Abstract
A retrospective study was made on 37 children with idiopathic nephrotic syndrome (INS). At the beginning, all patients were steroid sensitive but received more than one steroid course (median 4). Following several relapses, they became steroid dependent or steroid resistant. Group 1 consisted of 22 children [3 focal segmental glomerulosclerosis (FSGS), 19 minimal-change NS (MCNS)] who received cyclophosphamide (CP) orally for 2.5 ± 0.5 months. Group 2 consisted of 15 children (7 FSGS, 8 MCNS) who received cyclosporine-A (CSA) for 28 ± 15 months. The level of proteinuria decreased significantly and remained low during the follow-up. The relapse-free period was significantly longer in the CP group (CP 30 ± 21.5; CSA 26.2 ± 18 months, p < 0.001). The relapse rate decreased significantly in both groups and remained in this lower level during the follow-up (from 3.4 ± 2.8 to 0.1 ± 0.2/year in group 1, and from 3.7 ± 3.1 to 0.6 ± 0.8/year in group 2). At the end of the 5-year follow-up, 20/22 patients (90.9%) and 10/15 patients (66.6%) were in remission in groups 1 and 2 respectively, with or without treatment (p < 0.05). In the long term, both CP and CSA is effective second-line therapy following steroid monotherapy in INS patients, but the relapse rate was lower and the relapse free period was significantly longer in the CP-treated group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Childhood idiopathic nephrotic syndrome (INS) is often characterized by a relapsing course. Relapses result in the administration of further courses of high-dose corticosteroids, placing the child at the risk of side effects, including obesity, Cushing syndrome, hypertension, bone disease, growth retardation, striae, cataracts, and behavioral disturbances [1]. In the past two decades, alkylating agents such as cyclophosphamide (CP) and chlorambucil (Chl), the immunomodulatory drug levamisole, and calcineurin inhibitors such as cyclosporine A (CSA) have been used as the main steroid-sparing agents. Because of the relatively low prevalence of the disease, it is difficult to establish the precise stage at which a steroid-sparing agent should be introduced or which one should be prescribed to control the disease and minimize steroid toxicity [2]. In idiopathic steroid-dependent NS (SDNS) and frequently relapsing NS (FRNS), cytotoxic therapy is indicated after steroid using, and there is no significant difference between CP and Chl results. CSA can be used in teenage boys to avoid CP gonad toxicity or in children with steroid toxicity and in steroid-resistant NS (SRNS). In FRNS cases, levamisole can be used to reduce relapse rate [3].
CP has been used in nephrology since the 1960s, whereas CSA and levamisole were added to the armamentarium of therapies in 1987, and a consensus guideline for the treatment of NS was published by the British Association of Paediatric Nephrology in 1994 [4].
The alkylating agent CP is widely used in SDNS and FRNS in children, either orally (2–3 mg/kg per day for 8–12 weeks) or in intravenous form (500–750 mg/m2 per month for 6 months) [5]. CP has been shown to prevent progressive scarring within the kidney, preserve renal function, induce remission, and reduce the risk of end-stage renal failure, but it also causes lymphopenia, decreases immunoglobulin secretion, suppresses some T-cell functions, and enhances immune response by inhibiting suppressor T cells.
CSA, a lipophilic decapeptide, is well recognized as being effective in treating children with SDNS or SRNS. Response rates of 50–100% have been reported in the literature when twice-daily dosing of 5–32 mg/kg per day is applied (the usual dose is 5–6 mg/kg per day), with blood levels of 70–500 ng/ml being achieved [6]. Although there is no standard protocol, the initial CSA treatment normally lasts for 1–2 years [7]. Several mechanisms have been postulated to explain CSA-induced reduction in proteinuria in NS, including changes in the properties of the glomerular barrier, resulting in an increased charge and size selectivity [8]; a reduction in glomerular plasma flow or ultrafiltration pressure, which reduces proteinuria on a haemodynamic basis [8]; and the inhibition of interleukin (IL)-2 production [9].
