Abstract
Background
Sacrococcygeal pilonidal disease (SPD) is a common surgical condition for which a multitude of surgical treatments have been described. The present review aimed to evaluate the efficacy and safety of a novel endoscopic procedure for the treatment of SPD.
Methods
An organized literature search was conducted. Electronic databases including PubMed/Medline, Scopus, Embase, and Cochrane library were searched for articles that assessed the endoscopic treatment for SPD. The main outcome parameters were failure of the technique including persistence and recurrence of SPD, postoperative complications and pain, time to complete healing, and time to return to work.
Results
Nine studies with a total of 497 patients were included. Mean age of patients was 24.8 years. Mean operation time was 34.7 min. The procedure was performed as day-case surgery in all studies. The mean Visual analogue score of pain within the first week was 1.35. Failure of the technique was recorded in 40 (8.04%) patients, 20 (4.02%) had persistent SPD and 20 (4.02%) developed recurrence. The weighted mean failure rate of the technique was 6.3% (95% CI 3.6–9.1). Mean weighted complication rate was 1.1% (95% CI 0.3–2.4). Mean time to complete healing was 32.9 days and mean time to return to work was 2.9 days.
Conclusion
The endoscopic treatment of pilonidal sinus is a promising and safe method of treatment of SPD. The main advantages of the endoscopic treatment as compared to conventional surgery are the minimal postoperative pain, quick healing, and short time to return to work and daily activities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Sacrococcygeal pilonidal disease (SPD) was first described by Mayo in 1883, since that time a multitude of treatment modalities have been proposed for its management [1]. SPD predominantly affects young and middle-age males particularly individuals with increased body mass index (BMI) and positive family history [2]. The disease entails a spectrum of clinical presentations where it can be an asymptomatic condition in some patients while in other patients it presents with recurrent or persistent abscess with discharge or pain at the sacrococcygeal region.
Treatment of SPD is essentially surgical. A plethora of surgical procedures for SPD have been described in the literature that include excision with lay open of the sinus, excision and marsupialization, various flap procedures such as Karydakis procedure and modified Limberg flap, and finally minimally invasive techniques as curettage of the sinus cavity with injection of phenol, fibrin glue, or thrombin–gelatin matrix [3,4,5,6].
Minimally invasive treatments for SPD are associated with less pain, fewer complications, shorter hospital stay, and early resumption of daily activities. However, according to the practice parameters for the management of SPD devised by the American Society of Colon and Rectal Surgeons (ASCRS), phenol and fibrin glue injection should be used in select patients since they have a weak grade of recommendation owing to low quality of evidence [7].
In 2013, Meinero et al. [8] described a new type of minimally invasive treatment for SPD that is the Endoscopic Pilonidal Sinus Treatment (E.P.Si.T). The authors used the same equipment and technology for video-assisted anal fistula treatment (VAAFT) [9] for treatment of primary and recurrent pilonidal sinus. The concept of EPSiT is to endoscopically remove all infected and diseased area inside the pilonidal sinus cavity with a fistuloscope introduced through a small circular incision of around half a centimeter in diameter which should substantially reduce the operative morbidity associated with more extensive flap procedures.
The present review aimed to evaluate efficacy and safety of the video-assisted endoscopic pilonidal sinus treatment regarding the recurrence and complication rates and to illustrate different variations in the original technique described by Meinero et al. [8] and how these variations affected the final outcome of the procedure.
Methods
Registration
The protocol of this review has been registered a priori in http://www.researchregistry.com under the UIN: “reviewregistry371.”
Search strategy
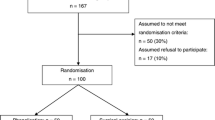
Two of the authors (S.E and V.G) conducted an organized literature search for studies evaluating the outcome of endoscopic pilonidal sinus treatment. The review was performed in adherence with the screening guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) [10] (Fig. 1).
A systematic search of electronic databases including PubMed/Medline, Scopus, Embase, and Cochrane library from inception through September 2017 was undertaken. PubMed function-“related articles” was used to search further articles. The authors manually screened the reference section of each article for other potentially relevant articles.
