Abstract
Background
Intentional or unintentional ingestions among children and adolescents are common. There are a number of ingestions amenable to renal replacement therapy (RRT).
Methods
We systematically searched PubMed/Medline, Embase, and Cochrane databases for literature regarding drugs/intoxicants and treatment with RRT in pediatric populations. Two experts from the PCRRT (Pediatric Continuous Renal Replacement Therapy) workgroup assessed titles, abstracts, and full-text articles for extraction of data. The data from the literature search was shared with the PCRRT workgroup and two expert toxicologists, and expert panel recommendations were developed.
Results and Conclusions
We have presented the recommendations concerning the use of RRTs for treatment of intoxications with toxic alcohols, lithium, vancomycin, theophylline, barbiturates, metformin, carbamazepine, methotrexate, phenytoin, acetaminophen, salicylates, valproic acid, and aminoglycosides.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Children are vulnerable to unintentional or intentional causes of intoxication. According to the 2017 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 35th Annual Report, there were 2,115,186 poison exposures across all age groups, including pediatric and adult populations, during 2017 [1]. Of all the reported exposures, children and adolescents 0–19 years old comprised over half of the exposures (1,265,052), with nearly 76% occurring in children < 5 years of age [1] (Fig. 1). Intoxicated children and adolescents were managed with a variety of treatments, including 137 children who received hemodialysis (HD) and 2 who received hemoperfusion [1].
Percentage distribution of exposures among children and adolescents according to age and gender [1]
Reported intoxicants in children who received renal replacement therapies (RRTs) include ethylene glycol, isopropanol, methanol, ethanol, lithium, vancomycin, theophylline, methotrexate, metformin, acetaminophen, carbamazepine, phenytoin, salicylate, valproic acid, aminoglycosides, and barbiturates. Table 1 lists the intoxicant/drug overdose exposures by age group from the 2017 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 35th Annual Report [1]. Table 2 depicts the toxicokinetic, physical, and chemical properties of the intoxicants.
Extracorporeal treatments, RRTs, are the cornerstone of management for certain intoxications when medical management fails to improve the patient’s clinical status or if the patient develops acute kidney injury. Various forms of RRT, such as HD, hemofiltration, hemoperfusion, continuous renal replacement therapy (CRRT), single-pass albumin dialysis (SPAD), peritoneal dialysis, and sustained low-efficiency dialysis (SLED), are used for the treatment of intoxications, with HD as the most commonly used modality. Currently, limited training and expertise hamper the approach to RRT use in pediatric poisoning cases. Furthermore, limited research into toxicokinetics and a lack of management guidelines to treat intoxicated children add to the complexity of the issue. A better understanding of toxicokinetics and specific RRT indications will help pediatric nephrologists provide therapy that is more effective. We, in turn, conducted a review of the literature and developed expert panel (Pediatric Continuous Renal Replacement Therapy (PCRRT) workgroup) recommendations concerning the use of RRT modalities in children with toxic exposures.
Methods
PubMed/Medline, Embase, and Cochrane databases were searched systematically for all the publications regarding drugs/intoxicants and treatment with RRT in pediatric populations, using a specific search strategy (Appendix A). Cleveland Clinic Library and Cleveland Clinic Akron General Library staff supported the literature search. Inclusion criteria were studies involving pediatric patients (ages 0–18 years) and reporting RRT for intoxications/poisonings comprising ethylene glycol, isopropyl alcohol (isopropanol), methanol (methyl alcohol), ethanol (ethyl alcohol), lithium, vancomycin, theophylline, metformin, methotrexate, carbamazepine, phenytoin, valproic acid, barbiturates, salicylates, and aminoglycosides. Two experts from the PCRRT workgroup independently assessed titles, abstracts, and full-text articles for inclusion/exclusion criteria. A third independent expert carried out a similar assessment if the initial two reviewers did not agree. Two expert toxicologists from the Division of Clinical Pharmacology & Toxicology, Akron Children’s Hospital, were also involved in the process of review and developing recommendations. Potentially relevant articles were considered for data extraction. All the data regarding patient characteristics, type of intoxicant, type of RRT, indications for RRT, and outcomes were extracted for review (Table 3).
PCRRT workgroup
The PCRRT workgroup is composed of international pediatric nephrology experts representing diverse pediatric populations and various international professional societies, in addition to expert toxicologists from the Akron Children’s Hospital (Appendix B). The extracted data from the literature search was shared with the PCRRT workgroup, which served as the basis for deliberations regarding the management of intoxications with RRT in children. Subsequently, expert recommendations were developed and presented during the PCRRT workgroup meeting co-chaired by Drs. Rupesh Raina and Timothy Bunchman at the International Society of Nephrology’s World Congress of Nephrology (WCN) from April 12 to 15, 2019, in Melbourne, Australia. The PCRRT workgroup supported the rationale, background, objectives, and outlaying of recommendations. Panel members were carefully chosen for content expertise, including a clinical pharmacist and an expert in epidemiology and guide methodology. All panel members disclosed potential conflicts of interests.
Intoxications
Alcohols
The 2017 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 35th Annual Report mentioned that more than 10,200 American children and adolescents suffered an alcohol intoxication in 2017 [1]. Nearly 53% of these exposures were attributed to ethanol, while isopropanol, ethylene glycol, and methanol comprised the remaining 31, 12, and 4% of cases, respectively [1]. There is still a lack of consensus regarding indications for and management of alcohol intoxications with RRT [35]. A common metabolic pathway (Fig. 2) can be followed for the primary alcohol intoxication [36].
Metabolism of alcohols and associated biochemical changes [36]
Methanol and ethylene glycol intoxications present with increased osmolal gap followed by an anion gap metabolic acidosis; however, isopropanol will present only with an increased osmolal gap.
Ethylene glycol
Ethylene glycol is a toxic alcohol found in anti-freeze, hydraulic brake fluids, de-icing agents, and pesticides [1].
-
Pharmacokinetics: It is a water-soluble substance with a molecular weight of 62 g/mol and a Vd of 0.5–0.8 L/kg and is absorbed in the gastrointestinal tract. It reaches peak levels within 30–60 min post-ingestion [2, 37,38,39] and has a half-life of 3–8 h. It is predominantly eliminated by the liver (80%) and kidney (20%) [40].
-
Toxidrome: The signs of ethylene glycol intoxication are divided into the following categories based on time of onset:
-
0–12 h: central nervous system (CNS) abnormalities, such as nausea/vomiting, ataxia, areflexia, seizures, and coma. CNS manifestations are accompanied by profound metabolic acidosis;
-
12–24 h: cardiopulmonary dysfunction, including hypertension, tachycardia, pulmonary edema, and dyspnea;
-
24–72 h: renal dysfunction characterized by flank pain, hypocalcemia, and acute tubular necrosis.
The clinical features of ethylene glycol poisoning are due to the toxic metabolites of ethylene glycol. Glycolic acid accumulates in high concentrations in the blood [41, 42] and causes severe metabolic acidosis and oxalate precipitates as calcium oxalate in the kidneys and other tissues [38, 39, 43]. Long-term sequelae of diethylene glycol poisoning have been reported in adult patients. In a prospective longitudinal study, diethylene glycol-poisoned survivors were analyzed at 0, 6, 12, and 18 months after the poisoning event. Patients who were dialysis-dependent at the time of enrolment continued to be dialysis-dependent, while the non-dialysis-dependent patients had improved renal function after the acute illness with minimal changes thereafter [44].
Methanol
Methanol is found in illegal spirits, cleaning agents, and automotive fluids. Methanol exposures can be due to ingestion, absorption through the skin, or inhalation.
-
Pharmacokinetics: It is a water-soluble toxic alcohol with a molecular weight of 32 g/mol and a low Vd of 0.6–0.8 L/kg [4, 39]. Depending on the dose, methanol elimination follows first-order kinetics in sub-toxic doses, whereas it changes to zero-order elimination at higher doses.
-
Toxidrome: Methanol is toxic at blood levels > 20 mg/dL, and clinical features appear after 8–24 h. Clinical features include visual, gastrointestinal (GI), and CNS disturbances. Visual changes range from cloudy or blurred vision to complete blindness. GI effects include nausea, vomiting, and abdominal pain [6, 7]. CNS manifestations range from headache, vertigo, lethargy, and confusion in mild–moderate toxicity to coma, depressed mental status, or seizures in severe cases [45]. Abnormal retinal nerve fiber layer evaluation, visual-evoked potentials, and neurological abnormalities have been reported in adult survivors of acute methanol ingestion [46, 47].
Ethanol
Ethanol is most commonly found in alcoholic beverages, but it is also a major component in many common household products, such as mouthwashes and perfumes.
