Abstract
We report the outcome of our single-center, long-term follow-up study of tacrolimus therapy in children with steroid-resistant nephrotic syndrome (SRNS). All cases of nephrotic syndrome (NS) with kidney biopsies treated at our center between January 2000 and July 2008 were reviewed. Children with systemic lupus erythematosus and steroid-dependent NS were excluded. Nineteen children with SRNS received tacrolimus. Histopathological analysis of the biopsy revealed the underlying conditions of these 19 patients to be focal segmental glomerulosclerosis (ten patients), C1q nephropathy (four), membranous nephropathy (two), minimal change disease (one), membranoproliferative glomerulonephritis (one), and immunoglobulin A nephropathy (one). The mean follow-up was 55 months, and the median age of the patient cohort was 10 years. We observed complete remission in 11 (58%) patients, partial remission in six (32%), and failure to respond in two (9%). The median time to response was 8 weeks. Side effects were mild and transient (one case of acute kidney injury and three cases of hyperglycemia). The initial rate for combined partial and complete remission of the NS in children with SRNS was 81%, which was sustained in 58% of the patients on follow-up. Among children with FSGS, the sustained remission rate was 50%, while 40% progressed to end-stage renal disease (ESRD) (mean time 52 months). Based on the results of this study, we conclude that tacrolimus is an effective and well-tolerated therapeutic option for the treatment of SRNS in children. However, the occurrence of relapses of the NS with progression to ESRD during the long-term follow-up indicates the need for careful monitoring of such patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nephrotic syndrome (NS) is the most common glomerulopathy encountered in pediatric practice.
In order to treat steroid-resistant nephrotic syndrome (SRNS), alternative regimes are required to delay the progressive renal damage incurred by the ongoing proteinuria. Proteinuria is an independent risk factor for the progressive renal failure and is usually monitored to determine the response to therapy and to predict prognosis [1, 2].
Tacrolimus, a recent addition to the armamentarium of therapies for managing SRNS, is a macrolide immunosuppressant that inhibits calcineurin and completely blocks the translocation of the cytosolic component of the nuclear factor of activated T cells (NF-AT). The genes regulated by the NF-AT transcription factor are necessary for T cell proliferation and prototypic T cell growth factor interleukin-2 (IL-2) [3]. Cyclosporine and tacrolimus have similar characteristics, but tacrolimus has been found to be more potent in both in vivo and in vitro studies. The severe cosmetic side effects of cyclosporine are absent with tacrolimus, making it a much better treatment option in young adolescents among whom compliance is a major concern.
There are only a few reports of treating SRNS in children with tacrolimus, the first being that published by McCauley et al. [4] in 1993 on seven patients (including four children) who exhibited a good response. The limited number of reports includes that of Li et al. [5] who, in an observational study, found that tacrolimus rapidly and effectively induced the remission of SRNS in Chinese adults with disease refractory to treatment with intravenous cyclophosphamide.
Recent pediatric experience has been encouraging, but limited by the short-term of the follow-ups in the respective studies [6–8]. Here, we report our long-term experience at a single center with tacrolimus therapy in pediatric patients with SRNS.
Subject and methods
Patient selection
The study design was that of a retrospective chart review of pediatric patients with SRNS who underwent a renal biopsy between January 2000 and July 2008. Of the 252 patient charts reviewed, 68 children with NS had undergone renal biopsies, of whom 26 had received tacrolimus. Kidney biopsy was performed in children who presented with NS at <15 months or >7 years of age or upon the diagnosis of SRNS. Four children with systemic lupus erythematosus (SLE) and three with steroid-dependent NS were excluded from this study. All 19 children included in this study were negative for Podocin and WT1 gene mutations (genetic testing was performed at the University of Michigan Medical Center—courtesy of Professor Friedhelm Hildebrandt).
All patients included in this study signed the study registry consent form approved by the institutional review board committee.