The aim of our study was to compare the effect and long-term outcome of CP and CSA therapy in INS patients who were originally steroid sensitive but after several relapses became SRNS or SDNS.
Patients and methods
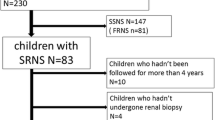
A retrospective study was made of the medical records of 37 children (25 boys, 12 girls) with INS who were admitted to the Department of Pediatrics between 1989 and 2000 (follow-up time 5–13, median 7.1 years). At the start of their disease, all were steroid sensitive, but following several relapses, they became steroid dependent or steroid resistant. Two groups of patients were identified. Group 1 consisted of 22 children (15 boys, 7 girls) age range 2–14 (mean 7.4 ± 3.6) years who received CP first as a second-line immunosuppressive drug because of their NS. Group 2 consisted of 15 children (10 boys, 5 girls) who received second-line treatment with CSA. Their ages at the time of diagnosis lay in the interval of 5–16 (mean: 11.7 ± 4.4) years. Inclusion criteria were age at onset >1 year and ≤18 years, SDNS or SRNS. Definitions were complete remission, reduced urinary protein excretion to ≤0.1 g/day (≤4 mg/m2) for 3 consecutive days; partial remission, decreased urinary protein by ≥50% from the baseline on initial presentation; SRNS, no improvement in proteinuria after 1 month of prednisolone therapy of 60 mg/m2/day; SDNS, at least two relapses during alternate-day steroid treatment or within 14 days after stopping steroid therapy; relapse, proteinuria ≥1.0 g/day (40 mg/m2) for 3 consecutive days.
Renal biopsy was performed in all cases, and it was indicated because we wanted to see the histology before the change of steroid therapy to another immunosuppressant. Biopsy revealed minimal-change nephrotic syndrome (MCNS) in 19 and focal segmental glomerular sclerosis (FSGS) in three patients in group 1. In group 2, FSGS was found in seven and MCNS in eight children.
The initial corticosteroid protocol at the start of NS was prednisolone 60 mg/m2 daily in two divided doses for 4 weeks, followed by 40 mg/m2 in a single dose every other day for 4 weeks, with the dose then being tapered by 10 mg/week according to the recommendations of the International Study of Kidney Disease in Children (ISKDC) protocol [10]. Relapses were treated by the same method in all patients. All patients were steroid sensitive at the first course of treatment, but they became SDNS or SRNS later on. They received more than one steroid course; the median number was four.
CP was introduced at 2–2.5 mg/kg per day orally for 8–12 weeks. Mean duration of CP treatment was 2.5 ± 0.5 (2–3) months. CP therapy was associated with 1 mg/kg oral prednisolone every other day. The mean proteinuria level at the time of diagnosis was 5 ± 3.5 g/day, which became <0.5 g/day during the initial steroid therapy. Before the start of CP treatment, proteinuria level was 3.9 ± 2.9 g/day, endogenous creatinine clearance was 100.4 ± 50 ml/min per 1.73 m2, and the relapse rate was 3.4 ± 2.8/year. The cumulative steroid dose before CP introduction was 6,941 ± 2,891.2 mg/year.
CSA was introduced at 3–5 mg/kg per day. Mean CSA treatment duration was 28 ± 15 (7–60) months. CSA serum drug level was monitored monthly; target concentration levels were 100–200 ng/ml at trough and 800–1,000 ng/ml at peak. CSA therapy was associated with 1 mg/kg prednisolone every other day.
Proteinuria level at the time of diagnosis was 4.5 ± 2.3 g/day and became <0.5 g/day at the end of the first steroid course. Before the start of CSA treatment, the mean proteinuria level was 3.9 ± 2.3 g/day, endogenous creatinine clearance was 86.6 ± 27.3 ml/min per 1.73 m2, and relapse rate was 3.7 ± 3.1/year. Cumulative steroid dose before CSA introduction was 7,656.4 ± 3,517.2 mg/year.
