 %) with a mean age of 71.7 ± 9.5 years (Table 1). A quantitative endotracheal aspirate sample was collected from 26 patients, while a spontaneously expectorating sputum sample was obtained from 51 patients. A total of 66 (85 %) patients fulfilled the criteria for adequate samples (< 10 epithelia in each field under 100 × magnification, and > 25 neutrophils in each field under 10 × magnification). A bacterial pathogen was isolated in 28 (37.6 %) of 77 patients with AECOPD: in 15 (26.7 %) of 56 patients (72.7 %) with a sputum sample vs. 13 (50 %) of 26 patients (27.3 %) with a tracheal aspirate sample. Of the isolated bacteria, 19 (68 %) were Gram-negative and 9 (32 %) were Gram-positive. No significant differences were found in variables such as PCT, CRP, or the N/L ratio among patients with isolated Gram-negative or Gram-positive bacteria. The most frequently isolated bacteria included Haemophilus influenzae in seven patients (25 %), Pseudomonas aeruginosa in six (21 %), and Streptococcus pneumonia in five (18 %) (Table 1). A total of 19 of 28 (67 %) patients with bacterial growth in their culture were admitted to the intensive care unit. Mortality rate was significantly higher in patients with positive culture results (57 %) than in those with negative culture results (22 %) (Table 2). The mean PCT, CRP, and N/L ratio levels were not significantly different between survivor and nonsurvivor AECOPD patients (data not shown). The mean pCO2 value was significantly higher in patients with positive culture results than in those with negative culture results, whereas no significant difference was observed for length of hospital stay, spirometric values, or leukocyte count between the two groups (Table 3). PCT level was below the lower detection limit of 0.05 ng/mL in 21 patients (27.2 %). Of these patients, 16 (76 %) were in the negative-culture group and 5 (24 %) were in the positive-culture group. In other words, PCT level was < 0.05 ng/mL in 32 % of the patients without any bacterial pathogen and 18 % of patients with a bacterial pathogen. Mean PCT and CRP levels and the N/L ratio were 2.93 ± 6.6 ng/mL, 106.7 ± 83 mg/dL, and 22.3 ± 20 in patients with positive culture results, respectively, and 0.75 ± 1.29 ng/mL, 105.6 ± 101 mg/dL, and 16.4 ± 13.9 in patients with a negative culture result, respectively (Table 3). Mean PCT level was significantly higher in patients with a positive culture result than those with a negative culture result (p = 0.027), whereas no significant difference was found in CRP level or the N/L ratio (Fig. 2). The best cut-off values in the ROC curve analysis for PCT, CRP, and the N/L ratio with a positive culture result were 0.40 ng/mL, 91 mg/L, and 11.5, respectively; sensitivity was 60, 53, and 60 %; specificity was 67, 52, and 52 %; and AUC values were 0.64, 0.52, and 0.58 for predicting a bacterial infection (Table 4). The AUC was significantly higher compared to the CRP level and the N/L ratio for predicting blood culture positivity with PCT (p = 0.041) (Fig. 1). When the cut-off value for PCT was 1.03 ng/mL, specificity increased to 83 % while sensitivity decreased to 40 %. Similarly, when the CRP and N/L ratio cut-off values were 42 mg/dL and 7.2, respectively, their sensitivity increased to 82 and 79 %, respectively, while specificity decreased to 35 % for each (Table 4). A correlation analysis showed a weak but significant positive correlation between PCT and the N/L ratio and PCT and CRP levels (r = 0.47, p = 0.000, and r = 0.409, p = 0.001, respectively).
Discussion
We found that the detection rate of bacterial pathogens using standard culture procedures was 37.4 % in patients who were admitted to the hospital for AECOPD. Bacterial pathogens were isolated in only one-third of our patients. Mean PCT level was significantly higher in patients with a positive culture result compared with those with a negative culture result.
Several studies have reported positive-culture rates of 17–58 % in patients with AECOPD [11, 14–17]. Our results are consistent with the literature. As expected, 68 % of potentially pathogenic bacteria in our study that were isolated in patients with AECOPD were Gram-negative. Similarly, Lacoma et al. [4] found that Gram-negative bacteria accounted for 73 % of the bacteria in sputum cultures of patients with AECOPD. In the present study, the most common pathogens in AECOPD included H. influenzae, P. aeruginosa, and Streptococcus pneumoniae. The most frequent causative agent in bacterial AECOPD is usually H. influenzae, which is often followed by S. pneumoniae and Moraxella catarrhalis [18, 19]. However, recent studies [2, 4, 11, 14–17] have reported H. influenzae, S. pneumoniae, and P. aeruginosa as the most common pathogens isolated. Furthermore, in a recent study by Peng et al. [20], P. aeruginosa (25.4 %) was the most common species isolated in patients with AECOPD. Therefore, we believe that bacteria isolated in patients with AECOPD may differ from patient to patient depending on conditions such as frequency of hospitalization, antibiotic use, underlying comorbid disease, and/or disease severity.
