Abstract
Background
Patients with sickle cell disease are at risk for developing chronic kidney disease (CKD). Acute kidney injury (AKI) has been linked to progression to CKD, but limited data exist to determine its role in acute complications of sickle cell disease. We hypothesized that AKI occurs in pediatric patients admitted for acute chest syndrome (ACS) and prolongs hospitalization.
Methods
We conducted a 6-year retrospective review of pediatric patients with ACS admitted to a single medical institution.
Results
Of the 149 pediatric patients admitted for ACS during the 6-year study period, 12 (8 %) developed AKI. Comparison of patients with and without AKI revealed a significant association between AKI and a larger drop in hemoglobin value from baseline (2.7 vs. 1.4 g/dL; p = 0.003), a lower hemoglobin value at admission (6.4 vs. 7.5 g/dL; p = 0.03), and an increased white blood cell count at admission (33.1 vs. 19.8 × 109/L; p < 0.0001), respectively. AKI (p < 0.0001) together with need for advanced respiratory support (biphasic positive airway pressure or mechanical ventilation) (p < 0.0001) and need for exchange transfusion (p < 0.0001) were associated with prolonged hospitalization.
Conclusions
Clinicians should monitor pediatric patients hospitalized for ACS for the development of AKI as a potentially modifiable risk factor for prolonged hospitalization.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Forty percent of adults with sickle cell disease (SCD) develop chronic kidney disease (CKD) and 15–30 % of deaths in patients with SCD are related to kidney disease [1–5]. Children with SCD develop hyposthenuria, hyperfiltration, and microalbuminuria [6–10]. Consequently, the early identification of risk factors and early initiation of therapies to mitigate disease progression could have significant long-term impact. A growing body of evidence shows that acute kidney injury (AKI) contributes to CKD in other patient populations [11]. Thus, an understanding of the prevalence of AKI during SCD events is paramount to improved care.
While the role of AKI in the development of CKD has become illuminated in other diseases, little research has focused on elucidating the role of AKI in SCD nephropathy [12–15]. To our knowledge, only one study to date has evaluated the incidence of AKI during SCD crisis, and based on the results, the authors suggested that 7–13 % of adult SCD patients hospitalized with acute chest syndrome (ACS) develop AKI [16]. However, this retrospective study is limited by the lack of an appropriate evaluation of serum creatinine (SCr) values, as the authors only looked at the day 1 SCr level (compared to prior baseline) to diagnose AKI [16]. In addition, patients in this adult cohort [16], as compared to a pediatric cohort, may have had underlying CKD which could influence the development of AKI during the acute setting. There are several potential risk factors for developing AKI during ACS. SCD is characterized by acute hemolytic/anemic events, ischemia/reperfusion episodes, hypoxia, and inflammation that may worsen during ACS. The risk of AKI may also be exacerbated by use of nephrotoxic agents (vancomycin and ketorolac) and concern for dehydration (poor oral intake during crisis and hyposthenuria).
To better understand the link between admission for ACS and AKI, we conducted a 6-year retrospective cohort study of pediatric patients admitted with ACS to our medical institution to determine the prevalence of AKI. We hypothesized that AKI is prevalent during ACS events and leads to prolonged hospital length of stay (LOS).
Methods
We conducted an institutional review board-approved 6-year retrospective cohort study of all pediatric SCD patients admitted to Children’s of Alabama with an ICD-9 code of ACS (517.3) as a primary or secondary diagnosis with the aims to determine the prevalence of AKI, identify potential risk factors for AKI at admission, and evaluate the association between AKI and hospital LOS. We excluded patients with an ICD-9 code of ACS (517.3) who did not have an identifiable pulmonary infiltrate on chest X-ray during their hospitalization or who were hospitalized for <24 h. AKI was defined by the Kidney Disease Improving Global Outcomes (KDIGO) definition of either a ≥0.3 mg/dL or 50 % increase in SCr from baseline [17]. Per institutional standard of care, patients with fever and pulmonary infiltrates (ACS) are treated with vancomycin, azithromycin, and ceftriaxone in the emergency room and can receive non-steroidal inflammatory medications (ibuprofen or ketorolac) as needed for pain or fevers [18]. After admission of the patient for ACS, individual attending physicians can determine whether they will discontinue vancomycin based on the initial clinical evaluation, wait for the 48-h cultures to be negative, or continue vancomycin until the patient is clinically stable. The type (simple or exchange) and timing of transfusion to the SCD patient is determined by the preferences of attending physician rather than by institutional protocol.