-
Pharmacokinetics: Ethanol, with a molecular weight of 46 g/mol and a Vd of 0.5 L/kg, is water-soluble and quickly reaches peak blood concentration within 30–90 min after consumption [8, 40]. In children younger than five years of age, there may be limited ability to metabolize ethanol due to a deficiency of alcohol dehydrogenase resulting in younger children achieving higher blood alcohol concentrations as compared to adults ingesting an equivalent amount per kg body weight. Accordingly, an ethanol dose of 3 g/kg in children can be lethal, compared to 5–8 g/kg in adults [40].
-
Toxidrome: Symptoms of acute ethanol intoxication range from nausea/vomiting, slurred speech, and hypothermia to more severe presentations, such as lactic acidosis, ketoacidosis, hypoglycemia, CNS manifestations, and respiratory depression [8]. A major distinction in presentation between children and adults is the extent of hypoglycemia that can be seen in children due to poorer glycogen stores and ethanol’s ability to inhibit gluconeogenesis greatly. Ethanol causes both metabolic and respiratory acidosis; however, respiratory acidosis is more predominant in children and adolescents compared to adults [8].
Isopropanol
Isopropanol is found in rubbing alcohol, hair sprays, hand sanitizers, and cleaning agents.
-
Pharmacokinetics: With a molecular weight of 60 g/mol and a Vd of 0.5 L/kg, isopropanol is water-soluble and rapidly reaches peak blood concentrations within 30 min post-consumption and has a half-life of 2.5–6.4 h [40]. A concentration > 4 g/L is toxic in pediatric patients [48].
-
Toxidrome: Major complications of isopropanol intoxication include CNS depression, gastrointestinal irritation, respiratory depression, and cardiovascular collapse. Patients may present with lethargy, stupor, ataxia, hyporeflexia, tremor, emesis, abdominal pain, or gastritis. Severe manifestations of intoxication include respiratory compromise, hypothermia, hypotension, and acute kidney injury along with rhabdomyolysis. Unlike methanol or ethylene glycol intoxication, isopropanol metabolism produces acetone rather than organic acids [48, 49].
Expert panel recommendations for the management of alcohol intoxication:
-
Stabilize the patient with airway, hemodynamic, and circulatory support
-
Obtain laboratory screenings if there is suspicion for toxic alcohol ingestion
-
Arterial blood gas, blood electrolyte panel, glucose level, serum osmolality
-
Acetaminophen and salicylate levels must be determined especially in patients with intentional suicidal ingestions.
-
Urine drug levels should be determined especially in adolescents who may have co-ingested recreational drugs, such as cocaine, marijuana, benzodiazepines, amphetamines, and opiates.
-
Anion gap (AG) = [Na+] − ([Cl−] + [HCO3−]), normal AG = 6–12 mmol/L
-
Calculated osmolarity (mOsm/L) = [2 × serum Na (in mmol/L)] + [glucose (in mmol/L)] + [blood urea nitrogen (in mmol/L)]; measured osmolality is determined by the freezing point depression method.
-
Osmolal gap (OG) = osmolality (measured) − osmolarity (calculated), normal OG = 10–20 mOsm/L of water
-
If both anion and osmolal gaps are elevated, it suggests the presence of unmeasured ions from the metabolism of ethylene glycol, methanol, and ethanol. If only the osmolal gap is elevated, it is more consistent with isopropanol poisoning.
-
Estimate the amount of toxic alcohol present in a patient using OG calculations to determine its contribution to OG: molecular weight of the alcohol × OG [molecular weight of alcohols (in g/mol): ethylene glycol 62, methanol 32, ethanol 46, isopropanol 60]
-
Consider medical management or RRT depending on the clinical status and blood alcohol level of the patient. The United States FDA for the management of methanol and ethylene glycol intoxication has approved Fomepizole, a competitive inhibitor of alcohol dehydrogenase. It is administered as a loading dose of 15 mg/kg body weight followed by infusions of 10 mg/kg every 12 h for four doses; then, it is increased to 15 mg/kg/dose; it should be administered every 4 h during dialysis.
-
In countries where Fomepizole is not available, ethanol is recommended for use in ethylene glycol and methanol poisoning due to its greater affinity for alcohol dehydrogenase than other alcohols. However, ethanol is difficult to dose and maintain appropriate levels, needs compounding by a pharmacist, and irritates the veins on administration. It can complicate fluid balance in oliguric patients, cause hypoglycemia (especially in malnourished patients), and has sedative effects which requires ICU admission and intubation [40, 50].
-
We recommend high-flux HD as the primary RRT modality for alcohol intoxication since it can rapidly lower toxic alcohol levels and correct metabolic abnormalities. CRRT can be an alternative in situations where HD cannot be performed. Despite its lower ability to achieve toxin clearance compared to HD or CRRT, peritoneal dialysis can also be an option if HD or CRRT is not available or medically contraindicated. For alcohol intoxication, the panel recommends initiating RRT in the following situations:
-
Severe acidosis (pH < 7.2)
-
Worsening renal function
-
Refractory clinical response to non-RRT supportive or medical therapy
-
Blood levels > 25–50 mg/dL and no improvement with medical or antidote therapy
Terminate RRT when blood levels < 20 mg/dL.
-
Persistent metabolic acidosis (pH < 7.2) despite non-RRT management
-
New visual changes
-
Worsening renal function
-
Blood levels > 50 mg/dL and no improvement with medical or antidote therapy
Terminate RRT when blood levels < 30 mg/dL
-
Ethanol [8]
-
Worsening CNS status or respiratory depression
-
Refractory clinical response to non-RRT supportive or medical therapy
-
Blood alcohol level > 300 mg/dL with worsening of renal function or presence of other co-ingestions.
-
Presence of hypotension and coma despite supportive therapy
-
Refractory clinical response to non-RRT supportive or medical therapy
-
Blood levels > 500 mg/dL
Lithium
Lithium is commonly used as a mood stabilizer for the treatment of bipolar disorder. In 2017, 623 lithium exposures, in the form of medication, were reported in American children aged 0–19 years [1].
-
Pharmacokinetics: Lithium is a small cation (7 Da) with a low Vd (0.7–0.9 L/kg) across two compartments. Initially, its Vd is 0.4 L/kg in the extracellular space, but following redistribution into intracellular fluid, its Vd is 0.9 L/kg. It has a narrow therapeutic range (0.8–1.2 mEq/L); therefore, monitoring of blood levels is essential to avoid toxic effects [52, 53]. It is quickly absorbed by the GI tract, excreted unchanged by the kidneys, and competes with sodium for reabsorption in the proximal renal tubules [53]. Serum lithium levels should ideally be drawn at least 6–12 h after the last therapeutic dose to avoid falsely elevated results. Note: do NOT measure serum lithium levels from specimen tubes that contain lithium heparin (green top tubes), because this can falsely elevate the levels.
-
Toxidrome: Lithium intoxication is categorized as acute, chronic, or acute-on-chronic. In acute intoxication, lithium-naive individuals present with GI disturbances, such as nausea, vomiting, diarrhea, and minimal neurological effects. Electrocardiographic changes, like bradycardia, prolonged QT interval, transient ST segment depression, and inverted T waves, may be noted. It takes several weeks of exposure to lithium before chronic intoxication can develop [52]. Manifestations of chronic toxicity include neurologic effects, such as lethargy, ataxia, confusion, agitation, neuromuscular excitability, and seizures, including non-convulsive status epilepticus. The clinical and toxic presentations are more concerning in the chronic and acute on chronic intoxication, as more time has elapsed for lithium to accumulate in the tissues [53, 54]. Lithium concentrations can inherently increase due to dehydration, sodium restriction and intrinsic renal dysfunction, or due to effects of medications, such as non-steroidal anti-inflammatory drugs and angiotensin-converting enzyme inhibitors [53, 55]. The final tubular handling of lithium takes place in the late distal tubules and the collecting duct. Lithium enters into the principal cells of the collecting duct through the epithelial sodium channels (ENaC) and causes dysregulation of the aquaporin-2 water channels on the apical surface of the principal cells, thereby preventing the reabsorption of water and causing nephrogenic diabetes insipidus. Lithium-induced nephrogenic diabetes insipidus presents as polyuria and polydipsia [56]. Patients with continued polyuria can develop hypovolemic acute kidney injury resulting in a further elevation of lithium blood levels [54]. Syndrome of irreversible lithium effectuated neurotoxicity (SILENT) is a persistent sequelae of lithium intoxication and may persist for weeks or even up to years. Patients present most commonly with cerebellar dysfunction as a result of lithium-induced demyelination in the CNS [57, 58].
