Abstract
Background
Acute kidney injury (AKI) and infection are common complications after pediatric cardiac surgery. No pediatric study has evaluated for an association between postoperative AKI and infection. The objective of this study was to determine if AKI in neonates after cardiopulmonary bypass was associated with the development of a postoperative infection.
Methods
We performed a single center retrospective chart review from January 2009 to December 2015 of neonates (age ≤ 30 days) undergoing the Norwood procedure. AKI was defined by the modified neonatal Kidney Disease Improving Global outcomes serum creatinine criteria using (1) measured serum creatinine and (2) creatinine corrected for fluid balance on postoperative days 1–4. Infection, (culture positive or presumed), must have occurred after a diagnosis of AKI and within 60 days of surgery.
Results
Ninety-five patients were included, of which postoperative infection occurred in 42 (44%). AKI occurred in 38 (40%) and 42 (44%) patients by measured serum creatinine and fluid overload corrected creatinine, respectively, and was most commonly diagnosed on postoperative day 2. The median time to infection from the time of surgery and AKI was 7 days (IQR 5–14 days) and 6 days (IQR 3–13 days), respectively. After adjusting for confounders, the odds of a postoperative infection were 3.64 times greater in patients with fluid corrected AKI (95% CI, 1.36–9.75; p = 0.01).
Conclusions
Fluid corrected AKI was independently associated with the development of a postoperative infection. These findings support the notion that AKI is an immunosuppressed state that increases the risk of infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sepsis is the leading cause of death in patients with acute kidney injury (AKI) [1,2,3,4]. Sepsis is also the most common cause of AKI. Sepsis-induced AKI significantly worsens patients’ prognosis, when compared to AKI from other causes [5,6,7,8,9,10,11,12,13]. Several adult studies have evaluated for the impact of AKI on subsequent rates of infection or sepsis [14,15,16,17,18,19]. In adults after cardiac surgery, infectious complications were significantly higher among patients with impaired preoperative renal function [15, 20] or postoperative AKI [15, 20, 21]. These findings have led to the conclusion that AKI—like end stage renal disease (ESRD)—is an immunosuppressed state [18, 22, 23].
AKI after pediatric cardiac surgery is common, occurring in 20–50% of patients [24, 25]. The etiology of cardiac surgery associated AKI is multifactorial and is associated with significant morbidity and mortality, including increased duration of mechanical ventilation, prolonged intensive care and hospital length of stay [24, 25], and increased hospital costs [26]. Although AKI is typically diagnosed by a rise in serum creatinine relative to baseline, recent studies in both adults and children suggest that AKI may be more accurately diagnosed when the change in serum creatinine is corrected for fluid overload [27,28,29]. This is particularly important in neonates, who have a higher percent of total body water, and thus fluid overload can have a significant diluting effect on serum creatinine and mask AKI. In neonates with transposition of the great arteries, correcting creatinine for fluid balance increased the incidence of AKI and strengthened the association between AKI and postoperative morbidity (duration of mechanical ventilation and length of stay) [27].
The Norwood procedure represents one of the most complex procedures performed for single ventricle heart disease in the neonatal period and is associated with much higher risk for AKI. Mortality rates may be as high as 40% [30,31,32,33,34,35] due to the development of certain postoperative complications such as infection, AKI, and cardiac arrest [35]. AKI requiring temporary or permanent dialysis was associated with the highest mortality risk of 67 and 91%, respectively [35]. We selected this population specifically for the high rate of AKI in order to assess for the outcome of interest.
The high rate of mortality associated with AKI suggests that there are deleterious systemic effects that affect mortality. Since sepsis is the leading cause of death in patient with AKI, it is plausible that AKI may predispose to subsequent infection/sepsis. To date, the relationship between postoperative infection, as a consequence of AKI in children, and cardiac surgery has not been evaluated. The purpose of this study was to evaluate for an association between AKI and postoperative infection. We hypothesized that AKI would be associated with subsequent infection in neonates after cardiac surgery based on associations seen in several adult studies [15,16,17,18,19,20,21, 36].
