Abstract
Background
Solitary functioning kidney (SFK) is an important condition in the spectrum of congenital anomalies of the kidney and urinary tract. The aim of this study was to describe the risk factors for renal injury in a cohort of patients with congenital SFK.
Methods
In this retrospective cohort study, 162 patients with SFK were systematically followed up (median, 8.5 years). The primary endpoint was time until the occurrence of a composite event of renal injury, which includes proteinuria, hypertension, and chronic kidney disease (CKD). A predictive model was developed using Cox proportional hazards model and evaluated by c statistics.
Results
Among 162 children with SFK included in the analysis, 132 (81.5%) presented multicystic dysplastic kidney, 20 (12.3%) renal hypodysplasia, and 10 (6.2%) unilateral renal agenesis. Of 162 patients included in the analysis, 10 (6.2%) presented persistent proteinuria, 11 (6.8%) had hypertension, 9 (5.6%) developed CKD stage ≥ 3, and 18 (11%) developed the composite outcome. After adjustment by the Cox model, three variables remained as independent predictors of the composite event: creatinine (HR, 3.93; P < 0.001), recurrent urinary tract infection (UTI) (HR, 5.05; P = 0.002), and contralateral renal length at admission (HR, 0.974; P = 0.002). The probability of the composite event at 10 years of age was estimated as 3%, 11%, and 56% for patients assigned to the low-risk, medium-risk, and high-risk groups, respectively (P < 0.001).
Conclusion
Our findings have shown an overall low risk of renal injury for most of infants with congenital SFK. Nevertheless, our prediction model enabled the identification of a subgroup of patients with an increased risk of renal injury over time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congenital anomalies of the kidney and urinary tract (CAKUT) are the most common cause of birth defects [1, 2]. In recent years, it has become clear that a solitary functioning kidney (SFK) is an important condition in the spectrum of CAKUT [3]. Longitudinal clinical studies have consistently shown that long-term clinical outcome of these patients is not as good as it thought before. For instance, Sanna-Cherchi et al. [4] reported data on 312 CAKUT patients followed until age 30 years and showed that the risk for dialysis was significantly higher for patients with SFK. Using a systematic review, Westland et al. [5] evaluated the occurrence of hyperfiltration injury in 43 published cohorts of unilateral renal agenesis. Analysis of data on 2684 patients identified hypertension in 16% of the patients, albuminuria in 21%, and reduced glomerular filtration rate (GFR) in 10%.
Regular clinical monitoring of these patients is necessary and requires a multidisciplinary approach [3]. However, since many children with uncomplicated SFK are not regularly followed up, its natural history was not fully established. Consequently, there is also lack of agreement on how best to monitor and how long these children should be followed [6]. Opinion-based recommendations for monitoring have been issued, although consensus is lacking [7,8,9]. Information about the clinical course of SFK and the identification of predictive factors for kidney injury in these patients may contribute to early recognition of patients at risk and to formulation of monitoring strategies. In the present study, we focused our analysis on children with congenital SFK longitudinally followed up in a long-term basis with the aim to evaluate the clinical outcomes and to identify possible risk factors for renal injury.
Patients and methods
Patients
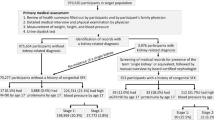
The study group comprised 190 patients with congenital SFK who were prospectively followed at the Pediatric Nephrourology Unit (Belo Horizonte, Brazil) between 1987 and 2015. For this study, the following phenotypes were included: renal agenesis, primary renal hypodysplasia, and multicystic dysplastic kidney (MCDK). For analysis, we stratified the sample into two groups: MCDK and renal agenesis/hypodysplasia. We excluded patients with bilateral severe renal hypodysplasia (n = 8), multiple malformations (n = 1), and those who abandoned postnatal follow-up (n = 19), resulting in a final sample of 162 infants. Among these 162 patients, 155 (96%) had prenatal diagnosis and in 7 (4%) infants, the diagnosis was incidental by findings of abdominal sonography imaging obtained for varied clinical conditions (mainly palpable masses).
The diagnosis criterion for MCDK was ultrasound evidence of a kidney with parenchyma completely substituted by large non-communicating cysts of varying size. The diagnosis criterion for primary renal hypodysplasia was sonography evidence of a small echogenic kidney with size less than two standard deviations below the mean for gender, age, and body size. The sonography criterion for unilateral renal agenesis was an empty lumbar fossa with elongated adrenal gland appearance [10, 11]. All diagnosis was confirmed by the postnatal renal ultrasonography (RUS) and by the absence of kidney function in renal scintigraphy.