-
Expert panel recommendations for RRT in lithium intoxication: We recommend intermittent HD as the preferred RRT modality for lithium intoxication. Multiple HD sessions may be required to prevent a post-HD rebound rise in lithium blood levels due to the shift of intracellular lithium into the intravascular space [54, 55, 59, 60]. If HD is not an option, CRRT can be considered. Use of sequential therapy, a combination of HD followed by CRRT, prevents the rebound phenomenon [53, 59]. For lithium toxicity, the panel recommends initiating RRT in the following situations: [52, 59, 61]
-
Presence of life-threatening arrhythmias
-
Presence of severe neurological symptoms, such as impaired mental status, progressive confusion, or seizures
-
Renal dysfunction and lithium blood levels > 2.5 mEq/L
-
Lithium blood levels > 4 mEq/L regardless of symptoms
Terminate RRT when blood lithium levels < 1.0 mEq/L
Vancomycin
Vancomycin is a tricyclic glycopeptide antibiotic that has been used for decades to treat methicillin-resistant Staphylococcus aureus and various resistant Gram-positive infections. It is commonly linked to nephrotoxicity, leading to a need for aggressive monitoring. In a retrospective review comparing vancomycin dose and the risk of developing nephrotoxicity, 14% of 167 vancomycin-treated children developed nephrotoxicity, with the greatest risk in those having higher trough levels (> 15 μg/mL) [62].
-
Pharmacokinetics: Vancomycin has a molecular weight of approximately 1450 Da and a high Vd of 0.4–1 L/kg. The kidneys clear approximately 80–90% of the drug; so, its elimination is largely dependent on renal function [63]. The therapeutic daily trough levels for pediatric patients range around 5–10 μg/mL, but higher levels of 15–20 μg/mL can be targeted in severe infections [12]. The elimination half-life for vancomycin is 4–6 h in adults (2–4 h in infants and children) with normal renal function, while in anephric patients, it may increase to as long as 7.5 days [64].
-
Toxidrome: The hallmark signs of toxicity are ototoxicity and nephrotoxicity [11]. The risk of toxicity increases with higher serum trough levels (> 15 μg/mL) and longer duration of therapy, as well as with concomitant use of other nephrotoxic agents, such as aminoglycosides, furosemide, radiocontrast dyes, and amphotericin B [12, 65]. Regular monitoring of vancomycin trough levels in patients receiving other nephrotoxic agents is essential to avoid toxic sequelae [65].
-
Expert panel recommendations for RRT in vancomycin toxicity: We recommend the early use of high-flux HD as the primary choice of RRT for the management of vancomycin intoxication in children. The high flux HD membranes have a larger pore size that enhances the elimination of large protein-bound molecules, such as vancomycin [12]. Charcoal hemoperfusion could be considered if high-flux HD is not available. Initial vancomycin clearance rate is targeted at 40% for charcoal hemoperfusion and 60–70% for high-flux HD [11, 65]. The rationale behind aggressive therapy in vancomycin overdose, especially in children and adolescents, is to avoid nephrotoxicity and ototoxicity [66]. For vancomycin toxicity, the panel recommends initiating RRT in the following situations [65, 66]:
-
Persistently high vancomycin trough levels despite ongoing medical therapy in patients with signs of nephrotoxicity/ototoxicity
-
Presence of renal dysfunction risking further accumulation of the drug
-
Terminate RRT once trough levels < 15 μg/mL and clinical improvement.
Theophylline
Theophylline is prescribed as an adjuvant treatment for acute exacerbations of the symptoms associated with asthma and other chronic lung diseases. In 2017, 11 American children and adolescents aged 0–19 experienced theophylline intoxication, with no reported fatalities [1] as opposed to 73 such exposures in 2006 [67]. This decline in toxic theophylline exposures results from a decrease in its prescription for bronchospasm, due to the availability of newer and safer asthma medications.
-
Pharmacokinetics: Theophylline is a plant-derived methylxanthine with a molecular weight of 180.17 Da that is structurally similar to aminophylline and caffeine [68,69,70]. Nearly 40% of theophylline is plasma protein bound, and it has apparent Vd of 0.45 L/kg (range 0.3–0.7 L/kg). Approximately 90% of the metabolism of theophylline takes place in the liver, and while about 50% of the theophylline dose is excreted unchanged in the urine in neonates, urinary excretion decreases to approximately 10% beyond the early infantile period [69, 70]. Theophylline has a narrow therapeutic range (5–15 mg/L), and non-specific adverse effects may manifest with supratherapeutic blood levels [69], thus making frequent monitoring of serum theophylline concentrations a necessity.
-
Toxidrome: Excessive loading dose or excessive maintenance doses for less than 24 h lead to acute overdose, while chronic over-dosage is due to an excessive maintenance dose for more than 24 h. Mild toxicity signs include nausea, repetitive vomiting, abdominal pain, restlessness, and gastroesophageal reflux. Severe toxicity symptoms include metabolic acidosis, hypokalemia, hypotension, ventricular arrhythmias, and seizures [13, 68, 69]. CNS symptoms such as nervousness, irritability, tremor, disorientation, and seizures occur with rising theophylline concentrations [69].
-
Expert panel recommendations for RRT in theophylline toxicity: We recommend HD as the primary choice of RRT in theophylline intoxication. Although hemoperfusion may have a higher clearance rate (up to six-fold increase) of theophylline than HD, it has limited availability and complications of the procedure may include hypotension, hypocalcemia, platelet consumption, and bleeding diathesis [69]. Serum theophylline concentrations may rebound 5–10 mg/L after discontinuation of RRT due to redistribution of theophylline from the tissue compartment. CRRT can be used if a patient has hypotension, life-threatening dysrhythmias, and seizures. In neonates, exchange transfusions may be considered as an alternative to HD [69]. Therapeutic plasma exchange has been proposed in the past [71], but with the increased use of both HD and CRRT, its application is now exceedingly rare. For theophylline toxicity, the panel recommends initiating RRT in the following situations [69, 70]:
-
For acute toxicity with serum concentration > 30 and < 100 mg/L, if emesis, seizures, or cardiac arrhythmias cannot be adequately controlled, and at serum concentration > 100 mg/L regardless of clinical features
-
In chronic intoxications, with serum concentration > 30 mg/L if vomiting, seizures, or arrhythmias cannot be controlled
-
Presence of depressed mental status or shock despite fluid resuscitation
Terminate RRT when the theophylline level has fallen < 15–20 mg/L.
Barbiturates
Barbiturates are CNS depressants that are used as sedatives, hypnotics, anesthetics, and anti-convulsants. The majority of barbiturate overdoses in American children and adolescents are from long-acting agents, composing 278 of the 287 barbiturate intoxications reported in 2017 [1].
-
Pharmacokinetics: Short-acting barbiturates have a quicker onset as well as a shorter duration of action (< 3 h) than their long-acting counterparts (> 6 h) due to the greater lipid solubility leading to a larger Vd of 0.5–1 L/kg. They are highly protein bound and are considered potentially fatal at levels > 50 mg/L. Long-acting barbiturates, on the other hand, have a smaller Vd (0.25–1.2 L/kg) and become fatal at levels > 80 mg/L [72]. Nearly complete metabolism and conjugation of barbiturates in the liver precedes their renal excretion except for long-acting agents, which are partially excreted unchanged in urine [73].
-
Toxidrome: Barbiturates exert most of their effects on the CNS, respiratory, and cardiovascular systems. Sedation and hypnosis followed by sluggishness, impaired coordination and speech eventually leading to coma are noted with progressively increasing doses. Suppression of the medullary respiratory center causes respiratory depression thereby leading to shallow breathing. Cardiac contractility and vascular tone are affected at higher doses causing low cardiac output and hypotension [72].
-
Expert panel recommendations for RRT in barbiturate intoxication: We recommend HD as the first choice of RRT in severe long-acting barbiturate intoxication. Although hemoperfusion has similar results as HD, due to its limited availability and the various procedure-related complications in hemoperfusion, HD remains the RRT of choice. CRRT is an acceptable modality if HD or hemoperfusion is not available. SLED may be considered as an RRT modality in severe cases, but there are limited data to support its use. For barbiturate toxicity, the panel recommends initiating RRT in the following situations [72, 74]:
-
Presence of prolonged coma with depression of autonomic control of respiratory or circulatory function
-
Presence of shock despite fluid resuscitation
-
Respiratory failure requiring invasive ventilation
Terminate RRT when the patient is clinically stable.
Metformin
Metformin is a biguanide oral anti-hyperglycemic agent used for the treatment of type 2 diabetes mellitus, pre-diabetes, and polycystic ovarian syndrome. In 2017, biguanide exposures occurred in 1399 American children and adolescents [1].
-
Pharmacokinetics: Metformin has a molecular weight of 165 Da with a Vd of 1.1–5 L/kg. The therapeutic range is 0.5–3 mg/L, and toxic effects have been reported at doses > 100 mg/kg in the pediatric age group [75, 76]. It is minimally plasma protein bound and is predominantly cleared by the kidneys. Patients with renal disease, acute kidney injury, and advanced liver disease are at highest risk of toxicity and can develop metformin-induced lactic acidosis.