Materials and methods
A single center retrospective chart review was performed in neonates (≤ 30 days of age) with single right ventricle congenital heart disease undergoing the Norwood operation from January 2009 to December 2015 following institutional review board approval and a waiver of informed consent. Subjects were excluded if they had preexisting abnormalities of the kidneys or genitourinary tract, use of preoperative extracorporeal membrane oxygenation (ECMO), or renal replacement therapy (RRT).
The primary outcome was the development of a postoperative infection. A postoperative infection was defined as either culture positive or culture negative and, for this study, had to occur after a diagnosis of AKI. The Society of Thoracic Surgeons (STS) database provides a comprehensive definition for the presence of a postoperative infection: Sepsis is defined as evidence of serious infection accompanied by a deleterious systemic response. In the time period of the first 48 postoperative or postprocedural hours, the diagnosis of sepsis requires the presence of a systemic inflammatory response syndrome (SIRS) resulting from a proven infection (such as bacteremia, fungemia, or urinary tract infection). In the time period after the first 48 postoperative or postprocedural hours, sepsis may be diagnosed by the presence of a SIRS resulting from suspected or proven infection. During the first 48 h, a SIRS may result from the stress associated with surgery and/or cardiopulmonary bypass. Thus, the clinical criteria for sepsis during this time period should be more stringent. A SIRS is present when at least two of the following criteria are present: hypo- or hyperthermia (> 38.5 or < 36.0), tachycardia or bradycardia, tachypnea, leukocytosis or leukopenia, and thrombocytopenia. Culture positive infection was broadly defined as detection of any organism (bacterial, viral, or fungal) from any source (surgical site, blood, urine, respiratory tract (tracheitis or pneumonia), and intracardiac). We modified the STS definition for culture negative patients, in which we assessed for at least two concurrent vital sign changes on the index day as well as at least one laboratory parameter (although a rise in serum lactate could not be used alone, and we did not consider thrombocytopenia as a marker of infection). Even if these criteria were met, but antimicrobial therapy was discontinued before 5 days, that patient was then considered to be not infected. Culture negative infection was defined as any patient in which there was a high clinical suspicion for infection with abnormal laboratory parameters and clinical signs and administration of at least a 5-day course of antimicrobial therapy. The clinical and laboratory signs included fever (temperature ≥ 38.4 °C), tachycardia (> 75th percentile for age), hypotension (< 25th percentile for age), inadequate tissue oxygen delivery defined by a rising lactate > 2 mmol/L and decline in cerebral near infrared spectroscopy from baseline, a rise in inflammatory markers from postoperative baseline measures, and an elevated or suppressed white blood cell count with abnormal differential cell count based on normative values for age. The infection had to occur after AKI and within 60 days of the index cardiac surgery.
AKI was defined using the neonatal modified Kidney Disease: Improving Global Outcomes (KDIGO) serum creatinine criteria [37] in two ways: (1) using measured creatinine and (2) creatinine corrected for fluid balance and total body water as previously described [27,28,29]. Baseline serum creatinine was the lowest measured value prior to cardiac surgery. AKI must have occurred no sooner than the first postoperative day and up to the fourth postoperative day.
Surgery was performed by two cardiac surgeons. Some patients underwent operative placement of a peritoneal dialysis catheter for passive drainage. This was performed at the discretion of the surgeon. Patients received standard peri-operative antimicrobial prophylaxis using cefazolin, which was continued for three doses following surgery. All patients received pre- and peri-operative steroids (two doses) using methylprednisolone (10 mg/kg) per standard protocol. For refractory low cardiac output syndrome (LCOS) (which is known to occur in the first 6–18 h after cardiac surgery), some patients received postoperative hydrocortisone (2 mg/kg) every 6 h for 24–48 h, which was weaned over the subsequent 2–3 days at the discretion of the cardiac intensivist. Mortality was defined as operative (died in the hospital or within 30 days if after hospital discharge) and other (died after discharge or > 30 days).