Baseline data
After the initial RUS, patients underwent urinary tract imaging workup according to a systematic protocol described elsewhere [12]. The first postnatal RUS was performed at a median time of 17 days of life (IQ range, 9–25 days). All patients underwent a 99m-technetium-dimercaptosuccinic acid isotope scan (DMSA scan) and voiding cystourethrography (VCUG). According to a clinical protocol, baseline data were obtained following strict conditions. Baseline creatinine was obtained during the neonatal period but not in the first 3 days of life to avoid confounding with maternal creatinine. Similarly, the first renal sonography was also obtained during the first month of life but not in the first week of due to the issue of physiologic neonatal dehydration (with possible false-negative results in cases of antenatal hydronephrosis). For the 7 patients with postnatal incidental diagnosis, we recovered the first exams available (all within the first 6 months of life).
Follow-up protocol
After initial evaluation, clinical, laboratory, and imaging assessments were carried out periodically at 6-month intervals, as described elsewhere in detail [12, 13]. In brief, ultrasound scans, clinical examination (including growth and blood pressure measurements), and laboratory reviews were performed at 6-month intervals during the first 2 years after birth and yearly thereafter. Sonograms were performed by the same trained examiner using a standard method [14, 15]. RUS measurements were performed on the maximal longitudinal and transverse kidney sections. The maximal length, width, and anteroposterior dimension (depth) of both kidneys were measured according to Dinkel et al. [16]. The renal volume was calculated according to the formula provided by Han and Babcock [17]. Plasma creatinine concentration was determined at baseline and yearly thereafter. Since creatinine measurements were made by Jaffe method until November 2011 in our institution, GFR was estimated by the conventional Schwartz formula [18] for data obtained until this period. After November 2011, creatinine was measured by IDMS (isotope dilution mass spectrometry) traceable method. Therefore, the modified Schwartz formula [19] was adopted to estimate GFR rather than the conventional Schwartz formula. Blood pressure was measured according to the recommendations of the Working Group of the National High Blood Pressure Education Program [20]. Proteinuria was assessed by the measurement of protein to creatinine ratio in spot urine for infants and by the measurement of protein excretion in 24-h urine samples for older patients. All children with hypertension and/or proteinuria have received ACE inhibitor enalapril in doses tailored according to age and body surface area.
Outcomes
The events of interest were defined as a composite of renal injury events, including eGFR < 60 ml/min per 1.73 m2, hypertension, and proteinuria. The primary endpoint for this study was time until the first occurrence of any of the composite events.
Outcomes and covariables definitions
Chronic kidney disease (CKD) was defined as GFR < 60 ml/min per 1.73 m2 in two consecutive exams with an interval of at least 3 months [21]. Reference values and definitions of normal blood pressure were based on the fourth report on high blood pressure in children and adolescents [22]. As recommend, we used conventional auscultatory method for most children and an oscillometric automatic device for newborns and young infants in whom auscultation is difficult. An elevated blood pressure reading obtained with an oscillometric device was repeated by using auscultation. Proteinuria was considered when urinary protein creatinine ratio is above 0.2 or 24-h protein excretion is > 150 mg/day in at least two consecutive evaluations. Urinary tract infection (UTI) was defined as growth of at least 100,000 cfu/ml of a single microbial agent in urine obtained by bag or from a mid-stream clean-catch urine specimen associated with fever (38.0 °C or more) and/or urinary symptoms. Recurrent UTI was defined as the occurrence of two or more episodes during the follow-up. The percentile of the contralateral renal length was established according to the nomogram proposed by Chen et al. [23], using the tool at the following website: https://www.prevmed.sunysb.edu/jjc/MrNomogram/.
