Abstract
The aim of the study was to analyze systematically our observation that children with severe nephrotic syndrome (NS) have hyperphosphatemia despite normal kidney function. Forty-seven children with NS and normal glomerular filtration rate (GFR) were studied [26 with steroid-sensitive nephrotic syndrome (SSNS) and 21 with persistent NS]. The plasma phosphate level was expressed as the number of standard deviations (SDs) from the mean levels in age- and gender-matched controls. In SSNS plasma phosphate concentration was elevated (+3.7±2.0 SDs) during relapse and normalized (−0.7±1.7 SDs) in remission. In persistent NS the phosphate level was +4.0±2.1 SDs. Patients with marked hyperphosphatemia (>4 SDs) were younger (p<0.001), had lower plasma albumin (p<0.001), and had higher urinary protein levels (p<0.05). Hyperphosphatemia did not correlate with GFR, plasma calcium, or urinary sodium levels. Children with persistent NS had decreased serum 25(OH)D3 and insulin-like growth factor 1 (IGF-1) concentrations. Hyperphosphatemia is prevalent among children with persistent nephrotic syndrome and normal renal function, correlates with its severity, and may result from increased urinary IGF-1 wasting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hyperphosphatemia (HPH) is a recognized feature of chronic renal failure and is due to a decrease in glomerular filtration rate (GFR). Plasma phosphate levels usually increase once GFR falls below 30% of normal values [1]. In tumor lysis syndrome HPH results from cytolysis, which is enhanced by cytotoxic agents, but may also be precipitated by acute renal failure [2, 3]. HPH is only infrequently encountered without renal function impairment; it may be a sign of the various forms of hypoparathyroidism or of the rare syndrome of tumoral calcinosis [4, 5]. Transient hyperphosphatemia has been reported during severe dehydration episodes with intravascular volume depletion [6, 7]. Importantly, HPH has been implicated as having an independent role in progression of renal diseases [8, 9], and strict control of serum phosphate concentration in this context is therefore highly recommended.
We recently noted that HPH is a consistent finding among children with nephrotic syndrome (NS), who have normal renal function. The following study was conducted in order to systematically study this observation.
Patients and methods
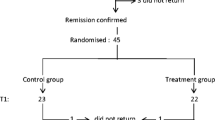
Forty-seven children with nephrotic syndrome and normal kidney function (GFR >100 ml/min per 1.73 m2) aged 6.5±0.6 years (range: 1–13.5) were studied retrospectively. All of these patients were treated in our center between 1997 and 2004. Twenty-six patients (31 relapses) suffered from steroid-sensitive nephrotic syndrome (SSNS). All of them responded to corticosteroids within 2 weeks of initiation of treatment. Twenty-one patients had persistent NS due to various etiologies (Table 1). Patients with mutations of podocin or nephrin and diffuse mesangial sclerosis were treated with steroids for a brief period of time until the exact diagnosis was established. The remaining patients who failed to respond to a 6-week course of daily steroids (oral and/or parenteral) were defined as having steroid-resistant NS (SRNS). In relapse, all patients had nephrotic range proteinuria (>40 mg/m2 per h) and hypoalbuminemia (<2.5 g/dl). Remission was defined as trace or negative urine protein on dipstick analysis. Plasma phosphate and other biochemical parameters used for this study were obtained from the records during periods of time when patients were off diuretics, calcium salts, corticosteroids, or cyclosporin A. None of the patients received vitamin D derivatives. Two patients received occasional intravenous albumin infusions to treat symptomatic edema. All children were on an unrestricted protein diet.
Creatinine clearance (Ccr) was calculated according to the Schwartz formula [10].
For each patient with persistent NS there were 3–70 (mean: 15.0±16.7) measurements of plasma phosphate, creatinine, total protein (TP), albumin, total calcium, and sodium as well as 1–10 measurements of serum ionized calcium, urinary phosphate, and sodium concentrations and total protein to creatinine ratio (TP/Cr). In children with SSNS there were 1–3 (mean: 1.45±0.74) measurements (according to the number of relapses), performed prior to initiation of corticosteroid therapy. Serum parathyroid hormone (PTH) was measured in 27 children (1–7 measurements). In general, fewer blood samples were drawn off treatment in patients who received immunosuppressive medications for prolonged periods. The highest number of blood tests was obtained in patients who did not receive immunosuppressive therapy at all and had normal kidney function for several years. Serum levels of 1,25(OH)2D and 25(OH)D were measured in 11 children and serum insulin-like growth factor 1 (IGF-1) in 10 patients.