Data were collected using Research Electronic Data Capture [38]. Normally distributed variables are summarized as mean ± standard deviation (SD) and were analyzed using t tests. Non-normally distributed variables are summarized as median with interquartile range (IQR) and were analyzed using Wilcoxon Rank Sum tests. Categorical variables are summarized using frequency and proportion and compared using chi-square or Fisher exact tests as appropriate. Multivariable logistic regression was performed to determine the association between AKI and subsequent infection for both measured creatinine and fluid corrected creatinine. We used a combination of criteria determined a priori based on subject matter considerations and biological understanding to designate three sets of covariates for inclusion in the regression models: unadjusted; model 1 adjusted for AKI, delayed sternal closure and use of postoperative steroids; model 2 adjusted for model 1 + peritoneal drain, cardiopulmonary bypass duration, and ethnicity; and model 3 adjusted for model 2 + total ventilation days. A p value of < 0.05 was considered statistically significant. Statistical analyses were performed using SAS software 9.4, Cary, NC, USA, and JMP.
Results
A total of 95 consecutive neonates with a single right ventricle who underwent the Norwood procedure were included in the analysis. No patients were excluded. Importantly, no patients presented in shock. A schematic of patient characteristics is summarized in Fig. 1.
Infection is a common complication after pediatric cardiac surgery
Postoperative infection occurred in 42 (44%) neonates after cardiac surgery. Demographics, operative, postoperative characteristics, and outcomes are summarized in Table 1. The median time to infection from surgery was 7 days (IQR 5–14 days). Cardiopulmonary bypass duration was significantly longer among those who developed a postoperative infection (188.48 ± 40.54 vs. 166.38 ± 36.76; p = 0.007). A greater proportion of patients with delayed sternal closure (69%) and a peritoneal drain (60%) developed a postoperative infection compared to immediate sternal closure (42%) and those who did not have a peritoneal drain (38%) (p = 0.01 and p = 0.04, respectively). A greater proportion of patients who developed a postoperative infection received postoperative hydrocortisone for LCOS (n = 28, 67% vs. n = 25, 47%) (p = 0.07). Duration of mechanical ventilation, intensive care unit length of stay, and hospital length of stay were all significantly longer among patients who developed a postoperative infection. Nineteen (45%) patients had culture positive infection, and 23 (55%) were culture negative (Supplementary Table 1).
AKI is common among neonates following the Norwood procedure
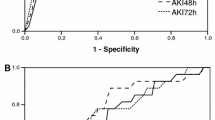
Thirty-eight (40%) patients developed AKI (measured creatinine): stage 1: n = 26, 68%; stage 2: n = 7, 18%, and stage III: n = 5, 13%. Most patients (n = 19, 50%) experienced AKI on postoperative day 2, and the remaining patients experienced AKI on postoperative day 1 (n = 7, 18%), postoperative day 3 (n = 7, 18%), and postoperative day 4 (n = 5, 13%). After correcting creatinine for fluid overload, the rate of AKI increased to 44% (n = 42), and the proportion of patients with stage 3 AKI increased to 21% (n = 9) (Supplementary Fig. 1) (adapted from Basu et al.) [27].
AKI is associated with development of a postoperative infection
AKI (measured creatinine) was more common among those who subsequently developed a postoperative infection (n = 23, 55% vs. n = 15, 28%) (p = 0.01). AKI (fluid corrected) was significantly more common in those with a subsequent postoperative infection (n = 27, 64%) versus those who did not develop a postoperative infection (n = 15, 28%) (p = 0.0008). There was no significant difference in the median time to infection from the day of surgery in patients with AKI (7 days; IQR 5–10 days) compared to those without AKI (8 days, IQR 5–15 days) (p = 0.22). The median time to infection following a diagnosis of AKI (measured and fluid corrected) was 6 days (IQR 3–13 days). In the univariate analysis, the odds of developing a postoperative infection was 3.07 times higher for patients with AKI (measured creatinine) (95% CI, 1.31–7.19) and 4.56 times higher for those with fluid corrected AKI (95% 1.91–10.88). A summary of the univariate analyses is shown in Table 2. When patients with only positive cultures were considered, there was no association between AKI and development of a postoperative infection. Twenty-three patients with AKI (measured) had a postoperative infection, of which 10 (43%) were culture positive (p = 1). Twenty-seven patients with AKI (fluid corrected) had a postoperative infection, of which 11 (40.7%) were culture positive (p = 0.52).