No significant differences were found in PCT, CRP, or the N/L ratio between patients with respect to bacterial pathogens isolated from culture. Similarly, no significant differences were observed in PCT, CRP, or the N/L ratio between patient groups with respect to Gram-negative and Gram-positive growth. Similarly, both Gaini et al. [21] and Lacoma et al. [4] reported no difference in PCT or CRP levels between pathogens with respect to Gram-staining results.
We found that mean PCT levels in patients with positive culture results were significantly higher than those in patients with negative culture results. However, no significant difference was found for CRP or the blood N/L ratio. Similar to our study, Mohamed et al. [11] found that mean PCT level was significantly higher in patients with bacterial AECOPD than in those with nonbacterial AECOPD (2.69 ± 0.62 and 0.07 ± 0.02 ng/mL, respectively). However, unlike our study, both CRP and leukocyte count were significantly higher in patients with bacterial AECOPD than in those with nonbacterial AECOPD (71.4 and 22.7 mg/L, 12,500 ± 4500 and 6500 ± 2600/mm3, respectively).
In a recent study [21], median PCT and CRP levels were significantly higher in patients with bacterial AECOPD than in those with nonbacterial AECOPD. They found a cut-off value of 19.65 mg/L for CRP to distinguish bacterial AECOPD from nonbacterial AECOPD. Although this cut-off value was substantially lower than our cut-off value, sensitivity, specificity, and AUC for predicting bacterial presence were higher than those in our study (84.61, 78.18, and 0.832 %, respectively). Similar to our results, Dev et al. [2] found that mean CRP level was 103 ± 98 mg/L in a group with bacterial infection, and 92 ± 90 mg/L in a group without bacterial infection. No significant difference was found between the two groups.
In contrast, Lacoma et al. [4] reported no significant difference in PCT or CRP levels when a group of bacterial isolation was compared with a group of negative culture or normal flora results. Gaini et al. [19] showed that PCT had no diagnostic role in mild infection and sepsis, whereas CRP, interleukin-6, and lipopolysaccharide-binding protein, performed better than PCT, but they all had sensitivity and specificity values < 80 %. Polzin et al. [8] found significantly higher PCT levels in patients with chronic bronchitis, nosocomial pneumonia, and community-acquired pneumonia compared with those in a control group. However, the levels were below their cut-off level of 0.5 ng/mL in patients with AECOPD.
In the present study, a correlation analysis showed a weak, but significant positive correlation between PCT and the N/L ratio and PCT and CRP (r = 0.47, p = 0.000, and r = 0.409, p = 0.001, respectively). The weak correlation may be attributed to the fact that PCT levels were less than the detection limit of 0.05 ng/mL in 27 % of patients, and < 0.5 ng/mL in 60 % of patients, which is the cut-off value for bacterial infection and sepsis in many studies. Bafadhel et al. [16] found that median PCT and CRP levels were 0.05 ng/mL and 11 mg/L in patients with AECOPD, respectively. They reported a strong correlation between PCT and CRP (r = 0.56 and p = 0.0001) and indicated that it might be related with the fact that bacterial exacerbations were more associated with systemic inflammation than were nonbacterial exacerbations.
In the present study, the ROC curve analysis showed that the best cut-off value for CRP was 91.5 mg/L for predicting bacterial infection, substantially higher than in other studies. It is likely that inflammation in our patients was more severe as the majority of them had severe COPD (GOLD spirometric stage III and IV in 60 % of patients), with severe exacerbations requiring invasive or noninvasive mechanical ventilation support. In the present study, PCT had significantly better performance for predicting bacterial infection than CRP or the N/L ratio. The ROC curve analysis showed that the best cut-off value for PCT in predicting culture positivity was 0.40 ng/mL, and sensitivity, specificity, and AUC values were 60 %, 67 %, and 0.640, respectively, which were significant compared with CRP and the N/L ratio (p = 0.041). Daniels et al. [5] found a correlation between CRP and the presence of bacteria, but not between PCT and the presence of bacteria. However, AUC values for CRP and PCT for predicting the presence of bacteria were similar (0.540 for PCT and 0.609 for CRP, p = 0.19). The authors reported that bacteria in sputum was not an indication of invasive bacterial infection in most patients with AECOPD; rather, it might have triggered local and systemic inflammatory responses, which does not necessarily mean that patients with low PCT levels would not benefit from antibiotics.
