Abstract
Background
There is a paucity of data on blood pressures (BP), urinary albumin, and mineral excretion in early childhood in contemporary cohorts of extremely low gestational age (GA) neonates. Our aim was to compare BPs and the urinary excretion of albumin, calcium, and phosphate in preterm and term-born cohorts in early childhood.
Methods
This was a prospective observational study conducted at a single center, involving children <5 years age, born preterm (GA <30 weeks) or at term (≥37 weeks’ GA). Urinary albumin (mg/L), calcium and phosphate levels indexed to creatinine (mg/dL), and BP were measured.
Results
The median (IQR) follow-up age of our cohort (n = 106) was 30 (16–48) months. Preterm-born children (n = 55) had a significantly lower mean GA and birth weight and higher mean systolic, diastolic, and mean BPs, compared with term (n = 51) controls. A significantly higher proportion of preterm-born children weighed <10th centile and had systolic BP >95th centile at follow-up. Albumin and calcium excretion did not differ between the groups; median urine–phosphate creatinine ratios were higher in the preterm group. On logistic regression, lower GA and younger age at follow-up were significantly associated with an increased risk of systolic and diastolic BP above the 95th centile; male gender was associated with decreased risk of diastolic hypertension.
Conclusions
Even in early childhood, children born preterm had significantly elevated BP, compared with their term-born counterparts. Closer monitoring of BPs in this population may be warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although survival among preterm (<37 weeks’ gestational age [GA]) infants has increased in recent years, there is a recognition that children born preterm may have long-term renal–metabolic sequelae. Low birth weight has been related to lower glomerular number at birth and impaired postnatal renal growth and glomerulogenesis, possibly secondary to nephrotoxic medications, acute kidney injury (AKI), hypotension, and impaired perfusion [1–3]. The reduced number of nephrons with a subsequent increase in renal blood flow per glomerulus may lead to glomerular hypertrophy, which, in turn, results in albuminuria [4]. A systematic review of the published literature found evidence for a possible causal link between chronic kidney disease, defined as albuminuria, low glomerular filtration rate or end-stage renal disease and low birth weight (excluding the <1,500-g subgroup) [5]. Hypercalciuria and albuminuria in children born preterm, compared with their term-born counterparts have been reported in early to mid-childhood in some, although not all, studies [2, 3, 6–8]. In addition, very low birth weight (<1.5 kg) infants with diuretic-related renal calcifications have impaired tubular reabsorption of phosphate at 1–2 years of age, compared with their counterparts without nephrocalcinosis [9].
A recent review of 15 studies reported that the prevalence of hypertension in children and adolescents born preterm, using casual or ambulatory blood pressure (BP) measurement ranged from 6 to 25% overall and 10 to 25% between the ages of 6 and 12 years [10]. Most studies had a follow-up of between 10 and 27 years of age, and only two studies were limited to extremely low birth weight (<1 kg) infants [6, 11]. Systolic and diastolic BPs were significantly higher at follow-up ages of 15–27 years in the very low birth weight compared with the normal cohort [12–16]. In another meta-analysis of 10 studies, 1,342 preterm (mean GA 30.2; range, 28.8–34.1 weeks) or very low birth weight (mean 1,280 g, range 1,098–1,958 g) subjects had a mean systolic BP of 2.5 mmHg (95% CI 1.7–3.3 mmHg), which was higher at a mean (range) age of 17.8 (6.3–22.4) years, compared with the 1,738 subjects born at term [17]. Elevated BP in children born extremely preterm is thought to be related to impaired renal development, dysregulation of the renin–angiotensin system, cardiovascular remodeling, altered autonomic control, and vascular/endothelial stiffness [18].
Data on BPs and biomarkers of renal injury in early childhood in contemporary cohorts of extremely low GA (<30 weeks) neonates are scant. It is important to know whether the differences in preterm and term-born cohorts manifest in early childhood so that earlier preventive efforts can be made. The aims of the present study, therefore, were to:
-
1.
Compare systolic, diastolic, and mean BP and urinary excretion of protein, calcium and phosphate, indexed to creatinine, in extremely preterm (<30 weeks) and term-born cohorts at follow-up ages of 6 months to 5 years
-
2.
