Abstract
Recent advances in our understanding of the excess mortality of chronic kidney disease (CKD) due to cardiovascular complications, obtained through observational studies, demonstrate that vascular calcification and hyperphosphatemia are major cardiovascular risk factors. Mechanistic studies demonstrate that these two risk factors are related and that hyperphosphatemia directly stimulates vascular calcification. The role of hyperphosphatemia in stimulating vascular calcification in CKD is associated with a block to the skeletal reservoir function in phosphate balance due to excess bone resorption. This has led to the realization that renal osteodystrophy is linked to vascular calcification by disordered mineral homeostasis (phosphate) and that a multiorgan system fails in CKD, leading to cardiovascular mortality. In children with renal disease, the multiorgan system fails, just as in adults, but the outcomes have been less well studied, and perceptions of differences from adults are possibly incorrect. Vascular calcification and cardiovascular mortality are less prevalent among pediatric patients, but they are present. However, CKD-induced vascular disease causes stiffness of the arterial tree causing, in turn, systolic hypertension and left ventricular hypertrophy as early manifestations of the same pathology in the adult. Because of the role of the skeleton in these outcomes, renal osteodystrophy has been renamed as the CKD mineral bone disorder (CKD-MBD). This review, which focuses on the pediatric patient population, describes our current state of knowledge with regards to the pathophysiology of the CKD-MBD, including the new discoveries related to early stages of CKD. As a new necessity, cardiovascular function issues are incorporated into the CKD-MBD, and new advances in our knowledge of this critical component of the disorder will lead to improved outcomes in CKD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic kidney disease mineral bone disorder (CKD-MBD) is a term coined by Kidney Disease Improving Global Outcomes Foundation (KDIGO) [1] to replace the term, renal osteodystrophy (ROD) in recognition of several pathophysiologic discoveries of the 21st century. The first of these pathophysiologic discoveries is that the disorders in mineral metabolism associated with CKD are key factors contributing to the excess mortality observed in CKD [2, 3]. Secondly, the skeletal remodeling disorders caused by CKD contribute directly to the disordered mineral metabolism and the heterotopic mineralization, especially the vascular calcification that accompanies CKD [4]. Thirdly, CKD or renal injury impairs skeletal anabolism, decreasing osteoblast function and bone formation rates [5]. In short, a multiorgan system has been defined, involving the kidney, skeleton, parathyroid glands, fat, the intestine and the cardiovasculature, which fails in CKD. This system failure produces cardiovascular morbidity, which is often fatal [6]. When CKD begins in childhood, the cardiovascular dysfunction produced by the CKD-MBD causes vascular stiffness and systolic hypertension. Left ventricular hypertrophy is a common complication, and vascular calcification and mortality are observed, though less prevalent than in adults.
Pathobiology of the CKD-MBD
The increasing incidence of CKD and ESKD in the USA, and the role of the CKD-MBD in the high mortality of CKD patients makes it a major health issue for Americans and all developed societies [6–8]. When CKD affects children, the CKD-MBD results [9]. In early CKD in children, hypertension and left ventricular hypertrophy are common. The left ventricular hypertrophy has been considered solely as an end organ complication of hypertension. However, vascular stiffness detected by the ankle-brachial index and carotid intimal medial thickness is very common in pediatric CKD, and vascular stiffness leading to systolic hypertension and wide pulse pressures are major factors contributing to left ventricular hypertrophy and cardiac dysfunction. In children, the skeletal disorders of CKD contribute to growth failure and, similar to left ventricular hypertrophy, this also begins early in the course of kidney disease. Renal osteodystrophy in children is predominantly due to hyperparathyroidism, hyperphosphatemia and calcitriol deficiency. However, the latter are relatively late complications of the CKD-MBD, which can clearly be shown to begin before these abnormalities are detectable. Virtually all children with end-stage kidney disease (ESKD) demonstrate skeletal histologic pathology [10], but a higher proportion of children with stages 2–4 CKD maintain normal bone formation rates than their adult counterparts. This is misleading because the CKD-MBD begins early following initial insults to kidney function that are demonstrable by high-resolution peripheral computed tomography (HRpQCT) [11] and elevated levels of fibroblast growth factor-23 (FGF-23) [12]. This high-resolution imaging study detected, for the first time, an early impairment of trabecular micro-architecture in CKD 2–4 patients before the onset of severe hyperparathyroidism and calcitriol deficiency. The skeleton contributes to the onset and progression of the cardiovascular complications of CKD in children. However, the lack of underlying atherosclerosis stimulated by CKD in children and the resistance of the growing skeleton to renal osteodystrophy may diminish the severity of the skeletal and cardiovascular complications. These do develop and they become phenotypically the same as in adults as the children transition out of pediatrics.
Pathogenesis of the CKD-MBD
Renal injuries produce a loss of mesenchymal cell anabolism manifested as a decrease in bone formation rates that derive from osteoblast activity [5] and loss of the vascular smooth muscle phenotype that may affect cardiovascular reactivity [13]. The loss of anabolism occurs in early CKD [14] in the presence of normal parathyroid hormone (PTH), vitamin D, Ca and PO4 levels, but it produces changes in the new hormonal systems that define the early phases of the CKD-MBD, leading to cardiovascular disease and growth failure. These two new defined hormonal systems are FGF23 [15, 16] and osteocalcin [17]. Loss of osteoblastic bone formation due to renal injury shrinks the size of the rapidly exchangeable phosphate and calcium pools, causing early stimuli for secondary hyperparathyroidism [18]. Osteoblasts form the hematopoietic stem cell niche [19], and an adaptation to the loss of osteoblast function in CKD is required to preserve hematopoiesis. This adaptation is secondary hyperparathyroidism [18]. Three (family of) factors, namely, bone morphogenetic proteins (BMP), wingless/ints proteins (Wnts) and PTH, regulate the hematopoietic stem cell niche [20]. Hyperparathyroidism may represent the adaptation necessary to maintain endosteal and bone marrow microenvironments, including the hematopoietic stem cell (HSC) niche due to the decreased influence of either BMPs or Wnts on osteoblast activity following renal injury. Adapting to maintain the niche size comes at the expense of high PTH levels and the increased influence of secondary hyperparathyroidism on skeletal remodeling.