Patients were checked monthly. At each visit, besides clinical assessment, the following were performed in every case: urinalysis, 24-h urinary protein measurement, urinary protein:creatinine ratio, endogenous creatinine clearance was mesured (based upon 24-h urine collection), estimated glomerular filtration rate (eGFR) was calculated with the Schwartz formula: \( GFR = {{k\, \times \,height\left( {cm} \right)} \mathord{\left/ {\vphantom {{k\, \times \,height\left( {cm} \right)} {serum\,creatinine\left( {{{mg} \mathord{\left/ {\vphantom {{mg} {dL}}} \right. \kern-\nulldelimiterspace} {dL}}} \right){\text{,}}\,{\text{where}}\,k = 0.55}}} \right. \kern-\nulldelimiterspace} {serum\,creatinine\left( {{{mg} \mathord{\left/ {\vphantom {{mg} {dL}}} \right. \kern-\nulldelimiterspace} {dL}}} \right){\text{,}}\,{\text{where}}\,k = 0.55}} \), complete blood count, serum creatinine determination, liver function tests, serum lipid profile, and CSA blood concentration determinations. Genetic analysis was not performed. At the start of the study, all patients had normal liver function tests and normal blood count. Endogenous creatinine clearance was initially abnormal in 7/22 patients in the CP and in 5/15 patients in the CSA group.
Statistical analysis
Patients’ clinical data are reported as median and mean ± standard deviation (SD). Statistical analyses included the t tests for comparison of parametric data. The level of statistical significance was taken as p < 0.05.
Results
Tables 1 and 2 present data on the treatment of patients according to histology and clinical course of the disease. Twenty-two INS patients received CP for 2.5 ± 0.5 months in the first course as a second immunosuppressive drug after a remission with steroids was achieved. The average time from the onset of NS to the start of CP therapy was 2.5 ± 2.0 years. Fifteen of the 22 patients also received methylprednisolone pulse therapy before administration of CP. Fifteen children had SDNS and seven had SRNS. Nineteen had MCNS and three had FSGS. Proteinuria decreased from 3.9 ± 2.9 to 0.5 ± 1.4 g/day (p < 0.01) and remained at 0.9 ± 1.7, 5 years later. One patient with FSGS, who had heavy proteinuria (12.8 g/day) at the start of CP, still had 6.2 g/day at the end of the 5-year follow-up. There were three patients with MCNS who developed increasing proteinuria, 1.8, 5.2, and 3.0 g/day, respectively, by this time. Nine patients had a reduced creatinine clearance and were ranged into the National Kidney Foundation Kidney Disease Quality Outcomes Initiative [11] stages for chronic kidney disease (NKF K/DOQI CKD stage III–V) at the end of CP therapy; one normalized by the time of the 5-year follow-up. Eight of 22 patients had an elevated systolic blood pressure (≥120 mmHg) at the end of the 5-year follow-up period.
The relapse-free period was 30 ± 21.5 months (29.9 ± 21.5 months in SDNS and 30.3 ± 23.3 months in SRND patients). The relapse rates decreased significantly from 3.4 ± 2.8 to 0.5 ± 0.6/year during the first course of CP therapy and remained at this level (0.1 ± 0.2/year) during the 5-year follow-up (p < 0.001). At the end of follow-up, five patients were in remission (<0.4 g /day proteinuria, ≥80 ml/min per 1.73 m2 creatinine clearance) with immunosuppressive therapy. In relation to CP therapy, 3/22 children had nausea, 2/22 had reversible hair loss, 1/22 had leucopenia, and 1/22 alopecia.