Assess the relationship, if any, between clinical variables and elevated BPs
Our hypothesis was that asymptomatic children born preterm will have higher levels of albumin and calcium excretion in urine and higher BPs than term controls in early childhood.
Materials and methods
This was a cross-sectional, prospective observational study conducted in the Developmental Assessment Clinic or General Pediatric Clinic of Children’s Hospital of Michigan between August 2010 and June 2011. Children included were 6 months to 5 years corrected age born preterm (GA < 30 weeks; n = 55). The neonatal hospitalization was either in the Hutzel Women’s Hospital (n = 31) or, following referral from a delivery center, in Children’s Hospital of Michigan (n = 24) tertiary care Neonatal Intensive Care Units (NICUs). These infants were all referred to and tracked for developmental follow-up at 6 months corrected age and every 6–12 months thereafter until 5 years of age. Term-born (≥37 weeks GA) controls (n = 51), 6 months to 5 years old, were recruited in the same time period at an out-patient pediatric well-child clinic visit if they had no known cardiac or renal disorder. Term infants who had been admitted to the NICU were excluded. The study was approved by the Wayne State University Institutional Review Board and written parental consent was obtained in all cases.
Gestational age was confirmed by the best obstetric estimate documented on the birth records, using an early ultrasound, last menstrual period or neonatal examination, in that order. Data for the preterm subgroup were extracted from the electronic medical records and included maternal demographic and clinical variables: race, maternal age, gravidity and parity, diabetes, chronic hypertension or pregnancy-induced hypertension, substance use, and receipt of prenatal care and antenatal steroids. Neonatal data including GA, gender, birth weight, Apgar score at 5 min, mode of delivery, history of hypotension, need for pressors, sepsis, cumulative antibiotic duration, hemodynamically significant patent ductus arteriosus requiring treatment and bronchopulmonary dysplasia, defined as supplemental oxygen at 36 weeks’ postmenstrual age, and length of hospitalization were recorded. Receipt of diuretics, specifically furosemide, were noted. In addition, peak and nadir values and ages of serum creatinine and its measure at discharge home were also recorded. A history of AKI was elicited in each preterm infant by an assessment of change in serum creatinine values over a 48-h period using the validated acute kidney injury network (AKIN) definition [19].
At the clinic visit, after obtaining informed parental consent, a urine sample was collected with a urine bag in children in diapers or a clean catch specimen in toilet-trained children. The sample was immediately sent to the laboratory for measurement of levels of albumin (mg/L), calcium, phosphate, and creatinine (mg/dL). Albumin–creatinine and calcium–creatinine ratios were calculated. Microalbuminuria was defined as an albumin–creatinine ratio above 20 mg/g [11]. Hypercalciuria and hyperphosphaturia were defined as values above the 95th age-specific centile [20]. Weight and height were recorded at the visit using a standard clinic weighing scale and stadiometer length boards or height scales. Weight and height centiles, categorized by gender, were determined based on Centers for Disease Control and Prevention curves [21]. For infants born preterm, corrected age, defined as age post-term was used until 2 years old. BPs were measured after 5 min of sitting quietly (when the infant was able to sit without support), with the back supported (on the parent’s lap or on a chair), uncrossed legs, feet on the floor and arm supported at the level of the heart. In younger children, BP was measured in the supine position. BPs were measured using an appropriate sized arm cuff, with a bladder length covering at least 80% and a width covering at least 40% of the mid-arm circumference [22]. BP was preferably measured in the right upper extremity. If this was not feasible for any reason (e.g., hemiplegia, contracture), the left upper extremity was used. BPs were measured using the automated technique (Dinamap®). Systolic, diastolic, and mean BP were obtained twice in the calm state, with at least 5 min between readings; the average measurement calculated from the recorded values was used for analysis. If only one BP could be obtained in a calm resting state, then that single value was recorded. BP measurement was timed during feeding or blowing bubbles to distract younger infants during measurement. Age-, gender-, and height-specific norms for BP for children were used to determine the centiles [22]. Z scores for systolic BPs were calculated using age, gender and height-adjusted nomograms [22].