The earliest immunohistochemical abnormalities of bone in the CKD-MBD are seen after a relatively mild reduction in the glomerular filtration rate (between 60 and 90 ml/min/1.73m2, stage 2 CKD) [12, 21] and before abnormalities of mineral homeostasis are detectable by serum assays of Ca, inorganic phosphorus (Pi), calcitriol and PTH (Fig. 1). At these early stages of CKD, elevated FGF-23 and PTH levels, although the latter less frequently, are observed before changes in the serum phosphorus, calcitriol or calcium are detectable [12, 22–24].
The pathogenesis of the chronic kidney disease mineral bone disorder (CKD-MBD). The onset of the CKD-MBD is in very early CKD when kidney injury/disease (KD) causes a decrease in bone formation. This decrease may still leave bone formation rates within the normal range, but it stimulates osteocytes to secrete fibroblast growth factor-23 (FGF-23). Elevations in FGF-23 are seen in pediatric CKD at stage 2 disease before abnormalities in phosphate homeostasis, calcitriol deficiency or parathyroid hormone (PTH) secretion are detectable. The effects of FGF-23 are to decrease the tubular reabsorption of inorganic phosphorus (Pi), because this Pi is not being put into the skeletal reservoir in the form of bone, and to inhibit calcitriol production. These early changes progress with progression of CKD to stimulate PTH secretion. During the progression to stage 3–4 CKD, positive phosphate balance, calcitriol deficiency and the switch from low-turnover to high-turnover osteodystrophy develop as the hyperparathyroidism progresses. In translational studies, the early phase of the CKD-MBD is involved with stimulation of vascular calcification (Vasc. Calcif.) in stage 2 CKD [14]
As kidney failure advances, a variety of factors directly stimulate PTH secretion, including hypocalcemia, low calcitriol levels, hyperphosphatemia and other factors (Fig. 1). These are additive to the initial stimulus produced by renal injury, increasing the strength of the adaptation, and they serve the additional purposes of attempting to maintain the homeostasis of calcium, calcitriol and phosphorus. Maintaining calcium homeostasis drives the hyperparathyroidism to stimulate bone resorption for release of Ca and Pi from the storage reservoir, but this sets up a block of the reservoir for the uptake of excess phosphorus when the balance of the latter becomes positive.
Pathogenetic factors in the CKD-MBD
Loss of smooth muscle phenotype
Early CKD produces a loss of smooth muscle terminal differentiation. This was discovered when it was found that CKD more than doubled the size of the neointimal hyperplastic lesion (NH) produced by an arterial-venous anastomosis [13]. The NH lesion is produced by migrating vascular smooth muscle cells (VSMC), and to migrate, VSMC have to dedifferentiate [25]. These data are in agreement with those of Chen et al. demonstrating that uremic serum stimulates the osteoblastic transition of VSMC in vitro, a step also requiring dedifferentiation to proceed [26]. The decrease in differentiation produces decreased expression of the contractile apparatus of the VSMC [27] and, as a result, decreased contractility. This decrease in contractility by definition produces vascular stiffness, which in turn leads to increased systolic pressures. Thus, early CKD produces vascular stiffness leading to systolic hypertension, a newly recognized early manifestation of the CKD-MBD especially important in kids.
Fibroblast growth factor-23
FGF-23 is the original phosphatonin (phosphate excretion regulating hormone) discovered in studies of autosomal dominant hypophosphatemic rickets and oncogenic osteomalacia [28, 29]. FGF-23 levels increase progressively during the course of CKD, including pediatric CKD [12, 22, 30]. The roles of FGF-23 in regulating phosphate homeostasis and calcitriol synthesis in CKD are just now being elucidated. It is known that FGF-23 is produced mainly by osteocytes and osteoblasts and that the stimulus for FGF-23 production is a decrease in bone formation. Thus, FGF23 represents a skeletal signal that Pi is not being deposited and that Pi excretion needs to be increased. FGF-23 represents a direct bone–kidney connection in the multiorgan system involved in the CKD-MBD (Fig. 1). The tendency of children to have higher rates of bone formation is associated with increased osteoid thickness and surfaces covered by osteoid in the CKD-MBD [12]. Whether these findings are the result of high turnover rates or a mineralization defect apparent in children with CKD-MBD is unknown. FGF-23 may be the pathogenetic factor in the latter instance. Furthermore, FGF-23-stimulated 24-hydroxylase and reduced vitamin D and calcitriol levels affect the vascular osteoblastic transition, causing calcification.
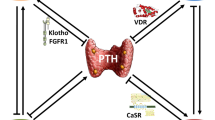
The actions of FGF-23 require FGF receptors (FGFR1c) which are widely expressed and a specific co-receptor, Klotho, which has limited tissue distribution and establishes high-affinity receptor binding. Klotho distribution defines the actions of FGF-23. In the proximal tubule, FGF-23 inhibits the activity of the sodium-dependent Pi transporter NaPT2a and the 25-OH cholecalciferol-1α hydroxylase, 27CYP2a, and it stimulates 24-OH hydroxylase. Thus, FGF-23 reduces calcitriol and vitamin D levels. Calcitriol, in turn, stimulates FGF-23 production in osteocytes. In the parathyroid chief cells, FGF-23 inhibits PTH secretion, and PTH, in turn, affects FGF-23 production in osteocytes. Behind the blood brain barrier there is central nervous system (CNS) FGF-23 production and Klotho-mediated signal transduction unrelated to the systemic hormone system at this time.
Osteocalcin
Osteocalcin is secreted by osteoblasts during bone formation. While osteocalcin is a well-known osteoblast-specific Ca-binding matrix protein, its uncarboxylated form is a newly discovered hormone regulating energy utilization and production [17]. Osteocalcin stimulates adipocytes to convert triglyceride to glucose, the pancreas to secrete insulin and myocytes and osteoblasts to respond to insulin and increase glucose uptake for energy production in the form of ATP. The early loss of bone formation in CKD systemically causes decreased osteocalcin and decreased energy production/utilization. This affects cardiac energy production, utilization and function and may contribute to the pathogenetic basis for developing left ventricular hypertrophy in children with CKD. This exciting new discovery requires extensive study in the CKD setting, but it sets up CKD-induced skeletal injury as a key factor in the multiorgan system failure that causes excess mortality.