-
Toxidrome: Metformin-induced lactic acidosis is defined as a blood lactate concentration > 5 mmol/L and arterial pH < 7.35 [77]. Non-specific symptoms, including nausea, vomiting, myalgias, diarrhea, abdominal pain, altered mental status, and hemodynamic instability, can be present. Physical examination findings may include tachycardia, hypotension, and tachypnea in patients with severe lactic acidosis [17, 75]. Alterations in mental status may be due to acidosis or hypoglycemia, although the latter is uncommon without the concurrent use of a hypoglycemic agent.
-
Expert panel recommendations for RRT in metformin toxicity: Despite a high Vd, metformin can be efficiently dialyzed due to its low molecular weight and low protein binding [78]. We recommend HD as the preferred RRT modality, whereas CRRT can be an alternative option. For metformin toxicity, the panel recommends initiating RRT in the following situations [76, 79, 80]:
-
Presence of shock despite fluid resuscitation
-
Severe acidosis with pH < 7.0
-
Deteriorating mental status
-
Refractory to supportive or non-RRT medical measures
Carbamazepine
Carbamazepine is used for the treatment of partial seizures, generalized tonic–clonic seizures, mixed seizure patterns, and trigeminal neuralgia. Carbamazepine overdoses occurred in 328 American children and adolescents in 2017 [1].
-
Pharmacokinetics: Carbamazepine, a lipophilic antiepileptic, has a molecular weight of 236 Da. It has a low Vd of 0.8–1.4 L/kg and is 76% protein bound. It is a major substrate for CYP3A4 which converts it into its active metabolite, Carbamazepine-10, 11-epoxide. The therapeutic concentration range is 4–12 mg/L following chronic administration. Following a single dose of carbamazepine, the average half-life ranges from 35 to 40 h and decreases to 12–17 h on repeated dosing due to carbamazepine inducing its own metabolism. Approximately 72% of an orally administered dose is excreted in urine largely in the form of hydroxylated and conjugated metabolites [81].
-
Toxidrome: Carbamazepine blood levels > 12 mg/L are associated with intoxication in children. Neurological symptoms are the first to appear with seizures being most common in children. Other CNS symptoms include tremors, ataxia, dizziness, extrapyramidal signs, irregular breathing, respiratory depression with impairment of consciousness up to deep coma [81]. Cardiovascular changes like tachycardia, hypotension or hypertension, and shock, conduction disorders with electrocardiographic changes, such as prolonged QRS and QT, can occur in some patients at very high doses. Chronic carbamazepine toxicity can cause headaches, diplopia, and ataxia [82].
-
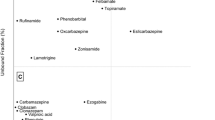
Expert panel recommendation for RRT in carbamazepine intoxication: We recommend high-flux or high-efficiency HD as the preferred RRT modality. Since carbamazepine is highly protein bound, it can be more efficiently removed via CRRT as compared to conventional HD if available. HD is preferred due to its low cost and better availability. For carbamazepine toxicity, the panel recommends initiating RRT in the following situations [83, 84]:
-
Presence of seizures refractory to treatment
-
Life-threatening arrhythmia
-
Declining neurological status/prolonged coma
-
Respiratory depression requiring mechanical ventilation
Terminate RRT when carbamazepine blood levels < 10 mg/L and patient has improved clinically.
Methotrexate
Methotrexate, an immunosuppressive agent [82], is one of the most widely used anti-cancer agents, and administration of high-dose methotrexate [> 0.5 g/m2] [85] followed by leucovorin rescue is an important element in the management of many pediatric cancers.
-
Pharmacokinetics: It has a molecular weight of 454 Da and a Vd of 0.4–0.8 L/kg. Up to 50% of the drug in plasma is protein bound. In pediatric patients, oral absorption of the drug ranges from 23 to 95% depending on the dose administered, while after parenteral administration the drug is completely absorbed [86]. The primary route of elimination is renal. At higher doses of 0.5 to 12 g/m2, methotrexate and its insoluble metabolites may precipitate in the renal tubules and cause reversible acute kidney injury.
-
Toxidrome: The incidence of methotrexate toxicity depends on host factors, supportive measures used, and the dose and schedule of methotrexate. Nephrotoxicity caused by methotrexate arises through crystal nephropathy, which occurs when methotrexate and its metabolites precipitate within the renal tubules. The serum concentration threshold for nephrotoxicity is 2.2 mmol/L when urine pH is 5.5 and 22 mmol/L when the urine pH is 6.9. Methotrexate crystallizes at low (acidic) pH; therefore, increased hydration and urinary alkalization are necessary steps in dosing protocols with high-dose methotrexate as they increase the solubility and excretion of methotrexate [85]. Other symptoms of methotrexate toxicity include stomatitis, esophagitis, myelosuppression, hepatitis, and neurologic dysfunction [82].
-
Expert panel recommendation for RRT in methotrexate intoxication: We recommend using high-flux HD as the preferred RRT modality in pediatric patients. CRRT is a safe alternative for treatment. Since methotrexate is highly protein bound, hemoperfusion, SPAD, and plasmapheresis are effective alternatives. For methotrexate toxicity, the panel recommends initiating RRT in the following situations [23, 77]:
-
Worsening renal dysfunction or acute kidney injury despite hydration, urinary alkalization, or leucovorin
-
Deteriorating neurological status/prolonged coma with depression of autonomic control of respiratory or circulatory function
We also recommend continuing leucovorin along with RRT. It is important to note that leucovorin is dialyzable; therefore, it should be dosed or redosed following HD. Furthermore, a rebound rise in methotrexate concentrations of 10–20% of the post-RRT levels has been reported [85, 87]. The panel recommends continuous monitoring and anticipation for repeat RRT in these cases.
Phenytoin
Phenytoin is a hydantoin derivative used in the management of tonic–clonic and psychomotor seizures and seizures associated with neurosurgery. In 2017, 102 American children and adolescents experienced intoxication with phenytoin [1].
-
Pharmacokinetics: Phenytoin is a highly protein-bound molecule with a molecular weight of 252 Da and a Vd of 0.6–0.8 L/kg. It has a narrow therapeutic index of 10–20 mg/L, and toxicity results if levels exceed 20 mg/L or if more unbound drug is circulating than anticipated, as in the case of hypoalbuminemia [27, 88]. Due to the weakly acidic nature of phenytoin, in patients with renal failure, the free plasma concentration of phenytoin increases. This may lead to the development of clinical symptoms despite the presence of levels below the threshold for intoxication [89].
-
Toxidrome: Phenytoin toxicity can result in an acute or chronic overdose. With mild intoxication, patients may experience nausea, vomiting, diplopia, agitation, nystagmus, and ataxia [82]. Severe intoxication manifests as stupor, coma, and respiratory arrest, although fatalities are rare. Seizures have been reported infrequently with phenytoin intoxication; therefore, other etiologies or ingestion of other drugs should be considered if this is the primary symptom [88].
-
Expert panel recommendations for RRT in phenytoin toxicity: We recommend using high-efficiency HD as the primary RRT modality with intermittent hemoperfusion as an acceptable alternative. Peritoneal dialysis, SPAD, exchange transfusion, and therapeutic plasma exchange do not offer comparable results to HD or hemoperfusion; therefore, they are not recommended for treatment of phenytoin poisoning. These types of continuous techniques result in much lower clearances and removal rates in comparison to intermittent techniques. For phenytoin toxicity, the panel recommends initiating RRT in the following situations [88]:
-
Deteriorating neurological status, or ataxia, or coma with depression of autonomic control of respiratory or circulatory function
-
Persistently elevated phenytoin blood levels refractory to use of non-RRT medical measures
Acetaminophen
Acetaminophen is a commonly used anti-pyretic and analgesic agent. In 2017, there were 35,090 reported cases of children and adolescents with acetaminophen ingestions in the United States and ~ 22% of those cases received n-acetylcysteine (NAC) [1].
-
Pharmacokinetics: Acetaminophen has a molecular weight of 151 Da and a Vd of 1.1–1.2 L/kg in pediatric patients. It has a plasma binding capacity of 10–25%. Lower doses could be considered for infants and children less than two years of age based on simulated pharmacokinetic data [90]. Metabolism of acetaminophen is primarily by glucuronidation and sulfation pathways, while < 5% is metabolized via CYP2E1 and produces the toxic free radical, N-acetyl-p-benzoquinoneimine (NAPQI), which conjugates to glutathione [91]. Following a toxic ingestion, more acetaminophen is metabolized to NAPQI as the primary pathways become saturated. Glutathione stores eventually become depleted, and NAPQI causes hepatotoxicity.
-
Toxidrome: The signs of acetaminophen intoxication are manifested in the following four progressive phases:
-
Phase 1 (0.5–24 h): anorexia, nausea/vomiting, lethargy, and diaphoresis;
-
Phase 2 (24–72 h): right upper quadrant pain, liver enlargement, oliguria, bilirubin and liver enzyme elevation, and prothrombin time prolongation. Phase 1 symptoms become less pronounced during phase 2.