Fifteen patients received CSA for an average of 28 ± 15 months in the first course as a second immunosuppressive drug after a remission with steroids had been achieved. Twelve of the 15 patients also received methylprednisolone pulse therapy before administration of CSA. Time from diagnosis to the start of CSA treatment was 3.5 ± 3 years. Eight children had SDNS and seven SRNS. Seven had FSGS and eight MCNS. Proteinuria decreased significantly (at the start of CSA treatment, it was 3.9 ± 2.3 g/day, whereas at the end of CSA treatment, it was 0.9 ± 1.4 g/day, p < 0.01; 5 years later, it was 0.7 ± 1.6 g/day). Creatinine clearance and eGFR did not significantly change during the 2-year follow-up but increased at the end of the study. Two patients with FSGS and one with MCNS did not respond to this CSA course: proteinuria was 3.5; 2.5, and 4.4 g/day, respectively. Proteinuria increased further in an FSGS case, to 6.1 g/day 5 years after the first CSA period, whereas in the other FSGS and the MCNS patient, a further course of CSA treatment resulted in a decrease in proteinuria to 0.4 and 0.5 g/day, respectively. After 5-years of follow-up, eGFR deceased <15 ml/min per 1.73 m2 in two FSGS patients. In these patients marked, hypertension had also developed. The relapse-free period was 26.2 ± 18 months (28.1 ± 22.4 months in SDNS and 24 ± 12.7 months in SRNS patients). Relapse rates significantly decreased, from 3.7 ± 3.1 to 0.9 ± 0.5/year during the first CSA course and remained at this lower level (0.6 ± 0.8/year) during the follow-up (p < 0.001). At the end of follow-up in the CSA group, four patients were in remission (<0.4 g/day proteinuria, ≥80 ml/min per 1.73 m2 creatinine clearance) with immunosuppressant therapy. During CSA treatment, 3/15 patients exhibited hirsutism, 2/15 tremor, 2/15 gingival hyperplasia, and 1/15 nausea and appetite loss.
Table 3 represents the further therapy after the examined period. In the CP group, CSA was introduced when CP results were not sufficient (6/22). Four of 22 patients received prednisolone/mycophenolate mofetil therapy as immunosuppression after CP. In the CSA group, 5/15 patients received more than one CSA course, and 4/15 needed other immunosuppressive therapy. One patient in each group needed renal replacement therapy at the end of the 5-year follow-up.
Figure 1 shows the clinical course according to the histology of patients in remission or in relapse during the follow-up period.
Clinical course of CP- and CSA-treated patients after 5 years’ follow-up. CP cyclophosphamide, CSA cyclosporine-A, SDNS steroid-dependent nephrotic syndrome, SRNS steroid-resistant nephrotic syndrome, RRT renal replacement therapy, MCNS minimal-change nephrotic syndrome, FSGS focal segmental glomerular sclerosis
Discussion
Our retrospective study documents that the long-term results of CP treatment in SDNS and SRNS in childhood are at least as effective as those for CSA.
Clinical course of nephrotic syndrome
In our study, CP treatment duration was 2.5 ± 0.5 months, and the relapse-free period was 30.05 ± 21.5 months (in 5/22 patients ≥60 months). Eighteen of the 22 patients (82%) had a relapse-free period of more than a year following CP therapy without other immunosuppressive treatment, and altogether, 10/22 patients (48%) did not need further immunosuppressive treatment until the end of the fifth year. Of the CP-treated patients, 45.5% were in complete and 36.3% in partial remission after the 5-year follow-up (81.8% altogether). Further immunosuppressive therapy was needed in 12/22 patients because of relapses.
In our CSA-treated group, CSA treatment duration was 28 ± 15 months (7–60 months). The relapse-free period following the start of CSA therapy was 26.2 ± 18 months (in 2/15 patients it was ≥60 months). Of the CSA-treated patients, 46.6% were in complete and 46.6% in partial remission (93.2% altogether) at the end of the 5-year follow-up, and 33% (5/15 patients) did not need therapy. Because many patients relapsed, their treatment was resumed or changed (see Table 3). Nevertheless, 9/15 patients still needed maintenance immunosuppressant therapy from the beginning until the end of the 5-year follow-up.
At the end of the fifth year, 10/15 patients were in remission (66.6%) in the CSA group and 15/22 (66.2%) in the CP group. The difference between the relapse-free period and relapse rates after the first CP or CSA period was significant in the 2-year and 5-year follow-up period, with much rarer relapses following CP therapy (p < 0.05). When estimating our results, we found that partial remission did not equal complete remission and might finally not turn out beneficial for the patients.
