Abstract
Background
Endoscopic techniques allow resections of deep submucosal invasion rectal carcinoma, but mostly are facing issues such as costs, follow-up care or size limit. Our aim was to design a new endoscopic technique, which retains the advantages over surgical resections while eliminating the disadvantages mentioned above.
Patients and methods
We propose a technique for the resection of the superficial rectal tumours, with highly suspicious deep submucosal invasion. It combines steps of endoscopic submucosal dissection, muscular resection and edge-to-edge suture of the muscular layers, finally performing the equivalent of a “transanal endoscopic microsurgery” with a flexible colonoscope (F-TEM).
Results
A 60-year-old patient was referred to our unit, following the discovery of a 15 mm distal rectum adenocarcinoma. The computed tomography and the endoscopic ultrasound examination revealed a T1 tumour, without secondary lesions. Considering that the initial endoscopic evaluation highlighted a depressed central part of the lesion, with several avascular zones, an F-TEM was performed, without severe complication. The histopathological examination revealed negative resection margins, without risk factors for lymph node metastasis, no adjuvant therapy being proposed.
Conclusion
F-TEM allows endoscopic resection of highly suspicious deep submucosal invasion T1 rectal carcinoma and it proves to be a feasible alternative to surgical resection or other endoscopic treatments as endoscopic submucosal dissection or intermuscular dissection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Adoption of national population-based screening programs and the rapid progress in endoscopic techniques have led to the increased detection of superficial colorectal neoplasms (including precancerous lesions and early cancer) [1]. Furthermore, colorectal lesions could be evaluated and resected by endoscopic techniques, such as endoscopic mucosal resection or endoscopic submucosal dissection (ESD) [2]. A free vertical margin is an important histological criteria to assess that the endoscopic resection is R0 [1]. The main concern of these classic techniques appears in the patients with deep submucosal invasion colorectal carcinoma (T1 sm2 or sm3), 10 to 50% of them having lymph node metastasis, according to the presence of histological high-risk features such as lymphovascular invasion, high-grade tumor budding, undifferentiated (grade 3) cancer or vertical margin invasion [1, 3]. Theoretically, in these cases, a subsequent colonic/colorectal resection with lymph node dissection is necessary or, particularly for rectal lesions, a chemoradiotherapy [3, 4].
In order to maximize the chances for a histologically complete resection (R0), even in cases of submucosal invasion, new endoscopic techniques came out—full-thickness resection device (FTRD), mixed ESD-FTRD or endoscopic intermuscular dissection (EID) [2, 5]. These new techniques have been developed as alternatives for rectal surgery and its possible burden, as surgical complications (rate between 12.6 and 13.5%), general severe complications (rate of 8.3 to 9.5%) and a postoperative mortality rate of 1.7% to 2.5% [6]. On the other hand, rectal surgery is associated with urinary, sexual, and defecatory dysfunctions associated with alteration of quality of life [7]. Some issues are related to these new techniques, such as costs, follow-up or size limit for FTRD, respectively technical challenge to perform a complete resection with the EID technique [2, 5].
Our aim was to delineate a new endoscopic technique, similar to Transanal Endoscopic Microsurgery (TEM), which could serve as alternative for the endoscopic treatment of the suspicious deep submucosal invasion T1 rectal carcinoma, eliminating the disadvantages mentioned above.
Materials and methods
We propose a new technique for the resection of the superficial rectal tumours, with highly suspicious deep submucosal invasion. It combines steps of ESD, muscular resection and edge-to-edge suture of the muscular layers, finally performing the equivalent of a “transanal endoscopic microsurgery” with a flexible endoscope (F-TEM).