Definitions
- Nephrotic syndrome::
-
The presence of a constellation of signs and symptoms, including edema, hypoalbuminemia (serum albumin <3.0 g/dl), urine protein (mg/dl)/creatinine (mg/dl) (UP/Cr) >2, and hypercholesterolemia.
- Complete remission of NS::
-
UP/Cr < 0.2.
- Partial remission::
-
Persistent non-nephrotic range proteinuria (UP/Cr between 0.3 and 2.0) with a serum albumin ≥3.5 g/dl.
- Steroid resistant nephrotic syndrome::
-
No response after 6 weeks of therapy with 1 mg/kg twice daily of prednisone (maximum 30 mg twice daily).
- Hypertension::
-
Blood pressure >95th percentile for age, sex and height on three separate occasions [9].
- Primary tacrolimus resistance::
-
Persistence of nephrotic range proteinuria after 3 months of therapy.
- Secondary tacrolimus resistance::
-
Failure to respond to tacrolimus after an initial PR or CR with persistence of NS.
Estimated creatinine clearance was calculated by the Schwartz formula [10]. Urine protein/creatinine (UP/Cr) was calculated in first-morning urine specimens.
Treatment protocol for childhood NS
All patients received prednisone at a dose of 1 mg/kg twice daily for 6 weeks (maximum 60 mg/day) followed by rapid tapering over 6 weeks using an alternate-day regimen as steroid resistance was established. They also received angiotensin receptor blockers (ARBs) (losartan 25–100 mg/day) and/or angiotensin converting enzyme inhibitors (ACEi) (enalapril 2.5–40 mg/dose/day) as adjunctive agents. The doses of these medications were titrated to control the proteinuria and blood pressure. The renal function and serum potassium levels were closely monitored.
Prior to the initiation of tacrolimus therapy, eight children had received various medications without response. These included intravenous (IV) cyclophosphamide (500–750 mg/m2 monthly, three doses), mycophenolate mofetil (MMF; 1200 mg/m2/day in two divided doses orally, 3 months), cyclosporine (5 mg/kg/dose twice daily, 3 months), or rituximab (375 mg/m2 weekly IV, four doses).
Tacrolimus dose
The initial tacrolimus dose was 0.1 mg/kg twice daily; this was adjusted to keep a blood trough level in the range of 5–8 ng/ml with close monitoring of blood chemistries.
Tacrolimus withdrawal
After complete remission, tacrolimus was continued for at least 1 year and slowly tapered thereafter by 20% each month with close monitoring of proteinuria levels over a 6- to 9-month period. During the tapering phase, tacrolimus levels were kept <5 ng/ml by design. The tacrolimus dose was increased with relapse of NS or if proteinuria increased.
Results
A total of 19 children with SRNS were treated with tacrolimus therapy at our center between 2000 and 2008. The demographic characteristics and clinical presentation of these 19 patients with SRNS are given in Table 1.
The patient cohort consisted of eight boys and 11 girls and ranged in age at presentation from 1.6 to 18 years (median 10 years). There was a predominance of African Americans (14/19).
At presentation, all the patients were nephrotic as per the study entry criteria. The median UP/Cr at presentation was 7.4 ± 2.57 (range 3.5–12). Hypertension was noted in 6/19 (32%) patients, microscopic hematuria in 2/19 (11%) patients, and gross hematuria in 1/19 (5%) patients. All of the patients initially had a normal estimated glomerular filtration rate (GFR). The time from diagnosis to initiation of tacrolimus treatment varied from 6 weeks to 4 months (mean 2.2 months).
The follow-up time ranged from 17 months to 111 months (mean 55 months).
The diagnosis of these 19 children with SRNS based on the histopathologic findings was focal segmental glomerulosclerosis (FSGS; ten patients), C1q nephropathy (C1qN; four), idiopathic membranous nephropathy (MN; two), minimal change disease (MCD; one), membranoproliferative glomerulonephritis (MPGN; one), and IgA nephropathy (IgAN; one).