AKI is independently associated with the development of a postoperative infection
AKI (measured creatinine) was independently associated with development of a postoperative infection in model 1 (adjusting for delayed sternal closure and use of postoperative steroids) and model 2 (adjusting for variables in model 1, the presence of a peritoneal drain, cardiopulmonary bypass duration, and ethnicity). AKI was not associated with postoperative infection in model 3, which was adjusted for those variables in model 2 plus total ventilation days (Table 3).
In the assessment of the association between fluid corrected AKI and development of postoperative infection after adjusting for delayed sternal closure, use of postoperative steroids, the presence of a peritoneal drain, cardiopulmonary bypass duration, ethnicity and duration of mechanical ventilation (model 3), the odds of a postoperative infection was 3.64 times greater in patients with fluid corrected AKI compared to those without AKI (95% CI 1.36–9.75, p = 0.01) (Table 4).
Discussion
This study is the first pediatric cardiac surgical cohort in which an association between cardiac surgery associated AKI and development of a subsequent postoperative infection is described. In this study, suspected or confirmed infection after a diagnosis of AKI was common, occurring in 44% of subjects, of which 55 and 64% developed AKI by measured and fluid corrected creatinine, respectively. We found that AKI, when correcting for fluid overload, unmasked additional cases and that fluid corrected AKI was independently associated with subsequent postoperative infection after adjusting for confounders. The pediatric population undergoing cardiac surgery is unique compared to their adult counterparts. Infection is not typically an indication for surgery. Other than genetic abnormalities [34], the comorbid conditions encountered in adults that may be associated with risk of both AKI and infection do not exist in neonates. Thus, our finding of an association between fluid corrected AKI and infection in this neonatal population, even after adjusting for confounders, supports the notion that AKI is an immunosuppressed state that increases the risk for infection. Correcting creatinine for fluid overload has been shown to provide a better parameter for earlier recognition of AKI progression [28] and better explain the significantly higher morbidity and mortality rates [27, 29]. Finally, we selected this particular cohort because the Norwood procedure is complex, with a high rate of both AKI and infection (with delayed sternal closure, longer duration of mechanical ventilation and use of postoperative steroids as known risk factors [39,40,41,42]), thus enriching the pool for the primary outcome.
While it is known that sepsis contributes to AKI, the frequency with which sepsis develops as a consequence of AKI is currently being investigated and has been reported in several adult studies [14,15,16,17,18,19, 43]. The investigators reported that 45% of non-survivors developed sepsis after the development of contrast-induced AKI [14]. In a retrospective analysis of nearly 25,000 adults after cardiac surgery, preoperative and postoperative AKI was independently associated with postoperative infection but the timing between AKI and subsequent infection was not reported [15]. Zanardo et al. [20] and Corwin et al. [21] also demonstrated an increased incidence of postoperative infection in patients with AKI; the independent contribution of postoperative AKI on infection was not assessed. In the non-cardiac surgical population, Mehta et al. evaluated a large cohort of adults who were enrolled in the multicenter observational study of AKI (PICARD) [18]. Approximately 40% of the population developed sepsis a median of 5 days after AKI, with mortality rates in those with sepsis after AKI being much higher than those without AKI. Interestingly, the timing of sepsis after AKI in this study was similar to the timing of infection after AKI in our study. In a separate critically ill cohort, infection occurred in 80% of critically ill patients with AKI who were treated with renal replacement therapy [17]. Finally, while most studies have focused on risk for infection during the index admission, investigators in Taiwan assessed for risk of developing severe sepsis with a median follow-up time of 3.96 years [19]. The incidence of severe sepsis in the AKI group was threefold than those without AKI [19].