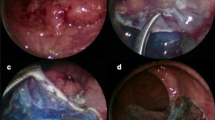
More precisely, the resection starts with standard ESD steps (Fig. 1, panel A)—marking the margins in soft coagulation mode (50 W), submucosal injection of fructose-glycerin solution, mucosal circumferential incision with Endocut mode (ERBE electrosurgical generator; ERBE Elektromedizin GmbH, Tübingen, Germany), trimming of the submucosa. Then, the lesion is suspended from the lateral sides, using two clips and one rubber band (standard orthodontic rubber band) for each side, exerting a continuous traction of the specimen, which allows a better exposure of the deep layers and to complete the resection of the lesion inside the colonic lumen (Fig. 1, panel B). The ESD is continued until the area suspected for deep submucosal invasion is reached. From this point, the procedure continues with the incision of the muscular layer using a TriangleTipKnife J (Olympus, Tokyo, Japan) (Fig. 1, panel C). Starting from the distal pole of the tumour, a direct and entire resection of the muscularis propria is realized, including both circular and longitudinal muscular layers, without an intermuscular dissection, until the lesion in completely extracted. During the total muscular section, the rubber band-clips system keeps the resected tumour inside the colonic lumen and it allows to complete the resection on the serosal side of the tumour, without the risk of migration of the specimen outside the rectum, in the mesorectum, neither the risk of implantation of cancerous cells in the mesorectum.
A Starting the resection using the classic steps of endoscopic submucosal dissection. B Suspension of the lesion from lateral sides using two clips and one rubber band for each side, allowing to complete the resection of the lesion and maintaining the resected specimen inside the colonic lumen. C Incision of the muscular layer from the area suspected of deep submucosal lesion. D End of resection and edge-to-edge suture of incised muscular layers with endoscopic clips
The final step consists in an edge-to-edge suture of the incised muscular layers, using clips. The resected lesion is retrieved with an endoscopic loop (Captiflex, Boston, USA) and detached from the rectal mucosa (Fig. 1, panel D).
This study was approved by our local institutional review board, the Ethical Review Committee for publications of the Cochin University Hospital. The written consent of the patient was obtained before the procedure.
The procedure was performed by an endoscopist with more than ten years of experience with endoscopic dissection and myotomy techniques (ESD and per oral endoscopic myotomy).
Results
A 60-year-old woman, without severe comorbidities, was referred to our Gastroenterology Unit following the discovery of a 15 mm distal rectum adenocarcinoma. Previously, the patient underwent an abdominal, pelvic and thoracic computed tomography (CT-TAP), no other suspect lesion being detected, and an endoscopic ultrasound examination, showing submucosal invasion (T1). An initial endoscopic examination reveals a 15 mm, superficial, elevated lesion, with a slightly depressed central part (0-IIa + IIc Paris classification [8]) (Video 1) (Fig. 2, panel A). The virtual chromoendoscopy shows a heterogeneous aspect of the central part, irregular capillary network and several avascular zones (IIIB Sano classification [9]) (Fig. 2, panel B).
A Superficial, elevated lesion, with slightly depressed central part (0-IIa + IIc Paris classification). B Chromoendoscopy view—heterogeneous central part, with irregular capillary network and several avascular zones. C Edge-to-edge suture with endoscopic clips. D En bloc resection of the lesion (3.1 × 2.5 cm). E Lesion overview, with different rectal wall layers (blue arrows: superior and inferior part of muscularis propria—2.4 mm of depth) and irregular deep part of the lesion (delimited by the blue lines). Negative excision margins (deep margin—2.27 mm; lateral margin—5.14 mm; width of tumour infiltration through muscularis mucosa—2.09 mm). The total length of the muscular layer measured on the pathological specimen was 10.2 mm. F Disruption of muscularis mucosa and infiltration of submucosa by malignant glands
Taking into account the endoscopic criteria for deep submucosal invasion and the possibility of profound resection of the submucosa, an endoscopic treatment by F-TEM technique was proposed. The resection was performed following all the steps mentioned above. For the ESD part, a 1 mm FlushKnife N-S (Fujifilm Co., Tokyo, Japan) was used. During the muscular incision, two hemorrhagic events were noticed, stopped with a Coagrasper hemostatic forceps (Olympus, Hamburg, Germany). A total of eight clips (Boston scientific, Boston, USA) were necessary for the suture (Fig. 2, panel C), the resection being en bloc (Fig. 2, panel D). No other complication was observed and the patient was discharged two days later.
The histopathological examination (Fig. 2, panel E and F) revealed well differentiated (G1) T1 rectal adenocarcinoma, with 800 µm depth of submucosal invasion (sm1), without lymphovascular invasion/emboli, with low-grade budding (bd1) and negative excision margins.