Statistical analysis
The values are expressed as medians and interquartile ranges (IQs) or means and standard deviations when appropriate. The overall incidence rate of UTI was calculated as follows. The total number of new episodes of UTI was identified and divided by the total number of person-months at risk. Then, the rate ratio was calculated by dividing the incidence rate of different groups. These analyses were performed using the public domain site Open Source Epidemiologic Statistics for Public Health (version 3.01) provided in the World Wide Web and developed by Rollins School of Public Health, Emory University. Survival analyses were performed by the Kaplan–Meier method (KM) and Cox proportional hazards model to evaluate time until the occurrence of the composite event. For KM analyses, the optimal cutoff point for continuous variables was determined by the receiver operating characteristic (ROC) curve using the Youden index [24]. Differences between dichotomous variables were assessed by the two-sided log-rank test [25]. The Cox proportional hazards model was applied to identify variables that were independently associated with the occurrence of the event. Variables selected for multivariable analyses were used to build a final model after discarding any violation of proportionality assumptions; proportional hazard assumption was checked graphically by log–log versus time plots for each variable [26, 27]. Possible interactions between variables that remained in the final model were evaluated by including interaction terms in the model. There were 9 missing values concerning the variable proteinuria, mainly in patients who were enrolled in the first years of cohort and were not being followed when we included the annual measurement of proteinuria in our clinical protocol. Missing values for proteinuria were filled in with multiple imputation (MI) procedure. Each missing value was imputed five times. Imputed values were drawn from the predictive distribution in an imputation model that included all candidate predictors and the outcome (time to surgery). MI resulted in five complete datasets, which were analyzed with standard complete data methods. The results were combined to produce overall estimates and standard errors that reflect missing data uncertainty [28].
A prognostic model was then constructed from these data by dividing each β coefficient in the final multivariable model with significant risk factors by the lowest β coefficient. The β coefficients were used for factor weighting; points were assigned to each independent prognostic factor, their coefficients being rounded to the nearest integer [29]. Finally, a prognostic score was calculated for each patient by summing up the points. The prognostic score derived was then grouped into three categories (low-, medium-, and high-risk groups). We assessed the accuracy of the derived model by looking at the components of accuracy (i.e., discrimination and calibration) [29, 30]. Discrimination was evaluated on the basis of 2, 5, and 10 years of follow-up using the c statistic, which represents the area under the receiver operating characteristic curve (for which larger values indicate better discrimination) [31]. Calibration was also assessed graphically by a KM plot for patients in different risk groups (low-risk, medium-risk, and high-risk) [32, 33]. To adjust for overfitting and overoptimistic performance of the model, we performed an internal validation of our model with a bootstrapping technique [31]. In each bootstrap sample, the entire modeling process was repeated, resulting in shrinkage of the regression coefficients when applicable [34]. All reported P values are two sided, and a P value < 0.05 was considered to represent a statistically significant difference for all analyses including interaction terms.
Results
Among 162 children with SFK included in the analysis, 132 (81.5%) presented MCDK, 20 (12.3%) renal hypodysplasia, and 10 (6.2%) unilateral renal agenesis. Baseline clinical characteristics stratified according to phenotype are summarized in Table 1. There was a significant greater proportion of males and a slight higher creatinine at baseline in the hypodysplasia/agenesis group. Forty-three (26.5%) patients presented with contralateral CAKUT, and patients in the hypodysplasia/agenesis group had a significant greater proportion of these abnormalities. Among 43 children with contralateral CAKUT, 14 presented mild hydronephrosis, 12 vesicoureteral reflux, 10 ureteropelvic junction obstruction, 4 renal scarring, and 3 primary megaureter.
Clinical course and outcomes
Median follow-up time was 8.5 years (interquartile range [IQ], 4.1–14.7 years); 104 patients (64.8%) were followed up for more than 5 years and 69 (42.6%) for more than 10 years.
Renal injury events
Of 162 patients included in the analysis, 10 (6.2%) presented persistent mild proteinuria, 11 (6.8%) had hypertension, 9 (5.6%) developed CKD stage III or higher, and 18 (11.1%) exhibited the composite outcome. The cumulative proportions of patients free from proteinuria, hypertension, CKD, and the composite event at 17 years old were 89.2%, 90.8%, 91.1%, and 84.2%, respectively. Table 2 summarizes the clinical outcomes according to the phenotype classification. There was no significant difference in occurrence of renal injury between phenotype groups.
Surgical interventions
Fourteen patients (8.6%) underwent surgical procedures. The most common surgical intervention was pyeloplasty for 7 patients, 4 patients underwent ureteral reimplant, and 2 patients underwent nephrectomy. The median age at surgical intervention was 1.6 months (IQ range, 10 days–26.7 months). As expected, surgical intervention was significantly more frequent in the hypodysplasia/agenesis group due to higher frequency of contralateral CAKUT (Table 2).