Patients were classified as hyper- or normophosphatemic according to their mean plasma phosphate concentration. Correlation analysis was performed using biochemical parameters which were derived from the same blood sample and from a simultaneously obtained urine sample.
Because serum phosphate level is age and gender dependent, we expressed it as the number of standard deviations (SDs) from the mean value in age- and gender-matched controls: the first control group [11]. The second control group consisted of 63 healthy children of comparable age with normal renal function [determined by serum creatinine (Scr) and blood urea nitrogen (BUN)], referred to the emergency room of our hospital for evaluation of mild acute illnesses excluding urinary tract infections.
Serum IGF-1 levels, which are also age dependent, were analyzed only among children aged 1–5 years, because only during this age period is the normal range of IGF-1 constant.
Biochemical parameters (phosphate, calcium, creatinine, total protein, albumin, sodium) were determined with Vitros 750/950 Chemistry System (Ortho-Clinical Diagnostics, Johnson & Johnson, Raritan, NJ, USA), ionized calcium with AVL OMNI (Medical Instruments, Graz, Austria), urine total protein with pyrogallol red colorimetric method (Sentinel Diagnostics, Milan, Italy), PTH by immunoradiometric assay (N-tact PTH SP IRMA, DiaSorin, Stillwater, MN, USA), and IGF-1 by enzyme-labeled chemiluminescent immunometric assay (Immulite 2000 Analyzer, Diagnostic Products, Los Angeles, CA, USA).
Statistical analysis
Data are presented as mean±SD, unless otherwise noted. For each patient the mean value of each parameter was used. Correlations were detected by principal component analysis, clustering of variables, univariate and multivariate regression analysis. For comparison between groups we used a paired or unpaired t-test as appropriate.
Results
All patients with a mild illness, the second control group, had plasma phosphate levels comparable to those of healthy children (first control group). Their plasma phosphate concentrations were all within ±2 SDs (Fig. 1). In contrast, only 9 of 47 (17.3%) children with NS studied had plasma phosphate levels within 2 SDs of the normal mean values. Mean plasma phosphate concentrations were above 2 SDs in 82.7% of nephrotic patients and above 4 SDs in 46.1% of them.
Plasma phosphate levels in nephrotic patients and control children with mild diseases. MD mild diseases controls, MCNS minimal change nephrotic syndrome, NS nephrotic syndrome. Phosphate levels are expressed as number of standard deviations (SDs) from the mean values in age- and gender-matched controls (1)
In SSNS, the mean plasma phosphate level was elevated at +3.7±2.0 SDs during relapse and normalized once remission was attained (−0.7±0.54 SDs, p<0.001; Fig. 1). In persistent NS, plasma phosphate concentration was +4.0±2.1 SDs and, as in SSNS, it was significantly higher than in the second control group (p<0.001; Fig. 1).
In order to demonstrate a difference in the absolute values of plasma phosphate between nephrotic patients and their age-matched control group, a subgroup of patients aged 1–5 years was analyzed. Within this group, mean plasma phosphate concentrations in children with persistent NS (6.4±0.35 mg/dl) and with SSNS (5.8±0.47 mg/dl) were significantly higher than in patients with mild illnesses and healthy controls (4.7±0.55 mg/dl and 4.85±0.27 mg/dl, respectively, p<0.001) (Fig. 2). Among 212 measurements of plasma phosphate in children aged 1–5 years with persistent NS, 5.6% were above 8 mg/dl, 14.2% were 7–7.9 mg/dl, 45.8% were 6–6.9 mg/dl, and only 34.4% were 5–5.9 mg/dl.
In order to determine clinical and laboratory features relevant to the degree of HPH in nephrotic children, various parameters were compared between patients with markedly elevated mean plasma phosphate levels (>4 SDs) and those with plasma phosphate concentration <4 SDs. This analysis was performed separately for children with SSNS and those with persistent NS (Table 2). Plasma total calcium levels in nephrotic patients were below the normal range, but did not differ between the two nephrotic groups. Ionized calcium concentrations were within normal range (1.23±0.048). There was no correlation between serum phosphate concentrations and GFR or PTH levels. Tubular reabsorption of phosphate (TRP) was found to be slightly higher in patients with HPH in both groups.