We conducted a chart review of patients diagnosed with ACS to determine the sickle cell genotype, age of patient, current SCD modifying therapy, results of the most recent outpatient (within 1 year of admission) complete blood count [baseline: hemoglobin (Hb) value, white blood cell count (WBC), and platelet count], and SCr level. We also collected the emergency room and daily inpatient complete blood counts and SCr values for all patients during their hospitalization. We calculated the difference in Hb and SCr from baseline (last Hb or SCr measurement prior to admission and within 1 year) to their admission for Hb and SCr values in ACS. We identified any transfusion intervention during the hospitalization period, transfer to pediatric intensive care unit (ICU), need for enhanced respiratory support [biphasic positive airway pressure (BIPAP) or mechanical ventilation] and length of hospital stay. Two categorical variables were created to reflect the clinical severity for patients based on SCD genotype: severe SCD (HbSS, SB0 thalassemia, and SD) and mild SCD (HbSC and SB + thalassemia). Among patients with multiple ACS admissions, we included only data from their most recent hospital admission in the analysis.
Characteristics of patients by AKI status were summarized using descriptive statistics. Comparisons of these characteristics were performed using the t test for continuous variables and Fisher’s exact test for categorical variables. To determine variables associated with AKI, we performed nominal logistic regression with baseline, admission, and change in the following variables: Hb, WBC and platelets (as explanatory variables). Similarly, we performed nominal logistic regression for type of transfusion support using laboratory variables, namely, Hb (baseline, admission, and change in Hb), WBC, and platelets. Kaplan–Meier curves and log rank tests were used to separately investigate the association of length of hospital stay with development of AKI, need for exchange transfusion, and need for increase in respiratory support. As intubation by itself can increase LOS, we stratified the association of LOS and AKI by need for increased respiratory support (BIPAP or intubation). All analyses were conducted using JMP Pro version 10 software (SAS Inc., Cary, NC).
Results
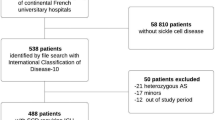
We identified 236 episodes with ACS codes in 163 patients admitted for hospitalization during a 6-year period. As only the most recent episode of ACS was included in the analysis, we excluded 73 episodes of ACS as they were repeat episodes of ACS in the same patient. Of the 163 unique patients with ACS, we excluded 14 patients due to an inability to determine AKI during admission because these patients did not have baseline SCr data for the preceding year. Among the 149 eligible patients, the mean SCr at baseline was 0.4 mg/dL [standard deviation (SD) 0.1] and the mean maximum serum creatinine during hospitalization was 0.5 mg/dL (SD 0.1). The mean age of patients admitted with ACS was 9.5 years (SD 4.8), and 64 % were male. Genotypes included 119 patients (80 %) with HbSS, seven patients (5 %) with HbSB0 thalassemia, eight patients (5 %) with HbSB + thalassemia, 14 patients (9 %) with HbSC, and one patient (1 %) with HbSD. Four patients (2 %) were on chronic transfusion at the time of ACS, 50 patients (32 %) were on hydroxyurea, and 95 patients (66 %) received no disease-modifying therapy. Twenty eight patients were admitted or transferred to the ICU of which 22 required >1 day in the ICU. Eleven patients (7 %) required mechanical ventilation and two were escalated to BIPAP (1 %) but not intubated. Thirty-three patients (22 %) required red cell exchange therapy, 102 patients (69 %) required simple transfusion, and 14 patients (9 %) were not transfused.