Urinary tract infections
During follow-up, information was obtained on 18,413 person-months. UTI occurred in 37 (22.8%) of the 162 and 25 patients (15.4) had a single UTI and only 12 (7.4%) had more than one episode. The overall incidence rate of UTI was 3.8 episodes per 1000 person-months (95% CI, 2.7–4.8). The incidence rate of UTI for patients with contralateral CAKUT was 9.7 episodes per 1000 person-months (95% CI, 7.0–12.7), whereas for patients without contralateral anomalies was 1.9 episodes per 1000 person-months (95% CI, 1.3–2.7) (P < 0.001).
Univariate analysis
Table 3 summarizes the results of the Cox univariate analysis of possible risk factors for renal injury. There was no significant difference in occurrence of renal injury with respect to gender, phenotype, and prematurity. Low birth weight and birth length associated only with the composite event and CKD, respectively. The percentile of contralateral renal length (pCRL) was associated with proteinuria and the composite event. On the other hand, presence of contralateral CAKUT, recurrent UTI, baseline creatinine, and baseline eGFR was strongly associated with most of the renal injury events (Table 3). For instance, Fig. 1a–c illustrates the probability of the composite event according to the presence of contralateral CAKUT (a), recurrent UTI (b), and baseline creatinine (cut-off 0.51 mg/dl) (c).
Kaplan–Meier survival curves reveal probability of the composite event according to the presence of contralateral congenital anomalies of the kidney and urinary tract (CAKUT) (a), occurrence of recurrent urinary tract infection (UTI) (b), and baseline creatinine > 0.51 mg/dl (c). The shaded areas represent the 95% confidence intervals. Number of patients at risk is shown below x-axis
Clinical predictive model
After adjustment by the Cox regression model, three variables remained as independent predictors of the composite event: baseline creatinine, recurrent UTI, and pCRL at admission (Table 4). A prognostic weighting was derived for each variable by dividing each β coefficient by the lowest β. The shrinkage factor obtained from bootstrap results was 0.9403 (Table 4). Finally, a prognostic risk score was calculated as the sum of these weightings for the three variables. A risk score was calculated for each patient by adding up these points. The risk score ranged from 0 to 12.5 points (median 2 points). The accuracy of the score applied to the sample was consistently high through time, with a mean c statistic of 0.850 (95% CI, 0.701–0.993), 0.866 (95% CI, 0.661–0.999), and 0.895 (95% CI, 0.793–0.997) for the follow-up periods of 2, 5, and 10 years, respectively (Fig. 2a–c). Finally, the prognostic risk score was divided into three categories: low risk (≤ 2 points, 96 infants, 59.3%), medium risk (3–5 points, 51, 31.5%), and high risk (> 5 points, 15, 9.3%) for the composite event. The probability of the composite event at 10 years of age was estimated as 3%, 11%, and 56% for patients assigned to the low-risk, medium-risk, and high-risk groups, respectively (P < 0.001) (Fig. 3).
Discussion
In this retrospective cohort study, we evaluated intermediate and long-term clinical outcomes in infants with congenital SFK from a single tertiary center. We found that about 11% of our cohort presented renal injury. After adjustment by multivariate model, renal injury was associated with the presence of CAKUT in the functioning kidney, renal length at birth of the functioning kidney, baseline kidney function, and episodes of UTI. Of particular interest, we developed a clinical predictive model that predicted with good accuracy, the occurrence of renal injury.
The long-term outcome of patients with a SFK has been currently a topic of intense debate [35,36,37]. A number of longitudinal observational studies have been published leading to somewhat conflicting results [9, 38,39,40,41]. These different findings could be attributed to several factors, including selection bias with oversampling of the most severely affected patients, inclusion of heterogeneous phenotypes (congenital and acquired SFK), difference in the length of follow-up time, and also to the diversity of endpoints used for analysis [35,36,37, 42].