Sample size was predetermined to detect a 7-mmHg difference in systolic BP between groups with a standard deviation of 10.5. The calculated sample size of 36 subjects in each group was increased to 50 in each group to account for the inability to measure reliable BP. Data were described as mean (SD) or median (interquartile range IQR) or n (%) as appropriate. Comparisons between groups utilized Student’s t test, the Mann–Whitney U test or Chi-squared test, as appropriate. Further, we conducted binary logistic regression analysis to examine the association between clinical variables and elevated systolic BPs above 95th centiles for gender and age. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. Data were analyzed using SPSS software version 20.0 (SPSS, Chicago, IL, USA).
Results
Our study cohort comprised 55 ex-preterm and 51 term children born between 2005 and 2011. Among the preterm-born subgroup of children, 34 (61.8%) of whom were male, the median (IQR) GA was 26 (24–28) weeks and birth weight was 750 (657–919) g. None of the mothers had a known history of chronic renal or cardiac disease. None of the children had a diagnosis of hypertension at discharge or during the birth hospitalization. Table 1 provides a description of maternal and neonatal characteristics of the ex-preterm children. For the control group, mothers’ mean (SD) age was 26 (5.7) years and median (IQR) gravidity was 2 (1–4). Most of the controls (46; 83.6%) had received prenatal care. Two (3.9%) mothers had diabetes and 4 (7.8%) had hypertension.
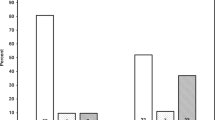
The median (IQR) follow-up age of the cohort was 30 (16–48) months. The comparison of demographic and neonatal variables and follow-up measures between the two groups is shown in Table 2. As expected, the groups had significant differences in mean GA, birth weight, and proportion of multiples, but were similar in age, race, and gender. A greater proportion of children born preterm had weights and heights below the 10th centile for corrected age at the time of follow-up. The preterm group had higher systolic, diastolic, and mean BPs and a greater proportion had systolic BP above the 90th (25, 45.5% vs 10, 19.2%; p = 0.010) and 95th centiles (17, 30.9% vs 2, 3.9%; p = 0.001) by the specific age, gender, and height centiles. The proportion with diastolic BP above the 90th centile (65.5% vs 48.0%; p = 0.13) in the two groups were comparable. Figure 1 depicts scatter plots of the z scores of systolic and diastolic BP in groups of term-born and preterm children at different ages. Albumin and calcium excretion did not differ between groups; median urine phosphate creatinine ratios were higher in the preterm group than in term-born controls. Microalbuminuria was detected in 13.2% of the cohort and did not differ between groups. Table 3 is a comparison of neonatal characteristics in preterm-born children with (n = 17) and without (n = 38) systolic BP above the 95th centile at follow-up. There was no difference in the proportion of infants who had an umbilical arterial catheter or received antibiotics between the two groups. The only significant difference between the groups was the younger age of the group with high systolic BP. The proportion of boys tended to be lower in those with BP above the 95th centile.
Binary logistic regression was performed to evaluate the association between high systolic BP (>95th centile for age, gender, and height centile) and GA, gender, multiples, weight centiles at follow-up, and age at follow-up. Table 4 depicts ORs and 95% CIs of the variables associated with systolic hypertension. Lower GA and younger age at follow-up were significantly associated with a higher risk of systolic BP > 95th centile. Similar analyses of diastolic BPs above the 95th centiles revealed significant associations with GA (OR 0.924; 95% CI 0.854–1.000, p = 0.049), age (OR 0.953; 95% CI 0.926–0.981, p = 0.001), and male gender (OR 0.217; 95% CI 0.079–0.599, p = 0.003).
Discussion
In this prospective observational case–control study, children born preterm at <30 weeks GA had significantly higher BPs and a higher prevalence of elevated BP beyond the 90th and 95th centiles based on age-, gender-, and height-specific norms at a median follow-up age of 30 months. Lower GA and age at follow-up were independently associated with elevated BP above the 95th centile. Male gender was associated with a lower risk of diastolic BP above the 95th centile. Urinary excretion of phosphate was also increased in children born extremely preterm, although the proportion of children with phosphaturia exceeding the 95th centile was similar in the two groups. Albumin and calcium excretion in the urine were similar in preterm-born children and term-born controls.