Within the SSNS group, children with marked HPH and those with normal or only mildly elevated plasma phosphate levels were of similar age and had comparable plasma albumin, total protein, and calcium concentrations, as well as creatinine clearance and urinary protein excretion (Table 2). In contrast, within the persistent NS group, children with marked HPH were much younger (p<0.001), had lower plasma albumin levels (p<0.001), and more severe proteinuria (p<0.05) compared to children with only slightly elevated or normal plasma phosphate levels. Overall then, marked HPH in children with normal renal function was associated with the severity of nephrotic syndrome but was independent of plasma total calcium concentration and GFR.
The etiology of NS differed between these two subgroups (Table 1): most of the patients with persistent NS and marked HPH suffered from kidney diseases resulting from genetic defects of the glomerular barrier including homozygous mutations of podocin (R138X) in five and congenital NS of the Finnish type due to mutation in NPHS1 in one. In addition, two patients had diffuse mesangial sclerosis and one had focal segmental glomerulosclerosis (FSGS). The subgroup of patients with milder hyperphosphatemia included older children with primary FSGS or other glomerular diseases such as membranoproliferative glomerulonephritis (GN), Henoch-Schönlein purpura, mesangioproliferative GN, Alport’s syndrome, or amyloidosis due to familial Mediterranean fever. Only one child in this subgroup suffered from steroid-resistant nephrotic syndrome due to a homozygous mutation of podocin.
We further investigated a homogeneous subgroup of eight children who fulfilled several inclusion criteria: persistent NS due to structural defects of the glomerular barrier (mutations of podocin or nephrin), not treated with immunosuppressants, age 1–5 years, and a large number of recorded tests (at least 12 samples drawn at 2–3 week intervals). Mean plasma phosphate levels were markedly elevated in all patients in this group (Fig. 3), with individual values ranging between 5.2 and 8.0 mg/dl. During the study period mean Ccr was 184.7±54.9 ml/min per 1.73 m2, and mean plasma creatinine level was 0.27±0.09 mg/dl. The mean time period between the first and last measurement was 21.9±16.6 (6.9–51.5) months. Plasma phosphate levels were found to be independent of the time period since its first measurement (r=−0.14), plasma creatinine (r=−0.11), Ccr (r=−0.04), total calcium (r=+0.28), calcium corrected for plasma albumin (r=+0.29), urinary sodium (r=+0.17), and PTH (r=−0.20). Principal component and multivariate analyses confirmed the absence of correlation between plasma phosphate and the above indicated biochemical parameters. However, in these young children with the most severe form of NS there was no longer a correlation between plasma phosphate and total protein (r=−0.007), albumin (r=+0.083), and urinary protein (TP/Cr ratio: r=−0.3, p=0.06). Serum IGF-1 levels were found to be very low in all the children of this group with a mean level of 2.7±2.2 nmol/l (normal range: lower limit=6.5–7.1 nmol/l, and upper limit=37.2–42.5 nmol/l).
Patients with persistent NS had a low mean level of 25(OH)D3, which was especially pronounced in those with marked HPH (2.1±0.2 ng/ml). The mean 1,25(OH)2D value was within normal range in children with mild (23±14.8 pg/ml) and significant (21+11.8 pg/ml) HPH. The mean serum PTH level was normal in patients with SSNS and persistent NS with normal creatinine clearance. There was no significant difference in PTH levels between patients with and without HPH (Table 2). There was no correlation between PTH and plasma total calcium levels (r=−0.038) in nephrotic patients with normal kidney function.
Discussion
We found hyperphosphatemia to be a common feature among children with NS with completely normal kidney function. In children with SSNS plasma phosphate levels were elevated during relapse and normalized in remission. Among all patients with persistent NS, HPH correlated with the severity of NS and with young age. Persistent HPH was most prevalent among the subgroup of younger children with heavy proteinuria and low plasma albumin levels, most of whom had a genetic defect of the glomerular barrier. In this subgroup of children with the most severe form of NS and marked HPH, there was no longer a correlation between plasma phosphate concentration and the degree of proteinuria or plasma albumin. Among all nephrotic patients, plasma phosphate level did not correlate with serum calcium or PTH levels, urinary sodium concentration, or creatinine clearance.