In spite of methodological differences, well-designed studies with larger samples have been giving a clearer view of the actual impact of solitary kidney on long-term clinical outcomes [4, 6, 43,44,45]. In this regard, the KIMONO study (KIdney of MONofunctional Origin) was designed to study the development of renal injury in children with different origins of SFK [45]. The authors reported an overall incidence of renal injury, defined as the presence of hypertension and/or albuminuria and/or the use of renoprotective medication, of 32% at a mean age of 9.5 (SD, 5.6) years. On the other hand, recent studies including only congenital SFK have shown a smaller prevalence of renal injury. In a retrospective study, La Scola et al. [6] evaluated 142 children with congenital SFK and demonstrated that a decreased estimated GFR rate was present in 12% of children at a median age of 2.2 years. They reported that survival analysis revealed an estimated event-free survival of 82% (95% CI, 74–91%) at 10 years. Recently, Marzuillo et al. [43] evaluated patients with prenatally diagnosed congenital SFK. Median follow-up time was 7.2 years (range, 1–23), and renal injury was found in 12 of 306 patients (3.9%). By Kaplan–Meier analysis, the cumulative proportion of patients free from renal function impairment at 17 years old was 93.7%. Our findings are in agreement with this recent series based on congenital SFK. Of 162 patients followed-up for a median of 8.5 years, 9 (5.6%) developed renal function impairment and 18 (11.1%) presented the composite outcome. In our survival analysis, the cumulative proportions of patients free from renal impairment and renal injury (composite event) at 17 years old were 91.1% and 84.2%, respectively.
In our study, we also sought for clinical risk factors for the development of renal injury. For this analysis, we decided to include a composite event of well-recognized factors associated with long-term impairment of the renal function, namely proteinuria, hypertension, and CKD stage III or higher [46, 47]. First, we found that there was no significant difference between MCDK and agenesis/hypodysplasia regarding renal injury, despite a greater proportion of contralateral CAKUT in the latter group. In unadjusted analysis, low birth weight, birth length, contralateral CAKUT, recurrent UTI, and baseline renal function were all associated with some of the components of the composite event. After multivariable adjustment, recurrent UTI, higher baseline creatinine levels, contralateral CAKUT, and smaller percentile of contralateral renal length RPT were each independently associated with the composite event. Interestingly, despite methodological differences, two recent studies reported similar risk factors for renal injury. Westland et al. [44] have shown that the development of renal injury increased by presence of ipsilateral CAKUT and renal length was inversely associated with the risk to develop renal injury. La Scola et al. [6] demonstrated that the probability of 10-year survival was significantly lower in children with additional CAKUT (54% vs 88%). Similar also to our findings, a lower estimated primary outcome-free survival could also be observed in children without compensatory hypertrophy of the functioning kidney and in children with a history of febrile UTIs.
Furthermore, our study has proposed the development of a clinical predictive model of progression to a composite event of renal injury. These patients were then classified into low-, medium-, and high-risk groups, with estimated renal injury 10-year free survival of about 97%, 89%, and 44%, respectively. Moreover, the model presented a consistently good accuracy through time. If these findings are confirmed in further studies, this clinical predictive model may allow clinicians to distinguish infants with SFK who may deserve closer follow-up from those with benign features. In addition, an identification of potential modifiable factor, such as recurrent UTI, might allow an intervention in a selected subgroup of SFK patients. In our series, about a quarter of patients had at least 1 episode of UTI and 12 (7.4%) had recurrent more episodes. The incidence of renal injury was about five times greater among patients with recurrent UTI even after adjustment for other covariates. Of particular interest, recurrent UTI was strongly associated with patients with contralateral CAKUT. Therefore, our findings suggest that repeated episodes of UTI seem to be a risk factor for renal injury. Nevertheless, it should be pointed out that the efficacy of prophylactic intervention for these patients requires future studies. The model described in the current study enables clinicians to identify patients with high risk of renal injury which may promote a tailored management and follow-up for these children. For instance, patients with a baseline creatinine higher than 0.58 mg/dl, a reduced contralateral renal length (< 50th percentile), and presence of contralateral CAKUT (higher risk of recurrent UTI) should undergo a long-term follow-up with a strict surveillance of blood pressure, proteinuria, and renal function. Furthermore, in this subgroup of patients with higher risk for recurrent UTI, antibiotic prophylaxis might have a positive impact on the rate of renal injury. On the other hand, for the group of patients without these features, assigned as low-risk group, it may be advisable only a regular follow-up with general pediatrician and maintain a healthy lifestyle in order to avoid comorbidities such obesity and diabetes.
