Abstract
Background
Iron deficiency anemia (IDA) is the most common nutritional deficiency in the world. The aim of our study was to evaluate and compare renal functional and structural integrity in 50 infants with IDA and 50 healthy controls and to assess the relation between IDA and oxidative stress and response to iron therapy.
Methods
This was a prospective study in which peripheral blood samples were collected from all study subjects and the following laboratory investigations performed: serum iron profile, urinary microalbumin, urinary leucine aminopeptidase (LAP), fractional excretion of sodium (FeNa), serum total antioxidant capacity (TAC), serum malondialdehyde (MDA), serum and urinary trace elements (iron, copper, zinc, calcium and magnesium). All patients received oral iron therapy and were followed-up for 3 months.
Results
The levels of baseline urinary markers were higher among the patients with IDA than among the controls (p < 0.05). Patients had a lower pre-therapy TAC and lower serum zinc and magnesium levels than controls as well as higher MDA and serum copper levels (p < 0.05). MDA level was positively correlated to microalbumin and LAP level (p < 0.05). Urinary LAP concentration was positively correlated to urinary trace element concentrations (p < 0.05). A significant decrease in microalbumin, LAP, FeNa, and urinary trace elements was observed post-iron therapy while hemoglobin and ferritin levels were increased (p < 0.05).
Conclusion
Among the study subjects, IDA had an adverse influence on renal functional and structural integrity which could be reversed with iron therapy. Oxidative stress played an important role in the pathogenesis of renal injury in IDA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Iron is a trace element required by most living organisms and is essential for multiple metabolic processes, including oxygen transport, DNA synthesis, and electron transport [1]. Iron deficiency anemia (IDA) is one of the most common nutritional problems in the world, especially in developing countries. Infants aged between 4 and 24 months are among the population groups most affected by iron deficiency [2].
It has been suggested that children with IDA undergo various changes in renal function and structure [1]. At the present time specific markers for different portions of the nephron are used to diagnose injury of the renal tubular and glomerular system. As such, urinary excretion of high-molecular-weight proteins, especially albumin and immunoglobulin G, is the best marker of glomerular dysfunction [3], and the brush border membrane enzyme leucine-aminopeptidase (LAP) is recommended as a marker of structural integrity of renal proximal tubules [4]. The fractional excretion of sodium (FeNa) describes the fraction of the filtered load of Na that is excreted in the final urine and is a reflection of tubular function [5].
The role of trace elements in metabolic processes and their importance in human health and diseases has led many researchers to study the status of these elements in normal and pathological conditions, including renal diseases [6]. Copper acts as a cofactor for oxidative metalloenzymes, including lysyl oxidase, cytochrome c oxidase, and superoxide dismutase (SOD) [7]. Zinc is known to be an essential element involved in the structure of about 120 enzymes, such as DNA polymerase, reverse transcriptase, and RNA polymerase [8].
The mammalian erythrocyte functions as an oxygen transporter and is therefore permanently in danger of oxidative damage. In order to avert this threat, the erythrocyte is well equipped with antioxidants and antioxidative enzymes [9–11]. Epidemiological and clinical studies suggest a possible correlation between antioxidant levels and the risk for anemic diseases [12].
Accumulating evidence suggests that oxidative stress plays an important role in the pathogenesis and progression of several renal diseases [13–15]. Therefore, we assessed renal functional and structural integrity in infants with IDA before and after oral iron therapy and tested the validity of a hypothesis linking oxidative stress among those children to glomerular and tubular dysfunction.
Materials and methods
This prospective study included 50 infants with IDA (38 males, 12 females; male-to-female ratio 3.2:1) recruited from the Children’s Hospital, Ain Shams University and 50 age- and sex-matched healthy subjects as controls. The control group was recruited from infants who visited the outpatient clinic for obligatory vaccination and consisted of 36 males and 14 females, with male to female ratio of 2.6:1. The mean age of the IDA patients anc controls was 1.3 ± 0.41 years (range 6 months to 2 years) and 1.4 ± 0.44 years (range 8 months to 2 years), respectively. Informed consent was obtained from the legal guardian of each patient or control before enrollment in the study. The procedures applied in this study were approved by the Ethical Committee of Human Experimentation of Ain Shams University and are in accordance with the Helsinki Declaration of 1975.