Table 1 summarizes the characteristics of the patients by AKI status as defined by KDIGO. AKI was identified in 12 of 149 (8 %) episodes of ACS over the 6-year study period. Compared to children without AKI, those patients with AKI had a larger drop in hemoglobin (2.7 vs. 1.4 g/dL; p = 0.003), lower Hb at admission (6.4 vs. 7.5 g/dL; p = 0.03), and higher WBC count at admission (33.1 vs. 19.8 × 103/L; p < 0.0001). The groups were similar for age, gender, and platelet count. We identified ten episodes of AKI in 127 cases of ACS for patients with severe SCD phenotypes and two episodes of AKI in 22 cases of ACS for patients with milder SCD phenotypes. No significant differences in the development of AKI were identified by genotype (p = 0.8). Among the 149 defined cases, two of the 50 patient cases (4 %) on hydroxyurea developed AKI, none of the four (0 %) on transfusion developed AKI, and ten of the 95 (11 %) receiving no disease-modifying therapy developed AKI. No differences in the development of AKI were identified by current SCD therapy (p = 0.3).
Nominal logistic regression revealed that compared to baseline values, a drop in Hb and WBC count at admission and in (g/dL; ×103/L) were associated with AKI (p values = 0.01 and 0.0007, respectively). The estimated odds ratios were 1.81 [95 % confidence interval (CI) 1.17–2.92] for change in Hb (g/dL) at admission and 1.10 (95 % CI 1.05–1.18) for WBC count (×103/L) at admission. The majority of patients developed AKI within 2 days of admission, with resolution at a median of 2 (range 1–7) days. The median hospitalization LOS for all patients was 4 (range 2–35) days, and the median and mean hospitalization LOS was significantly longer among patients who developed AKI (p < 0.0001) (Fig. 1a). In addition, the median and mean hospitalization LOS was significantly longer among patients who required exchange transfusion (p < 0.0001) (Fig. 1b) and in patients who required increased respiratory support (either intubation or BIPAP; p < 0.0001) (Fig. 1c). As increased respiratory support (intubation) was an expected strong predictor of LOS, additional analysis on AKI and LOS was performed with stratification by need for increased respiratory support. Among those who were intubated or required BIPAP, the development of AKI was still significantly associated with LOS (p = 0.02). (Fig. 1d)
Length of hospital stay for patients admitted with acute chest syndrome. a. Total length of hospital stay (LOS) by acute kidney injury (AKI), b total LOS by type of transfusion [no transfusion (None), simple red blood cell (RBC) transfusion (Simple), RBC pheresis (Pheresis)], c total LOS by type of respiratory support [intubation or biphasic positive airway pressure (BIPAP)] vs. no increase in respiratory support, d total LOS by acute kidney injury (AKI) among patients who required intubation or BIPAP. CI Confidence interval
Discussion
This research shows that a subset of pediatric patients with SCD who were admitted to our medical institution for ACS developed AKI during hospitalization. These results suggest that clinicians should monitor for this complication with daily SCr monitoring during admission for ACS as it could alter management strategies. At our institution, nephrotoxic agents are often administered to patients with severe ACS and fever (vancomycin and ibuprofen) or pain (ketorolac) that could potentiate kidney injury [18]. As protection against pneumococcus from vaccination improves and resistance to third-generation cephalosporin stays limited, institutional policies and individual clinicians should consider the option of withholding vancomycin or of discontinuing therapy with this agent early when treating presumed resistant pneumococcus as a rare pathogen for ACS and, alternatively, consider less aggressive strategies to manage fever with ibuprofen or ketorolac in patients that develop AKI [19].
One variable identified as a strong risk factor for developing AKI was an acute drop in Hb. For every 1 unit drop in Hb from baseline to admission, the odds of AKI is estimated to increase by about 81 % While prior research has identified severe anemia at baseline as a risk factor for overall disease severity in pediatric SCD, clinicians should also consider an acute drop in Hb from baseline as a risk factor for kidney injury during hospitalization [20, 21]. Patients with an acute and sustained drop in Hb during hospitalization are at risk for complicated ICU admissions, stroke, and ischemic brain injury, and now AKI [22–26]. Potential mechanisms linking an acute anemic event and AKI include renal ischemia from reduced oxygen carriage or acute increases in plasma free heme/Hb from hemolysis, producing direct kidney injury [27, 28]. Future prospective studies should evaluate the relationship between anemia and kidney injury in patients with SCD.