In the present study, the blood N/L ratio, as calculated from the complete blood count, showed similar sensitivity and specificity with CRP. Similarly, a stronger correlation was detected between PCT and the N/L ratio similar to that between PCT and CRP. As there was a moderate and significant correlation between PCT and the N/L ratio, the N/L ratio had similar sensitivity and specificity with CRP for predicting a bacterial infection. It is also cheaper and readily accessible; thus, we believe that the N/L ratio can be used as an alternative to both CRP and PCT for predicting bacterial infection in patients with AECOPD. In a study that compared the N/L ratio with traditional parameters including CRP for predicting bacteremia in patients with community-acquired pneumonia presenting to the emergency unit, De Jager et al. [22] showed that the AUC of the N/L ratio ROC curve was significantly higher than that of conventional infection markers, including CRP level. In addition, they found that both positive predictive value and negative predictive value for predicting bacteremia were highest for the N/L ratio.
Gunay et al. [10] compared patients with AECOPD, stable COPD, and healthy controls and found that the N/L ratio values of the stable patients with COPD were significantly higher than those of the healthy controls. During acute exacerbation of the disease there was a further increase compared with the stable period. The N/L ratio values were also positively correlated with serum CRP levels [10].
Undoubtedly our study had some limitations. First, the number of patients was relatively small. Second, we did not perform serological tests for atypical bacterial pathogens. However, if pneumonia is excluded in patients with AECOPD and a fourfold increase in titre or a positive culture result are taken as diagnostic criteria, the incidence of Chlamydia pneumoniae is 3–5 % (Mycoplasma pneumoniae and Legionella species are even more rare) [23]. Thus, we think that not assessing atypical bacteria for the etiology of AECOPD did not greatly affect our results. Similarly, we did not assess the presence of a coinfection for viral etiology via either blood serology or viral culture. This could clarify why we had very high mean CRP levels in patients with bacterial and nonbacterial AECOPD. Another limitation was the absence of any control assessments of CRP, PCT, or N/L ratio. Similarly, any combination of PCT, CRP, and the N/L ratio parameters in two or three groups instead of their individual use would likely have provided very different results. Despite all respiratory samples (sputum/aspirate) were obtained in first 24 h, 20 (26 %) patients’ respiratory samples were obtained after emprical antibotherapy started that might decrease the sensitivity of sputum/aspirate cultures. Another limitation was that pneumonia was excluded with only routine chest radiography in most of the patients (number of the patients that were investigated only supine chest radiography, only erect posteroanterior chest radiography and both chest radiography and computered tomography were 13 (17 %), 47 (61 %), 17 (22 %), respectively). Pneumonic infiltrates may be missed in up to 30 % of patients in routine chest radiographs when compared with high resolution computed tomography of chest [24]. In our patient population especially in patients who were admitted to ICU and who were investigated with supine chest radiography, pneumonia may be missed because of the low sensitivity of routine chest radiography. And this may explain the high mortality rates and high PCT and CRP levels in patients with negative culture results.
Conclusion
In conclusion, we showed that PCT was a better marker for predicting positivity of sputum culture compared with CRP and the N/L ratio especially in severe and hospitalized patients with AECOPD who requires ICU or mechanical ventilation support. Although a significant difference was detected, both sensitivity and specificity of PCT were < 70 % for predicting bacterial etiology, suggesting that it may not be an ideal marker. Considering that CRP and the N/L ratio showed inferior but similar results for predicting bacterial infection in hospitalized AECOPD, and the fact that they are cheaper and more easily accessible, those parameters can also be beneficial and more cost-effective for routine use.
Conflict of interest
The authors declare that they have no competing interests.
References
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: updated 2014. http://www.goldcopd.org/uploads/users/files/GOLD_Report2014_Feb07.pdf. Accessed 30 April 2014.
Dev D, Wallace E, Sankaran R, et al. Value of C-reactive protein measurements in exacerbations of chronic obstructive pulmonary disease. Respir Med. 1998;92:664–7.
Torres A. COPD guidelines in relation to infections: a critical analysis. Breathe. 2009;5(4):317–32. doi:10.1183/18106838.0504.317.
Lacoma A, Prat C, Andreo F, et al. Value of procalcitonin, C-reactive protein, and neopterin in exacerbations of chronic obstructive pulmonary disease. Int J COPD. 2011;6:157–69.