We diagnosed IDA in infants aged <2 years based on serum iron concentration of <40 μg/dL, transferrin saturation of <20 %, and serum ferritin concentration of <100 ng/mL [16, 17]. Exclusion criteria were history of any disorder likely to impair renal functions, urinary tract infection, history of cardiovascular diseases, inflammatory or infectious diseases, cancer, and diabetes mellitus which may induce oxidative stress. Patients with a previous or present exposure to agents with potential nephrotoxicity or who received iron treatment in the last 3 months were also excluded.
Sample collection
For the complete blood count (CBC), peripheral blood samples were collected in sterile Vacutainer tubes containing potassium ethylenediaminetetraacetic acid (K2-EDTA; Beckton Dickinson, Franklin Lakes, NJ) to a final concentration of 1.5 mg/mL. For the chemical analysis and determination of the iron profile, total antioxidant capacity (TAC) and malondialdehyde (MDA) level, blood samples were obtained and clotted and the serum separated by centrifugation for 15 min at 1000 g. Spot morning urine samples were collected using a Japan style Alpk2 collection bag placed over the infant’s external genitalia or polyethylene containers, with centrifugation at for 5 min at 1000 g. The top 15 mL of the supernatant was collected and placed into polyethylene tubes and kept frozen at −20 °C without preservatives until analysis.
Laboratory assessment
Laboratory investigations included CBC (Sysmex XT-1800i; Sysmex, Kobe, Japan), the measurement of serum creatinine and serum Na concentrations (Cobas Integra 800 analyzer; Roche Diagnostics, Mannheim, Germany), determination of the iron profile (Cobas Integra 800 CTS analyzer, Roche Diagnostics) based on the calculation of transferrin saturation, and hemoglobin analysis by high-performance liquid chromatography (D-10; BioRad, Hercules, CA) to exclude other causes of microcytic anemia. Morning urine samples were collected for the measurement of urinary Na and creatinine levels (Beckman synchron X9; Beckman Coulter, Inc., Brea, CA), the calculation of the FeNa, urinary albumin excretion (Cobas Integra 800; Roche Diagnostics), urinary LAP level (commercial kit from Randox Laboratories, Belfast, UK) and quantitative determination of serum and urinary iron, copper, zinc, calcium and magnesium concentrations (SOLAR System Unicam 939 atomic absorption spectrometer; Unicam, Cambridge, UK).
To assess oxidant–antioxidant status, TAC was measured using an assay kit supplied by Bio Diagnostic, Dokki, Giza, Egypt) and MDA level was determined by measuring the production of thiobarbituric acid reactive substances (TBARS) using a colorimetric kit (Bio Diagnostic) according to the manufacturer’s instructions.
Treatment protocol and follow-up
Patients with proven IDA were given oral iron therapy (Ferose®; SPIMACO, Al-Qassim Pharma, Saudi Arabia) at a dose of 6 mg/kg for 3 months to allow repletion of iron stores based on the IDA treatment guidelines [18, 19]. Clinical and laboratory follow-up was performed for all treated patients post-therapy with a focus on signs of anemia, infections, changes in hemoglobin level, and iron profile.
Statistical analysis
Data were analyzed using the Statistical Program for Social Science version 17 (IBM Corp., Armonk, NY). Quantitative variables were described as the mean and standard deviation or as the median and interquartile range (25th–75th percentiles). Qualitative variables were described as the number and percentage. The Student t-test was applied to compare parametric quantitative variables between the two groups, and the Mann–Whitney test was used to compare non-parametric quantitative variables between two groups. Qualitative variables were compared using the chi-square (X2) test or Fischer’s exact test when frequencies were <5. Correlation studies were performed using Spearman’s rank correlation coefficient. A p value of <0.05 was considered to be significant in all analyses.
Results
Compared to the healthy controls, the patients with IDA had significantly lower hemoglobin, red blood cell (RBC) indices, iron, ferritin, and transferrin saturation (p < 0.001) and higher white blood cell (p = 0.014) and platelet (p = 0.006) counts (Table 1). Pre-therapy levels of all urinary markers studied, including trace elements, were markedly increased among IDA patients compared to controls (p < 0.05) (Table 1). Patients with IDA had significantly lower pre-therapy TAC, serum zinc and magnesium levels than controls, while the serum copper and MDA levels and MDA:TAC ratio were significantly higher (p < 0.05) (Table 2).