The association between elevated BPs and preterm birth has been demonstrated in several studies at school age, adolescence, and young adulthood. Very few studies have evaluated this association in early childhood. In a recent population-based subset cohort of 68 extremely preterm (GA <27 weeks) infants in Sweden, systolic and diastolic BP z scores at a corrected age of 2.5 years were significantly higher than in term controls [23]. Among the children born extremely preterm, 44% had systolic BPs at or higher than the 90th centile. Extreme prematurity was associated with a 2.63 (95% CI 1.24–5.57) higher odds ratio for systolic hypertension; when stratified by gender, the significant effect of extreme prematurity was limited to boys. Diastolic BP z scores were significantly higher in both boys and girls born preterm than in the term-born controls. In another cross-sectional study of systolic BPs in very low birth weight infants at 1, 2, and 3 years of age, observed values and systolic BP z scores exceeded the expected value at each age (p < 0.01) [23]. At 2 years, the mean (SD) systolic BP (91.5 [10] vs 87.1 [2.9] mmHg) and z scores (0.41 [0.98] vs reference value 0) were significantly higher than expected norms in the very low birth weight infants (n = 33). Systolic BP was greater than the 90th and 95th centiles in 15% and 9% of infants respectively [24]. In this study, in contrast to girls, systolic BP z scores in boys fell from 1–3 years of age and did not differ from what was expected at 3 years. The rate of prehypertension, defined as levels above 90th centile, decreased from 42 to 0% in boys and was unchanged (17–24%) in girls. At 2 years of age, rates of prehypertension were similar in both genders [24].
Our study confirms that elevated systolic and diastolic BPs in children born preterm, compared with term controls, may manifest as early as 1–5 years of age, although the exact age of onset of this predilection cannot be determined. Rates of elevated BPs above the 90th centile in our cohort are almost identical to those reported in the Swedish study, but higher than the other cross-sectional study. This difference may be due to the automated method of BP measurement in our study and the Swedish study, compared with the manual method. In the current study, male gender was associated with a significantly lower risk of diastolic, but not systolic BP, above the 95th centile. Although results are conflicting, a previous large follow-up study of 296 children born in 1989–1992 with birth weights 600 to 1,250 g and 95 term controls at 16 years demonstrated that male gender was associated with increased systolic BP (5.1 mmHg) and decreased diastolic BP (−2.4 mmHg) compared with female gender [25]. Other studies have also shown higher BPs in adolescent girls and adult women born preterm [25–27]. The decline in the rate of systolic hypertension with increasing age is also consistent with previous literature [24]. The reasons for elevated BPs at younger ages may be related to anxiety in the younger child during measurement, or “white coat hypertension,” or catch-up growth, or renal recovery during early childhood. Neither our study nor the Swedish study was able to find any associations between neonatal variables and BPs at follow-up in the preterm-born group of children, perhaps because of the small sample size [23].
In addition to BP measurement, we evaluated urinary excretion of albumin, calcium, and phosphate indexed to creatinine. Previous studies have shown that low birth weight is a risk factor (OR 1.81 [95% CI 1.19–2.77]) for albuminuria in adulthood [5]. At younger ages, though, this association has not been consistently seen. Microalbuminuria above 20 mg/g creatinine, though, was detected in 5 preterm-born children and was not significantly different in the two groups [12]. In another single-center study, 2 out of 50 preterm-born (<30 weeks GA and <1,000 g birth weight) children had microalbuminuria and 2 had hypercalciuria [8].
Microalbuminuria, defined as an albumin–creatinine ratio above 20 mg/g, was noted in 8.3% of a preterm group of children in one study [7]. Rates of microalbuminuria were similar in preterm-born and term-born children in our study and higher than the previous reports at older ages. Calcium excretion was comparable in the two groups, and below the reported 95th age-specific centiles in the healthy population. Median phosphate excretion was higher in the preterm-born group, but rates of phosphaturia above the 95th age-specific centile were comparable in the two groups. In early childhood, therefore, we could not detect any strong evidence for microalbuminuria, or altered calcium, or phosphate excretion. We speculate that this might reflect newer management approaches or better growth in the neonatal period. In addition, Luyckx and colleagues have opined that low nephron number is unlikely to be the sole risk factor for renal disease, and would probably be associated with renal disease only in the presence of additional intrauterine and postnatal insults [28]. The wide age range of follow-up in our study and the variation of some urinary markers with age may have precluded the detection of abnormalities. Ongoing follow-up of the high-risk preterm population appears to be warranted.