-
Phase 3 (72–96 h): phase 1 symptoms reappear plus signs of hepatic failure like jaundice, hypoglycemia, and encephalopathy, and eventually renal and cardiac failure may develop. With severe toxicity, patients may develop metabolic acidosis, hypothermia, shock, and CNS depression [92].
-
Phase 4 (4–14 days): patient will either recover from liver failure or die from multi-organ failure.
-
-
Expert panel recommendation for RRT in acetaminophen intoxication: NAC is the mainstay of treatment that reduces hepatotoxicity by replenishing glutathione stores and enhancing sulfation, thereby decreasing the toxic effects of NAPQI. For severe acetaminophen ingestions, RRT with HD should be considered. Hemoperfusion or CRRT can be used as alternative treatment options, but HD results in rapid correction of metabolic acidosis and is associated with significantly lesser complications than hemoperfusion [93]. For acetaminophen toxicity, the panel recommends initiating RRT in the following situations:
-
Declining neurological status, such as encephalopathy or coma, with depression of autonomic control of respiratory or circulatory function
-
Severe acidosis pH < 7.1 refractory to supportive therapy
-
Acetaminophen blood levels > 1000 mg/L and NAC therapy has not been initiated
Salicylates
Salicylates have analgesic, anti-inflammatory, and anti-pyretic properties. The most common salicylates include aspirin (acetylsalicylic acid), a phenolic ester, and methyl salicylate (oil of wintergreen), a carboxylic acid ester. Salicylate intoxication was reported in 5734 American children and adolescents in 2017 with 5629 of those exposures due to aspirin alone [1].
-
Pharmacokinetics: Most of the understanding of the pharmacokinetic properties of salicylates comes from aspirin. It has a molecular weight of 180 Da, a narrow Vd of 0.1–0.2 L/kg, and is metabolized primarily in the liver and eliminated by the kidneys. Protein binding at therapeutic doses is about 90%, but at higher serum levels, the unbound fraction increases [94].
-
Toxidrome: Symptoms of mild or early salicylate intoxication include nausea, vomiting, and tinnitus. Respiratory alkalosis occurs early in presentation by stimulation of the medullary respiratory center [13, 74]. If toxicity persists, respiratory alkalosis with anion gap metabolic acidosis results. Moderate salicylate intoxication presents with tachypnea, hyperpyrexia, sweating, dehydration, loss of coordination, and restlessness. In severe intoxication, patients can present with hallucinations, stupor, convulsions, cerebral edema, renal failure, cardiovascular failure, and even coma [95].
-
Expert panel recommendation for RRT in salicylate intoxication: We recommend using HD in severe salicylate poisoning as the primary RRT modality as it is more widely available and is associated with prompt clearance of salicylates and faster resolution of acidemia. Hemoperfusion or CRRT can be used as alternative treatment options. For salicylate toxicity, the panel recommends initiating RRT in the following situations [78, 96]:
-
Deteriorating neurological status or presence of coma with depression of autonomic control of respiratory or circulatory function.
-
Pulmonary or cerebral edema despite use of non-RRT medical therapy
-
Severe acidosis pH < 7.2 despite supportive therapy
-
Salicylate blood levels > 100 mg/dL with normal renal function.
-
Salicylate blood levels > 90 mg/dL with impaired renal function
Valproic acid
Valproic acid, a common anti-epileptic medication, is widely used in the treatment of partial and generalized seizure disorders, as well as mood disorders. It was involved in 836 toxic exposures in American children and adolescents in 2017 [1].
-
Pharmacokinetics: It has a molecular weight of 144 Da, a Vd of 0.1–0.5 L/kg, and the typical therapeutic range for seizures is 50–100 mg/L. At therapeutic doses, it undergoes first-order elimination. The plasma protein binding of valproic acid increases with an increase in the concentration of the drug. With significantly elevated drug concentrations (> 300 mg/L), protein-binding sites become saturated and free valproic acid can accumulate [97, 98].
-
Toxidrome: In mild toxicity (doses ~ 200 mg/kg), patients can develop ataxia and depressed mental status. In severe toxicity (doses > 400 mg/kg), coma, respiratory depression, and hemodynamic instability can occur [97]. Hyperammonemia encephalopathy can occur with therapeutic and supratherapeutic concentrations. Toxic metabolites include 2-propyl-2-pentenoic acid, 2-propyl-4-pentenoic acid, and propionic acid, and they are thought to cause cerebral edema, hepatotoxicity, and hyperammonemia, respectively. Additional valproic acid intoxication complications include hypernatremia, hypocalcemia, hyperosmolarity, and anion gap metabolic acidosis [29]. In patients on long-term valproic acid therapy, it causes subclinical defects of renal tubular function leading to secondary Fanconi syndrome. Fanconi syndrome is characterized by urinary excretion of amino acids, glucose, phosphate, bicarbonate, and uric acid resulting in renal tubular acidosis and eventually growth failure and myopathy [99, 100].
-
Expert panel recommendation for RRT in valproic acid intoxication: We recommend using HD in severe valproic acid intoxication as the primary RRT modality, since at high plasma concentrations, the plasma protein-binding sites become saturated, and more of the free drug is available. Hemoperfusion is an alternate option [97]. For valproic acid toxicity, the panel recommends initiating RRT for any of the indications [97, 101]:
-
Deteriorating neurological status or coma
-
Presence of shock despite fluid resuscitation
-
Respiratory failure requiring invasive ventilation
-
Severe acidosis with pH < 7.1 despite supportive therapy
-
Aminoglycosides
Aminoglycosides, such as gentamicin, amikacin, and tobramycin, are bactericidal antibiotics that act on the 30s ribosomal subunit to inhibit protein synthesis. They provide broad-spectrum coverage of Gram-positive and Gram-negative bacterial species.
-
Pharmacokinetics: Aminoglycosides have poor oral bioavailability, low protein-binding capacity, high Vd, and are primarily eliminated in urine [102]. The standard daily dose varies for each subtype of aminoglycoside but is generally between 7 and 15 mg/kg/day. Dosing regimens can be either once-daily or divided dosing. Therapeutic drug monitoring should be performed with their use, since efficacy and toxicity are associated with low peak and high trough concentrations, respectively. The timing and reference ranges for aminoglycoside concentrations will depend on if the dosing regimen is once-daily or divided dosing.
-
Toxidrome: Aminoglycosides can cause nephrotoxicity, ototoxicity, and neuromuscular blockade at toxic levels [82]. Nephrotoxicity is the most concerning adverse effect associated with aminoglycoside exposure and is associated with a varying degree of renal tubular dysfunction that may lead to acute kidney injury [102]. Neomycin is administered topically or oral due to its systemic toxicity.
-
Expert panel recommendations for RRT in aminoglycoside intoxication: We recommend HD in severe aminoglycoside intoxication as the primary RRT modality. Peritoneal dialysis can be used as an alternative option. For aminoglycoside toxicity, the panel recommends initiating RRT in the following situations:
-
Deteriorating neurological status or coma
-
Presence of shock despite fluid resuscitation
-
Worsening renal function
Conclusion
Accidental and intentional ingestions are relatively common among children and adolescents. RRT may be indicated for some ingestions to enhance elimination (e.g., phenobarbital, toxic alcohols, lithium, salicylates) of the drug or due to side effects of the drug (e.g., nephrotoxicity, metabolic acidosis, hyperammonemia). Currently, there is limited pediatric literature on the use of RRT in the management of ingestions. We have provided our recommendations on the role of RRT for select drug exposures. Nephrologists and toxicologists should continue to explore the role and utility of RRT for different drug toxicities in pediatric patients.