Renal function, proteinuria, and hypertension
Compared with the CSA group, a significant decrease in creatinine clearance was seen in patients who were treated with CP first after steroids, at the end of CP treatment, and 2 years after CP therapy, but this change was reversible and disappeared after 5 years. Endogenous creatinine clearance and eGFR also showed a significant increase in the CSA-treated group after the 5 years of follow-up. In the CP-treated group, a significantly higher proportion of patients had <0.4 g/day proteinuria (16/22 patients, 72.7%) than those in CSA therapy (9/15 patients, 60%) at the end of the 5-year follow-up. At this time, blood pressure was significantly lower after CP than following CSA therapy.
Renal histology
FSGS is an indicator for poor prognosis: 6/10 patients relapsed, 3/10 patients developed end-stage renal failure and needed renal replacement therapy, and only 1/10 patients was in remission at the end of the fifth year with FSGS histology. In FSGS, the likelihood of remission is much lower than in MCNS, which should make a mixture of these two groups obsolete. The weakness of our study is that whereas in the CSA group we had 7/15 FSGS patients, there were only 3/25 FSGS in the CP-treated group, and genetic studies were not performed. Although our patients had documented steroid sensitivity at the onset, the histology and the refractory course ending in end-stage renal disease in some patients suggests that a subgroup might have had a resistant or very poor response to steroids initially.
Adverse events
The types of side-effects during CP and CSA therapy were different. CP therapy applied for less than 3 months was not associated with more side-effects than was CSA treatment. Any complications in the two treatment groups proved to be reversible, though none of our patients received more than one course of CP therapy. There were no patients who needed hospitalization due to severe infections during the administration of oral CP or CSA.
The known side effects of CSA in the long term should be taken into account in the treatment decision. Its use for more than 1 year can result in chronic nephrotoxicity in 17–60% of patients [6] (i.e. CSA-associated arteriolopathy, tubulointerstitial lesions, and focal glomerular lesions [12]). Other side effects include hypertension, gingival hyperplasia, and hirsutism. Lijima et al. reported that CSA treatment duration and duration of heavy proteinuria during CSA treatment were independent risk factors for the development of CSA-induced tubulointerstitial lesions in children with MCNS who had been treated with long-term moderate-dose CSA [13]. Also, when using cyclophosphamide, the physician also must take into account the potential risk of infertility, cardiac disease, and late cancer [14].
Cyclophosphamide or cyclosporine A for treatment?
Studies in which alkylating agents and CSA have been compared have led to the conclusion that a course of cytotoxic drug leads to a higher rate of cumulative sustained remission compared with CSA [15, 16]. Pena et al. achieved high remission rates (73.3%) in histologically proven MCNS and FSGS SRNS patients using methylprednisolone pulses and alkylating agents (CP, Chl) together. They also concluded that initial steroid resistance is a poor prognostic factor compared with late-onset steroid resistance [17]. Our patients were steroid sensitive at the beginning, which can explain our better results.
The efficiency of CP and Chl in patients with SDNS, SRNS, and FRNS is defined by remission duration. The effect of cytotoxic drug therapy in steroid-sensitive NS (SSNS) depends on several factors, such as the underlying glomerular disorder, e.g. MCNS, mild mesangial proliferation, immunoglobulin (Ig)M glomerulopathy [13, 18–20], FSGS, steroid sensitivity, FRNS or SDNS course of NS [21], type of cytotoxic drug [22], drug dose [14, 23], treatment duration [24], and concomitant drug therapy [18].
The reported remission rates after cytotoxic therapy vary from 0% after 12 months to about 30% after 5 years [25, 26]. In approximately 10% of the patients, however, NS may relapse during cytotoxic treatment. The applied CP dose varies from 105 to 588 mg/kg body weight cumulatively [27–29]. Higher dosages are associated with a higher chance of relapse-free intervals, although the risk of side-effects increases. According to the meta-analysis of cytotoxic treatment in FRNS children published by Latta et al., remission lasted for a maximum of 57 months after the first course of cytotoxic therapy, and the overall relapse-free survival after 4 years is <50%. On average, studies on FRNS result in remission rates of 72% after 2 years and 36% after 5 years; rates for SDNS are 40% and 24%, respectively [30]. Second courses of cytotoxic therapy are reported to increase the rate of long-lasting remissions [31–33]. We gave a CP dose of 112–168 mg/kg cumulatively in one course, and we did not apply a second CP course in any of the NS patients. Our better results may partially be explained by the fact that our patients had SSNS at the start of the disease.