Response to tacrolimus therapy
The clinical data on the 19 children with SRNS treated with tacrolimus are given in Table 2. Five patients failed to respond to MMF (nos. 2, 3, 4, 15, 17), three failed to respond to cyclophosphamide (nos. 13, 16, 19), one failed to respond to rituximab (no. 13), and one failed to respond to cyclosporine (no. 9).
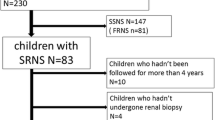
Figure 1 summarizes the response of the children to tacrolimus therapy during the study period. The initial and the follow-up status of the NS in these 19 children is represented.
Of the 19 patients treated with tacrolimus, 11 (58%) achieved complete remission, which occurred between 3 weeks to 3 months (median 8 weeks) of therapy. The initial combined rate of complete and partial remission was 89% (17/19).
One child was lost to follow-up after 5 months (no. 16). Among the remaining 18 patients, the overall rate of sustained partial or complete remission after tacrolimus therapy at the last follow-up visit was 55% (10/18); the remaining eight children were either initial non-responders (two), showed “secondary tacrolimus resistance” (two), or had progressed to ESRD (four). With the exception of the four children who developed ESRD, all children had maintained a normal estimated GFR at the time of the last visit. Eight of these are currently off all immunosuppressant medications.
The histopathology diagnosis for those children with complete remission was FSGS (four children), C1qN (two), MPGN (one), MN (one), and IgAN (one), for those children with partial remission, FSGS (five) and MN (one), and for those children who failed to respond to tacrolimus, MCD (one) and FSGS (one).
The average UP/Cr among those with partial remission after tacrolimus therapy was 1.3 (range 0.5–2.0). This represents an average decline in proteinuria of 82.5% compared to the proteinuria levels prior to tacrolimus therapy (p < 0.001).
All children with C1qN achieved remission despite steroid resistance. Two had relapse of proteinuria (nos. 4 and 17) and required re-initiation of tacrolimus therapy, but responded promptly. These patients were re-biopsied, with proven C1qN recurrence and no signs of tacrolimus toxicity. The only other two patients that are currently still on tacrolimus have not been rebiopsied (no. 1 with FSGS and poor compliance; no. 19 with IgAN, who is in remission on tapering doses of tacrolimus). Patient no. 13, who has MCNS, had a repeat renal biopsy after failing to respond to tacrolimus therapy, which again showed MCNS without any sign of tacrolimus toxicity.
Follow-up of children with FSGS (n = 10)
Among the children with SRNS due to FSGS, complete remission was attained in four (40%) and partial remission in five (50%). Two children with FSGS relapsed after being in complete remission (nos. 9 and 11), and two others relapsed after partial remission (nos. 6 and 8). The relapses occurred 16–18 months after a stable clinical status had been achieved and were characterized by secondary resistance to tacrolimus with rapid progression to ESRD.
The overall rate of ESRD due to SRNS from FSGS was 40%. The time to ESRD varied from 36 to 72 months (mean 52 months).
Sustained complete remission was seen in two of the ten children (20%) with FSGS and sustained partial remission was observed in three of the ten (30%). The combined rates of complete and partial relapse and were 50% among these ten children with FSGS.
Summary of tacrolimus resistance
After 16–18 months of tacrolimus therapy, primary resistance to tacrolimus was seen in two patients (one FSGS, one MCNS) and secondary resistance was seen in four patients (all FSGS).
Adverse reactions to tacrolimus
Three patients with SRNS had significant side effects related to tacrolimus (nos. 3, 5, 10) which took the form of acute kidney injury with transient rising of serum creatinine and hyperkalemia (one patient) and hyperglycemia (two). All side effects resolved upon discontinuation of tacrolimus therapy. Both children who developed hyperglycemia were African American and had family history of diabetes mellitus. Two children were switched to MMF (nos. 3, 5), and the other child was switched to cyclosporine (no. 10).