The search process used the following keywords: “pilonidal sinus,” “pilonidal disease,” “PNS,” “pilonidal abscess,” “video-assisted,” “treatment,” “endoscopic pilonidal sinus treatment,” “E.P.Si.T,” “endoscopic,” “minimally-invasive,” “outcome,” “recurrence,” and “complications”. The following medical subject headings (MeSH) terms were also used in the literature search: (video-assisted surgery), (pilonidal sinus), (treatment outcome), and (recurrence).
After excluding duplicate reports and conference abstracts with no full-text version, the remaining publications were screened and filtered by title and abstract, then subsequently by full-text. The full-text of each article was independently reviewed by one of the three authors (H.E, M.S, and A.S) to check its eligibility for inclusion to the review then the principal author (S.E.) performed a final review of the articles to be included.
Eligibility criteria
All studies, whether cohort or comparative studies, that assessed the outcome of endoscopic pilonidal sinus treatment were considered eligible to be included. No language restrictions were applied.
We excluded irrelevant articles, editorials, letters, case reports, reviews, and meta-analyses. Studies that included less than three patients and studies with data overlapping with subsequent studies were excluded. Articles that did not report the main outcomes of the review clearly were also excluded.
Assessment of methodological quality and risk of bias within the studies
Two reviewers (S.E & M.S) assessed the methodological quality of each study in an independent manner. In case of discrepancy in interpretation of study quality, a third author (H.E) was consulted.
The checklist for the quality of case series of the National Institute for Health and Clinical Excellence (NICE) [11] was used for the assessment of the studies included and each study was given a score. Quality of the studies was defined as good (score = 7–8), fair (score = 4–6), and poor (score = 0–3). The revised grading system of the Scottish Intercollegiate Guidelines Network (SIGN) [12] was used to assess comparative studies, a score of less than 8 indicated poor quality; a score of 8–14 implied fair quality and a score of more than 14 indicated good quality.
Data extraction
Data extracted from each study included type, duration and country of the study; patient characteristics including age, male-to-female ratio, BMI, number of previously recurrent cases; technical details of the procedure particularly injection of specific material inside the sinus cavity; operation time; length of hospital stay (LoS); incidence of persistence or recurrence of SPD; complication rate; time to complete healing, time to return to work and daily activities, and duration of follow-up.
Outcomes
The primary outcomes of the review were the incidence of failure of the technique and complication rate. Failure of the technique was defined as persistence (non-healing) or postoperative recurrence of SPD. Persistence or incomplete healing of SPD was defined as the persistence of wound discharge or swelling more than 2 months after the procedure. Recurrence was diagnosed when patients reported symptoms of local pain, discharge, or intermittent swelling at least 4 months after complete healing. Secondary outcomes comprised operation time, LoS, time to complete healing, time to return to daily activities, and postoperative pain.
Assessment of publication bias among the studies included
Publication bias across the studies was assessed using a funnel plot of the standard error of the failure rates against the failure rates of the studies reviewed. A straight vertical line in the plot indicates the zone in which 95% of studies should be if there were no publication bias (Fig. 2). The Begg and Mazumdar rank correlation test was used to investigate publication bias and the Kendall’s tau-b (corrected for ties) was − 0.166 with a one-tailed P value of 0.26 and a two-tailed P value of 0.53. Egger’s regression test was also performed and the intercept (B0) was − 0.463 (95% CI − 1.85 to 0.92), with t = 0.77 and eight degrees of freedom. The one-tailed P value was 0.23 and the two tailed P value was 0.46 indicating no significant publication bias among the studies included.
Statistical analysis
Data were analyzed using SPSS version 23 (IBM corp, Bristol, UK). Continuous variables were expressed as mean ± standard deviation (SD), or median and normal range. Categorical variables were expressed as number and percentage. P value less than 0.05 was considered significant.