After a multidisciplinary oncology reunion analysis, it was concluded to follow-up with CT-TAP and pelvic magnetic resonance imaging (MRI) in 6 months and colonoscopy in 12 months. No adjuvant treatment was proposed. No sign of local or metastatic recurrence was observed at the 6 months follow-up check.
Discussion
F-TEM could be a therapeutic option of T1 rectal cancers, realizing a complete resection of all the layers of the colon or the rectum and increasing the probability to obtain a free vertical resection margin, compared to standard ESD in patients with deep submucosal invasion. For the case report presented above, according to Japanese recommendations, a surgical resection should have been proposed, since the depth of invasion in Sano IIIb is sm2 or sm3 in 80% of cases and the risk of R1 resection is higher [10]. The presence of this criteria as an independent risk factor for lymph node metastasis has been questioned recently [11, 12]. Instead of this, the F-TEM could allow a complete resection of the submucosa and R0 histopathological results even for sm2 or sm3 lesions. Recent data showed that in case of T1 colorectal cancers with deep invasion (sm2 and sm3), but without pejorative qualitative histological parameters, the risk of lymph node invasion is between 3 and 8%, suggesting a possible “watch and wait” strategy as it has been proposed in patients with T2 to T4 rectal cancer, who have a clinical complete response after neoadjuvant chemoradiotherapy [1, 13]. For our patient, the risk of ESD was to obtain a positive vertical margin since there was an 80% risk of sm2 or sm3 invasion in case of Sano IIIb [10].
Other techniques as EID or FTRD have been recently described. Comparing it with the FTRD, the F-TEM technique has some advantages: the cost (all materials used are usually found in a tertiary referral center for digestive endoscopy, no additional material being necessary), the possibility of follow-up by MRI (impractical with the over-the-scope clip), no size limit of the resected lesion (< 20 mm imposed by the FTRD cap) and the possibility to change from normal ESD to F-TEM during the same session in case of suspicion of deep invasion. In case of larger resections, where wall defect closure may be difficult, an endoloop or other suturing techniques could be used to approach the clips [14]. Previously, it has been shown that the use of rubber band-clips system simplifies an ESD and decreases time of resection [15]. In this case, the rubber band technique allows the dissection of all the layers of the rectum, the section of the specimen on the serosal side without loop and avoids the migration of the specimen in the mesorectum fat, with the potential risk of cell implantation and cancer recurrence.
Questions could be raised on long-term oncologic outcomes and randomized prospective studies are needed. However, we consider that F-TEM is a promising resection technique of the deep submucosal invasive T1 rectal cancers. In conclusion, this new method of TEM which allows endoscopic resection of rectal cancers with a standard digestive endoscope is a feasible alternative option to surgical resection or FTRD in the treatment of highly suspicious deep submucosal invasion rectal carcinoma.
References
Dang H, Dekkers N, le Cessie S, van Hooft JE, van Leerdam ME, Oldenburg PP, Flothuis L, Schoones JW, Langers AMJ, Hardwick JCH, van der Kraan J, Boonstra JJ (2022) Risk and time pattern of recurrences after local endoscopic resection of T1 colorectal cancer: a meta-analysis. Clin Gastroenterol Hepatol 20:e298–e314
Guillaumot MA, Barret M, Jacques J, Legros R, Pioche M, Rivory J, Rahmi G, Lepilliez V, Chabrun E, Leblanc S, Chaussade S (2020) Endoscopic full-thickness resection of early colorectal neoplasms using an endoscopic submucosal dissection knife: a retrospective multicenter study. Endosc Int Open 8:E611–E616
Ichimasa K, Kudo SE, Miyachi H, Kouyama Y, Misawa M, Mori Y (2021) Risk stratification of T1 colorectal cancer metastasis to lymph nodes: current status and perspective. Gut Liver 15:818–826