The mechanism by which AKI increases the risk for infection/sepsis is not completely understood. Tsalik et al. used a systems biology approach to examine the impact of renal disease and hemodialysis on patient response during critical illness. The metabolome, proteome, and transcriptome were examined to identify factors associated with early community acquired sepsis and non-infectious systemic inflammatory response syndrome [43]. After stratifying for AKI, 58% of the metabolites were different, with the majority of differences accounted for by AKI [43]. While it has been previously hypothesized that accumulation of toxic substances in patients with AKI is what leads to its poor outcomes. However, based on the study by Tsalik et al., plasma levels of seven primary amino acids were decreased in patients with AKI. Interestingly, several of these primary amino acids have also been implicated in endothelial and immune dysfunction [43], which may contribute to the association between AKI and development of subsequent infection. Further studies exploring the mechanistic pathway between AKI and infection are necessary. It is possible that assessment of both immune function and the metabolome concurrently would allow for an improved understanding of the immunosuppressed state caused by AKI.
This study has several important strengths that include the homogenous cohort with a high rate of AKI and postoperative complications such as infection. The timing of AKI can be reasonably assumed to occur during cardiopulmonary bypass. While patients with single ventricle heart disease may not have normal renal function prior to surgery, use of the modified neonatal KDIGO criteria identified a significant proportion with postoperative AKI, and more refined definitions may in fact increase the rate of AKI and strengthen the association with infection. In addition, we assessed for AKI using measured and fluid corrected creatinine, unmasking additional cases. However, there are several important limitations. First, we did not use urine output criteria to define AKI in this cohort as it has not been validated in the pediatric cardiac surgery cohort. This may result in missed cases of AKI, based on a recently published pediatric epidemiology study of critically ill children [44]. Second, there may be other specific factors associated with postoperative infection that we were not able to identify based on the retrospective nature of this study and collinearity between variables. Third, our sample size was relatively small, and validation of these findings in a larger cohort is necessary. Fourth, it is possible that the diagnosis of LCOS could be interpreted as culture negative infection given the similar constellation of clinical findings. However, none of the patients developed an infection within the typical period of LCOS (12–18 h after cardiac surgery). Our criteria for assessment of infection were slightly more rigorous than the STS database.
In conclusion, fluid corrected AKI was independently associated with subsequent postoperative infection. Thus, finding an association between AKI and infection, even after adjusting for confounders, supports the notion that AKI is an immunosuppressed state that increases the risk of infection. Future large prospective studies in children after cardiac surgery are necessary to validate the association between postoperative AKI and infection and to investigate the mechanistic pathways by which this occurs.