The exact pathogenesis of HPH in NS is unclear. The influence of low total plasma calcium levels was excluded: there was no correlation between plasma phosphate level and total (or corrected for plasma albumin) calcium level. Repeated measurements of ionized calcium were normal in all patients.
Although exact measurement of GFR in nephrotic children is problematic, and actual GFR may be lower than estimated by creatinine clearance, we believe that the mean value of Ccr (165 ml/min per 1.73 m2) among patients with persistent HPH is high enough to exclude a decrease in GFR as a cause for HPH.
All nephrotic patients were on an unrestricted protein diet. We did not intentionally use high or low protein diets and since all patients were off steroid therapy they have not had markedly increased appetite. It is therefore unlikely that dietary phosphate intake played a major role in determining the degree of hyperphosphatemia.
One of the main mechanisms of regulation of plasma phosphate concentration is its proximal tubular reabsorption, which is known to be sodium dependent [12, 13]. Severe NS is often accompanied by intravascular volume depletion with increased tubular sodium and probably phosphate reabsorption, which could cause HPH. Alternatively, massive proteinuria per se could result in increased sodium and phosphate reabsorption [14]. In our study, TRP was high in most children with HPH, but there was no correlation between urinary sodium and plasma phosphate level. Thus, HPH in our patients cannot be attributed to enhanced urinary sodium reabsorption related to intravascular volume depletion or to mishandling of sodium by nephrotic kidneys. The mechanism suggested for transient HPH, described in severely dehydrated children (>10%) with acute diarrhea [6], is redistribution of phosphate and calcium between the intra- and extracellular space. In contrast to our patients, a strong correlation between HPH and hypocalcemia was found.
HPH may be caused by IGF-1-induced increase of phosphate transport in proximal tubules. Decreased serum IGF-1 levels in our nephrotic patients are in accordance with the results of experimental studies in rats with doxorubicin-induced NS [15] as well as with clinical data on low IGF-1 concentration in NS [16–18]. This may result, at least in part, from urinary excretion of IGF-1 with its carrier proteins [15, 16]. Nephron micropuncture studies showed that proximal tubular fluid of nephrotic rats contains IGF-1 at biologically meaningful concentrations, in contrast to normal animals [19]. IGF-1 was shown to stimulate marked phosphate reabsorption in the proximal convoluted tubule. This was demonstrated by in vitro microperfusion experiments [20], in proximal tubular cell culture [21], and by intravenous infusion of IGF-1 to healthy volunteers which resulted in a decrease in urinary phosphate excretion [22]. IGF-1-induced increase in tubular phosphate reabsorption seems to be a very probable mechanism of HPH in nephrotic patients. We were unable to measure IGF-1 in urine samples and therefore could not confirm this hypothesis.
Low serum 25(OH)D concentrations may result from urinary loss with its corresponding binding proteins [23].
In SSNS, HPH usually does not persist beyond 1–2 weeks, is clinically silent, and does not require treatment. In chronic NS, persistent HPH should be corrected in order to decrease the calcium-phosphate product and prevent early development of secondary hyperparathyroidism. The use of calcium-based phosphate binders and vitamin D preparations may be problematic, as these medications can cause further increase in the calcium-phosphate product and/or exacerbation of HPH. Phosphate binders such as sevelamer, which do not contain calcium, seem to be more suitable.
In conclusion, most children with NS, especially young children with a chronic and severe form of NS, were found to have persistent HPH, despite normal kidney function. HPH does not correlate with creatinine clearance, plasma calcium, or urinary sodium levels. HPH may be caused by increased urinary excretion of IGF-1, known to stimulate phosphate tubular reabsorption. Further studies are needed in order to document hyperphosphatemia in other populations of nephrotic children and to identify factors which may be responsible for HPH within this context.