References
Gummin DD, Mowry JB, Spyker DA, Brooks DE, Osterthaler KM, Banner W (2018) 2017 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 35th annual report. Clin Toxicol (Phila) 56(12):1213–1415
Cox RD, Phillips WJ (2004) Ethylene glycol toxicity. Mil Med 169(8):660–663
Stapenhorst L, Hesse A, Hoppe B (2008) Hyperoxaluria after ethylene glycol poisoning. Pediatr Nephrol 23(12):2277–2279
Tadokoro M, Ozono Y, Hara K, Taguchi T, Harada T, Ideguchi M, Senju M (1995) A case of acute renal failure due to ethylene glycol intoxication. Nihon Jinzo Gakkai Shi 37(6):353–356
Brown MJ, Shannon MW, Woolf A, Boyer EW (2001) Childhood methanol ingestion treated with fomepizole and hemodialysis. Pediatrics 108(4):E77
Loza R, Rodriguez D (2014) A case of methanol poisoning in a child. Case Rep Nephrol 2014:652129. https://doi.org/10.1155/2014/652129
Sutton TL, Foster RL, Liner SR (2002) Acute methanol ingestion. Pediatr Emerg Care 18(5):360–363
Gormley NJ, Bronstein AC, Rasimas JJ et al (2012) The rising incidence of intentional ingestion of ethanol containing hand sanitizers. Crit Care Med 40(1):290–294
Mecikalski MB, Depner TA (1982) Peritoneal dialysis for isopropanol poisoning. West J Med 137(4):322–325
Meyer RJ, Flynn JT, Brophy PD et al (2001) Hemodialysis followed by continuous hemofiltration for treatment of lithium intoxication in children. Am J Kidney Dis 37(5):1044–1047
Panzarino VM, Feldstein TJ, Kashtan CE (1998) Charcoal hemoperfusion in a child with vancomycin overdose and chronic renal failure. Pediatr Nephrol 12(1):63–64
Stidham T, Reiter PD, Ford DM, Lum GM, Albietz J (2011) Successful utilization of high-flux hemodialysis for treatment of vancomycin toxicity in a child. Case Rep Pediatr 2011:678724
Yaman A, Kendirli T, Odek C, Azapağası E, Erkol H, Pişkin İE, Teber-Tıraş S, Yalçınkaya F (2016) Severe theophylline poisoning treated with continuous venovenous hemodialysis in a child. Turk J Pediatr 58(3):297–300
Soylemezoglu O, Bakkaloglu A, Yigit S, Saatci U (1993) Haemodialysis treatment in phenobarbital intoxication in infancy. Int Urol Nephrol 25(1):111–113
Kihtir HS, Yildirim HM, Yesilbas O, Duramaz BB, Sevketoglu E (2016) Single-pass albumin dialysis in a child aged six months with phenobarbital poisoning. Turk Pediatri Ars 51(4):228–230
Lacher M, Hermanns-Clausen M, Haeffner K, Brandis M, Pohl M (2005) Severe metformin intoxication with lactic acidosis in an adolescent. Eur J Pediatr 164(6):362–365
Soyoral YU, Begenik H, Emre H, Aytemiz E, Ozturk M, Erkoc R (2011) Dialysis therapy for lactic acidosis caused by metformin intoxication: presentation of two cases. Hum Exp Toxicol 30(12):1995–1997
Harvey B, Hickman C, Hinson G, Ralph T, Mayer A (2005) Severe lactic acidosis complicating metformin overdose successfully treated with high-volume venovenous hemofiltration and aggressive alkalinization. Pediatr Crit Care Med 6(5):598–601
Yildiz TS, Toprak DG, Arisoy ES, Solak M, Toker K (2006) Continuous venovenous hemodiafiltration to treat controlled-release carbamazepine overdose in a pediatric patient. Paediatr Anaesth 16(11):1176–1178
Askenazi DJ, Goldstein SL, Chang IF, Elenberg E, Feig DI (2004) Management of a severe carbamazepine overdose using albumin-enhanced continuous venovenous hemodialysis. Pediatrics 113(2):406–409
Duzova A, Baskin E, Usta Y, Ozen S (2001) Carbamazepine poisoning: treatment with plasma exchange. Hum Exp Toxicol 20(4):175–177
Chan WK, Hui WF (2016) Sequential use of hemoperfusion and single-pass albumin dialysis can safely reverse methotrexate nephrotoxicity. Pediatr Nephrol 31(10):1699–1703
Saland J, Leavey PJ, Bash RO et al (2002) Effective removal of methotrexate by high-flux hemodialysis. Pediatr Nephrol 17:825
Nemoto T, Imai C, Kaneko U et al (2009) Effect of charcoal hemoperfusion for removal of plasma methotrexate in a patient with acute renal failure. Pediatr Hematol Oncol 26(7):520–525
Cecyn KZ, Lee J, Oguro T, Petrilli AS, Bordin JO (2003) Use of plasma exchange in methotrexate removal in a patient with osteosarcoma and acute renal insufficiency. Am J Hematol 72(3):209–211
Singh S (2015) Tandem plasmapheresis with hemodialysis in phenytoin intoxication: a case report. Int J Adv Med 2(3):269–271
Kumar PP, Lingappa L, Shah MA, Shaikh FA (2012) Charcoal hemoperfusion 150 for phenytoin intoxication. Indian Pediatr 49(2):152–153
Ghannoum M, Kazim S, Grunbaum AM, Villeneuve E, Gosselin S (2016) Massive acetaminophen overdose: effect of hemodialysis on acetaminophen and acetylcysteine kinetics. Clin Toxicol (Phila) 54(6):519–522
Muniandy RK, Sinnathamby V (2012) Salicylate toxicity from ingestion of traditional massage oil. BMJ Case Rep. https://doi.org/10.1136/bcr-2012-006562
Papacostas MF, Hoge M, Baum M, Davila SZ (2016) Use of continuous renal replacement therapy in salicylate toxicity: a case report and review of the literature. Heart Lung 45(5):460–463
Tsai MF, Chen CY (2008) Valproate-induced hyperammonemic encephalopathy treated by hemodialysis. Ren Fail 30(8):822–824
Dharnidharka VR, Fennell RS, Richard GA (2002) Extracorporeal removal of toxic valproic acid levels in children. Pediatr Nephrol 17(5):312–315
Schurman SJ, Keeler V, Welch TR (2009) Massive gentamicin overdose in a 14-month-old. Pediatr Nephrol 24(1):211–213
Fuquay D, Koup J, Smith AL (1981) Management of neonatal gentamicin overdosage. J Pediatr 99(3):473–476
Hirsch DJ, Jindal KK, Wong P, Fraser AD (2001) A simple method to estimate the required dialysis time for cases of alcohol poisoning. Kidney Int 60(5):2021–2024
Kraut JA, Mullins ME (2018) Toxic alcohols. N Engl J Med 378(3):270–280
Roberts DM, Yates C, Megarbane B et al (2015) Recommendations for the role of extracorporeal treatments in the management of acute methanol poisoning: a systematic review and consensus statement. Crit Care Med 43(2):461–472
Ronco C, Bellomo R, Kellum JA, Ricci Z (2019) Critical care nephrology, 3rd edn. Elsevier
Wiley JF (1999) Novel therapies for ethylene glycol intoxication. Curr Opin Pediatr 11(3):269–273
Kraut JA, Kurtz I (2008) Toxic alcohol ingestions: clinical features, diagnosis, and management. Clin J Am Soc Nephrol 3(1):208–225
Porter WH, Rutter PW, Bush BA, Pappas AA, Dunnington JE (2001) Ethylene glycol toxicity: the role of serum glycolic acid in hemodialysis. J Toxicol Clin Toxicol 39(6):607–615
Hewlett TP, McMartin KE, Lauro AJ, Ragan FA Jr (1986) Ethylene glycol poisoning. The value of glycolic acid determinations for diagnosis and treatment. J Toxicol Clin Toxicol 24(5):389–402
Shannon MW, Borron SW, Burns MJMD, Haddad LM, Winchester JF (2007) Haddad and Winchester’s clinical management of poisoning and drug overdose, 4th edn. Saunders Elsevier, Philadelphia, London
Conklin L, Sejvar JJ, Kieszak S, Sabogal R, Sanchez C, Flanders D, Tulloch F, Victoria G, Rodriguez G, Sosa N, McGeehin MA, Schier JG (2014) Long-term renal and neurologic outcomes among survivors of diethylene glycol poisoning. JAMA Intern Med 174(6):912–917. https://doi.org/10.1001/jamainternmed.2014.344
Litovitz T (1986) The alcohols: ethanol, methanol, isopropanol, ethylene glycol. Pediatr Clin N Am 33(2):311–323
Zakharov S, Pelclova D, Diblik P, Urban P, Kuthan P, Nurieva O, Kotikova K, Navratil T, Komarc M, Belacek J, Seidl Z, Vaneckova M, Hubacek JA, Bezdicek O, Klempir J, Yurchenko M, Ruzicka E, Miovsky M, Janikova B, Hovda KE (2015) Long term visual damage after acute methanol poisonings: longitudinal cross-sectional study in 50 patients. Clin Toxicol (Phila) 53(9):884–892. https://doi.org/10.3109/15563650.2015.1086488