Calcitriol deficiency
Decreased calcitriol production is a direct outcome of increased FGF-23 production. Early in CKD, these decreases are detectable as changes within the normal range (Fig. 1). As CKD advances, the functioning nephron mass is decreased and this, combined with an increased phosphate load in the remaining nephrons, results in calcitriol deficiency from proximal tubular 25-hydroxycholecalciferol 1α-hydroxylase activity [31]. Calcitriol deficiency in turn decreases intestinal calcium absorption and leads to hypocalcemia and, in cases of advanced kidney failure, diminishes tissue levels of vitamin D receptors (VDR), in particular, the VDR of parathyroid gland cells [32]. Because the chief cell VDR suppresses the expression of pre-pro-PTH mRNA, lower circulating calcitriol levels together with a low number of vitamin D receptors in patients with ESKD result in stimulation of both the synthesis and secretion of PTH [33]. The VDR is expressed in vascular smooth muscle cells and cardiac myocytes. What remains to be defined is the role of vitamin D and calcitriol deficiency in the cardiovascular complications of CKD. Despite the role of high levels of vitamin D analogs in stimulating vascular calcification [34, 35], low doses of vitamin D analogs that are sufficient to act as hormone replacement therapy actually inhibit vascular calcification [36, 37].
Hyperparathyroidism
All of the mechanisms discussed above result in an increased production of PTH and nodular hyperplasia of the parathyroid glands in CKD. The size of the parathyroid glands progressively increases during CKD, mainly due to diffuse cellular hyperplasia; in dialyzed patients with CKD, this increase in size is positively correlated with increasing serum PTH levels. Monoclonal chief cell growth also develops, resulting in the formation of nodules. Nodular hyperplastic glands have fewer vitamin D and calcium-sensing receptors than diffusely hyperplastic glands, thereby promoting parathyroid gland resistance to calcitriol and calcium. Sustained elevation in PTH levels, while adaptive to maintaining osteoblast surfaces, produce an abnormal phenotype of osteoblast function with relatively less type 1 collagen and more RANKL ligand production than anabolic osteoblasts. This leads to a high-turnover osteodystrophy, PTH receptor desensitization and excess bone resorption.
Hyperphosphatemia
As renal injury decreases nephron number, the stimulus to hyperphosphatemia due a reduction in filtered phosphate is reversed through PTH- and FGF-23-mediated reductions in tubular epithelial phosphate transport. The increase in phosphate excretion by the remaining nephrons restores phosphate homeostasis at the cost of higher PTH and FGF-23 levels and maintains normal phosphate excretion. In stage IV and V CKD, when renal injury is severe enough that the glomerular filtration rate reaches levels of less than 30% of normal, hyperphosphatemia becomes fixed due to insufficient renal excretion despite high PTH and FGF-23 levels [38]. At this level of reduced renal function, the ability of the remaining nephrons to increase phosphate excretion above roughly 80–90% of the filtered load fails due to as yet unclear reasons. Studies have demonstrated that failure of calcium and phosphorous deposition into the skeleton or excess resorption of the skeleton also contribute to abnormal calcium and phosphorus levels in CKD and ESKD [4, 39]. Hyperphosphatemia decreases serum calcium through physicochemical binding and suppresses 1α-hydroxylase activity, which results in further lowering of the circulating calcitriol levels. Moreover, a direct stimulatory effect of phosphorus on the parathyroid gland cells, independent of calcium and calcitriol, produces increased secretion and nodular hyperplasia of parathyroid gland cells [40, 41]. Finally, hyperphosphatemia is a signaling mechanism for the induction of heterotopic mineralization of the vasculature in CKD and ESKD [42, 43].
Hypocalcemia
As CKD progresses, hypocalcemia develops due to decreased intestinal Ca absorption. Low blood levels of ionized calcium stimulate PTH secretion, whereas high calcium concentrations suppress it. The action of calcium on parathyroid gland chief cells is mediated through a calcium sensor; a G-protein-coupled plasma membrane receptor (CASR) expressed in chief cells, kidney tubular epithelia and, at lower levels widely throughout the body [44, 45]. The short-term stimulation of PTH secretion induced by low calcium is due to exocytosis of PTH packaged in granules, and longer term stimulation results from an increase in the number of cells that secrete PTH. More prolonged hypocalcemia induces changes in intracellular PTH degradation and mobilization of a secondary storage pool. Within days or weeks of the onset of hypocalcemia, pre-pro-PTH mRNA expression is stimulated. This effect is exerted through a negative calcium response element located in the upstream flanking region of the gene for PTH. Expression of the CASR has been shown to be suppressed by calcitriol deficiency and stimulated by calcitriol administration, suggesting an additional regulatory mechanism of the active vitamin D metabolite on PTH production. The decreased number of calcium-sensing receptors with low circulating calcitriol may, at least in part, explain the relative insensitivity of parathyroid gland cells to calcium in patients undergoing dialysis. In addition, the CASR may be expressed and regulated similarly in vascular smooth muscle cells and cardiac myocytes, suggesting that hypocalcemia may have direct actions on cardiovascular function in CKD.
Inflammatory mediators
CKD is well-known as an inflammatory state with elevated levels of numerous inflammatory cytokines, chemokines and their receptors [46–48]. For example, interleukin-8 (IL-8) levels are elevated in CKD, contributing to PTH secretion. A central inflammatory cytokine, IL-6, is a direct marker of inflammation in CKD [49], and it contributes to ROD pathogenesis [46]. However, the critical roles of inflammatory mediators in the CDK-MBD remain to be defined [50].
Leptin
One of the roles of inflammatory mediators in the CKD-MBD is the stimulation of leptin secretion from adipose tissue. Leptin is a small anorexiogenic hormone that acts directly on the hypothalamus to decrease appetite and through its action on the melanocortin receptor 4, leptin leads to β-adrenergic nervous system-dependent inhibition of osteoblast function. Leptin is increased in CKD and implicated in the cachexia of uremia. Its metabolism is delayed by kidney disease through decreased proximal tubular metabolism. Its role as a pathogenic factor in the adynamic bone disorder remains to be fully characterized.
Acidosis
As nephron mass declines in CKD, the ability to regenerate bicarbonate consumed in the buffering of metabolic acids is lost. As a result, metabolic acidosis is a uniform finding in stage 4/5 CKD. In this setting, bone becomes an important buffer of acid production in patients with ESKD [51]. Metabolic acidosis stimulates bone resorption and suppresses bone formation [52], thereby resulting in negative bone balance and contributing significantly to the pathogenesis of CKD-MBD.
Aluminum
The accumulation of aluminum (Al3+) in bone and other organs, such as the parathyroid glands, may occur in patients undergoing dialysis or before the initiation of dialysis. Aluminum accumulation in the parathyroid glands results in the decreased secretion of PTH and suppression of bone turnover. In addition, aluminum inhibits renal and intestinal 25-hydroxycholecalciferol 1-α-hydroxylase activity and, therefore, aluminum may further contribute to reduced levels of calcitriol. Possible sources of aluminum include high aluminum concentrations in the water used for dialysis, prescription of aluminum-containing phosphate binders and aluminum in drinking water, infant formula and other liquids or solid food.