Prior studies of hydroxyurea in pediatrics have suggested a protective effect on progressive sickle cell nephropathy in children with SCD, yet the role of hydroxyurea in preventing AKI has not been explored [6, 29]. While hydroxyurea can prevent admissions for ACS, we were unable to demonstrate that patients prescribed hydroxyurea had statistically lower rates of AKI (2 of 50 cases of AKI) as compared to patients not on disease-modifying therapy (10 of 95 cases of AKI) [8]. One prior study evaluating the role of hydroxyurea in preventing kidney injury suggests that at steady state, hydroxyurea reduced biomarkers of inflammation and oxidative stress in the kidney [30]. The lack of a statistical advantage for hydroxyurea against AKI may reflect an underpowered retrospective study, poor adherence to hydroxyurea among those patients admitted with ACS, issues inherent in defining AKI by SCr in SCD, or lack of efficacy of hydroxyurea to prevent AKI.
An additional finding suggests that the development of AKI may contribute to possible prolonged hospitalization. The length of hospitalization for ACS frequently results from the time required to discontinue supplemental oxygenation. Recent research in bi-directional organ cross-talk during critical illness offers insight into the association between AKI and acute lung injury. Hypoxemia and acute lung injury due to respiratory failure lead to a decrease in renal blood flow and is a risk factor for AKI [31, 32]. Understanding the pathophysiology of ACS in the context of AKI could explain part of the severity of this disease and the prolonged need for respiratory support.
The strengths of this study are the use of the most contemporary definition of AKI, clear SCD phenotypes, including standard therapy, and the availability of baseline SCr values for most of the children. Despite these strengths, we acknowledge several limitations to this study by its nature of being a retrospective study. As some patients in this study were seen at satellite sickle cell clinics, a baseline SCr was not performed on all patients admitted to our hospital. Similarly, all laboratory data and clinical records were reviewed from Children’s of Alabama electronic medical records; therefore, patients admitted and transferred from an outside emergency room or hospital may have had additional SCr values that we did not evaluate. As some patients in this study did not have daily SCr measurements, it is possible that a few cases of AKI may not have been appropriately captured. Strict urine output was not calculated in most patients, and our definition only uses SCr-based criteria. An inherent concern in AKI reporting in SCD is that SCr may not accurately reflect the estimated glomerular filtration rate. Despite the concern that SCD patients may have a lower SCr value, this study utilized the contemporary definition of AKI which incorporates a change in SCr from baseline. Large multi-center studies will be needed to determine if this current definition of AKI predicts short- and long-term outcomes. . A limitation affecting the generalizability of these findings to other institutions is the inclusion of vancomycin at diagnosis of ACS. The only adult study for which data are available identified a similar incidence of AKI (7 % in moderate ACS and 14 % in severe ACS), but the authors did not report their antibiotic regimen for ACS. Finally, as we evaluated the most recent admission for patients with ACS in a single center, we identified 12 cases of AKI among 149 unique patients admitted over a 6-year period. As not all patients with HbSS and SB0 thalassemia develop ACS, this study is limited by a small sample size of patients that developed AKI. Future studies that could better delineate risk factors and outcomes of AKI require a larger, multi-center study.
In conclusion, AKI occurs during hospitalization for ACS, and the role of AKI in progression to SCD nephropathy needs further evaluation. We suggest that clinicians monitor for the risk factors of AKI that we identified, namely, acute decline in Hb concentration and leukocytosis, and consider modifying empiric therapy for ACS by limiting nephrotoxic agents and optimizing fluid balance. We are currently conducting a long-term prospective study for all SCD patients admitted with ACS to better define AKI and evaluate potential mechanistic links between ACS, AKI, and progression to CKD. With early detection of AKI, better methods for identifying AKI, and modifications to present-day therapy for patients with AKI, we hope to improve outcomes in sickle cell nephropathy.