Discussion
Experimental and several controlled therapeutic intervention studies have confirmed that persistence of severe proteinuria is associated with a higher risk of progression to ESRD [2, 11]. Thus, it is necessary to aggressively and safely control proteinuria to prevent progressive renal damage. Tacrolimus, a calcineurin inhibitor, is one of the many therapies used to manage SRNS, but its mechanism of action at the molecular level remains unclear. Faul et al. [12] recently demonstrated that cyclosporine stabilizes actin cytoskeleton in podocytes, which results in its anti-proteinuric effect. Disruption of the foot processes and glomerular slit diaphragm with manifestation of proteinuria is the primary mechanisms of most glomerulopathies, but the variability of response among patients to various medications indicates the complexity of the diseases.
We have observed that nephrotic range proteinuria responds well to tacrolimus irrespective of the histopathologic diagnosis, so we have been using tacrolimus to treat children with established steroid resistance. We have also noted that the literature on the clinical effectiveness of treatments for idiopathic SRNS in children is very limited and that this the lack of sufficient cost and outcome data limits reliable modeling [13]. A few small non-randomized preliminary studies on the beneficial treatment of MCD or FSGS-related SRNS with tacrolimus in adult patients have been published [14, 15]. A small number of published studies have addressed the use of tacrolimus specifically in children with SRNS [7, 8, 16]. A summary of the largest series published in pediatric patients with tacrolimus therapy in SRNS is shown in Table 3.
The mean duration of the NS before initiation of tacrolimus therapy was significantly shorter in our series (2.2 months) than that reported in other series, where the mean duration was as long as 4–5 years [6, 7]. The use of prednisone with tacrolimus for the treatment of SRNS has been variable in the published studies [4–7, 16, 17]. In our series, we rapidly withdraw steroids in order to minimize its side effects as patients already had SRNS. Only two other reports follow this approach [4, 6].
In recent publications, the time of response to tacrolimus in children with SRNS has been described by different authors to be about 8 weeks [4, 6–8], which is similar to our findings. As in other published studies, we targeted tacrolimus trough levels between 5 and 8 ng/ml, but lower levels were accepted if the child was in remission.
Some authors have reported the successful treatment of FSGS in both children and adults who failed to respond to cyclosporine therapy [4, 14, 18]. Notably, concerns on the long-term effect of calcineurin inhibitors on renal function have been raised. In a randomized controlled trial comparing the efficacy and safety of tacrolimus and cyclosporine in children with SRNS, similar rates of remission were reported at 6 and 12 months, but the rate of nephrotoxicity was significantly higher in the cyclosporine group [16]. Histopathological evidence of tacrolimus toxicity in children with SRNS is not available. However, an advantage of using tacrolimus over cyclosporine is the former’s lack of cosmetic side effects, which translates into better compliance in teenage populations [16].
In our series, repeated biopsies were performed in three patients with no evidence of tacrolimus toxicity. Three of 22 children had adverse reactions that required the discontinuation of tacrolimus. Other researchers have also reported serious side effects associated with tacrolimus toxicity that have required the discontinuation of tacrolimus [7, 8]. However, the rate of adverse reactions to tacrolimus for the treatment of NS varies among the different series (Table 3).
Bhimma et al. [17] treated 20 children with FSGS–SRNS for 12 months with tacrolimus and alternate-day prednisone for 12 months with a mean follow-up of 27.5 months and reported a rate of sustained complete remission similar to that observed in our series, 25%. However, their rate of sustained partial remission (50%) was higher than the one we observed (30%) although we followed the children for a longer time (mean follow-up 55 months).
The reported relapse rate of children with SRNS treated with tacrolimus varies from 11 to 20%. We observed relapses in six of the 16 patients (37.5%) followed for more than 1 year who had initially responded (complete or partial response) to tacrolimus. These rates can not be compared to those of the other studies in Table 3 as the latter had a significantly shorter follow-up period. It is also important to note that the percentage of MCD varies significantly between the published studies. There was only one case of MCD in our series. This child remains nephrotic despite multiple treatment protocols, and repeated renal biopsy has confirmed the initial diagnosis.