References
Delmez JA, Slatopolsky E (1992) Hyperphosphatemia: its consequences and treatment in patients with chronic renal disease. Am J Kidney Dis 19:303–317
Tsokos GC, Balow JE, Spiegel RJ, Magrath IT (1981) Renal and metabolic complications of undifferentiated and lymphoblastic lymphomas. Medicine (Baltimore) 60:218–229
Hande KR, Garrow GC (1993) Acute tumor lysis syndrome in patients with high grade non-Hodgkin’s lymphoma. Am J Med 94:133–139
Wilson MP, Lindsley CB, Warady BA, Johnson JA (1989) Hyperphosphatemia associated with cortical hyperostosis and tumoral calcinosis. J Pediatr 114:1010–1013
Mitnick PD, Goldfarb S, Slatopolsky E, Lemann J Jr, Gray RW, Agus ZS (1980) Calcium and phosphate metabolism in tumoral calcinosis. Ann Intern Med 92:482–487
Murtaza A, Khan SR, Butt KS, Lindblad BS, Aperia A (1988) Hypocalcemia and hyperphosphatemia in severely dehydrated children with and without convulsions. Acta Paediatr Scand 77:251–256
Langman CB (2004) Disorders of phosphorus, calcium and vitamin D. In: Avner ED, Harmon WE, Niaudet P (eds) Pediatric nephrology, 5th edn. Lippincott Williams & Wilkins, Philadelphia, pp 236–254
Seikaly MG, Ho PL, Emmett L, Fine RN, Tejani A (2003) Chronic renal insufficiency in children: the 2001 Annual Report of the NAPRTCS. Pediatr Nephrol 18:796–804
Alfrey AC (2004) The role of abnormal phosphorus metabolism in the progression of chronic kidney disease and metastatic calcification. Kidney Int Suppl 90:S13–S17
Schwartz GJ, Brion LP, Spitzer A (1987) The use of plasma creatinine concentration for estimating glomerular filtration rate in infants, children and adolescents. Pediatr Clin North Am 34:571–590
Burritt MF, Slockbower JM, Forsman RW, Offord KP, Bergstralh EJ, Smithson WA (1990) Pediatric reference intervals for 19 biologic variables in healthy children. Mayo Clin Proc 65:329–336
Cheng L, Sacktor B (1981) Sodium gradient-dependent phosphate transport in renal brush-border membrane vesicles. J Biol Chem 256:1556–1564
Walker JJ, Yan TS, Quamme GA (1987) Presence of multiple sodium-dependent phosphate transport processes in proximal brush-border membranes. Am J Physiol 252:F226–F231
Besse-Eschmann V, Klisic J, Nief V, Le Hir M, Kaissling B, Ambuhl PM (2002) Regulation of the proximal tubular sodium/proton exchanger NHE3 in rats with puromycin aminonucleoside (PAN)-induced nephrotic syndrome. J Am Soc Nephrol 13:2199–2206
Hirschberg R, Kaysen GA (1995) Insulin-like growth factor I and its binding proteins in the experimental nephrotic syndrome. Endocrinology 136:1565–1571
Garin EH, Grant MB, Silverstein JH (1989) Insulinlike growth factors in patients with active nephrotic syndrome. Am J Dis Child 143:865–867
Lee DY, Park SK, Kim JS (1996) Insulin-like growth factor I (IGF-I) and IGF-binding proteins in children with nephrotic syndrome. J Clin Endocrinol Metab 81:1856–1860
Haffner D, Tonshoff B, Blum WF, Vickers-M, Siebler T, Cronin MJ, Baxter RC, Mehls O (1997) Insulin-like growth factors (IGFs) and IGF binding proteins, serum acid-labile subunit and growth hormone binding protein in nephrotic children. Kidney Int 52:802–810
Hirschberg R (1993) IGF-I is ultrafiltered into the urinary space and may exert biological effects in proximal tubules in the nephrotic syndrome (abstract). J Am Soc Nephrol 4:771
Quigley R, Baum M (1991) Effects of growth hormone and insulin-like growth factor I on rabbit proximal convoluted tubule transport. J Clin Invest 88:368–374
Hirschberg R, Ding H, Wanner C (1995) Effect of insulin-like growth factor 1 on phosphate transport in cultured proximal tubule cells. J Lab Clin Med 126:428–434
Giordano M, DeFronzo RA (1995) Acute effect of human recombinant insulin-like growth factor I on renal function in humans. Nephron 71:10–15
Colston K, Williams NJ, Cleeve HJ (1985) Studies on vitamin D binding protein in the nephrotic syndrome. Clin Chem 31:718–721
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Feinstein, S., Becker-Cohen, R., Rinat, C. et al. Hyperphosphatemia is prevalent among children with nephrotic syndrome and normal renal function. Pediatr Nephrol 21, 1406–1412 (2006). https://doi.org/10.1007/s00467-006-0195-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-006-0195-2