Hypertension
The major factor in the cardiovascular manifestations of CKD-MBD is hypertension. Hypertensive phenotypes determined by automatic blood pressure monitoring are relatively specific to CKD, including pediatric CKD. The results of early studies suggest that phosphate contributes to vascular stiffness in pediatric CKD, which in turn indicates that the CKD-MBD is a contributing factor of unknown importance to hypertension and possibly cardiac function in CKD.
Hypogonadism
Patients with ESKD have various states of gonadal dysfunction. Estrogen and testosterone deficiency significantly contributes to CKD-MBD pathogenesis.
Matrix Gla protein, fetuin, pyrophosphate and other factors
Some patients with CKD are treated with glucocorticoids, which have an impact on bone metabolism. Patients maintained on chronic dialysis retain of β2-microglobulin. Additionally, alterations in growth factors and other hormones involved in the regulation of bone remodeling may be disordered in CKD/ESRD, thus affecting bone remodeling and contributing to the development of CKD-MBD. Matrix Gla protein, fetuin and pyrophosphate are inhibitors of mineralization. The regulation of these factors is disordered in CKD, especially in the vasculature, contributing to vascular calcification in the CKD-MBD. Extensive review of these factors is beyond the scope of this article.
Pathology of the CKD-MBD
Renal osteodystrophy
The pathology of renal osteodystrophy (ROD) is not uniform. Depending on the relative contribution of the different pathogenic factors discussed above and their treatment, various pathologic patterns of bone remodeling are expressed in CKD and ESKD.
Low-turnover bone disease, adynamic bone disorder
Low-turnover uremic osteodystrophy may be the initial pathology of renal osteodystrophy, but it is most often missed. Children with this disorder often experience a transition from normal bone formation rates to high-turnover disease. The histologic hallmark of the adynamic bone disorder (ABD) group is a profound decrease in bone turnover due to a low number of active remodeling sites, the suppression of bone formation and low resorption, with the latter not as decreased as formation. The result is a low turnover condition that will lead to osteopenia and osteoporosis. The majority of trabecular bone is covered by lining cells, with few osteoclasts and osteoblasts. Bone structure is predominantly lamellar, and the extent of mineralizing surfaces is markedly reduced. Only a few thin, single tetracycline labels are usually observed. Two subgroups can be identified in this type of renal osteodystrophy based on the causal events leading to a decline in osteoblast activity: ABD and low-turnover osteomalacia from aluminum intoxication.
Low-turnover osteomalacia is characterized by an accumulation of unmineralized matrix in which a diminution in mineralization precedes or is more pronounced than the inhibition of collagen deposition. Unmineralized bone represents a sizable fraction of trabecular bone volume. The increased lamellar osteoid volume is due to the presence of wide osteoid seams that cover a large portion of the trabecular surface. The occasional presence of woven bone buried within the trabeculae indicates past high bone turnover. When osteoclasts are present, they are usually seen within trabecular bone on at the small area of the trabecular surface left without osteoid coating.
Predominant hyperparathyroid bone disease, high-turnover ROD and osteitis fibrosa
Sustained excess PTH results in increased bone turnover, with osteoclasts, osteoblasts and osteocytes found in increased numbers. Disturbed osteoblastic activity results in a disorderly production of collagen, which in turn results in the formation of woven bone. The accumulation of fibroblastic osteoprogenitors not in the osteoblastic differentiation program results in collagen deposition (fibrosis) in the peritrabecular and marrow space. The non-mineralized component of bone, osteoid, is consequently increased, and the normal three-dimensional architecture of osteoid is frequently lost. Osteoid seams no longer exhibit their usual birefringence under polarized light; instead, a disorderly arrangement of woven osteoid and woven bone with a typical crisscross pattern under polarized light is seen. The mineral apposition rate and number of actively mineralizing sites are increased, as documented under fluorescent light after the administration of time-spaced fluorescent (tetracycline) markers.
Mixed uremic osteodystrophy, high-turnover ROD plus a mineralization defect
Mixed uremic osteodystrophy is caused primarily by hyperparathyroidism and defective mineralization with or without increased bone formation. These features may coexist in varying degrees in different patients. Increased numbers of heterogeneous remodeling sites can be seen, and the number of osteoclasts is usually increased. Because active foci with numerous cells, woven osteoid seams and peritrabecular fibrosis coexist next to lamellar sites with a more reduced activity, the greater production of lamellar or woven osteoid causes an accumulation of osteoid with osteoid seams that are normal or increased in thickness. Whereas active mineralizing surfaces increase in woven bone with a higher mineralization rate and diffuse labeling, mineralization surfaces may be reduced in lamellar bone with a decreased mineral apposition rate.
Associated features of renal osteodystrophy
Osteoporosis and osteosclerosis
With a progressive loss of renal function, cancellous bone volume may be increased along with a loss of cortical bone, but this is in part due to the deposition of woven immature collagen fibrils instead of lamellar fibrils. Thus, bone strength suffers despite the increase in mass detected by dual energy X-ray absorptiometry (DEXA). Patients undergoing chronic dialysis may have a loss or gain in bone volume depending on bone balance. When the bone balance is positive, osteosclerosis may be observed when osteoblasts are active in depositing new bone (especially woven), thus superseding bone resorption. This is relatively rare in the 21st century due to improved therapy of secondary hyperparathyroidism, and it is less common in children than adults.
In the case of negative bone balance, bone loss occurs in cortical and cancellous bone and is more rapid when bone turnover is high. In those cases, bone densitometry will detect osteopenia or osteoporosis. The prevalence of osteoporosis in the population with CKD exceeds its prevalence in the general population [53–55], and children are not necessarily spared from osteopenia or osteoporosis. Osteoporosis is observed in CKD before dialysis is required for end-stage kidney failure [56]. When bone turnover is high, as in secondary hyperparathyroidism with osteitis fibrosa, bone resorption rates are in excess of bone formation, and osteopenia progressing to osteoporosis may result. When bone turnover is low, although both bone formation rates and bone resorption may be reduced, resorption is in excess and loss of bone mass occurs. Thus, osteoporosis may be observed with either high-turnover [56–59] or low-turnover [60] forms of osteodystrophy. When bone resorption exceeds bone formation rates in CKD, a positive phosphorus and calcium balance results in hyperphosphatemia and hypercalcemia without an increase in skeletal mineral deposition, but with a stimulation of heterotopic mineralization, especially of the vasculature. The failure of the skeleton to absorb the positive phosphate balance in CKD is an important stimulus to heterotopic mineralization and links the skeleton and osteoporosis in CKD to cardiovascular events and mortality [61].