Comparison of the pre- and post-iron therapy hematological parameters among the patients with IDA revealed a significant increase in hemoglobin (p = 0.001), mean corpuscular hemoglobin (p = 0.011), and ferritin levels (p = 0.005) post-iron therapy. Pre- and post-therapy levels of serum creatinine and serum Na were not significantly different among the patients and controls. Regarding the urinary markers, there was a significant decrease in urinary microalbumin (p = 0.048), LAP (p = 0.023), FeNa (p = 0.017), iron (p = 0.007), copper (p = 0.023), zinc (p = 0.006), and calcium (p = 0.042) post-iron therapy. The level of post-therapy urinary magnesium was lower than the baseline level, but the difference did not reach significance (p = 0.156) (Table 1). However, a significant difference was found when post-iron therapy levels of the studied hematological and urinary parameters were compared with those of the healthy controls, with the exception of TIBC, serum creatinine, serum Na, FeNa, and urinary calcium levels (Table 1). Moreover, TAC and MDA levels were significantly decreased post-iron therapy compared with their respective baseline levels, although they did not reach the levels of the controls (p < 0.001; Fig. 1).
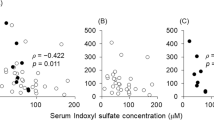
Significant positive relations were found between pre-therapy levels of TAC and hemoglobin (r = 0.668, p < 0.001) and between baseline MDA and iron levels (r = 0.993, p < 0.001), while baseline TAC and MDA (r = −0.989, p < 0.001) were negatively correlated. TAC was negatively correlated to the urinary zinc level (r = −0.429, p = 0.002), and MDA level was positively correlated to urinary microalbumin (r = 0.399, p = 0.004) and urinary LAP (r = 0.6476, p < 0.001) levels (Fig. 2). Baseline urinary LAP was positively correlated to urinary microalbumin (r = 0.437, p = 0.025) and to the studied urinary trace elements (p < 0.001 for all) (Fig. 3). Urinary copper levels were positively correlated to urinary microalbumin (r = 0.437, p = 0.029), while urinary magnesium levels were positively correlated to FeNa (r = 0.426, p = 0.034) (Fig. 3). Moreover, significant positive correlations were observed between urinary trace elements and each other (p < 0.001 for all).
Discussion
Iron deficiency anemia is a major public health problem in developing countries, especially in Egypt [20, 21]. Iron deficiency is known to have serious adverse effects on the cardiovascular and nervous systems [22, 23], but relatively fewer studies have focused on the effect of IDA on renal functions. To investigate whether IDA has negative impacts on the structural and functional integrity of renal tubules and glomeruli, we estimated different urinary parameters, including trace elements.
We found a significant increase in the baseline urinary microalbumin level among patients in the IDA group compared with the controls, implying glomerular injury in the former. These results are in agreement with those of Walter et al. [24] who reported that IDA leads to decreased glomerular density and surface area and promotes fibrosis. We also found an increased urinary LAP level among IDA patients and a positive correlation between LAP and urinary microalbumin levels. These findings indicate the presence of structural damage of proximal tubules and suggest nephrotoxicity [25] as well as simultaneous injury to the renal glomeruli. In an earlier study, Özçay et al. [1] examined renal proximal tubule damage in children with IDA using a different panel of enzymes and proteins from that used in our study. These authors reported that there was a significant elevation in urinary excretion of both N-acetyl glucosamine and a low-molecular-weight protein (β2 microglobulin).
We also assessed the functional integrity of renal tubules using FeNa and found this marker to be higher in infants with IDA than in healthy controls and to be positively correlated to urinary magnesium level. This result is in line with those reported elsewhere [1]. Compared to our controls, the IDA patients included in our study had markedly elevated pre-therapy urinary levels of iron, copper, zinc, calcium, and magnesium, with significant positive correlations between each other, most probably due to similar excretion sites in the kidney.