Peterová K, Brožová H, Klempíř J, Lišková I, Bezdicek O, Ridzoň P, Vaněčková M, Zakharov S, Pelclová D, Miovský M, Růžička E (2018) Gait and balance impairment after acute methanol poisoning. Basic Clin Pharmacol Toxicol 122(1):176–182. https://doi.org/10.1111/bcpt.12853
Slaughter RJ, Mason RW, Beasley DM, Vale JA, Schep LJ (2014) Isopropanol poisoning. Clin Toxicol (Phila) 52(5):470–478
Church AS, Witting MD (1997) Laboratory testing in ethanol, methanol, ethylene glycol, and isopropanol toxicities. J Emerg Med 15(5):687–692
Rietjens SJ, de Lange DW, Meulenbelt J (2014) Ethylene glycol or methanol intoxication: which antidote should be used, fomepizole or ethanol? Neth J Med 72(2):73–79
Barceloux DG, Bond GR, Krenzelok EP, Cooper H, Vale JA (2002) American Academy of Clinical Toxicology practice guidelines on the treatment of methanol poisoning. J Toxicol Clin Toxicol 40(4):415–446
Baird-Gunning J, Lea-Henry T, Hoegberg LCG, Gosselin S, Roberts DM (2017) Lithium poisoning. J Intensive Care Med 32(4):249–263
Rosen MS (2017) Lithium in child and adolescent bipolar disorder. Am J Psychiatry Residents J. https://doi.org/10.1176/appi.ajp-rj.2017.120202
Bruns AS, Sebestyen J (2015) Twelve-year-old female with nausea, vomiting, edema, tremor, and slurred speech. Clin Pediatr (Phila) 54(2):194–196
McLean MM, Sherwin H, Madabhushi V, Tilney PV (2015) A 17-year-old female patient with a lithium overdose. Air Med J 34(4):162–165
Alsady M, Baumgarten R, Deen PM, de Groot T (2016) Lithium in the kidney: friend and foe? J Am Soc Nephrol 27(6):1587–1595. https://doi.org/10.1681/ASN.2015080907
Adityanjee, Munshi KR, Thampy A (2005) The syndrome of irreversible lithium-effectuated neurotoxicity. Clin Neuropharmacol 28(1):38–49
Anani S, Goldhaber G, Wasserstrum Y, Dagan A, Segal G (2018) The “62 SILENT alarm”: when history taking reveals a potentially fatal toxicity. Eur J Case Rep Intern Med 5(6):000843. https://doi.org/10.12890/2018_000843
Decker BS, Goldfarb DS, Dargan PI et al (2015) Extracorporeal treatment for lithium poisoning: systematic review and recommendations from the EXTRIP workgroup. Clin J Am Soc Nephrol 10(5):875–887
Schmidt JJ, Lorenzen J, Chatzikyrkou C, Lichtinghagen R, Kielstein JT (2014) Total collected dialysate lithium concentration after successful dialysis treatment in case of intoxication. BMC Pharmacol Toxicol 15:49
Haussmann R, Bauer M, von Bonin S, Grof P, Lewitzka U (2015) Treatment of lithium intoxication: facing the need for evidence. Int J Bipolar Disord 3:23. https://doi.org/10.1186/s40345-015-0040-2
McKamy S, Hernandez E, Jahng M, Moriwaki T, Deveikis A, Le J (2011) Incidence and risk factors influencing the development of vancomycin nephrotoxicity in children. J Pediatr 158(3):422–426
Rybak MJ (2006) The pharmacokinetic and pharmacodynamic properties of vancomycin. Clin Infect Dis 42(S1):S35–S39
Vancomycin injections US prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/060180s047lbl.pdf Accessed on 20 February 2019
Bunchman TE, Valentini RP, Gardner J, Mottes T, Kudelka T, Maxvold NJ (1999) Treatment of vancomycin overdose using high-efficiency dialysis membranes. Pediatr Nephrol 13(9):773–774
Lemaire M, Connolly B, Harvey E, Licht C (2010) Treatment of paediatric vancomycin intoxication: a case report and review of the literature. NDT Plus 3(3):260–264
Bronstein AC, Spyker DA, Cantilena LR, Green J, Rumack BH, Heard SE (2007) 2006 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS). Clin Toxicol (Phila) 45(8):815–917
Ma YJ, Jiang DQ, Meng JX et al (2016) Theophylline: a review of population pharmacokinetic analyses. J Clin Pharm Ther 41(6):594–601
Ghannoum M, Wiegand TJ, Liu KD et al (2015) Extracorporeal treatment for 92 theophylline poisoning: systematic review and recommendations from the EXTRIP workgroup. Clin Toxicol (Phila) 53(4):215–229
Theophylline in dextrose injections USPI. https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/019211s042lbl.pdf accessed 19 February 2019.
Laussen P, Shann F, Butt W, Tibballs J (1991) Use of plasmapheresis in acute theophylline toxicity. Crit Care Med 19:288–290
Mactier R, Laliberte M, Mardini J, Ghannoum M, Lavergne V, Gosselin S, Hoffman RS, Nolin TD; EXTRIP Workgroup (2014) Extracorporeal treatment for barbiturate poisoning: recommendations from the EXTRIP workgroup. Am J Kidney Dis 64(3):347–358
Mihic S, Harris R (2011) Hypnotics and sedatives. In: Brunton LL, Chabner BA, Knollmann BC (eds) Goodman & Gilman’s the pharmacological basis of therapeutics, 12th edn. McGraw-Hill, New York, pp 457–480
Hoyland K, Hoy M, Austin R et al (2013) Successful use of haemodialysis to treat phenobarbital overdose. BMJ Case Rep 21;2013:cr2013010011. https://doi.org/10.1136/bcr-2013-010011
Metformin tablet US prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/020357s037s039,021202s021s023lbl.pdf Accessed 20 February 2019
Calello DP, Liu KD, Wiegand TJ Roberts DM, Lavergne V, Gosselin S, Hoffman RS, Nolin TD, Ghannoum M; Extracorporeal Treatments in Poisoning Workgroup (2015) Extracorporeal treatment for metformin poisoning: systematic review and recommendations from the extracorporeal treatments in poisoning workgroup. Crit Care Med 43(8):1716–1730
Luft D, Deichsel G, Schmülling RM et al (1983) Definition of clinically relevant lactic acidosis in patients with internal diseases. Am J Clin Pathol 80:484–489
Mirrakhimov AE, Barbaryan A, Gray A, Ayach T (2016) The role of renal replacement therapy in the management of pharmacologic poisonings. Int J Nephrol. https://doi.org/10.1155/2016/3047329
Regolisti G et al (2017) Treatment of metformin intoxication complicated by lactic acidosis and acute kidney injury: the role of prolonged intermittent hemodialysis. Am J Kidney Dis Aug 70(2):290–296
Leonaviciute D, Madsen B, Schmedes A, Buus NH, Rasmussen BS (2018) Severe metformin poisoning successfully treated with simultaneous venovenous hemofiltration and prolonged intermittent hemodialysis. Case Reps Crit Care. https://doi.org/10.1155/2018/3868051
Carbamazepine US prescribing information. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=7a1e523a-b377-43dc-b231-7591c4c888ea. Accessed 21 February 2019.
Goldfrank LR, Flomenbaum N (2006) Goldfrank’s toxicologic emergencies, 8th edn. McGraw-Hill Medical Pub. Division, New York
Ozhasenekler A, Gokhan Ş, Guloglu C, Orak M, Ustundag M (2012) Benefit of hemodialysis in carbamazepine intoxications with neurological complications. Eur Rev Med Pharmacol Sci 16(Suppl 1):43–47
Ghannoum M, Yates C, Galvao TF, Sowinski KM, Vo TH, Coogan A, Gosselin S, Lavergne V, Nolin TD, Hoffman RS, EXTRIP workgroup (2014) Extracorporeal treatment for carbamazepine poisoning: systematic review and recommendations from the EXTRIP workgroup. Clin Toxicol (Phila) 52(10):993–1004
Howard SC, McCormick J, Pui CH, Buddington RK, Harvey RD (2016) Preventing and managing toxicities of high-dose methotrexate. Oncologist 21(12):1471–1482
Methotrexate US prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/008085s066lbl.pdf. Accessed 23 February 2019
Widemann BC, Balis FM, Murphy RF et al (1997) Carboxypeptidase-G2, thymidine, and leucovorin rescue in cancer patients with methotrexate-induced renal dysfunction. J Clin Oncol 15(5):2125–2134
Anseeuw K, Mowry JB, Burdmann EA et al (2016) Extracorporeal treatment in phenytoin poisoning: systematic review and recommendations from the EXTRIP (Extracorporeal Treatments in Poisoning) workgroup. Am J Kidney Dis 67(2):187–197
Olyaei AJ, Bennett WM (2008) Drug dosage in renal failure. In: De Broe ME, Porter GA (eds) Clinical nephrotoxins, renal injury from drugs and chemicals, 3rd edn. Springer, US
Acetaminophen US prescribing information https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/204767s000lbl.pdf Accessed 26 February 2019.