Bone aluminum, iron, lanthanum and bisphosphonate accumulation
These substances accumulate in bone at the mineralization front, at the cement lines, or diffusely. The extent of stainable aluminum at the mineralization front correlates with histologic abnormalities in mineralization. Aluminum deposition is most severe in cases of low-turnover osteomalacia. However, it can be observed in all histologic forms of renal osteodystrophy. In patients in whom an increased aluminum burden develops, bone mineralization and bone turnover progressively decrease. These abnormalities are reversed with the removal of the aluminum. Iron also accumulates at the mineralization front and can cause low-turnover forms of ROD similar to aluminum, although much less is known of iron intoxication than aluminum. Bisphosphonates are drugs used in the treatment of osteoporosis and hypercalcemia. There are increasing instances of bisphosphonate use in patients with CKD and ESKD. However, the nature of the bone remodeling abnormalities in CKD, especially with woven bone formation and mineralization defects, lend a high level of risk to skeletal deposition of a substance that once deposited may not be removed. Such a risk of long-term retention of an active drug inhibiting bone turnover is now being recognized with the use of bisphosphonates in osteogenesis imperfecta and the rare side effect of the drugs in osteonecrosis of the jaw [62] and subtrochanteric fractures of the hip. Lanthanum has recently been added as a rare earth ion administered to CKD and ESKD patients. It is poorly absorbed, and its levels in bone are much less than that of aluminum. Long-term administration appears to be safe with early 10-year data available. Five-year data demonstrate that the levels of skeletal accumulation remain below those with any biologic or toxic effects. Lanthanum disappearance from bone deposits is slow, but not as slow as that of bisphosphonate.
Cardiovascular
Specific cardiovascular pathology in the CKD-MBD is unknown. Studies of the vasculature in CKD indicate the presence of osteoblastic differentiation in the vessel wall. These findings are in agreement with studies suggesting that uremic serum and high phosphate levels stimulate osteoblastic differentiation of calcifying vascular cells and vascular smooth muscle cells. Cardiac remodeling with the concomitant loss of myotubes and stimulation of interstitial myofibroblasts is a complication of CKD, and this remodeling is probably stimulated by calcitriol deficiency, hyperphosphatemia and unknown factors of the CKD-MBD. This is an important area for new research as we improve our understanding and treatment of the CKD-MBD.
Clinical manifestations
Patients with mild to moderate kidney insufficiency are rarely symptomatic due to the CKD-MBD and its skeletal pathology. However, cardiovascular symptoms are more common, such as hypertension. We must also consider vascular calcification to be a complication of the CKD-MBD and the appearance of the CKD-MBD to be a cause of vascular stiffness. In CKD, vascular stiffness causes an increase in systolic blood pressure, a widening of the pulse pressure and an increase in pulse wave velocity. Vascular calcification is a clinically important CKD-MBD complication and may develop while the patient is asymptomatic in terms of the musculoskeletal system.
Symptoms of CKD-MBD related to the skeleton appear in patients with advanced kidney failure. Clinical manifestations are preceded, however, by an abnormal biochemical profile (hypocalcemia, hyperphosphatemia, calcitriol deficiency and elevated PTH levels) that should alert the physician and prompt steps to prevent more severe complications. When symptoms related to the skeleton occur, they are usually insidious, subtle, nonspecific and slowly progressive.
Vascular calcification, calciphylaxis and tumoral calcinosis
Vascular calcification is common in patients with ESKD, causing left ventricular hypertrophy, congestive heart failure and coronary ischemia. The pathogenesis of vascular calcification in CKD is complex and can be classified pathologically into two types: neointimal and arterial medial. Atherosclerotic neointimal calcification is multifactorial, but it involves activation of an osteoblastic differentiation program in cells of the neointima around atherosclerotic plaques and the tunica media. Diffuse calcification of arterial tunica media is referred to as Mönckeberg’s sclerosis. CKD is the most common cause of Mönckeberg’s sclerosis, especially when it complicates diabetes mellitus. All forms of ROD are associated with vascular calcification, but the association between low-turnover osteodystrophy and atherosclerotic neointimal calcification is of particular importance. Here, the decrease in skeletal osteoblast function is associated with osteoblastic differentiation of cells in the vasculature. Furthermore, signals deriving from the skeleton, such as hyperphosphatemia, are direct causes of vascular mineralization.
Heterotopic tissue calcification may occur in the eyes and manifest as band keratopathy in the sclera or induce an inflammatory response known as the red eye syndrome in the conjunctiva. These types of calcifications are usually associated with hyperparathyroidism or increased calcium phosphate production. Calcium deposits are also found in the lungs and lead to restrictive lung disease. Deposits in the myocardium may cause arrhythmias, annular calcifications, valvular calcification or myocardial dysfunction. Most soft tissue calcifications are attributed to secondary hyperparathyroidism or to the increased calcium phosphate product associated with it. However, they have also been described in patients with ABD. This diversity could be explained by increased calcium and/or phosphate release from bone in patients with severe hyperparathyroidism and an inability to maintain normal mineral accretion in patients with ABD.
The syndrome of calciphylaxis is characterized by vascular calcification in the tunica media of peripheral arteries. These calcifications induce painful violaceous skin lesions that progress to ischemic necrosis. This syndrome is associated with serious complications and often death. Calciphylaxis has been associated with high serum calcium phosphate production and severe secondary hyperparathyroidism. However, it can also be seen in patients with normal or mildly elevated serum phosphate or PTH levels. The pathogenesis of calciphylaxis is probably multifactorial because hyperparathyroidism, high calcium phosphate production, steroid therapy, vitamin D therapy, iron overload, aluminum toxicity and protein C deficiency have all been implicated.
Tumoral calcinosis is a form of soft tissue calcification that usually involves the periarticular tissues. Calcium deposits may grow to an enormous size and interfere with the function of adjacent joints and organs. Although this type of calcification is usually associated with high calcium phosphate production, its exact pathogenesis is poorly understood. The recent discoveries of three single gene mutations in FGF-23, Klotho and GALNT3, respectively, causing inherited tumoral calcinosis has shed light on the role of hyperphosphatemia in its pathogenesis [63–65] because FGF-23 is a phosphatonin [66] and Klotho is a co-receptor for FGF-23 in the proximal tubule of the kidney [67]. Similar to soft tissue calcification, tumoral calcinosis is observed with severe hyperparathyroidism and low-turnover bone disease.