References
Hamideh D, Alvarez O (2013) Sickle cell disease related mortality in the United States (1999–2009). Pediatr Blood Cancer 60:1482–1486
Powars DR, Chan LS, Hiti A, Ramicone E, Johnson C (2005) Outcome of sickle cell anemia: a 4-decade observational study of 1056 patients. Medicine (Baltimore) 84:363–376
Gosmanova EO, Zaidi S, Wan JY, Adams-Graves PE (2014) Prevalence and progression of chronic kidney disease in adult patients with sickle cell disease. J Investig Med 62:804–807
McClellan AC, Luthi JC, Lynch JR, Soucie JM, Kulkarni R, Guasch A, Huff ED, Gilbertson D, McClellan WM, DeBaun MR (2012) High one year mortality in adults with sickle cell disease and end-stage renal disease. Br J Haematol 159:360–367
Powars DR, Elliott-Mills DD, Chan L, Niland J, Hiti AL, Opas LM, Johnson C (1991) Chronic renal failure in sickle cell disease: risk factors, clinical course, and mortality. Ann Intern Med 115:614–620
Lebensburger J, Johnson SM, Askenazi DJ, Rozario NL, Howard TH, Hilliard LM (2011) Protective role of hemoglobin and fetal hemoglobin in early kidney disease for children with sickle cell anemia. Am J Hematol 86:430–432
Miller ST, Wang WC, Iyer R, Rana S, Lane P, Ware RE, Li D, Rees RC, Investigators B-H (2010) Urine concentrating ability in infants with sickle cell disease: baseline data from the phase III trial of hydroxyurea (BABY HUG). Pediatr Blood Cancer 54:265–268
Wang WC, Ware RE, Miller ST, Iyer RV, Casella JF, Minniti CP, Rana S, Thornburg CD, Rogers ZR, Kalpatthi RV, Barredo JC, Brown RC, Sarnaik SA, Howard TH, Wynn LW, Kutlar A, Armstrong FD, Files BA, Goldsmith JC, Waclawiw MA, Huang X, Thompson BW, Investigators BH (2011) Hydroxycarbamide in very young children with sickle-cell anaemia: a multicentre, randomised, controlled trial (BABY HUG). Lancet 377:1663–1672
Statius van Eps LW, Pinedo-Veels C, de Vries GH, de Koning J (1970) Nature of concentrating defect in sickle-cell nephropathy. Microradioangiographic studies. Lancet 1:450–452
Aygun B, Mortier NA, Smeltzer MP, Hankins JS, Ware RE (2011) Glomerular hyperfiltration and albuminuria in children with sickle cell anemia. Pediatr Nephrol 26:1285–1290
Chawla LS, Eggers PW, Star RA, Kimmel PL (2014) Acute kidney injury and chronic kidney disease as interconnected syndromes. N Engl J Med 371:58–66
Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Ronco C, Beginning, Ending Supportive Therapy for the Kidney I (2005) Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA 294:813–818
Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW (2005) Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol 16:3365–3370
Chawla LS, Amdur RL, Amodeo S, Kimmel PL, Palant CE (2011) The severity of acute kidney injury predicts progression to chronic kidney disease. Kidney Int 79:1361–1369
Schneider J, Khemani R, Grushkin C, Bart R (2010) Serum creatinine as stratified in the RIFLE score for acute kidney injury is associated with mortality and length of stay for children in the pediatric intensive care unit. Crit Care Med 38:933–939
Audard V, Homs S, Habibi A, Galacteros F, Bartolucci P, Godeau B, Renaud B, Levy Y, Grimbert P, Lang P, Brun-Buisson C, Brochard L, Schortgen F, Maitre B, Mekontso Dessap A (2010) Acute kidney injury in sickle patients with painful crisis or acute chest syndrome and its relation to pulmonary hypertension. Nephrol Dial Transplant 25:2524–2529
Kidney Diseases: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group (2012). KDIGO clinical practice guidelines for acute kidney Injury. Kidney Int Suppl 2:1–138
Miller ST (2011) How I treat acute chest syndrome in children with sickle cell disease. Blood 117:5297–5305
De Montalembert M, Abboud MR, Fiquet A, Inati A, Lebensburger JD, Kaddah N, Mokhtar G, Piga A, Halasa N, Inusa B, Rees DC, Heath PT, Telfer P, Driscoll C, Al Hajjar S, Tozzi A, Jiang Q, Emini EA, Gruber WC, Gurtman A, Scott DA (2015) 13-valent pneumococcal conjugate vaccine (PCV13) is immunogenic and safe in children 6–17 years of age with sickle cell disease previously vaccinated with 23-valent pneumococcal polysaccharide vaccine (PPSV23): results of a phase 3 study. Pediatr Blood Cancer 62:1427–1436