Several potential mechanisms may be involved in the increased loss of copper and zinc in the urine of IDA patients. First, increased glomerular permeability can lead to increased urinary excretion of zinc and copper–albumin complexes across the glomerulus, as reflected by the significant positive correlation between urinary microalbumin and urinary copper among our IDA patients. A positive relation between urinary copper and urinary β2-microglobulin level, another marker of glomerular structure, has been previously reported [26]. A second possible mechanism is tubular reabsorption failure secondary to tubular damage. The presence of proximal tubular structural damage among our IDA patients, as evidenced by increased urinary excretion of LAP and the significant positive correlation between LAP and the level of each of urinary zinc and copper, supports this possibility. Urinary levels of copper and zinc have been found to be correlated with both glomerular and tubular functional and structural parameters [27]. Thus, it would appear that both mechanisms may operate simultaneously in IDA, leading to the increased urinary excretion of zinc and copper which could serve as reliable markers for glomerular and proximal tubular alterations.
In the current analysis, the urinary iron level was significantly increased among IDA patients, probably secondary to glomerular leakage, and there was a significant correlation between urinary iron level and microalbumin. Swaminathan et al. [28] examined the link between urinary albumin, transferrin, and iron excretion in diabetic patients and reported an early increase in urinary iron excretion that was associated with the degree of proteinuria. These authors also observed a positive correlation between urinary iron and LAP levels, possibly due to the presence of iron transporters at the apical membrane of the proximal tubule [29]. Therefore, any damage to the proximal tubules can lead to increased urinary iron and LAP excretion.
The significant increase in calcium excretion among our IDA patients and its positive correlation with urinary LAP level may suggest defective reabsorptive properties of proximal tubular cells. In this context, El-Safty et al. [30] reported increased urinary excretion of calcium among workmen exposed to mercury vapor and positive correlations with other studied markers of proximal tubules.
The increased urinary magnesium level in the studied infants with IDA could be explained by the strong relationship between the renal handling mechanisms of both urinary magnesium and calcium. Another possible explanation is the presence of renal tubulopathy in our IDA patients, as evidenced by increased FeNa and urinary LAP levels, leading to decreased tubular reabsorption of magnesium and to renal magnesium wasting. The positive correlation between urinary magnesium level and FeNa as well as urinary LAP level further supports the aforementioned explanation.
In the context of oxidant–antioxidant status in the studied IDA patients, we observed high MDA levels, which is a measure of lipid peroxide, and low TAC levels, with significant relations between MDA and both iron and hemoglobin. In addition, serum zinc and magnesium levels were decreased in IDA patients while serum copper level was increased. The suicidal death of RBCs occurs in iron deficiency. This process results in a vicious cycle of iron liberation, which in turn leads to an increased potential for oxidative stress, which then results in increased membrane stiffness and decreased deformability. Furthermore, with fewer RBCs and less hemoglobin available, the consumption of oxygen by the tissues lowers the partial pressure of oxygen. The resultant hypoxia and the associated decrease in the oxygenation of RBC hemoglobin increase the rate of hemoglobin autoxidation generating methemoglobin and superoxide [31].
Similar to our results, increased parameters of oxidative stress, including MDA, in IDA have been reported in several studies [32–35]. Deokar et al. [36] recently reported a significant increase in MDA in association with decreased antioxidants, SOD, vitamin C, vitamin E, and zinc in patients with IDA. Other studies have also reported decreased TAC levels in IDA patients [37, 38]. This was attributed to an overproduction of free radicals which consume the antioxidant system and to the decrease in erythrocyte antioxidant enzymes [32]. Kocyigit et al. [39] found a negative correlation between TAC and MDA values, and Amirkhizi et al. [32] reported that plasma MDA was positively correlated with plasma iron and that plasma TAC was positively correlated with hemoglobin concentration and ferritin levels. We also found a significant positive correlation between indices of oxidative stress and urinary markers. This may be a cause–effect relationship in which oxidative stress led to glomerular and tubular injury with subsequent increases in the studied urinary markers. However, this hypothesis remains to be fully elucidated.