van Oostendorp SE, Smits LJH, Vroom Y, Detering R, Heymans MW, Moons LMG, Tanis PJ, de Graaf EJR, Cunningham C, Denost Q, Kusters M, Tuynman JB (2020) Local recurrence after local excision of early rectal cancer: a meta-analysis of completion TME, adjuvant (chemo)radiation, or no additional treatment. Br J Surg 107:1719–1730
Moons LMG, Bastiaansen BAJ, Richir MC, Hazen WL, Tuynman J, Elias SG, Schrauwen RWM, Vleggaar FP, Dekker E, Bos P, Fariña Sarasqueta A, Lacle M, Hompes R, Didden P (2022) Endoscopic intermuscular dissection for deep submucosal invasive cancer in the rectum: a new endoscopic approach. Endoscopy 54(10):993–998
Vermeer NCA, Backes Y, Snijders HS, Bastiaannet E, Liefers GJ, Moons LMG, van de Velde CJH, Peeters KCMJ, Dutch T1 Colorectal Cancer Working Group (2018) National cohort study on postoperative risks after surgery for submucosal invasive colorectal cancer. BJS Open 3:210–217
Giglia MD, Stein SL (2019) Overlooked long-term complications of colorectal surgery. Clin Colon Rectal Surg 32:204–211
Endoscopic Classification Review Group (2005) Update on the Paris classification of superficial neoplastic lesions in the digestive tract. Endoscopy 37:570–578
Uraoka T, Saito Y, Ikematsu H, Yamamoto K, Sano Y (2011) Sano’s capillary pattern classification for narrow-band imaging of early colorectal lesions. Dig Endosc 23:112–115
Hashiguchi Y, Muro K, Saito Y, Ito Y, Ajioka Y, Hamaguchi T, Hasegawa K, Hotta K, Ishida H, Ishiguro M, Ishihara S, Kanemitsu Y, Kinugasa Y, Murofushi K, Nakajima TE, Oka S, Tanaka T, Taniguchi H, Tsuji A, Uehara K, Ueno H, Yamanaka T, Yamazaki K, Yoshida M, Yoshino T, Itabashi M, Sakamaki K, Sano K, Shimada Y, Tanaka S, Uetake H, Yamaguchi S, Yamaguchi N, Kobayashi H, Matsuda K, Kotake K, Sugihara K, Japanese Society for Cancer of the Colon and Rectum (2020) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol 25:1–42
Zwager LW, Bastiaansen BAJ, Montazeri NSM, Hompes R, Barresi V, Ichimasa K, Kawachi H, Machado I, Masaki T, Sheng W, Tanaka S, Togashi K, Yasue C, Fockens P, Moons LMG, Dekker E (2022) Deep submucosal invasion is not an independent risk factor for lymph node metastasis in T1 colorectal cancer: a meta-analysis. Gastroenterology 163:174–189
Rönnow CF, Arthursson V, Toth E, Krarup PM, Syk I, Thorlacius H (2022) Lymphovascular infiltration, not depth of invasion, is the critical risk factor of metastases in early colorectal cancer: retrospective population-based cohort study on prospectively collected data, including validation. Ann Surg 275:e148–e154
Oka S, Tanaka S, Nakadoi K, Kanao H, Chayama K (2013) Risk analysis of submucosal invasive rectal carcinomas for lymph node metastasis to expand indication criteria for endoscopic resection. Dig Endosc 25(Suppl 2):21–25
Shi Q, Chen T, Zhong YS, Zhou PH, Ren Z, Xu MD, Yao LQ (2013) Complete closure of large gastric defects after endoscopic full-thickness resection, using endoloop and metallic clip interrupted suture. Endoscopy 45(5):329–334
Jacques J, Charissoux A, Legros R, Tailleur A, Rivory J, Albouis J, Pioche M (2018) Double-clip counter-traction using a rubber band is a useful and adaptive tool for colonic endoscopic submucosal dissection. Endoscopy 50:179–181
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Stanislas Chaussade received honoraria for lectures, presentations or educational events from FujiFilm, Norgine, Life Europe, iFred. Flavius-Stefan Marin, Einas Abou Ali, Arthur Belle, Frédéric Beuvon, and Romain Coriat have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 157611 KB) Video 1: “Transanal endoscopic microsurgery” with a flexible colonoscope of a distal rectum adenocarcinoma
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marin, FS., Abou Ali, E., Belle, A. et al. “Transanal endoscopic microsurgery” with a flexible colonoscope (F-TEM): a new endoscopic treatment for suspicious deep submucosal invasion T1 rectal carcinoma. Surg Endosc 37, 5714–5718 (2023). https://doi.org/10.1007/s00464-023-10141-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10141-7