Our study has some limitations, and several clinical and methodologic considerations should be taken into account in evaluating our findings. First, from the clinical point of view, systematic assessment for proteinuria was not uniformly performed across the entire period of study, especially for patients who were enrolled in the first decade. Missing data are a frequent problem in retrospective cohort studies. We have addressed this problem by using multiple imputations that have the advantage of not ignoring observations with incomplete information and, at the same time, reflecting the uncertainty of the imputation process [48]. Nevertheless, this fact has certainly hampered a more robust analysis of the risk factors for renal injury. Another limitation that we must consider is the difficulty in ascertaining the accurate incidence of UTI especially in younger patients. We are aware that the incidence of UTI might have been either overestimated in infants from whom urine was collected by bag or underestimated in patients with less obvious symptoms or when a urine sample was not collected in a timely manner. From the methodological point of view, we have not validated the risk prediction instrument in an independent cohort. External validation is a key component in the development of clinical predictive models because accurate predictions in the patients that were used to develop a model are no guarantee for good predictions in a new set of patients [33, 49]. Alternatively, we internally validated our model with bootstrapping technique, which has been claimed to be the most efficient strategy, to adjust for overfitting and overoptimistic performance of the model [50]. On the other hand, we believe that the most original aspect of our study was the systematic analysis of clinical outcomes in this selected group of infants. The strength of the present study is its evaluation of homogeneous population of infants with SFK enrolled in a single tertiary center, managed with standardized workup and systematically followed up in a long-term basis by the same medical team since birth.
In summary, in this retrospective cohort study, we observed an overall low risk of renal injury for the majority of the infants with congenital SFK. Nevertheless, a subgroup of patients had an increased risk of renal injury over time. Independent risk factors for these outcomes included a lower baseline renal function, presence of contralateral CAKUT, a reduced renal length of the functioning kidney at birth, and recurrent UTIs during follow-up. If confirmed in future studies, infants with SFK and any of these risk factors may benefit from closer surveillance for proteinuria, hypertension, and impaired renal function, during long-term follow-up.
References
Loane M, Dolk H, Kelly A, Teljeur C, Greenlees R, Densem J (2011) Paper 4: EUROCAT statistical monitoring: identification and investigation of ten year trends of congenital anomalies in Europe. Birth Defects Res A Clin Mol Teratol 91(Suppl 1):S31–S43
Wiesel A, Queisser-Luft A, Clementi M, Bianca S, Stoll C (2005) Prenatal detection of congenital renal malformations by fetal ultrasonographic examination: an analysis of 709,030 births in 12 European countries. Eur J Med Genet 48:131–144
Westland R, Schreuder MF, van Goudoever JB, Sanna-Cherchi S, van Wijk JA (2014) Clinical implications of the solitary functioning kidney. Clin J Am Soc Nephrol 9:978–986
Sanna-Cherchi S, Ravani P, Corbani V, Parodi S, Haupt R, Piaggio G, Innocenti ML, Somenzi D, Trivelli A, Caridi G, Izzi C, Scolari F, Mattioli G, Allegri L, Ghiggeri GM (2009) Renal outcome in patients with congenital anomalies of the kidney and urinary tract. Kidney Int 76:528–533
Westland R, Schreuder MF, Ket JC, van Wijk JA (2013) Unilateral renal agenesis: a systematic review on associated anomalies and renal injury. Nephrol Dial Transplant 28:1844–1855
La Scola C, Ammenti A, Puccio G, Lega MV, De Mutiis C, Guiducci C, De Petris L, Perretta R, Venturoli V, Vergine G, Zucchini A, Montini G (2016) Congenital solitary kidney in children: size matters. J Urol 196:1250–1256
Corbani V, Ghiggeri GM, Sanna-Cherchi S (2011) Congenital solitary functioning kidneys: which ones warrant follow-up into adult life? Nephrol Dial Transplant 26:1458–1460