The effect of iron therapy on the studied hematological and urinary markers of our IDA patients was a significant post-therapy increase in hemoglobin and serum ferritin levels concomitantly with evident decreases in FeNa, urinary albumin, urinary LAP, and urinary trace elements. These results suggest that recovery of both glomerular and tubular functions post-therapy could be achieved. We also found a significant improvement in the markers of oxidative stress after iron therapy. However, a longer follow-up duration may be needed for the studied markers to reach control levels. Sundaram et al. [35] reported a significant increase in iron, ferritin, and hemoglobin levels as well as a significant decrease MDA level in IDA patients after 1 month of treatment. Kurtoglu et al. [40] observed a significant decrease of oxidative stress after 6 weeks of iron supplementation relative to controls, with no significant differences between treated patients at 6 weeks and at the end of the study (at the time when body iron stores are saturated).
Akça et al. [41] investigated total oxidative stress (TOS) and TAC in 40 children with IDA aged 6 to 60 months who were treated with oral iron for 2 months. Prior to initiating the iron treatment, the TAC level was similar between patients and controls while TOS was significantly higher in the IDA group; the latter decreased after treatment. These authors did not find any correlation between hemoglobin, serum iron, iron-binding capacity, ferritin levels, and TOS or TAC among IDA patients, leading them to conclude that oxidative stress increases in children with IDA and that this increase can be returned to normal levels by treatment.
To the best of our knowledge the effect of iron therapy on renal tubular and glomerular integrity has not been widely described in the literature. Altun et al. [42] investigated the effects of iron deficiency on oxidative stress and renal tubular functions before and after treatment of children. After treatment, these levels decreased and this difference disappeared. In contrast to our results, their findings showed that treatment of iron deficiency did not have significant effect on proximal renal tubular functions; however, we examined both glomerular and tubular integrity using different markers including trace elements.
A short follow-up duration is the major limitation of our current study. Even though we found a significant improvement in hematological and urinary parameters in the post-therapy period, a longer follow-up may be needed for the levels to reach control values.
In conclusion, we suggest that IDA wields an adverse influence on renal functional and structural integrity. Increased MDA levels and decreased TAC, zinc, and magnesium levels in infants with IDA denote increased oxidative stress and depletion of antioxidant defense mechanisms. Adequate treatment of IDA is crucial to prevent the adverse effects of oxidative stress and could also protect against permanent glomerular and tubular damage. Urinary excretion of albumin, LAP, and trace elements in IDA could be used as potential biomarkers of renal dysfunction and for monitoring response to iron therapy. The underlying mechanism of renal injury in IDA may be multifactorial and represents an important area for future research. Further studies are needed to investigate concomitant nutritional deficiencies with IDA and their possible influence on renal structural and functional integrity.
References
Özçay F, Derbent M, Aldemir D, Türkoğlu S, Baskın E, Özbek N, Saatçi Ü (2003) Effect of iron deficiency anemia on renal tubular function in childhood. Pediatr Nephrol 18:254–256
Monajemzadeh SM, Zarkesh MR (2009) Iron deficiency anemia in infants aged 12–15 months in Ahwaz, Iran. Indian J Pathol Microbiol 52:182–184
Reiser J, von Gersdorff G, Simons M, Schwarz K, Faul C, Giardino L, Heider T, Loos M, Mundel P (2002) Novel concepts in understanding and management of glomerular proteinuria. Nephrol Dial Transplant 17:951–955