In the study by Cattran et al., 49 SRNS FSGS patients were treated with CSA + low-dose prednisolone and compared with low-dose prednisolone + placebo and followed for 200 weeks. They found 70% of the treatment group vs. 4% of the placebo group had a partial or complete remission by 26 weeks. Relapse occurred in 40% of patients by week 52 and in 60% by week 78, but the remainder stayed in remission to the end of 200 weeks. There was a decrease of 50% in baseline creatinine clearance in 25% of the treated group compared with 52% of the controls [34].
In the Cochrane Review, eighteen trials involving 828 children were identified. CP and Chl significantly reduced the relapse risk at 6–12 months compared with prednisolone alone. In the single Chl vs. CP trial, no difference in relapse risk was observed at 2 years. CSA was as effective as CP and Chl, but the effect was not sustained when CSA was ceased. The reviewers concluded that an 8-week course of CP or Chl and prolonged courses of CSA reduce the risk of relapse in children with relapsing SSNS compared with corticosteroids alone. Meanwhile, the choice of agent depends on the physician and patient preferences related to therapy duration and the type and frequency of complications [35].
Kemper et al. reported that SDNS can recur in patients despite CSA maintenance therapy [36], and despite its efficacy, the majority of patients relapse if CSA is stopped [12, 37–39].
The effect of other alternative treatments before using cytotoxic drugs—such as alternate-day steroids or levamisole—was not examined in this paper. We previously published our results with levamisole in FRNS, SSNS, and SDNS [3].
In summary, in the long term, both CP and CSA are effective second-line therapies following steroid monotherapy in INS patients, but the relapse rate is lower and the relapse-free period significantly longer in the CP-treated group. An important message of our study is that most children who have a difficult course of nephrotic syndrome after an initial remission induced by steroids do well 7–8 years after presentation. A good remission rate can be achieved after 5 years following initial CP and CSA therapy, and the incidence of side effects is low.
On the other hand, our study is finally not able to give an answer to the question as to which is the better treatment in the examined patient population because it is a retrospective study with unequal distribution of FSGS in the different treatment groups. In addition, no genetic studies were performed, which means that about 10% of our patients are expected to have a genetic disorder.
References
Ehrich JH, Brodehl J (1991) Long versus standard prednisolone therapy for initial treatment of idiopathic nephrotic syndrome in children (Arbeitsgemeinschaft für Padiatrische Nephrologie). Eur J Pediatr 150:380–387
Abeyagunawardena AS, Dillon MJ, Rees L, van’t Hoff W, Trompeter RS (2003) The use of steroid-sparing agents in steroid-sensitive nephrotic syndrome. Pediatr Nephrol 18:919–924
Sümegi V, Haszon I, Ivanyi B, Bereczki Cs, Papp F, Turi S (2004) Long-term effects of levamisole treatment in childhood nephrotic syndrome. Pediatr Nephrol 19:1354–1360
Report of a workshop by the British Association for Paediatric Nephrology and Research Unit, Royal College of Physicians (1994) Consensus statement on management and audit potential for steroid responsive nephrotic syndrome. Arch Dis Child 71:151–157
Bircan Z, Kara B (2003) Intravenous cyclophosphamide is the drug of choice for steroid dependent nephrotic syndrome. Pediatr Int 45:65–67