References
Woodrow G, Turney JH (1992) Cause of death in acute renal failure. Nephrol Dial Transplant 7:230–234
Liano F, Pascual J (1996) Epidemiology of acute renal failure: a prospective, multicenter, community-based study. Madrid Acute Renal Failure Study Group. Kidney Int 50:811–818
Barretti P, Soares VA (1997) Acute renal failure: clinical outcome and causes of death. Renal Fail 19:253–257
Selby NM, Kolhe NV, CW MI, Monaghan J, Lawson N, Elliott D, Packington R, Fluck RJ (2012) Defining the cause of death in hospitalised patients with acute kidney injury. PLoS One 7:e48580
Bagshaw SM, George C, Bellomo R (2008) Early acute kidney injury and sepsis: a multicentre evaluation. Crit Care 12:R47
Bagshaw SM, Uchino S, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Oudemans-van Straaten HM, Ronco C, Kellum JA (2007) Septic acute kidney injury in critically ill patients: clinical characteristics and outcomes. Clin J Am Soc Nephrol 2:431:439
Kim WY, Huh JW, Lim CM, Koh Y, Hong SB (2012) Analysis of progression in risk, injury, failure, loss, and end-stage renal disease classification on outcome in patients with severe sepsis and septic shock. J Crit Care 27:104.e101–104.e107
Piccinni P, Cruz DN, Gramaticopolo S, Garzotto F, Dal Santo M, Aneloni G, Rocco M, Alessandri E, Giunta F, Michetti V, Iannuzzi M, Belluomo Anello C, Brienza N, Carlini M, Pelaia P, Gabbanelli V, Ronco C (2011) Prospective multicenter study on epidemiology of acute kidney injury in the ICU: a critical care nephrology Italian collaborative effort (NEFROINT). Minerva Anestesiol 77:1072–1083
Poukkanen M, Vaara ST, Pettila V, Kaukonen KM, Korhonen AM, Hovilehto S, Inkinen O, Laru-Sompa R, Kaminski T, Reinikainen M, Lund V, Karlsson S (2013) Acute kidney injury in patients with severe sepsis in Finnish Intensive Care Units. Acta Anaesthesiol Scand 57:863–872
Shah PR, Gireesh MS, Kute VB, Vanikar AV, Gumber MR, Patel HV, Goplani KR, Trivedi HL (2013) Renal involvement in sepsis: a prospective single-center study of 136 cases. Saudi J Kidney Dis Transpl 24:620–629
Vandijck DM, Reynvoet E, Blot SI, Vandecasteele E, Hoste EA (2007) Severe infection, sepsis and acute kidney injury. Acta Clin Belg 62(Suppl 2):332–336
Zang ZD, Yan J (2013) An analysis of clinical characteristics of septic acute kidney injury by using criteria of Kidney Disease: Improving Global Outcomes. Zhonghua Nei Ke Za Zhi 52:299–304
Zhu J, Zhang M (2015) Analysis of the characteristics of patients suffering from acute kidney injury following severe trauma receiving renal replacement therapy. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 27:349–353
Levy EM, Viscoli CM, Horwitz RI (1996) The effect of acute renal failure on mortality. A cohort analysis. JAMA 275:1489–1494
Thakar CV, Yared JP, Worley S, Cotman K, Paganini EP (2003) Renal dysfunction and serious infections after open-heart surgery. Kidney Int 64:239–246
Hoste EA, Blot SI, Lameire NH, Vanholder RC, De Bacquer D, Colardyn FA (2004) Effect of nosocomial bloodstream infection on the outcome of critically ill patients with acute renal failure treated with renal replacement therapy. J Am Soc Nephrol 15:454–462
Reynvoet E, Vandijck DM, Blot SI, Dhondt AW, De Waele JJ, Claus S, Buyle FM, Vanholder RC, Hoste EA (2009) Epidemiology of infection in critically ill patients with acute renal failure. Crit Care Med 37:2203–2209
Mehta RL, Bouchard J, Soroko SB, Ikizler TA, Paganini EP, Chertow GM, Himmelfarb J (2011) Sepsis as a cause and consequence of acute kidney injury: Program to Improve Care in Acute Renal Disease. Intensive Care Med 37:241–248