Daniels JMA, Schoorl M, Snijders D, et al. Procalcitonin vs C-reactive protein as predictive markers of response to antibiotic therapy in acute exacerbations of COPD. Chest. 2010;138(5):1108–15.
Nuutilia J, Lilius EM. Distinction between bacterial and viral infections. Curr Opin Pulm Med. 2007;20:304–10.
Wedzicha JA. Exacerbations: etiology and pathophysiologic mechanisms. Chest. 2002;121:136–41.
Polzin A, Pletz M, Erbes R. Procalcitonin as a diagnostic tool in lower respiratory tract infections and tuberculosis. Eur Respir J. 2003;21:939–43. doi:10.1183/09031936.03.00055103
Antonescu-Turcu AL, Tomic R. C-reactive protein and copeptin: prognostic predictors in chronic obstructive pulmonary disease exacerbations. Curr Opin Pulm Med. 2009;15:120–5.
Günay E, Sarınç UlaşlıS, Akar O, et al. Neutrophil-to-lymphocyte ratio in chronic obstructive pulmonary disease: a retrospective study. Inflammation. 2014;37:2. doi:10.1007/s10753-013-9749-1.
Mohamed KH, Abderabo MM, Ramadan ES, et al. Procalcitonin as a diagnostic marker in acute exacerbation of COPD. Egypt J Chest Dis Tuberculosis. 2012;61:301–5.
Delèvaux I, André M, Colombier M, et al. Can procalcitonin measurement help in differentiating between bacterial infection and other kinds of inflammatory processes? Ann Rheum Dis. 2003;62:337–40.
Simon L, Gauvin F, Amre DK, et al. Serum procalcitonin and c-reactive protein levels as markers of bacterial infection: a systematic review and meta-analysis. Clin Infect Dis. 2004;39:206–17.
Daubin C, Parienti JJ, Vabret A, et al. Procalcitonin levels in acute exacerbation of COPD admitted in ICU: a prospective cohort study. BMC Infect Dis. 2008;8:145. doi:10.1186/1471-2334-8-145.
Ko FWS, Ng TKC, Li TST, et al. Sputum bacteriology in patients with acute exacerbations of COPD in Hong Kong. Respir Med. 2005;99:454–60.
Bafadhel M, Clark TW, Reid C, et al. Procalcitonin and C-reactive protein in hospitalized adult patients with community-acquired pneumonia or exacerbation of asthma or COPD. Chest. 2011;139(6):1410–8.
Kherad O, Bridevaux PO, Kaiser L, et al. Is acute exacerbation of COPD (AECOPD) related to viral infection associated with subsequent mortality or exacerbation rate? Open Respir Medi J. 2014;8:18–21.
Domenech A, Puig C, Martí S, et al. Infectious etiology of acute exacerbations in severe COPD patients. J Infect. 2013;67:516–23.
Lieberman D, Lieberman D, Ben-Yaakov M, et al. Infectious etiologies in acute exacerbation of COPD. Diagn Microbiol Infect Dis. 2001;40(3):95–102.
Peng C, Tian C, Zhang Y, et al. C-reactive protein levels predict bacterial exacerbation in patients with chronic obstructive pulmonary disease. Am J Med Sci. 2013;345(3):190–4.
Gaïni S, Koldkjaer OG, Pedersen C, Pedersen SS,. Procalcitonin, lipopolysaccharide-binding protein, interleukin-6 and C-reactive protein in community-acquired infections and sepsis: a prospective study. Crit Care. 2006;10(2):R53.
De Jager CPC, van Wijk PTL, Mathoera RB, et al. Lymphocytopenia and neutrophil-lymphocyte count ratio predict bacteremia better than conventional infection markers in an emergency care unit. Crit Care. 2010;14:R192.
Bartlett JG, Senthi S. Management of infection in exacerbations of chronic obstructive pulmonary disease. In Sexton JD, editor. UpToDate. Waltham. http://www.uptodate.com. Accessed 6 June 2014.
Syrjala H, Broas M, Suramo I, Ojala A, Lahde S. High-resolution computed tomography for the diagnosis of community-acquired pneumonia. Clin Infect Dis. 1998;27:358–63.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tanrıverdi, H., Örnek, T., Erboy, F. et al. Comparison of diagnostic values of procalcitonin, C-reactive protein and blood neutrophil/lymphocyte ratio levels in predicting bacterial infection in hospitalized patients with acute exacerbations of COPD. Wien Klin Wochenschr 127, 756–763 (2015). https://doi.org/10.1007/s00508-014-0690-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-014-0690-6