Bone pain, fractures and skeletal deformities
Bone pain is usually vague, ill defined and deep seated. It may be diffuse or localized in the lower part of the back, hips, knees or legs, and weight bearing and changes in position commonly aggravate it. Bone pain may progress slowly to the degree that patients are completely incapacitated. Bone pain in patients with ESKD usually does not manifest itself physically; however, local tenderness may be apparent with pressure. A sharp chest pain may indicate rib fracture. Spontaneous fractures or fractures after minimal trauma may also occur in vertebrae (crush fractures) and in tubular bones.
Bone pain and bone fractures can be observed in all patients with ESKD independent of the underlying histologic bone disease, especially when osteoporosis is present [53]. The incidence of fractures is markedly elevated in patients with CKD relative to the general population.
Skeletal deformities can be observed in children and adults. Most children with ESKD have growth retardation, and bone deformities may develop from vitamin D deficiency (rickets) or secondary hyperparathyroidism. Bowing of the long bones, especially the tibiae and femora, is seen in children with rickets, accompanied with typical genu valgum that becomes more severe with adolescence. Long-standing secondary hyperparathyroidism in children may be responsible for slipped epiphyses secondary to the impaired transformation of growth cartilage into regular metaphyseal spongiosa. This complication most commonly affects the hips, becomes obvious in preadolescence and causes limping; however, it is usually painless. When the radius and ulna are involved, ulnar deviation of the hands and local swelling may occur. In adults, skeletal deformities can be observed in cases of severe osteomalacia or osteoporosis and include lumbar scoliosis, thoracic kyphosis and recurrent rib fractures.
Hypertension, congestive heart failure, coronary ischemia peripheral vascular disease
A discussion of the clinical manifestations of the cardiovascular complications of the CKD-MDB is beyond the scope of this review. The role of the CKD-MBD in the pathogenesis of these prevalent complications of CKD remains unclear. A clear-cut contribution of the CKD-MBD to vascular stiffness, at least through vascular calcification in CKD, has been established, but it is likely that the role of the CKD-MBD in the cardiovascular complications of CKD is much greater. Emerging and future studies will provide important clarifications of these clinical issues, which are very prevalent in children receiving renal replacement therapy.
References
Moe S, Drueke T, Cunningham J, Goodman W, Martin K, Olgaard K, Ott S, Sprague S, Lameire N, Eknoyan G (2006) Definition, evaluation, and classification of renal osteodystrophy: A position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int 69:1945–1953
Stevens LA, Djurdjev O, Cardew S, Cameron EC, Levin A (2004) Calcium, phosphate, and parathyroid hormone levels in combination and as a function of dialysis duration predict mortality: Evidence for the complexity of the association between mineral metabolism and outcomes. J Am Soc Nephrol 15:770–779
Block GA, Hulbert-Shearon TE, Levin NW, Port FK (1998) Association of serum phosphorus and calcium X phosphate product with mortality risk in chronic hemodialysis patients: a national study. Am J Kidney Dis 31:607–617
Davies MR, Lund RJ, Mathew S, Hruska KA (2005) Low turnover osteodystrophy and vascular calcification are amenable to skeletal anabolism in an animal model of chronic kidney disease and the metabolic syndrome. J Am Soc Nephrol 16:917–928
Lund RJ, Davies MR, Brown AJ, Hruska KA (2004) Successful treatment of an adynamic bone disorder with bone morphogenetic protein-7 in a renal ablation model. J Am Soc Nephrol 15:359–369
Foley RN, Parfrey PS, Sarnak MJ (1998) Clinical epidemiology of cardiovascular disease in chronic renal disease. Am J Kidney Dis 32:S112–S119
Slinin Y, Foley RN, Collins AJ (2005) Calcium, phosphorus, parathyroid hormone, and cardiovascular disease in hemodialysis patients: the USRDS waves 1, 3, and 4 study. J Am Soc Nephrol 16:1788–1793
Shlipak MG, Sarnak MJ, Katz R, Fried LF, Seliger SL, Newman AB, Siscovick DS, Stehman-Breen C (2005) Cystatin C and the risk of death and cardiovascular events among elderly persons. N Engl J Med 352:2049–2060
Foley RN, Collins AJ, Herzog CA, Ishani A, Kalra PA (2009) Serum phosphorus levels associate with coronary atherosclerosis in young adults. J Am Soc Nephrol 20:397–404
Malluche HH, Faugere MC (1990) Renal bone disease 1990: challenge for nephrologists. Kidney Int 38:193–211
Bacchetta J, Boutroy S, Vilayphiou N, Juillard L, Guebre-Egziabher F, Rognant N, Sornay-Rendu E, Szulc P, Laville M, Delmas PD, Fouque D, Chapurlat R (2009) Early impairment of trabecular microarchitecture assessed with HR-pQCT in patients with stage II–IV chronic kidney disease. J Bone Miner Res. doi:0.1359/jbmr.090831
Pereira RC, Juppner H, Azucena-Serrano CE, Yadin O, Salusky IB, Wesseling-Perry K (2009) Patterns of FGF-23, DMP1 and MEPE expression in patients with chronic kidney disease. Bone. doi:10.1016/j.bone.2009.08.008
Kokubo T, Ishikawa N, Uchida H, Chasnoff SE, Xie X, Mathew S, Hruska KA, Choi ET (2009) CKD accelerates development of neointimal hyperplasia in arteriovenous fistulas. J Am Soc Nephrol 20:1236–1245
Fang Y, Zhang Y, Mathew S, Futhey J, Lund RJ, Hruska KA (2009) Early chronic kidney disease (CKD) stimulates vascular calcification (VD) and decreased bone formation rates prior to positive phosphate balance (abstract). J Am Soc Nephrol 20:36 A (abstract TH - FC 153)