A meta-analysis of recurrence and complication rates across the studies was conducted using open-source, cross-platform software for advanced meta-analysis “openMeta[Analyst]™” version 12.11.14. Data was pooled and the weighted mean rates with 95% confidence interval (CI) were calculated. Statistical heterogeneity was determined by the Cochrane Q test and the Inconsistency (I2) statistics. I2 is the proportion of total variation observed between the studies attributable to differences between studies rather than sampling error. Heterogeneity is considered low if I2 < 25% and high if I2 > 75%. If no significant statistical heterogeneity was present, a fixed-effect model was used to pool data, whereas in the case of significant (P < 0.1) statistical heterogeneity, the binary random-effect model was utilized for pooling of data.
A random-effect meta-regression model was used weighing the studies by their within-study variance and the degree of heterogeneity. The heterogeneity between the studies was explored in relation to differences in patients’ age, sex, history of surgery for SPD, presence of lateral sinus pits, and development of complications. The statistical significance of each examined variable was determined using slope coefficient (SE) and P value.
Results
Patient and study characteristics
Nine studies [8, 13,14,15,16,17,18,19,20] were found eligible and were included to the review. The studies were published between 2014 and 2017. Six studies were conducted in Italy, one in the United Kingdom, one in Turkey, and one in Singapore. There were six prospective studies, two retrospective series, and one randomized controlled trial. All publications had a fair methodologic quality with exception to two trials [16, 17] that had good quality. The median quality score of the case-series studies is 6 (range, 5–7), whereas the median quality score of comparative studies was 12 (range, 8–16).
The studies included 497 patients with a mean age of 24.8 ± 1.6 (range, 23–27.6) years and with male-to-female ratio of 3.2:1. Three hundred and sixty-four (73.2%) patients had primary SPD and 133 (26.8%) had history of previous surgery for pilonidal sinus. One-hundred and forty-two patients (38%) out of 373 patients reported in five studies had complex SPD with lateral pits (Table 1).
Technical details
Endoscopic procedures were performed using the Meinero fistuloscope (Karl Storz™, Tuttlingen, Germany) “E.P.Si.T” in all studies except two studies [17, 20] that used 4-mm continuous flow operative Bettocchi Office Hysteroscope fistuloscope (Karl Storz™, Tuttlingen, Germany) “Video-assisted pilonidal sinus treatment”. Four studies performed the procedure under local anesthesia [16, 17, 19, 20], two used sedation in addition to local anesthesia [13, 14], and one study [8] used either spinal or local anesthesia.
The procedure was divided into diagnostic and therapeutic phases. In the diagnostic phase the anatomy of the pilonidal sinus was defined and any secondary tracks or abscess cavities were identified. In the therapeutic phase, the sinus was irrigated with Glycine/Mannitol 1% solution, then all hairs and granulation tissue were removed thoroughly by a forceps under direct vision followed by cautery ablation of the sinus cavity using monopolar electrode. The necrotic material was removed with an endobrush or a Volkmann spoon, then the sinus cavity is irrigated with saline solution and light dressing is applied without packing.
Two studies added an additional step to the procedure after complete ablation of the sinus cavity; the first study [14] injected crystallized phenol crystals inside the sinus and the second study [19] inserted a Gore Bio-A® fistula plug (W.L.Gore Corporation, Newark, Delaware, USA) inside the sinus cavity.
The mean operation time was 34.7 ± 17.7 (range, 20–45) min. The procedure was performed as day-case surgery in all of the studies.
Postoperative pain
Postoperative pain was assessed by using visual analogue scale (VAS) ranging from 0 to 10, or by estimating the percentage of patients that required analgesia in the first postoperative day. Seven studies reported the pain VAS within the first week after the procedure, the mean VAS was 1.35 ± 0.8 (range, 0.5–2). As regards the need for analgesia, seven studies including 416 patients reported that 36 (8.6%) patients required intravenous analgesics in the first postoperative day, ranging from 0 to 22.2% of patients across the studies (Table 2).
Failure of the technique
Overall, failure of the technique was recorded in 40 (8.04%) patients, 20 (4.02%) had persistent (non-healing) pilonidal sinus, and 20 (4.02%) developed recurrence of SPD after complete initial healing of the primary wound. Persistence of SPD ranged between 0 and 20% and recurrence of SPD ranged between 0 and 5.2% across the studies (Table 2).