We acknowledge the limitations of our study. BP was measured at a single clinic visit using an automated device. Children in the study underwent a maximum of two BP measurements. However, a previous study showed that at 2.5 years of age, there was no difference in mean systolic or diastolic BP among children in whom BP was measured 1, 2, or 3 times. We did not have measures of renal size on ultrasound and used random urine samples for the measurement of albumin, calcium, and phosphate excretion. We did not have information on vitamin supplementation and details of the pregnancy were unavailable for the term-born controls. Although we used published age-specific norms for calcium and phosphate to creatinine ratios derived from a healthy population, children born preterm may weigh less and have decreased creatinine excretion, with an alteration in these ratios. Our sample size, although small, was in line with that of other studies. Our cohorts had a wide age range, with the associated limitations of age-related variability in urinary electrolyte and albumin excretion. Although not statistically significant, the mean ages in the preterm and term subgroups were also different, and this could have altered our BP findings. The preterm sample was drawn from among those who attended developmental follow-up clinic, with the consequent selection bias. Nonetheless, the current prospective evaluation of renal function and BP at a young age in a high-risk, preterm contemporary cohort provides important insights into the developmental origins of adult disease. The age at follow-up was earlier than in many studies and allowed an investigation of the interplay of morbidities associated with preterm birth and environmental factors. Our data suggest that BP might be elevated at an age below 3 years in preterm children and should be measured at every medical visit. Earlier detection of elevated BP at this age may allow targeted interventions to prevent further progression.
Abbreviations
- AKI:
-
Acute kidney injury
- BP:
-
Blood pressure
- GA:
-
Gestational age
- NICU:
-
Neonatal Intensive Care Unit
References
Hughson M, Farris AB, Douglas-Denton R, Hoy WE, Bertram JF (2003) Glomerular number and size in autopsy kidneys: the relationship to birth weight. Kidney Int 63:2113–2122
Franco MC, Nishida SK, Sesso R (2008) GFR estimated from cystatin C versus creatinine in children born small for gestational age. Am J Kidney Dis 51(6):925–932
Puddu M, Podda MF, Mussap M, Tumbarello R, Fanos V (2009) Early detection of microalbuminuria and hypertension in children of very low birthweight. J Matern Fetal Neonatal Med 22(2):83–88
Zanardo V, Fanelli T, Weiner G, Fanos V, Zaninotto M, Visentin S, Cavallin F, Trevisanuto D, Cosmi E (2011) Intrauterine growth restriction is associated with persistent aortic wall thickening and glomerular proteinuria during infancy. Kidney Int 80(1):119–123
White SL, Perkovic V, Cass A, Chang CL, Poulter NR, Spector T, Haysom L, Craig JC, Salmi IA, Chadban SJ, Huxley RR (2009) Is low birth weight an antecedent of CKD in later life? A systematic review of observational studies. Am J Kidney Dis 54:248–261
Rodríguez-Soriano J, Aguirre M, Oliveros R, Vallo A (2005) Long-term renal follow-up of extremely low birth weight infants. Pediatr Nephrol 20(5):579–584
Iacobelli S, Loprieno S, Bonsante F, Latorre G, Esposito L, Gouyon JB (2007) Renal function in early childhood in very low birthweight infants. Am J Perinatol 24(10):587–592
Bacchetta J, Harambat J, Guy B, Putet G, Cochat P, Dubourg L (2009) Long term renal outcome of children born preterm: a regular follow-up is needed. Arch Pediatr 16 [Suppl 1]:S42–S48
Downing GJ, Egelhoff JC, Daily DK, Thomas MK, Alon U (1992) Kidney function in very low birth weight infants with furosemide-related renal calcifications at ages 1 to 2 years. J Pediatr 120(4Pt1):599–604
Poplawska K, Dudek K, Koziarz M, Cieniawski D, Drożdż T, Smiałek S, Drożdż D, Kwinta P (2012) Prematurity-related hypertension in children and adolescents. Int J Pediatr 2012:537936