Lai TS, Wang CY, Pan SC, Huang TM, Lin MC, Lai CF, Wu CH, Wu VC, Chien KL, National Taiwan University Hospital Study Group on Acute Renal F (2013) Risk of developing severe sepsis after acute kidney injury: a population-based cohort study. Crit Care 17:R231
Zanardo G, Michielon P, Paccagnella A, Rosi P, Calo M, Salandin V, Da Ros A, Michieletto F, Simini G (1994) Acute renal failure in the patient undergoing cardiac operation. Prevalence, mortality rate, and main risk factors. J Thorac Cardiovasc Surg 107:1489–1495
Corwin HL, Sprague SM, GA DL, Norusis MJ (1989) Acute renal failure associated with cardiac operations. A case-control study. J Thorac Cardiovasc Surg 98:1107–1112
Faubel S, Shah PB (2016) Immediate consequences of acute kidney injury: the impact of traditional and nontraditional complications on mortality in acute kidney injury. Adv Chronic Kidney Dis 23:179–185
Himmelfarb J, Le P, Klenzak J, Freedman S, McMenamin ME, Ikizler TA, Group P (2004) Impaired monocyte cytokine production in critically ill patients with acute renal failure. Kidney Int 66:2354–2360
Blinder JJ, Goldstein SL, Lee VV, Baycroft A, Fraser CD, Nelson D, Jefferies JL (2012) Congenital heart surgery in infants: effects of acute kidney injury on outcomes. J Thorac Cardiovasc Surg 143:368–374
Li S, Krawczeski CD, Zappitelli M, Devarajan P, Thiessen-Philbrook H, Coca SG, Kim RW, Parikh CR (2011) Incidence, risk factors, and outcomes of acute kidney injury after pediatric cardiac surgery: a prospective multicenter study. Crit Care Med 39:1493–1499
Kwiatkowski DM, Goldstein SL, Cooper DS, Nelson DP, Morales DL, Krawczeski CD (2017) Peritoneal dialysis vs furosemide for prevention of fluid overload in infants after cardiac surgery: a randomized clinical trial. JAMA Pediatr 171:357–364
Basu RK, Andrews A, Krawczeski C, Manning P, Wheeler DS, Goldstein SL (2013) Acute kidney injury based on corrected serum creatinine is associated with increased morbidity in children following the arterial switch operation. Pediatr Crit Care Med 14:e218–e224
Macedo E, Bouchard J, Soroko SH, Chertow GM, Himmelfarb J, Ikizler TA, Paganini EP, Mehta RL, Program to Improve Care in Acute Renal Disease S (2010) Fluid accumulation, recognition and staging of acute kidney injury in critically-ill patients. Crit Care 14:R82
Liu KD, Thompson BT, Ancukiewicz M, Steingrub JS, Douglas IS, Matthay MA, Wright P, Peterson MW, Rock P, Hyzy RC, Anzueto A, Truwit JD (2011) Acute kidney injury in patients with acute lung injury: impact of fluid accumulation on classification of acute kidney injury and associated outcomes. Crit Care Med 39:2665–2671
Ohye RG, Sleeper LA, Mahony L, Newburger JW, Pearson GD, Lu M, Goldberg CS, Tabbutt S, Frommelt PC, Ghanayem NS, Laussen PC, Rhodes JF, Lewis AB, Mital S, Ravishankar C, Williams IA, Dunbar-Masterson C, Atz AM, Colan S, Minich LL, Pizarro C, Kanter KR, Jaggers J, Jacobs JP, Krawczeski CD, Pike N, BW MC, Virzi L, Gaynor JW (2010) Comparison of shunt types in the Norwood procedure for single-ventricle lesions. N Engl J Med 362:1980–1992
Reemtsen BL, Pike NA, Starnes VA (2007) Stage I palliation for hypoplastic left heart syndrome: Norwood versus Sano modification. Curr Opin Cardiol 22:60–65
Sano S, Huang SC, Kasahara S, Yoshizumi K, Kotani Y, Ishino K (2009) Risk factors for mortality after the Norwood procedure using right ventricle to pulmonary artery shunt. Ann Thorac Surg 87:178–185 discussion 185-176
Shamszad P, Gospin TA, Hong BJ, McKenzie ED, Petit CJ (2013) Impact of preoperative risk factors on outcomes after Norwood palliation for hypoplastic left heart syndrome. J Thorac Cardiovasc Surg 147:897–901