The weighted mean failure rate of the technique was 6.3% (95% CI 3.6–9.1) (I2 = 23.6, Q = 10.4, P = 0.23) (Fig. 3). The moderate heterogeneity observed among the studies in failure rates of the procedure can be attributed to different patients’ characteristics and some variations in the methodology of each study. Failure of the technique was managed with re-do of endoscopic treatment in 24 patients, surgical excision and primary closure in 3 patients, and lotus petal flap in 2 patients. Management of 11 patients with persistent or recurrent SPD was not clarified in three studies [13, 17, 18].
Complications
Eight (1.6%) patients developed complications after the procedure as reported by two studies [17, 18]. Complication rate across the study ranged between 0 and 11.1%. Complications included hematoma, infection, persistent discharge, and failure of healing. The mean weighted complication rate was 1.1% (95% CI 0.3–2.4) (I2 = 24.4. Q = 10.6, P = 0.22) (Fig. 4).
Time to return to work and patient satisfaction
The mean time to complete healing after the procedure was 32.9 ± 23 (range, 15–75) days. The mean time to return to work and normal activities was 2.9 ± 1.8 (range, 1.6–6) days. Three studies [13, 18, 20] including 113 patients assessed patient satisfaction after endoscopic pilonidal sinus treatment and 108 (95.6%) were completely satisfied with the procedure with satisfaction ranging from 77.7 to 97.4% of patients. The median follow-up across the studies was 12 months, ranging from 2.5 to 25 months.
Predictors for failure of endoscopic pilonidal sinus treatment (persistence or recurrence of SPD)
The potential effect of clinical confounders on the technical failure of endoscopic pilonidal sinus treatment was investigated using the random effect meta-regression model. The variables that were significantly associated with failure of endoscopic pilonidal sinus treatment were patients’ age (SE = − 0.017, P = 0.02) and history of previous surgery for SPD (SE = 0.001, P = 0.022). Variables that were not significantly associated with failure of E.P.Si.T were male gender (SE = − 0.002, P = 0.8), presence of lateral sinus pit (SE = 0.001, P = 0.19), and development of complications (SE = − 0.005, P = 0.27).
Discussion
The multitude and diversity of the current treatment options attests to the challenge of SPD management. The present review examined the efficacy and safety of a novel treatment strategy for SPD, the endoscopic pilonidal sinus treatment. More than five hundred patients were studied, the majority of whom were young adult males. This distribution is the typical pattern of patients with SPD perhaps because of their more hirsute nature as previously reported in the literature [21].
Endoscopic pilonidal sinus treatment is a minimally invasive technique for treatment of SPD that was adopted from the concept of a similar minimally invasive technique for anal fistula, the video-assisted anal fistula treatment (VAAFT) [22]. Although there are other minimally invasive techniques which involve curettage of the pilonidal sinus with local injection of fibrin glue or phenol [7], such techniques are performed in a blind manner without being able to visualize the interior of the sinus cavity which may lead to incomplete debridement and cleansing of hairs and infected tissues inside the sinus. In contrast, the endoscopic pilonidal sinus treatment is done under direct vision, allowing the removal of all infected tissues and lining of the sinus cavity.
According to the findings of this systematic review, the endoscopic pilonidal sinus treatment managed to achieve satisfactory outcome with a weighted mean failure rate of 6.3%. This percentage is lower than the recurrence rate recorded after surgical excision and primary closure of SPD (8%) [23], yet higher than various flap procedures (0–6%) [7], off-midline closure technique (5.8%) [23], and deroofing and curettage of the sinus (4.5%) [24].
However, in comparison with other minimally invasive techniques the failure rate of the endoscopic pilonidal sinus treatment was much lower than that of fibrin sealant injection (20%) [25] and phenol injection (13%) [4]. Even in case of recurrence of SPD after endoscopic treatment, the re-do of the procedure proved feasible and was conducted successfully in more than half of the patients presenting with recurrent disease which can be regarded as an advantage of the procedure.