Kwinta P, Klimek M, Drozdz D, Grudzień A, Jagła M, Zasada M, Pietrzyk JJ (2011) Assessment of long-term renal complications in extremely low birth weight children. Pediatr Nephrol 26(7):1095–1103
Hovi P, Andersson S, Raikkonen K, Strang-Karlsson S, Järvenpää AL, Eriksson JG, Pesonen AK, Heinonen K, Pyhälä R, Kajantie E (2010) Ambulatory blood pressure in young adults with very low birth weight. J Pediatr 156(1):54–59
Pharoah PO, Stevenson CJ, West CR (1998) Association of blood pressure in adolescence with birthweight. Arch Dis Child Fetal Neonatal Ed 79(2):F114–F118
Doyle LW, Faber B, Callanan C, Morley R (2003) Blood pressure in late adolescence and very low birth weight. Pediatrics 111(2):252–257
Hack M, Schluchter M, Cartar L, Rahman M (2005) Blood pressure among very low birth (<1.5 kg) young adults. Pediatr Res 58(4):677–684
Pyhala R, Raikkonen K, Feldt K, Andersson S, Hovi P, Eriksson JG, Järvenpää AL, Kajantie E (2009) Blood pressure responses to psychosocial stress in young adults with very low birth weight: Helsinki study of very low birth weight adults. Pediatrics 123(2):731–734
de Jong F, Monuteaux MC, van Elburg RM, Gillman MW, Belfort MB (2012) Systematic review and meta-analysis of preterm birth and later systolic blood pressure. Hypertension 59(2):226–234
Norman M (2010) Preterm birth: an emerging risk factor for adult hypertension? Semin Perinatol 34:183–187
Askenazi DJ, Griffin R, McGwin G, Carlo W, Ambalavanan N (2009) Acute kidney injury is independently associated with mortality in very low birthweight infants: a matched case–control analysis. Pediatr Nephrol 24:991–997
Matos V, van Melle G, Boulat O, Markert M, Bachmann C, Guignard JP (1997) Urinary phosphate/creatinine, calcium/creatinine and magnesium/creatinine ratios in a healthy paediatric population. J Pediatr 131(2):252–257
Centers for Disease Control and Prevention, National Center for Health Statistics. CDC growth charts: United States. http://www.cdc.gov/growthcharts/. 30 May 2000
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114 [2 Suppl 4 report]:555–576
Bonamy AK, Källén K, Norman M (2012) High blood pressure in 2.5-year-old children born extremely preterm. Pediatrics 129(5):e1199–e1204
Duncan AF, Heyne RJ, Morgan JS, Ahmad N, Rosenfeld CR (2011) Elevated systolic blood pressure in preterm very-low-birth-weight infants ≤3 years of life. Pediatr Nephrol 26(7):1115–1121
Vohr BR, Allan W, Katz KH, Schneider KC, Ment LR (2010) Early predictors of hypertension in prematurely born adolescents. Acta Paediatr 99(12):1812–1818
Bonamy AK, Bendito A, Martin H, Andolf E, Sedin G, Norman M (2005) Preterm birth contributes to increased vascular resistance and higher blood pressure in adolescent girls. Pediatr Res 58(5):845–849
Kistner A, Jacobson L, Jaconson SH, Svensson E, Hellstrom A (2002) Low gestational age associated with abnormal retinal vascularization and increased blood pressure in adult women. Pediatr Res 51(6):675–680
Luyckx VA, Bertram JF, Brenner BM, Fall C, Hoy WE, Ozanne SE, Vikse BE (2013) Effect of fetal and child health on kidney development and long-term risk of hypertension and kidney disease. Lancet 382:273–283
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics statement
The study was approved by the Wayne State University Institutional Review Board and written parental consent was obtained in all cases.
Sources of financial assistance
Sarnaik Endowment for Resident and Fellow Research, PI: Namrata Vashishta, Faculty supervisor: G Natarajan.
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Vashishta, N., Surapaneni, V., Chawla, S. et al. Association among prematurity (<30 weeks’ gestational age), blood pressure, urinary albumin, calcium, and phosphate in early childhood. Pediatr Nephrol 32, 1243–1250 (2017). https://doi.org/10.1007/s00467-017-3581-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-017-3581-z