Hayes WN, Watson AR, Trent AMSG (2012) Unilateral multicystic dysplastic kidney: does initial size matter? Pediatr Nephrol 27:1335–1340
Vu KH, Van Dyck M, Daniels H, Proesmans W (2008) Renal outcome of children with one functioning kidney from birth. A study of 99 patients and a review of the literature. Eur J Pediatr 167:885–890
Avni EF, Thoua Y, Lalmand B, Didier F, Droulle P, Schulman CC (1986) Multicystic dysplastic kidney: evolving concepts. In utero diagnosis and post-natal follow-up by ultrasound. Ann Radiol 29:663–668
Avni EF, Thoua Y, Van Gansbeke D, Matos C, Didier F, Droulez P, Schulman CC (1987) Development of the hypodysplastic kidney: contribution of antenatal US diagnosis. Radiology 164:123–125
Rabelo EA, Oliveira EA, Diniz JS, Silva JM, Filgueiras MT, Pezzuti IL, Tatsuo ES (2004) Natural history of multicystic kidney conservatively managed: a prospective study. Pediatr Nephrol 19:1102–1107
Rabelo EA, Oliveira EA, Silva JM, Bouzada MC, Sousa BC, Almeida MN, Tatsuo ES (2005) Conservative management of multicystic dysplastic kidney: clinical course and ultrasound outcome. J Pediatr 81:400–404
Rabelo EA, Oliveira EA, Silva GS, Pezzuti IL, Tatsuo ES (2005) Predictive factors of ultrasonographic involution of prenatally detected multicystic dysplastic kidney. BJU Int 95:868–871
Siqueira Rabelo EA, Oliveira EA, Silva JM, Oliveira DS, Colosimo EA (2006) Ultrasound progression of prenatally detected multicystic dysplastic kidney. Urology 68:1098–1102
Dinkel E, Ertel M, Dittrich M, Peters H, Berres M, Schulte-Wissermann H (1985) Kidney size in childhood. Sonographical growth charts for kidney length and volume. Pediatr Radiol 15:38–43
Han BK, Babcock DSV (1985) Sonographic measurements and appearance of normal kidneys in children. Am J Roentgenol 145:611–616
Schwartz GJ, Brion LP, Spitzer A (1987) The use of plasma creatinine concentration for estimating glomerular filtration rate in infants, children, and adolescents. Pediatr Clin N Am 34:571–590
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Anonymous (1996) Update on the 1987 task force report on high blood pressure in children and adolescents: a working group report from the National High Blood Pressure Education Program. Pediatrics 98:649–657
Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, Hogg RJ, Perrone RD, Lau J, Eknoyan G (2003) National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med 139:137–147
Anonymous (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114:555–576
Chen JJ, Zhi J, Mao W, Steinhardt GF (2006) MrNomogram: a web-based multivariable pediatric renal nomogram. J Pediatr Urol 2:436–438
Youden WJ (1950) Index for rating diagnostic tests. Cancer 3:32–35
Jager KJ, van Dijk PC, Zoccali C, Dekker FW (2008) The analysis of survival data: the Kaplan-Meier method. Kidney Int 74:560–565
Ravani P, Parfrey P, Gadag V, Malberti F, Barrett B (2007) Clinical research of kidney diseases III: principles of regression and modelling. Nephrol Dial Transplant 22:3422–3430
van Dijk PC, Jager KJ, Zwinderman AH, Zoccali C, Dekker FW (2008) The analysis of survival data in nephrology: basic concepts and methods of Cox regression. Kidney Int 74:705–709
Rubin DB, Schenker N (1991) Multiple imputation in health-care databases: an overview and some applications. Stat Med 10:585–598
Sullivan LM, Massaro JM, D'Agostino RB Sr (2004) Presentation of multivariate data for clinical use: the Framingham study risk score functions. Stat Med 23:1631–1660
Moons KG, Kengne AP, Grobbee DE, Royston P, Vergouwe Y, Altman DG, Woodward M (2012) Risk prediction models: II. External validation, model updating, and impact assessment. Heart 98:691–698
Harrell FE Jr, Lee KL, Mark DB (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15:361–387
Cook NR, Buring JE, Ridker PM (2006) The effect of including C-reactive protein in cardiovascular risk prediction models for women. Ann Intern Med 145:21–29
Steyerberg EW, Vickers AJ, Cook NR, Gerds T, Gonen M, Obuchowski N, Pencina MJ, Kattan MW (2010) Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology 21:128–138
Moons KG, Kengne AP, Woodward M, Royston P, Vergouwe Y, Altman DG, Grobbee DE (2012) Risk prediction models: I. development, internal validation, and assessing the incremental value of a new (bio)marker. Heart 98:683–690