The safety of the endoscopic treatment of SPD was confirmed by a low weighted complication rate of 1.1%, much lower than that of surgical excision with lay open of pilonidal sinus (8.2%), excision with primary closure (12.1%) [23], flap procedures (7–20%) [7], and fibrin sealant injection (14.6%) [25]. While the majority of the studies included to the present review did not report any postoperative morbidities, only two studies [17, 18] reported minor wound-related complications of the endoscopic treatment that were managed successfully with conservative treatment.
The paramount advantages of the endoscopic pilonidal sinus treatment were minimal postoperative pain, rapid healing, and short time to return to work and daily activities. The mean time needed for complete healing after endoscopic treatment was approximately one month and the mean time to return to work was less than three days, much shorter than surgical excision with midline closure (8.5 days), excision with off-midline closure (15.3 days), modified Limberg flap (9.3 days) [23], and deroofing and curettage of the sinus (8.4 days) [24]. Early recovery and resumption of daily activities is a unique advantage that is much appreciated by the patient and can help reduce time away from work, and hence decrease health-related economic loss.
A randomized trial [17] compared the endoscopic pilonidal sinus treatment with conventional surgery (Bascom cleft lift procedure) in a cohort of 145 consecutive patients. Although patients who underwent endoscopic treatment had significantly shorter time off work (1.6 vs. 3.9 days) and higher patient satisfaction, the recurrence and complication rates were comparable amongst the two groups with no significant differences observed. An important finding of this particular study was that a distance of more than 2.5 cm between the lateral sinus orifice and the midline was a significant predictor for postoperative wound complications with hazard ratio of 9.6 and P value of 0.004.
Some technical variations of the endoscopic treatment of SPD were recognized through this review. Some studies [17, 20] used a continuous-flow operative hysteroscope instead of the original Meinero fistuloscope kit and attained similar results to the other studies with failure rate of less than 4%. Other trials injected certain materials inside the sinus cavity upon the end of procedure, one study [14] injected crystallized phenol crystals inside the sinus and the second [19] inserted a Gore Bio-A® fistula plug inside the sinus cavity. Both studies conferred excellent results with no recurrence or complications recorded in any of the studies which may stimulate further trials combining the endoscopic technique with injection of various materials inside the sinus cavity to accelerate healing and prevent recurrence.
One study [14] applied the endoscopic treatment in the acute setting of SPD for the treatment of pilonidal abscess. Although 20% of patients required further definitive treatment of SPD, the endoscopic pilonidal sinus treatment was associated with less postoperative pain, quicker healing, and shorter time to return to work compared to conventional incision and drainage. The short hospital stay and reduced need for dressing changes motivated the authors of the studies to conclude that endoscopic treatment is a safe, cost-effective treatment for of pilonidal abscess.
Another benefit of the endoscopic pilonidal sinus treatment was its effectiveness in patients with recurrent SPD. Although more than one-quarter of patients included in the present review had recurrent sinus after previous surgery for SPD, the outcome of the procedure was satisfactory. Moreover, in one study [19], all patients who underwent endoscopic treatment had previously recurrent SPD, yet none developed recurrence after the endoscopic treatment. With such versatility, the endoscopic pilonidal sinus treatment may emerge as a viable alternative to extensive flap procedures that are usually used for the treatment of complicated and recurrent SPD [26].
The limitations of the endoscopic pilonidal sinus treatment are similar to those of VAAFT which we elaborated on in a previous review [22]. These drawbacks include the need for proper training to gain the required experience, in addition to the cost of the fistuloscope and the kit. On the other hand, the cost of the equipment required for the procedure is incurred only once and the fistuloscope can be used for treatment of both SPD and anal fistula. The short hospital stay, less postoperative pain, reduced need for dressing changes, and shorter time away of work can help reduce secondary costs and render the procedure a cost-effective treatment of SPD.
Limitations of the present review include the small number and fair quality of the studies reviewed with only one randomized controlled trial being included while the remaining studies were case series which entail the possibility of selection and reporting bias. More than half of the patients were included in one study [16] which may affect the reliability of the analysis. It is also worthy to note that half of the studies included were conducted at two centers which may limit the generalizability of the final results. Furthermore, the short follow-up of patients in can prevent drawing firm conclusions on the long-term outcome of the technique. Further prospective studies are required, preferably randomized trials comparing the endoscopic pilonidal sinus treatment with other minimally invasive or conventional procedures in order to reach more solid conclusions on the efficacy and safety of the technique.