Quarles LD (2003) FGF23, PHEX, and MEPE regulation of phosphate homeostasis and skeletal mineralization. Am J Physiol Endocrinol Metab 285:1–9
Shimada T, Kakitani M, Yamazaki Y, Hasegawa H, Takeuchi Y, Fujita T, Fukumoto S, Tomizuka K, Yamashita T (2004) Targeted ablation of FGF23 demonstrates an essential physiological role of FGF23 in phosphate and vitamin D metabolism. J Clin Invest 113:561–568
Lee NK, Sowa H, Hinoi E, Ferron M, Ahn JD, Confavreux C, Dacquin R, Mee PJ, McKee MD, Jung DY, Zhang Z, Kim JK, Mauvais-Jarvis F, Ducy P, Karsenty G (2007) Endocrine regulation of energy metabolism by the skeleton. Cell 130:456–469
Hruska KA, Mathew S (2008) The chronic kidney disease mineral bone disorder (CKD-MBD). In: Rosen CJ (ed) Primer on the metabolic bone diseases and disorders of mineral metabolism. Am Soc Bone Miner Res, Washington D.C, pp 343–349
Calvi LM, Adams GB, Weibrecht KW, Weber JM, Olson DP, Knight MC, Martin RP, Schipani E, Divieti P, Bringhurst FR, Milner LA, Kronenberg HM, Scadden DT (2003) Osteoblastic cells regulate the haematopoietic stem cell niche. Nature 425:841–846
Zhang J, Niu C, Ye L, Huang H, He XI, Tong W-G, Ross J, Haug J, Johnson T, Feng JQ, Harris S, Wiedemann LM, Mishina Y, Li L (2003) Identification of the haematopoietic stem cell niche and control of the niche size. Nature 425:836–841
Malluche HH, Ritz E, Lange HP (1976) Bone histology in incipient and advanced renal failure. Kidney Int 9:355–362
Larsson T, Nisbeth U, Ljunggren O, Juppner H, Jonsson KB (2003) Circulating concentration of FGF-23 increases as renal function declines in patients with chronic kidney disease, but does not change in response to variation in phosphate intake in healthy volunteers. Kidney Int 64:2272–2279
Craver L, Marco MP, Martinez I, Rue M, Borras M, Martin ML, Sarro F, Valdivielso JM, Fernandez E (2007) Mineral metabolism parameters throughout chronic kidney disease stages 1–5–achievement of K/DOQI target ranges. Nephrol Dial Transplant 22:1171–1176
Levin A, Bakris GL, Molitch M, Smulders M, Tian J, Williams LA, Andress DL (2006) Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: Results of the study to evaluate early kidney disease. Kidney Int 71:31–38
Liaw L, Skinner MP, Raines EW, Ross R, Cheresh DA, Schwartz SM, Giachelli CM (1995) The adhesive and migratory effects of osteopontin are mediated via distinct cell surface integrins. Role of αvβ3 in smooth muscle cell migration to osteopontin in vitro. J Clin Invest 95:713–724
Chen NX, O’Neill KD, Duan D, Moe SM (2002) Phosphorus and uremic serum up-regulate osteopontin expression in vascular smooth muscle cells. Kidney Int 62:1724–1731
Li X, Yang HY, Giachelli CM (2008) BMP-2 promotes phosphate uptake, phenotypic modulation, and calcification of human vascular smooth muscle cells. Atherosclerosis 199:271–277
The ADHR consortium (Group 1: White KE, Evans WE, O’Riordan JLH, Speer MC, Econs JJ, Groups 2: Lorenz-Depiereux B, Grabowski M, Meitinger T, Strom TM) (2000) Autosomal dominant hypophosphatemic rickets is associated with mutations in FGF23. Nat Genet 26:345–348
White KE, Jonsson KB, Carn G, Hampson G, Spector TD, Mannstadt M, Lorenz-Depiereux B, Miyauchi A, Yang IM, Ljunggren O, Meitinger T, Strom TM, Juppner H, Econs MJ (2001) The autosomal dominant hypophosphatemic rickets (ADHR) gene is a secreted polypeptide overexpressed by tumors that cause phosphate wasting. J Clin Endocrinol Metab 86:497–500
Shimada T, Muto T, Urakawa I, Yoneya T, Yamazaki Y, Okawa K, Takeuchi Y, Fujita T, Fukumoto S, Yamashita T (2002) Mutant FGF-23 responsible for autosomal dominant hypophosphatemic rickets is resistant to proteolytic cleavage and causes hypophosphatemia in vivo. Endocrinology 143:3179–3182
Goodman WG, Quarles LD (2007) Development and progression of secondary hyperparathyroidism in chronic kidney disease: Lessons from molecular genetics. Kidney Int 74:276–288
Naveh-Many T, Marx R, Keshet E, Pike JW, Silver J (1990) Regulation of 1, 25-dihydroxyvitamin D3 receptor gene expression by 1, 25-dihydroxyvitamin D3 in the parathyroid in vivo. J Clin Invest 86:1968–1975
Silver J, Russell J, Sherwood LM (1985) Regulation by vitamin D metabolites of messenger ribonucleic acid for preproparathyroid hormone in isolated bovine parathyroid cells. Proc Natl Acad Sci USA 82:4270–4273
Wu-Wong JR, Noonan W, Ma J, Dixon D, Nakane M, Bolin AL, Koch KA, Postl S, Morgan SJ, Reinhart GA (2006) Role of phosphorus and vitamin D analogs in the pathogenesis of vascular calcification. J Pharmacol Exp Ther 318:90–98
Mizobuchi M, Finch JL, Martin DR, Slatopolsky E (2007) Differential effects of vitamin D receptor activators on vascular calcification in uremic rats. Kidney Int 72:709–715
Mathew S, Lund RJ, Chaudhary LR, Geurs T, Hruska KA (2008) Vitamin D receptor activators can protect against vascular calcification. J Am Soc Nephrol 19:1509–1519
Mathew S, Strebeck F, Hruska KA (2007) Vascular calcification (VC) protective actions of doxercalciferol in CKD. In: Gendreau MA, Mangili A, Zavod A (eds) Vitamin D therapy in dialysis patients: impact on survival and vascular calcification. Millennium CME Institute, Hampton
Slatopolsky E, Robson AM, Elkan I, Bricker NS (1968) Control of phosphate excretion in uremic man. J Clin Invest 47:1865–1874
Kurz P, Monier-Faugere M-C, Bognar B, Werner E, Roth P, Vlachojannis J, Malluche HH (1994) Evidence for abnormal calcium homeostasis in patients with adynamic bone disease. Kidney Int 46:855–861