Meier ER, Wright EC, Miller JL (2014) Reticulocytosis and anemia are associated with an increased risk of death and stroke in the newborn cohort of the Cooperative Study of Sickle Cell Disease. Am J Hematol 89:904–906
Lebensburger JD, Miller ST, Howard TH, Casella JF, Brown RC, Lu M, Iyer RV, Sarnaik S, Rogers ZR, Wang WC, Investigators BH (2012) Influence of severity of anemia on clinical findings in infants with sickle cell anemia: analyses from the BABY HUG study. Pediatr Blood Cancer 59:675–678
Dowling MM, Quinn CT, Plumb P, Rogers ZR, Rollins NK, Koral K, Buchanan GR (2012) Acute silent cerebral ischemia and infarction during acute anemia in children with and without sickle cell disease. Blood 120:3891–3897
Dowling MM, Quinn CT, Rogers ZR, Buchanan GR (2010) Acute silent cerebral infarction in children with sickle cell anemia. Pediatr Blood Cancer 54:461–464
Cecchini J, Lionnet F, Djibre M, Parrot A, Stojanovic KS, Girot R, Fartoukh M (2014) Outcomes of adult patients with sickle cell disease admitted to the ICU: a case series*. Crit Care Med 42:1629–1639
Bernaudin F, Verlhac S, Arnaud C, Kamdem A, Vasile M, Kasbi F, Hau I, Madhi F, Fourmaux C, Biscardi S, Epaud R, Pondarre C (2015) Chronic and acute anemia and extracranial internal carotid stenosis are risk factors for silent cerebral infarcts in sickle cell anemia. Blood 125:1653–1661
Wierenga KJ, Serjeant BE, Serjeant GR (2001) Cerebrovascular complications and parvovirus infection in homozygous sickle cell disease. J Pediatr 139:438–442
Tracz MJ, Alam J, Nath KA (2007) Physiology and pathophysiology of heme: implications for kidney disease. J Am Soc Nephrol 18:414–420
Nath KA, Grande JP, Haggard JJ, Croatt AJ, Katusic ZS, Solovey A, Hebbel RP (2001) Oxidative stress and induction of heme oxygenase-1 in the kidney in sickle cell disease. Am J Pathol 158:893–903
Aygun B, Mortier NA, Smeltzer MP, Shulkin BL, Hankins JS, Ware RE (2013) Hydroxyurea treatment decreases glomerular hyperfiltration in children with sickle cell anemia. Am J Hematol 88:116–119
dos Santos TE, Goncalves RP, Barbosa MC, da Silva GB, Daher EF Jr (2015) Monocyte chemoatractant protein-1: a potential biomarker of renal lesion and its relation with oxidative status in sickle cell disease. Blood Cells Mol Dis 54:297–301
Kilburn KH, Dowell AR (1971) Renal function in respiratory failure. Effects of hypoxia, hyperoxia, and hypercapnia. Arch Intern Med 127:754–762
Basu RK, Wheeler DS (2013) Kidney-lung cross-talk and acute kidney injury. Pediatr Nephrol 28:2239–2248
Acknowledgments
J.L would like to acknowledge the NIH (1K23HL127100-01) and American Society of Hematology Scholar Award for funding an ongoing cohort to study progression to CKD. The authors would like to thank the participants living with sickle cell disease as we strive to improve their care. The authors would also like to thank the additional members of the UAB Pediatric Sickle Cell team (Lee Hilliard, MD, Christina Bemrich-Stolz, MD, MSPH, Kristen Osborn CRNP, Susan Dobbins, CRNP, Heather Carlton, CRNP, Michelle McCall CRNP, and the SCD clinic nurses) for providing excellent care. The authors thank the UAB Pediatric Research office for their helpful resources and the Pediatric and Infant Center for Acute Nephrology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to disclose
Rights and permissions
About this article
Cite this article
Lebensburger, J.D., Palabindela, P., Howard, T.H. et al. Prevalence of acute kidney injury during pediatric admissions for acute chest syndrome. Pediatr Nephrol 31, 1363–1368 (2016). https://doi.org/10.1007/s00467-016-3370-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-016-3370-0