Conclusions
The endoscopic treatment of pilonidal sinus is a novel and promising method of treatment of SPD. The endoscopic treatment proved effective at the acute setting in the treatment of pilonidal abscess with only one-fifth of patients needed further definitive treatment.
The main advantages of the endoscopic treatment as compared to conventional surgery are the mild postoperative pain, quick healing, and short time to return to work and daily activities. Although the initial reports documented the safety and short-term effectiveness of endoscopic treatment of SPD, the long-term outcome of the procedure is still unclear and longer follow-up is warranted to ascertain the efficacy of this novel technique. Furthermore, well-designed randomized trial comparing the endoscopic treatment of SPD with conventional surgical treatment is required to substantiate the promising outcomes reported in this review.
References
Hull TL, Wu J (2002) Pilonidal disease. Surg Clin N Am 82(6):1169–1185
da Silva JH (2000) Pilonidal cyst: cause and treatment. Dis Colon Rectum 43(8):1146–1156
Tokac M, Dumlu EG, Aydin MS, Yalcın A, Kilic M (2015) Comparison of modified Limberg flap and Karydakis flap operations in pilonidal sinus surgery: prospective randomized study. Int Surg 100(5):870–877. https://doi.org/10.9738/INTSURG-D-14-00213.1
Kayaalp C, Aydin C (2009) Review of phenol treatment in sacrococcygeal pilonidal disease. Tech Coloproctol 13(3):189–193. https://doi.org/10.1007/s10151-009-0519-x
Lund J, Tou S, Doleman B, Williams JP (2017) Fibrin glue for pilonidal sinus disease. Cochrane Database Syst Rev 1:CD011923. https://doi.org/10.1002/14651858.CD011923.pub2
Elbanna HG1, Emile SH, Youssef M, Thabet W, El-Hamed TM, Ghnnam WM (2016) Novel approach of treatment of pilonidal sinus disease with thrombin gelatin matrix as a sealant. Dis Colon Rectum 59(8):775–780. https://doi.org/10.1097/DCR.0000000000000604
Steele SR, Perry WB, Mills S, Buie WD, Standards Practice Task Force of the American Society of Colon and Rectal Surgeons (2013) Practice parameters for the management of pilonidal disease. Dis Colon Rectum 56(9):1021–1027. https://doi.org/10.1097/DCR.0b013e31829d2616
Meinero P, Mori L, Gasloli G (2014) Endoscopic pilonidal sinus treatment (E.P.Si.T.). Tech Coloproctol 18(4):389–392. https://doi.org/10.1007/s10151-013-1016-9
Meinero P, Mori L (2011) Video-assisted anal fistula treatment (VAAFT): a novel sphincter-saving procedure for treating complex anal fistulas. Tech Coloproctol 15:417–422
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta analyses of studies that evaluate health care interventions: explanation and elaboration. BMJ 339:b2700. https://doi.org/10.1136/bmj.b2700
National Institute for Health and Clinical Excellence. NICE clinical guidelines, appendix 4 quality of case series form. http://www.nice.org.uk/nicemedia/pdf/Appendix_04_qualityofcase_series_form_preop.pdf. Accessed 10 Oct 2017
Scottish Intercollegiate Guidelines Network (SIGN) Guidelines, methodology checklist 3. http://www.sign.ac.uk/checklists-and-notes.html. Accessed 10 Oct 2017
Giarratano G, Toscana C, Shalaby M, Buonomo O, Petrella G, Sileri P (2017) Endoscopic pilonidal sinus treatment: long-term results of a prospective series. JSLS. https://doi.org/10.4293/JSLS.2017.00043
Gecim IE, Goktug UU, Celasin H (2017) Endoscopic pilonidal sinus treatment combined with crystalized phenol application may prevent recurrence. Dis Colon Rectum 60(4):405–407. https://doi.org/10.1097/DCR.0000000000000778