Chisthi AS, Solof JM, Brewer ED, Kale AS (2001) Long-term treatment of focal segmental glomerulosclerosis in children with cyclosporine given as a single daily dose. Am J Kidney Dis 38:754–760
Eddy AA, Symons JM (2003) Nephrotic syndrome in childhood. Lancet 362:629–639
Zietse R, Derkx FH, Schalekamp MA, Weimar W (1995) Cyclosporine and the glomerular filtration barrier in minimal change disease and membranous nephropathy. Contrib Nephrol 114:6–18
Borel JF, Feurer C, Gubler HU, Stahelin H (1994) Biological effects of cyclosporine A: A new antilymphocytic agent. 1976. Agents Actions 43:179–186
Abramowicz M, Barnett HL, Edelmann CM Jr, Greifer I, Kobayashi O, Arneil GC, Barron BA, Gordillo-P G, Hallman N, Tiddens HA (1970) Controlled trial of azathioprine in children with nephrotic syndrome. A report for the international study of kidney disease in children. Lancet 1:959–961
Hogg RJ, Furth S, Lemley KV, Portman R, Schwartz GJ, Coresh J, Balk E, Lau J, Levin A, Kausz AT, Eknoyan G, Levey AS; National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative (2003) National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative clinical practice guidelines for chronic kidney disease in children and adolescents: evaluation, classification, and stratification. Pediatrics 111:1416–1421
Hamahira K, Iijima K, Tanaka R, Nakamura H, Yoshikawa N (2001) Recovery from cyclosporine-associated arteriolopathy in childhood nephrotic syndrome. Pediatr Nephrol 16:723–727
Lijima K, Hamahira K, Tanaka R, Kobayashi A, Nozu K, Nakamura H, Yoshikawa H (2002) Risk factors for cyclosporine-induced tubulointerstitial lesions in children with minimal change nephrotic syndrome. Kidney Int 61:1801–1805
McCrory WW, Shibuya M, Lu WH, Lewy JE (1973) Therapeutic and toxic effects observed with different dosage programs of cyclophosphamide in treatment of steroid-responsive but frequently relapsing nephrotic syndrome. J Pediatr 82:614–618
Ponticelli C, Edefonti A, Ghio L, Rizzoni G, Rinaldi S, Gusmano R, Lama G, Zacchello G, Confalonieri R, Altieri P, Bettinelli A, Maschio G, Cinotti GA, Fuiano G, Schena FP, Castellani A, Della Casa-Alberighi O (1993) Cyclosporine versus cyclophosphamide for patients with steroid-dependent and frequently relapsing idiopathic nephrotic syndrome: a multicentre randomized controlled trial. Nephrol Dial Transplant 8:1326–1332
Niaudet P (1992) Comparison of cyclosporine and chlorambucil in the treatment of steroid-dependent idiopathic nephrotic syndrome: a multicentre randomized controlled trial. The French Society of Paediatric Nephrology. Pediatr Nephrol 6:1–3
Pena A, Bravo J, Melgosa M, Fernandez C, Meseguer C, Espinosa L, Alonso A, Navarro M (2007) Steroid-resistant nephritic syndrome: long-term evolution after sequential therapy. Pediatr Nephrol 22:1875–1880
Grupe WE, Heymann W (1966) Cytotoxic drugs in steroid-resistant renal disease. Alkylating and antimetabolic agents in the treatment of nephrotic syndrome, lupus nephritis, chronic glomerulonephritis, and purpura nephritis in children. Am J Dis Child 112:448–458
Querfeld U, Waldherr R, Scharer K (1985) The significance of focal global sclerosis in idiopathic nephratic nephrotic syndrome. Long-term clinical observations. Acta Paediatr Scand 74:913–919
Report of the International Study Group of Kidney Disease in Children (1974) Prospective, controlled trial of cyclophosphamide therapy in children with the nephrotic syndrome. Lancet 2:423–427
Geary DF, Farine M, Thorner P, Baumal R (1984) Response to cyclophosphamide in steroid-resistant focal segmental glomerulosclerosis: a reappraisal. Clin Nephrol 22:109–113