Tabbutt S, Ghanayem N, Ravishankar C, Sleeper LA, Cooper DS, Frank DU, Lu M, Pizarro C, Frommelt P, Goldberg CS, Graham EM, Krawczeski CD, Lai WW, Lewis A, Kirsh JA, Mahony L, Ohye RG, Simsic J, Lodge AJ, Spurrier E, Stylianou M, Laussen P (2012) Risk factors for hospital morbidity and mortality after the Norwood procedure: a report from the Pediatric Heart Network Single Ventricle Reconstruction trial. J Thorac Cardiovasc Surg 144:882–895
Hornik CP, He X, Jacobs JP, Li JS, Jaquiss RD, Jacobs ML, O'Brien SM, Peterson ED, Pasquali SK (2011) Complications after the Norwood operation: an analysis of the Society of Thoracic Surgeons Congenital Heart Surgery Database. Ann Thorac Surg 92:1734–1740
Liano F, Junco E, Pascual J, Madero R, Verde E (1998) The spectrum of acute renal failure in the intensive care unit compared with that seen in other settings. The Madrid Acute Renal Failure Study Group. Kidney Int Suppl 66:S16–S24
Selewski DT, Charlton JR, Jetton JG, Guillet R, Mhanna MJ, Askenazi DJ, Kent AL (2015) Neonatal acute kidney injury. Pediatrics 136:e463–e473
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381
Algra SO, Driessen MM, Schadenberg AW, Schouten AN, Haas F, Bollen CW, Houben ML, Jansen NJ (2012) Bedside prediction rule for infections after pediatric cardiac surgery. Intensive Care Med 38:474–481
Barker GM, O'Brien SM, Welke KF, Jacobs ML, Jacobs JP, Benjamin DK Jr, Peterson ED, Jaggers J, Li JS (2010) Major infection after pediatric cardiac surgery: a risk estimation model. Ann Thorac Surg 89:843–850
Kansy A, Jacobs JP, Pastuszko A, Mirkowicz-Malek M, Manowska M, Jezierska E, Maruszewski P, Burczynski P, Maruszewski B (2012) Major infection after pediatric cardiac surgery: external validation of risk estimation model. Ann Thorac Surg 94:2091–2095
Mastropietro CW, Barrett R, Davalos MC, Zidan M, Valentine KM, Delius RE, Walters HL 3rd (2013) Cumulative corticosteroid exposure and infection risk after complex pediatric cardiac surgery. Ann Thorac Surg 95:2133–2139
Tsalik EL, Willig LK, Rice BJ, van Velkinburgh JC, Mohney RP, McDunn JE, Dinwiddie DL, Miller NA, Mayer ES, Glickman SW, Jaehne AK, Glew RH, Sopori ML, Otero RM, Harrod KS, Cairns CB, Fowler VG, Rivers EP, Woods CW, Kingsmore SF, Langley RJ (2015) Renal systems biology of patients with systemic inflammatory response syndrome. Kidney Int 88:804–814
Kaddourah A, Basu RK, Bagshaw SM, Goldstein SL, Investigators A (2017) Epidemiology of acute kidney injury in critically ill children and young adults. N Engl J Med 376:11–20
Acknowledgements
We would like to thank the Heart Institute at Children’s Hospital Colorado and Pediatric Kidney Injury and Disease Stewardship (PKIDS) Program for their support during this study. An abstract was presented at the 2016 Pediatric Cardiac Intensive Care Society Meeting, Miami, FL.
Financial support
None
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any financial relationships to disclose.
Electronic supplementary material
Supplementary Fig. 1
Shifts of patients between Kidney Disease Improving Global Outcomes (KDIGO) stages after fluid correction of serum creatinine. Serum creatinine was corrected for fluid balance after the Norwood procedure. Several patients shifted between KDIGO stages (stage listed: number of patients) on the day of acute kidney injury (AKI). (GIF 56.6 kb)
Supplementary Table 1
(DOCX 59.6 kb)
Rights and permissions
About this article
Cite this article
SooHoo, M., Griffin, B., Jovanovich, A. et al. Acute kidney injury is associated with subsequent infection in neonates after the Norwood procedure: a retrospective chart review. Pediatr Nephrol 33, 1235–1242 (2018). https://doi.org/10.1007/s00467-018-3907-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-018-3907-5