Marzuillo P, Polito C (2018) Congenital solitary kidney in childhood: not so bad. Pediatr Nephrol 33:723–724
Schreuder MF (2018) Life with one kidney: response to comments by Marzuillo and Polito. Pediatr Nephrol 33:725–726
Schreuder MF (2018) Life with one kidney. Pediatr Nephrol 33:595–604
Abou Jaoude P, Dubourg L, Bacchetta J, Berthiller J, Ranchin B, Cochat P (2011) Congenital versus acquired solitary kidney: is the difference relevant? Nephrol Dial Transplant 26:2188–2194
Schreuder MF, Langemeijer ME, Bokenkamp A, Delemarre-Van de Waal HA, Van Wijk JA (2008) Hypertension and microalbuminuria in children with congenital solitary kidneys. J Paediatr Child Health 44:363–368
Seeman T, Patzer L, John U, Dusek J, Vondrak K, Janda J, Misselwitz J (2006) Blood pressure, renal function, and proteinuria in children with unilateral renal agenesis. Kidney Blood Press Res 29:210–215
Siomou E, Giapros V, Papadopoulou F, Pavlou M, Fotopoulos A, Siamopoulou A (2014) Growth and function in childhood of a normal solitary kidney from birth or from early infancy. Pediatr Nephrol 29:249–256
Westland R, Schreuder MF, van der Lof DF, Vermeulen A, Dekker-van der Meer IM, Bokenkamp A, van Wijk JA (2014) Ambulatory blood pressure monitoring is recommended in the clinical management of children with a solitary functioning kidney. Pediatr Nephrol 29:2205–2211
Marzuillo P, Guarino S, Grandone A, Di Somma A, Della Vecchia N, Esposito T, Macchini G, Marotta R, Apicella A, Diplomatico M, Rambaldi PF, Perrone L, Miraglia Del Giudice E, La Manna A, Polito C (2017) Outcomes of a cohort of prenatally diagnosed and early enrolled patients with congenital solitary functioning kidney. J Urol 198:1153–1158
Westland R, Kurvers RA, van Wijk JA, Schreuder MF (2013) Risk factors for renal injury in children with a solitary functioning kidney. Pediatrics 131:e478–e485
Westland R, Schreuder MF, Bokenkamp A, Spreeuwenberg MD, van Wijk JA (2011) Renal injury in children with a solitary functioning kidney--the KIMONO study. Nephrol Dial Transplant 26:1533–1541
Cerqueira DC, Soares CM, Silva VR, Magalhaes JO, Barcelos IP, Duarte MG, Pinheiro SV, Colosimo EA, Simoes e Silva AC, Oliveira EA (2014) A predictive model of progression of CKD to ESRD in a predialysis pediatric interdisciplinary program. Clin J Am Soc Nephrol 9:728–735
Ishikura K, Uemura O, Hamasaki Y, Ito S, Wada N, Hattori M, Ohashi Y, Tanaka R, Nakanishi K, Kaneko T, Honda M, Pediatric CKDSGiJ, Committee of Measures for Pediatric CKDoJSoPN (2014) Progression to end-stage kidney disease in Japanese children with chronic kidney disease: results of a nationwide prospective cohort study. Nephrol Dial Transplant 29:878–884
Larkins NG, Craig JC, Teixeira-Pinto A (2018) A guide to missing data for the pediatric nephrologist. Pediatr Nephrol. https://doi.org/10.1007/s00467-018-3932-4
Toll DB, Janssen KJ, Vergouwe Y, Moons KG (2008) Validation, updating and impact of clinical prediction rules: a review. J Clin Epidemiol 61:1085–1094
Steyerberg EW, Harrell FE Jr, Borsboom GJ, Eijkemans MJ, Vergouwe Y, Habbema JD (2001) Internal validation of predictive models: efficiency of some procedures for logistic regression analysis. J Clin Epidemiol 54:774–781
Funding
R.H.M. is supported by NIH grants U01 DK-03012 and R24HD050837. E.A.O. is supported by CAPES grant 2746-15-8. This study was partially supported by CNPq (Brazilian National Research Council, Grant 481649/2013-1), FAPEMIG (Fundação de Amparo à Pesquisa do Estado de Minas Gerais, Grant PPM-00228-15), and the INCT-MM Grant (FAPEMIG: CBBAPQ-00075-09/CNPq 573646/2008-2).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The Ethics Committee of the Federal University of Minas Gerais approved the study, and the parents or individuals responsible for the children gave written informed consent to participate.
Conflicts of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Poggiali, I.V., Simões e Silva, A.C., Vasconcelos, M.A. et al. A clinical predictive model of renal injury in children with congenital solitary functioning kidney. Pediatr Nephrol 34, 465–474 (2019). https://doi.org/10.1007/s00467-018-4111-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-018-4111-3