Gulati et al. [7] recently published a series of 22 children with SRNS in which they reported a complete remission rate of 84%. However, 41% of those children had biopsy-proven MCD, and the mean follow-up time was <12 months. Initially, we also noticed a very high combined rate of complete and partial remission of SRNS. However, during the long-term follow-up, we observed relapses of SRNS after a period of complete or partial remission. These relapses were frequently associated with the development of resistance to tacrolimus, often progressing to ESRD. The onset of ESRD in such cases occurred after 32 months of follow-up. Bhimma et al. [17] also reported two cases of ESRD (followed by death) after 21 months of follow-up in children treated with tacrolimus for SRNS.
Such late relapses with a malignant outcome are naturally of great concern. These relapses may be due to inherent progression of the FSGS. One possible therapeutic approach is to resort to a longer initial treatment period followed by a slow taper off of tacrolimus over a period of time. This concept of a longer treatment period for children with FSGS–SRNS was recently proposed by Hamasaki et al. [19] after observing a 100% rate of late relapses following the cessation of cyclosporine therapy in such patients. These authors suggested a minimum of 24 months of therapy [19].
There is clearly a need to establish the ideal duration of tacrolimus therapy with protocols addressing the time on tapering its dose. It is currently unknown whether completely stopping all immunosuppressants is preferable to their long-term use. For example, Butani et al. [8] reported a series of 16 children treated with tacrolimus for 27 months; however, they do not clearly state the length of the final follow-up period. Although these authors observed a high rate of complete remission (n = 15), 46% of these patients were still on steroids and 87% on tacrolimus at the end of the study [8]. In our series, we were able to completely stop all immunossuppressant in eight children (50%). Interestingly, Westhoff et al. [15] have also described secondary resistance to tacrolimus in one patient with SRNS–FSGS, which may be yet another factor to consider in a longer treatment time with tacrolimus.
Taking into account the heterogeneity of the response after tacrolimus therapy, we suggest the close monitoring of all children with SRNS, even after complete remission of the NS has been achieved. Such an approach will facilitate the prompt re-initiation of tacrolimus therapy upon detection of proteinuria to prevent progression to ESRD.
We conclude that tacrolimus therapy in children with severe NS is well tolerated and initially quite efficacious in achieving remission. A well-designed, adequately powered, randomized controlled trial comparing tacrolimus with or without prednisone with other treatments (namely rituximab) in children with SRNS without genetic mutation is required to develop the needed protocols. Studies with a long-term follow-up with close monitoring are also required to determine the ideal length of tacrolimus therapy in children with SRNS in order to improve long-term renal survival, particularly in those patients with FSGS.