Ogilvie JD, Rieder MJ, Lim R (2012) Acetaminophen overdose in children. CMAJ 184(13):1492–1496
Marzullo L (2005) An update of N-acetylcysteine treatment for acute acetaminophen toxicity in children. Curr Opin Pediatr 17(2):239–245
Gosselin S, Juurlink DN, Kielstein J et al (2014) Extracorporeal treatment for acetaminophen poisoning: recommendations from the EXTRIP workgroup. Clin Toxicol 52(8):856–867
Aspirin US prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/200671s000lbl.pdf Accessed on 28 February 2019
Dargan PI, Wallace CI, Jones AL (2002) An evidence-based flowchart to guide the management of acute salicylate (aspirin) overdose. Emerg Med J 19(3):206–209
Juurlink DN, Gosselin S, Kielstein JT, Ghannoum M, Lavergne V, Nolin TD, Hoffman RS, EXTRIP Workgroup (2015) Extracorporeal treatment for salicylate poisoning: systematic review and recommendations from the EXTRIP workgroup. Ann Emerg Med 266(2):165–181
Ghannoum M, Laliberte M, Nolin TD et al (2015) Extracorporeal treatment for valproic acid poisoning: systematic review and recommendations from the EXTRIP workgroup. Clin Toxicol (Phila) 53(5):454–465
Thanacoody RH (2009) Extracorporeal elimination in acute valproic acid poisoning. Clin Toxicol (Phila) 47(7):609–616
Knorr M, Schaper J, Harjes M, Mayatepek E, Rosenbaum T (2004) Fanconi syndrome caused by antiepileptic therapy with valproic acid. Epilepsia 45(7):868–871
Hanley P, Cunningham RJ, Lou L, Vog B, Raina R (2015) Muscle weakness and pain with profound hypophosphatemia: mystery revealed. Clin Pediatr (Phila) 54(10):1012–1013. https://doi.org/10.1177/0009922815590225
Hicks LK, McFarlane PA (2001) Valproic acid overdose and haemodialysis. Nephrol Dial Transplant 16(7):1483–1486
Singh J, Burr B, Stringham D, Arrieta A (2001) Commonly used antibacterial and antifungal agents for hospitalised paediatric patients: implications for therapy with an emphasis on clinical pharmacokinetics. Paediatr Drugs 3(10):733–761
Acknowledgments
The authors would like to thank Stephanie Lam for her contribution in reviewing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Both Rupesh Raina and Manpreet K Grewal are first authors.
Appendices
Search strategy
Total = 1752 (Ovid Medline = 475, Ovid Embase = 1240, Cochrane CENTRAL = 37) Duplicates removed = 246 Total citations for review = 1506 | |
Database: Ovid MEDLINE(R) Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily, Ovid MEDLINE and Versions(R) Search strategy: 1 renal replacement therapy/ or exp renal dialysis/ 2 (kidney or renal) adj3 replacement adj3 therap*).mp. 3 (haemofiltrat* or haemodialys* or dialysis or “peritoneal dialysis” or capd or haemodiafiltrat* or haemoperfus*).mp. 4 1 or 2 or 3 5 ethylene glycol/ or methanol/ 6 2-propanol/ 7 ethanol/ 8 lithium/ 9 vancomycin/ 10 theophylline/ 11 methotrexate/ 12 exp metformin/ 13 acetaminophen/ 14 carbamazepine/ 15 phenytoin/ 16 exp salicylates/ 17 thallium/ 18 valproic acid/ 19 exp barbiturates/ 20 (“methyl alcohol” or ethanol or “ethyl alcohol” or lithium or vancomycin).mp. 21 (theophylline or methotrexate or metformin or acetaminophen or carbamazepine or phenytoin).mp. 22 (salicylate* or thallium or “valproic acid” or barbiturate* or barbital or pentobarbital or phenobarbital).mp. 23 (“ethylene glycol” or “isopropyl alcohol” or isopropanol or methanol).mp. 24 4 and (or/5-23) 25 24 and (intoxicat* or poison* or toxic* or overdos*).mp. 26 24 and drug overdose/ 27 24 and (complicat* or adverse or nephrotoxic* or “kidney injury” or “renal injury”).mp. 28 25 or 26 or 27 29 limit 28 to “all child (0 to 18 years)” 30 28 and (neonat* or newborn* or infan* or child* or adolescen*).mp,jw. 31 28 and (pediatr* or paediatr*).mp,jw. 32 29 or 30 or 31 Database: Embase Search strategy: 1 exp renal replacement therapy/ 2 ((kidney or renal) adj3 replacement adj3 therap*).mp. 3 (h?emofiltrat* or h?emodialys* or dialysis or “peritoneal dialysis” or capd or h?emodiafiltrat* or h?emoperfus*).mp. 4 1 or 2 or 3 5 ethylene glycol/ 6 methanol/ 7 2 propanol/ 8 alcohol/ 9 lithium/ 10 vancomycin/ 11 theophylline/ 12 methotrexate/ 13 metformin/ 14 paracetamol/ 15 carbamazepine/ 16 phenytoin/ 17 exp salicylic acid derivative/ 18 thallium/ 19 valproic acid/ 20 exp barbituric acid derivative/ 21 (“methyl alcohol” or ethanol or “ethyl alcohol” or lithium or vancomycin).mp. 22 (theophylline or methotrexate or metformin or acetaminophen or carbamazepine or phenytoin).mp. 23 (salicylate* or thallium or “valproic acid” or barbiturate* or barbital or pentobarbital or phenobarbital).mp. 24 (“ethylene glycol” or “isopropyl alcohol” or isopropanol or methanol or paracetamol).mp. 25 4 and (or/5-24) 26 25 and (intoxicat* or poison* or toxic* or overdos*).mp. 27 25 and (intoxication/ or drug intoxication/ or drug overdose/) 28 25 and (complicat* or adverse or nephrotoxic* or “kidney injury” or “renal injury”).mp. 29 26 or 27 or 28 30 limit 29 to (embryo <first trimester> or infant <to one year> or child <unspecified age> or preschool child <1 to 6 years> or school child <7 to 12 years> or adolescent <13 to 17 years>) 31 29 and (neonat* or newborn* or infan* or child* or adolescen*).mp,jw. 32 29 and (pediatr* or paediatr*).mp. 33 30 or 31 or 32 34 limit 33 to Embase Cochrane CENTRAL through Wiley Online Library Search strategy: #1 [mh ^“renal replacement therapy”] or [mh “renal dialysis”] #2 (kidney or renal) near/3 replacement near/3 therap* #3 hemofiltrat* or haemofiltrat* or hemodialys* or haemodialys* or dialysis or “peritoneal dialysis” or capd or hemodiafiltrat* or haemodiafiltrat* or hemoperfus* or haemoperfus* #4 #1 or #2 or #3 #5 [mh “ethylene glycol”] or [mh methanol] #6 [mh 2-propanol] #7 [mh ethanol] or [mh lithium] or [mh vancomycin] or [mh theophylline] #8 [mh methotrexate] or [mh metformin] or [mh acetaminophen] or [mh carbamazepine] #9 [mh phenytoin] or [mh salicylates] or [mh thallium] or [mh “valproic acid”] or [mh barbiturat #10 “methyl alcohol” or ethanol or “ethyl alcohol” or lithium or vancomycin #11 theophylline or methotrexate or metformin or acetaminophen or carbamazepine or phenytoin #12 salicylate* or thallium or “valproic acid” or barbiturate* or barbital or pentobarbital or phenobarbital #13 “ethylene glycol” or “isopropyl alcohol” or isopropanol or methanol #14 #4 and (#5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13) #15 #14 and (neonat* or newborn* or infan* or child* or adolescen* or pediatr* or paediatr*) in Trials |
Represented professional societies in consensus conference
Acute Dialysis Quality Initiative http://www.adqi.net American Nephrology Nurses Association http://anna.inurse.com American Society of Nephrology http://www.asn-online.org American Society of Pediatric Nephrology http://www.aspneph.com British Association for Paediatric Nephrology http://www.bapn.org Continuous Renal Replacement Therapies http://www.crrtonline.com Hemolytic Uremic Syndrome (HUS) http://www.hus-online.at International Pediatric Nephrology Association http://www.ipna-online.org Pediatric Critical Care Medicine http://pedsccm.wustl.edu PedsCCM: Pediatric Critical Care Nursing http://pedsccm.wustl.edu/NURSING/APN_info.html RenalWEB http://www.renalweb.com Toxicologists and Pharmacists from Akron Children’s Hospital, Akron, Ohio, USA Dr. Martha Blackford PharmD, BCPS Clinical Pharmacologist & Toxicologist Akron Children’s Hospital, Akron, Ohio, USA Dr. Michelle Bestic PharmD, BCPS Clinical Pharmacologist & Toxicologist Akron Children’s Hospital, Akron, Ohio, USA Literature search support Ms. Marian Simonson Assistant Director Floyd D Loop Alumni Library Cleveland Clinic 9500 Euclid Ave., NA30, Cleveland, Ohio, USA Ms.Clare Leibfarth, M.L.S.Coordinator, Library Services Cleveland Clinic Akron General Akron, Ohio, USA Ms. Denise Mullins, M.L.I.S.Library Operations Assistant Cleveland Clinic Akron General Akron, Ohio, USA |
Rights and permissions
About this article
Cite this article
Raina, R., Grewal, M.K., Blackford, M. et al. Renal replacement therapy in the management of intoxications in children: recommendations from the Pediatric Continuous Renal Replacement Therapy (PCRRT) workgroup. Pediatr Nephrol 34, 2427–2448 (2019). https://doi.org/10.1007/s00467-019-04319-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-019-04319-2