EL-Safty IA, Afifi AM, Shouman AE, EL-Sady AK (2004) Effects of smoking and lead exposure on proximal tubular integrity among Egyptian industrial workers. Arch Med Res 35:59–65
Koyner JL, Vaidya VS, Bennett MR, Ma Q, Worcester E, Akhter SA, Raman J, Jeevanandam V, O’Connor MF, Devarajan P, Bonventre JV, Murray PT (2010) Urinary biomarkers in the clinical prognosis and early detection of acute kidney injury. Clin J Am Soc Nephrol 5:2154–2165
Basaki M, Saeb M, Nazifi S, Shamsaei HA (2012) Zinc, copper, iron, and chromium concentrations in young patients with type 2 diabetes mellitus. Biol Trace Elem Res 148:161–164
Burjonrappa SC, Miller M (2012) Role of trace elements in parenteral nutrition support of the surgical neonate. J Pediatr Surg 47:760–771
Jeejeebhoy K (2009) Zinc: an essential trace element for parenteral nutrition. Gastroenterology 137:S7–S12
Grzelak A, Kruszewski M, Macierzynska E, Piotrowski L, Pulaski L, Rychlik B, Bartosz G (2009) The effects of superoxide dismutase knockout on the oxidative stress parameters and survival of mouse erythrocytes. Cell Mol Biol Lett 14:23–34
Takami T, Sakaida I (2011) Iron regulation by hepatocytes and free radicals. J Clin Biochem Nutr 48:103–106
Samhan-Arias AK, Tyurina YY, Kagan VE (2011) Lipid antioxidants: free radical scavenging versus regulation of enzymatic lipid peroxidation. J Clin Biochem Nutr 48:91–95
Madhikarmi NL, Murthy KR (2014) Antioxidant enzymes and oxidative stress in the erythrocytes of iron deficiency anemic patients supplemented with vitamins. Iran Biomed J 18:82–87
Crawford A, Fassett RG, Coombes JS, Kunde DA, Ahuja KD, Robertson IK, Ball MJ, Geraghty DP (2011) Glutathione peroxidase, superoxide dismutase and catalase genotypes and activities and the progression of chronic kidney disease. Nephrol Dial Transplant 26:2806–2813
Ozbek E (2012) Induction of oxidative stress in kidney. Int J Nephrol 2012:465897
Suvakov S, Damjanovic T, Stefanovic A, Pekmezovic T, Savic-Radojevic A, Pljesa-Ercegovac M, Matic M, Djukic T, Coric V, Jakovljevic J, Ivanisevic J, Pljesa S, Jelic-Ivanovic Z, Mimic-Oka J, Dimkovic N, Simic T (2013) Glutathione S-transferase A1, M1, P1 and T1 null or low-activity genotypes are associated with enhanced oxidative damage among haemodialysis patients. Nephrol Dial Transplant 28:202–212
Brugnara C, Schiller B, Moran J (2006) Reticulocyte hemoglobin equivalent (Ret He) and assessment of iron-deficient states. Clin Lab Haematol 28:303–308
Miwa N, Akiba T, Kimata N, Hamaguchi Y, Arakawa Y, Tamura T, Nitta K, Tsuchiya K (2010) Usefulness of measuring reticulocyte hemoglobin equivalent in the management of haemodialysis patients with iron deficiency. Int J Lab Hematol 32:248–255
Goddard AF, James MW, McIntyre AS, Scott BB, British Society of Gastroenterology (2011) Guidelines for the management of iron deficiency anaemia. Gut 60:1309–1316
Short MW, Domagalski JE (2013) Iron deficiency anemia: evaluation and management. Am Fam Physician 87:98–104
Al Ghwass ME, Halawa EF, Sabry SM, Ahmed D (2015) Iron deficiency anemia in an Egyptian pediatric population: a cross-sectional study. Ann Afr Med 14:25–31
Elalfy MS, Hamdy AM, Abdel Maksoud SS, Abdel Megeed RI (2012) Pattern of milk feeding and family size as risk factors for iron deficiency anemia among poor Egyptian infants 6 to 24 months old. Nutr Res 32:93–99
Kabakus N, Ayar A, Yoldas TK, Ulvi H, Dogan Y, Yilmaz B, Kilic N (2002) Reversal of iron deficiency anemia-induced peripheral neuropathy by iron treatment in children with irondeficiency anemia. J Trop Pediatr 48:204–209
Hegde N, Rich MW, Gayomali C (2006) The cardiomyopathy of iron deficiency. Tex Heart Inst J 33:340–344
Walter PB, Knutson MD, Paler-Martinez A, Lee S, Xu Y, Viteri FE, Ames BN (2002) Iron deficiency and iron excess damage mitochondria and mitochondrial DNA in rats. Proc Natl Acad Sci USA 99:2264–2269
El-Safty IAM, Mohy El-Deen IE, El-Rasheed AH, El-Ashmawy MFM (2015) Renal effects of tramadol addiction and cannabinoid abuse. RJPBCS 6:1212–1218