Moallem E, Kilav R, Silver J, Naveh-Many T (1998) RNA-protein binding and post-transcriptional regulation of parathyroid hormone gene expression by calcium and phosphate. J Biol Chem 273:5253–5259
Naveh-Many T, Rahamimov R, Livni N, Silver J (1995) Parathyroid cell proliferation in normal and chronic renal failure rats. J Clin Invest 96:1786–1793
Jono S, McKee MD, Murry CE, Shioi A, Nishizawa Y, Mori K, Morii H, Giachelli CM (2000) Phosphate regulation of vascular smooth muscle cell calcification. Circ Res 87:e10–e17
Li X, Yang HY, Giachelli CM (2006) Role of the sodium-dependent phosphate cotransporter, Pit-1, in vascular smooth muscle cell calcification. Circ Res 98:905–912
Brown EM, Gamba G, Riccardi D, Lombardi M, Butters R, Kifor O, Sun A, Hediger MA, Lytton J, Hebert SC (1993) Cloning and characterization of an extracellular Ca2 + -sensing receptor from bovine parathyroid. Nature 366:575–580
Brown EM, Hebert SC (1995) A cloned Ca2+ sensing receptor: a mediator of direct effects of extracellular Ca2+ on renal function? J Am Soc Nephrol 6:1530–1540
Langub MC Jr, Koszewski NJ, Turner HV, Monier-Faugere MC, Geng Z, Malluche HH (1996) Bone resorption and mRNA expression of IL-6 and IL-6 receptor in patients with renal osteodystrophy. Kidney Int 50:515–520
Stenvinkel P, Barany P, Heimburger O, Pecoits-Filho R, Lindholm B (2002) Mortality, malnutrition, and atherosclerosis in ESRD: What is the role of interleukin-6? Kidney Int 61:S103–S108
Simmons EM, Himmelfarb J, Sezer MT, Chertow GM, Mehta RL, Paganini EP, Soroko S, Freedman S, Becker K, Spratt D, Shyr Y, Ikizler TA (2004) Plasma cytokine levels predict mortality in patients with acute renal failure. Kidney Int 65:1357–1365
Pecoits-Filho R, Barany P, Lindholm B, Heimburger O, Stenvinkel P (2002) Interleukin-6 is an independent predictor of mortality in patients starting dialysis treatment. Nephrol Dial Transplant 17:1684–1688
Hruska KA (1998) Growth factors and cytokines in renal osteodystrophy. In: Bushinsky DA (ed) Renal osteodystrophy. Lippincott-Raven, Philadelphia, pp 221–261
Bushinsky DA (1995) The contribution of acidosis to renal osteodystrophy. Kidney Int 47:1816–1832
Krieger NS, Sessler NE, Bushinsky DA (1992) Acidosis inhibits osteoblastic and stimulates osteoclastic activity in vitro. Am J Physiol 262:F442–F448
Alem AM, Sherrard DJ, Gillen DL, Weiss NS, Beresford SA, Heckbert SR, Wong C, Stehman-Breen C (2000) Increased risk of hip fracture among patients with end-stage renal disease. Kidney Int 58:396–399
Cunningham J, Sprague S, Cannata-Andia J, Coco M, Cohen-Solal M, Fitzpatrick L, Goltzmann D, Lafage-Proust MH, Leonard M, Ott S, Rodriguez M, Stehman-Breen C, Stern P, Weisinger J (2004) Osteoporosis in chronic kidney disease. Am J Kidney Dis 43:566–571
Stehman-Breen C (2004) Osteoporosis and chronic kidney disease. Semin Nephrol 24:78–81
Rix M, Andreassen H, Eskildsen P, Langdahl B, Olgaard K (1999) Bone mineral density and biochemical markers of bone turnover in patients with predialysis chronic renal failure. Kidney Int 56:1084–1093
Bonyadi M, Waldman SD, Liu D, Aubin JE, Grynpas MD, Stanford WL (2003) Mesenchymal progenitor self-renewal deficiency leads to age-dependent osteoporosis in Sca-1/Ly-6A null mice. Proc Natl Acad Sci USA 100:5840–5845
Stehman-Breen C (2001) Bone mineral density measurements in dialysis patients. Semin Dial 14:228–229
Stehman-Breen C, Sherrard D, Walker A, Sadler R, Alem A, Lindberg J (1999) Racial differences in bone mineral density and bone loss among end-stage renal disease patients. Am J Kidney Dis 33:941–946
Coco M, Rush H (2000) Increased incidence of hip fractures in dialysis patients with low serum parathyroid hormone. Am J Kidney Dis 36:1115–1121
Hruska KA, Saab G, Mathew S, Lund R (2007) Renal osteodystrophy, phosphate homeostasis, and vascular calcification. Semin Dial 20:309–315
Khosla S, Burr D, Cauley J, Dempster DW, Ebeling PR, Felsenberg D, Gagel RF, Gilsanz V, Guise T, Koka S, McCauley LK, McGowan J, McKee MD, Mohla S, Pendrys DG, Raisz LG, Ruggiero SL (2007) Bisphosphonate-associated osteonecrosis of the jaw: report of a task force of the American society for bone and mineral research. J Bone Miner Res 22:1479–1491
Ichikawa S, Imel EA, Kreiter ML, Yu X, Mackenzie DS, Sorenson AH, Goetz R, Mohammadi M, White KE, Econs MJ (2007) A homozygous missense mutation in human KLOTHO causes severe tumoral calcinosis. J Clin Invest 117:2684–2691
Ichikawa S, Lyles KW, Econs MJ (2005) A novel GALNT3 mutation in a pseudoautosomal dominant form of tumoral calcinosis: Evidence that the disorder is autosomal recessive. J Clin Endocrinol Metab 90:2420–2423
Benet-Pages A, Orlik P, Strom TM, Lorenz-Depiereux B (2005) An FGF23 missense mutation causes familial tumoral calcinosis with hyperphosphatemia. Hum Mol Genet 14:385–390
Schiavi SC, Kumar R (2004) The phosphatonin pathway: New insights in phosphate homeostasis. Kidney Int 65:1–14
Kurosu H, Ogawa Y, Miyoshi M, Yamamoto M, Nandi A, Rosenblatt KP, Baum MG, Schiavi S, Hu MC, Moe OW, Kuro-o M (2006) Regulation of fibroblast growth factor-23 signaling by Klotho. J Biol Chem 281:6120–6123
Acknowledgments
The writing of this manuscript was supported by NIH grants DK070790, and AR41677, and research grants from Shire, Genzyme, Fresenius and Abbott.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hruska, K.A., Choi, E.T., Memon, I. et al. Cardiovascular risk in chronic kidney disease (CKD): the CKD-mineral bone disorder (CKD-MBD). Pediatr Nephrol 25, 769–778 (2010). https://doi.org/10.1007/s00467-009-1337-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-009-1337-0