Javed MA1, Fowler H, Jain Y, Singh S, Scott M, Rajaganeshan R (2016) Comparison of conventional incision and drainage for pilonidal abscess versus novel endoscopic pilonidal abscess treatment (EPAT). Tech Coloproctol 20(12):871–873
Meinero P, Stazi A, Carbone A, Fasolini F, Regusci L, La Torre M (2016) Endoscopic pilonidal sinus treatment: a prospective multicentre trial. Colorectal Dis 18(5):O164–O170. https://doi.org/10.1111/codi.13322
Milone M, Fernandez LM, Musella M, Milone F (2015) Safety and efficacy of minimally invasive video-assisted ablation of pilonidal sinus: a randomized clinical trial. JAMA Surg 151(6):547–553. https://doi.org/10.1001/jamasurg.2015.5233
Chia CL, Tay VW, Mantoo SK (2015) Endoscopic pilonidal sinus treatment in the Asian population. Surg Laparosc Endosc Percutan Tech 25(3):e95–e97. https://doi.org/10.1097/SLE.0000000000000131
Milone M, Bianco P, Musella M, Milone F (2014) A technical modification of video-assisted ablation for recurrent pilonidal sinus. Colorectal Dis 16(11):O404–O406. https://doi.org/10.1111/codi.12770
Milone M, Musella M, Di Spiezio Sardo A, Bifulco G, Salvatore G, Sosa Fernandez LM, Bianco P, Zizolfi B, Nappi C, Milone F (2014) Video-assisted ablation of pilonidal sinus: a new minimally invasive treatment: a pilot study. Surgery 155(3):562–566. https://doi.org/10.1016/j.surg.2013.08.021.24300343
Bendewald FP, Cima RR (2007) Pilonidal disease. Clin Colon Rectal Surg 20(2):86–95. https://doi.org/10.1055/s-2007-977486
Emile SH, Elfeki H, Shalaby M, Sakr A (2017) A Systematic review and meta-analysis of the efficacy and safety of video-assisted anal fistula treatment (VAAFT). Surg Endosc. https://doi.org/10.1007/s00464-017-5905-2
McCallum IJD, King PM, Bruce J (2008) Healing by primary closure versus open healing after surgery for pilonidal sinus: systematic review and meta-analysis. BMJ 336(7649):868–871. https://doi.org/10.1136/bmj.39517.808160.BE
Garg P, Menon GR, Gupta V (2016) Laying open (deroofing) and curettage of sinus as treatment of pilonidal disease: a systematic review and meta-analysis. ANZ J Surg 86(1–2):27–33. https://doi.org/10.1111/ans.13377
Kayaalp C, Ertugrul I, Tolan K, Sumer F (2016) Fibrin sealant use in pilonidal sinus: systematic review. World J Gastrointest Surg 8(3):266–273. https://doi.org/10.4240/wjgs.v8.i3.266
Elalfy K, Emile S, Lotfy A, Youssef M, Elfeki H (2016) Bilateral gluteal advancement flap for treatment of recurrent sacrococcygeal pilonidal disease: a prospective cohort study. Int J Surg 29:1–8. https://doi.org/10.1016/j.ijsu.2016.03.006
Author information
Authors and Affiliations
Contributions
SHE and MS designed the study. SHE, HE, MS, and AS participated in data collection and analysis, writing and drafting of the manuscript. VG and PS participated in data interpretation, drafting and critical revision of the manuscript. SDW reviewed the collected results on regular basis and participated in drafting and critical revision of the manuscript.
Corresponding author
Ethics declarations
Disclosures
Steven D. Wexner, M.D. is a paid consultant and receives royalties from Karl Storz Endoscopy, America. Sameh Emile, Hossam Elfeki, Mostafa Shalaby, Ahmad Sakr, Valentina Giaccaglia, and Pierpaolo Sileri have no conflict of interests or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Emile, S.H., Elfeki, H., Shalaby, M. et al. Endoscopic pilonidal sinus treatment: a systematic review and meta-analysis. Surg Endosc 32, 3754–3762 (2018). https://doi.org/10.1007/s00464-018-6157-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6157-5