References
Cameron JS (1990) Proteinuria and progression in human glomerular diseases. Am J Nephrol 10[Suppl 1]:81–87
Tryggvason K, Pettersson E (2003) Causes and consequences of proteinuria: the kidney filtration barrier and progressive renal failure. J Intern Med 254:216–224
Ho S, Clipston N, Timmermann L, Northrop J, Graef I, Fiorentino D, Nourse J, Crabtree GR (1996) The mechanism of action of cyclosporine A and FK506. Clin Immunol Immunopathol 80:S40–S45
McCauley J, Shapiro R, Ellis D, Igdall H, Tzakis A, Starzl TE (1993) Pilot trial of FK506 in the management of steroid-resistant nephrotic syndrome. Nephrol Dial Transplant 8:1286–1290
Li X, Li H, Ye H, Li Q, He H, Zhang X, Chen Y, Han F, He Q, Wang H, Chen J (2009) Tacrolimus therapy in Adults with Steroid- and cyclophosphamide- resistant nephritic syndrome and normal or mildly reduced GFR. Am J Kidney Dis 54:51–58
Loeffler K, Gowrishankar M, Yiu V (2004) Tacrolimus therapy in pediatric patients with treatment-resistant nephrotic syndrome. Pediatr Nephrol 19:281–287
Gulati S, Prasad N, Sharma RK, Kumar A, Gupta A, Baburaj VP (2008) Tacrolimus: a new therapy for steroid-resistant nephrotic syndrome in children. Nephrol Dial Transplant 23:910–913
Butani L, Ramsamooj R (2009) Experience with tacrolimus in children with steroid-resistant nephrotic syndrome. Pediatr Nephrol 24:1517–1523
National High Blood Pressure Education Program (1996) Update on the 1987 task force report on high-blood pressure in children and adolescents: a working group report from the National High Blood Pressure Education Program. Pediatrics 98:649–658
Schwartz GJ, Haycock GB, Edelman CM, Spitzer A (1967) A simple estimation of glomerular filtration rate in children derived from body weight and plasma creatinine. Pediatrics 58:259–263
Ruggenenti P, Perna A, Mosconi L, Pisoni R, Remuzzi G (1998) Urinary protein excretion rate is the best independent predictor of ESRF in non-diabetic proteinuric chronic nephropathies. ‘Gruppo Italiano di Studi Epidemiologici in Nefrologia’ (GISEN). Kidney Int 53:1209–1216
Faul C, Donnelly M, Merscher-Gomez S, Chang YH, Franz S, Delgaauw J, Chang JM, Choi HY, Campbell KN, Kim K, Reiser J, Mundel P (2008) The actin cytoskeleton of kidney podocytes is a direct target of the antiproteinuric effect of cyclosporine A. Nat Med 14:931–938
Colquitt JL, Kirby J, Green C, Cooper T, Trompeter RS (2007) The clinical effectiveness and cost effectiveness of treatments for children with idiopathic steroid-resistant nephrotic syndrome: a systematic review. Health Technol Assess 11:iii–iv, ix–xi, 1–93
Segarra A, Vila J, Pou L, Majo J, Arbos A, Quiles T, Piera LL (2002) Combined therapy of tacrolimus and corticosteroids in cyclosporine-resistant or dependent idiopathic focal glomerulosclerosis: a preliminary uncontrolled study with prospective follow-up. Nephrol Dial Transplant 17:655–662
Westhoff TH, Schmidt S, Zidek W, Beige J, van der Geit M (2006) Tacrolimus in steroid-resistant and steroid-dependant nephrotic syndrome. Clin Nephrol 65:393–400
Choudhry S, Bagga A, Hari P, Sharma S, Kalaivani M, Dinda A (2009) Efficacy and safety of tacrolimus versus cyclosporine in children with steroid-resistant nephritic syndrome: a randomized controlled trial. Am J Kidney Dis 53:760–769
Bhimma R, Adhikari M, Asharam K, Connolly C (2006) Management of steroid-resistant focal segmental glomerulosclerosis in children using tacrolimus. Am J Nephrol 26:544–551
Suzuki K, Tsugawa K, Tanaka H (2006) Tacrolimus for treatment of focal segemental glomerulosclerosis resistant to cyclosporine A. Pediatr Nephrol 21:1913–1914
Hamasaki Y, Yoshikawa N, Hattori S, Sasaki S, Iijima K, Nakanishi K, Matsuyama T, Ishikura K, Yata N, Kaneko T, Honda M, Japanese Study Group of Renal Disease (2009) Cyclosporine and steroid therapy in children with steroid resistant nephrotic syndrome. Pediatr Nephrol 24:2177–2185
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roberti, I., Vyas, S. Long-term outcome of children with steroid-resistant nephrotic syndrome treated with tacrolimus. Pediatr Nephrol 25, 1117–1124 (2010). https://doi.org/10.1007/s00467-010-1471-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-010-1471-8