Nakajima M, Kobayashi E, Suwazono Y, Uetani M, Oishi M, Inaba T, Kido T, Shaikh ZA, Nogawa K (2005) Excretion of urinary cadmium, copper, and zinc in cadmium-exposed and nonexposed subjects, with special reference to urinary excretion of beta2-microglobulin and metallothionein. Biol Trace Elem Res 108:17–31
EL-Safty IAM, Gadallah M, Shouman AE (2003) Effect of silica exposure on urinary excretion of copper and zinc. Am J Med Sci 326:122–127
Swaminathan S, Fonseca VA, Alam MG, Shah SV (2007) The role of iron in diabetes and its complications. Diabetes Care 30:1926–1933
Moulouel B, Houamel D, Delaby C, Tchernitchko D, Vaulont S, Letteron P, Thibaudeau O, Puy H, Gouya L, Beaumont C, Karim Z (2013) Hepcidin regulates intrarenal iron handling at the distal nephron. Kidney Int 84:756–766
El-Safty IA, Gadallah M, Shafik A, Shouman AE (2002) Effect of mercury vapour exposure on urinary excretion of calcium, zinc and copper: relationship to alterations in functional and structural integrity of the kidney. Toxicol Ind Health 18:377–388
Hebert PC, Van der Linden P, Biro G, Hu LQ (2004) Physiologic aspects of anemia. Crit Care Clin 20:187–212
Amirkhizi F, Siassi F, Minaie S, Djalali M, Rahimi M, Chamari M (2008) Assessment of lipid peroxidation and activities of erythrocyte cytoprotective enzymes in women with iron deficiency anemia. J Res Med Sci 13:248–254
Vives Corrons JL, Miguel-Garcia A, Pujades MA, Miguel-Sosa A, Cambiazzo S, Linares M, Dibarrart MT, Calvo MA (1995) Increased susceptibility of microcytic red blood cells to in vitro oxidative stress. Eur J Haematol 55:327–331
Tiwari AK, Mahdi AA, Zahra F, Chandyan S, Srivastava VK, Negi MP (2010) Evaluation of oxidative stress and antioxidant status in pregnant anemic women. Indian J Clin Biochem 25:411–418
Sundaram RC, Selvaraj N, Vijayan G, Bobby Z, Hamid A, Rattina Dasse N (2007) Increased plasma malondialdehyde and fructosamine in iron deficiency anemia: effect of treatment. Biomed Pharmacother 61:682–685
Deokar SA, Rai PSK, Bakshi AA, Rai AB (2013) Study of biochemical markers in iron deficiency anemia. Int J Res Med Sci 1:541–544
Madhikarmi NL, Murthy KR (2012) Enzymatic and non enzymatic antioxidant and lipid peroxidation status in iron deficiency. Int J Appl Biol Pharm Technol 3:130–136
Aslan M, Horoz M, Çelik H (2011) Evaluation of oxidative status in iron deficiency anemia through total antioxidant capacity using an automated method. Turk J Hematol 28:42–46
Kocyigit A, Armutcu F, Gurel A, Ermis B (2004) Alterations in plasma essential trace elements selenium, manganese, zinc, copper, and iron concentrations and the possible role of these elements on oxidative status in patients with childhood asthma. Biol Trace Elem Res 97:31–41
Kurtoglu E, Ugur A, Baltaci AK, Undar L (2003) Effect of supplementation on oxidative stress and antioxidant status in iron deficiency anemia. Biol Trace Elem Res 96:117–123
Akça H, Polat A, Koca C (2013) Determination of total oxidative stress and total antioxidant capacity before and after the treatment of iron-deficiency anemia. J Clin Lab Anal 27:227–230
Altun D, Kurekci AE, Gursel O, Hacihamdioglu DO, Kurt I, Aydin A, Ozcan O (2014) Malondialdehyde, antioxidant enzymes, and renal tubular functions in children with iron deficiency or iron-deficiency anemia. Biol Trace Elem Res 161:48–56
Financial disclosure
None.
Competing interest
None.
Contributors
All authors were involved in concept, design, data collection, analysis and drafting of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Mohamed S. El Shimi, Rania A. El-Farrash, Eman A. Ismail, Ibrahim A. El Safty, Ahmed S. Nada, Omayma A. El Gamel, Yomna M. Salem and Sara M. Shoukry contributed equally to this work.
Rights and permissions
About this article
Cite this article
El-Shimi, M.S., El-Farrash, R.A., Ismail, E.A. et al. Renal functional and structural integrity in infants with iron deficiency anemia: relation to oxidative stress and response to iron therapy. Pediatr Nephrol 30, 1835–1842 (2015). https://doi.org/10.1007/s00467-015-3122-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-015-3122-6