Arbeitsgemeinschaft für Pädiatrische Nephrologie (1982) Effect of cytotoxic drugs in frequently relapsing nephrotic syndrome with and without steroid dependence. N Engl J Med 306:451–454
Williams SA, Makker SP, Ingelfinger JR, Grupe WE (1980) Long-term evaluation of chlorambucil plus prednisone in the idiopathic nephrotic syndrome of childhood. N Engl J Med 302:929–933
Arbeitsgemeinschaft für Pädiatrische Nephrologie (1987) Cyclophosphamide treatment of steroid dependent nephrotic syndrome: comparison of eight week with 12 week course. Report of Arbeitsgemeinschaft für Pädiatrische Nephrologie. Arch Dis Child 62:1102–1106
Drummond KN, Hillman DA, Marchessault JH, Feldman W (1968) Cyclophosphamide in the nephrotic syndrome of childhood: its use in two groups of patients defined by clinical, light microscopic and immunopathologic findings. Can Med Assoc J 98:524–531
Moncrieff MW, White RH, Oggs CS, Cameron JS (1969) Cyclophosphamide therapy in the nephrotic syndrome in childhood. Br Med J 1:666–671
Rance CP, Arbus GS, Balfe JW (1976) Management of the nephrotic syndrome in children. Pediatr Clin North Am 23:735–750
Dundon S, O’Callaghan U, Raftery J (1980) Stability of remission in minimal lesion nephrotic syndrome after treatment with prednisolone and cyclophosphamide. Int J Pediatr Nephrol 1:22–25
Griswold WR, Kaufman DB, Smith FG, McIntosh RM (1971) Cyclophosphamide in nephrotic syndrome. Clin Res 19:233
Latta K, von Schnakenburg C, Ehrich JH (2001) A meta-analysis of cytotoxic treatment for frequently relapsing nephrotic syndrome in children. Pediatr Nephrol 16:271–282
Barratt TM, Soothill JF (1970) Controlled trial of cyclophosphamide in steroid-sensitive relapsing nephrotic syndrome of childhood. Lancet 2:479–482
Ghose S, Kumar M, Kundu B, Bindal S (1977) Long-term follow up of steroid and cyclophosphamide therapy in nephrosis. Indian Pediatr 14:885–889
Grushkin CM, Fine RN, Heuser E, Lieberman E (1970) Cyclophosphamide therapy of idiopathic nephrosis. Calif Med 13:1–5
Cattran DC, Appel GB, Hebert LA, Hunsicker LG, Pohl MA, Hoy WE, Maxwell DR, Kunis CL (1999) A randomized trial of cyclosporine in patients with steroid-resistant focal segmental glomerulosclerosis. Kidney Int 56:2220–2226
Durkan A, Hodson E, Willis N, Craig J (2003) Non-corticosteroid treatment for nephrotic syndrome in children (Cochrane Review) The Cochrane Library. 1. Oxford, Update Software Ltd
Kemper MJ, Kuwertz-Broeking E, Bulla M, Mueller-Wiefel DE, Neuhaus TJ (2004) Recurrence of severe steroid dependency in cyclosporin A-treated childhood idiopathic nephrotic syndrome. Nephrol Dial Transplant 19:1136–1141
Ingulli E, Singh A, Baqi N, Ahmad H, Moazami S, Tejani A (1995) Aggressive, long-term cyclosporine therapy for steroid-resistant focal segmental glomerulosclerosis. J Am Soc Nephrol 5:1820–1825
Sairam VK, Kaila A, Rajaraman S, Travis LB (2002) Secondary resistance to cyclosporin A in children with nephrotic syndrome. Pediatr Nephrol 17:842–846
Waldo FB, Benfield MR, Kohaut EC (1998) Therapy of focal and segmental glomerulosclerosis with methylprednisolone, cyclosporine A, and prednisone. Pediatr Nephrol 12:397–400
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sümegi, V., Haszon, I., Bereczki, C. et al. Long-term follow-up after cyclophosphamide and cyclosporine-A therapy in steroid-dependent and -resistant nephrotic syndrome. Pediatr Nephrol 23, 1085–1092 (2008). https://doi.org/10.1007/s00467-008-0771-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-008-0771-8