Abstract
Background
Laparoscopic proximal gastrectomy (LPG) with double tract reconstruction (DTR) is known to reduce reflux symptoms, which is a major concern after proximal gastrectomy. The aim of this study is to compare retrospectively the clinical outcomes of patients undergoing LPG with DTR with those treated by laparoscopic total gastrectomy (LTG).
Methods
Ninety-two and 156 patients undergoing LPG with DTR and LTG for proximal stage I gastric cancer were retrospectively analyzed for short- and long-term clinical outcomes.
Results
There were no significant differences in the demographics, T-stage, N-stage, and complications between the groups. The LPG with DTR group had a shorter operative time and lower estimated blood loss than the LTG group (198.3 vs. 225.4 min, p < 0.001; and 84.7 vs. 128.3 mL p = 0.001). The incidence of reflux symptoms ≥ Visick grade II did not significantly differ between the groups during a mean follow-up period of 37.2 months (1.1 vs. 1.9%, p = 0.999). The hemoglobin change was significantly lower in the LPG with DTR group compared to in the LTG group in the first and second postoperative years (5.03 vs. 9.18% p = 0.004; and 3.45 vs. 8.30%, p = 0.002, respectively), as was the mean amount of vitamin B12 supplements 2 years after operation (0.1 vs. 3.1 mg, p < 0.001). The overall survival rate was similar between the groups.
Conclusions
LPG with DTR maintained comparable oncological safety and anastomosis-related late complications compared to LTG and is preferred over LTG in terms of preventing postoperative anemia and vitamin B12 deficiency.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Gastric cancer is the most common malignancy in Korea. The epidemiological characteristics of gastric cancer have changed over the last several decades, with the incidence of early gastric cancer (EGC) in Korea having increased from 24.8 to 48.9% as a result of improved surveillance through the National Cancer Screening Program of Korea. Similarly, the incidence of proximal gastric cancer has also gradually increased from 5.3 to 14.0% in recent years [1].
The Korean Laparoscopic Gastrointestinal Surgery Study Group recently reported that the long-term oncologic outcomes of laparoscopic gastrectomy for patients with gastric cancer were comparable to those of open gastrectomy [2]. Moreover, many other groups have also reported the oncological safety of laparoscopic gastrectomy [3, 4]; accordingly, various extents of laparoscopic gastrectomy and various reconstruction methods according to the different kinds of gastrectomy have been attempted.
On the other hand, laparoscopic proximal gastrectomy (LPG) is generally not considered as a suitable operation for proximal EGC in Korea. In fact, in 2009, in spite of the increased incidence of proximal EGC, proximal gastrectomy (PG) comprised only 1% (141 cases) of all gastric operations in Korea, including open cases [5]. In several previous studies, the oncological safety of PG for proximal EGC has been demonstrated to be comparable to that of total gastrectomy (TG) [6–9]; however, the unpopularity of PG is largely due to the high incidences of reflux symptoms and anastomotic stenosis associated with this method, with approximately 21.4–56.2% of patients experiencing reflux symptoms or anastomotic stenosis after PG [9–12]. In addition, LPG is considered a relatively technically demanding procedure.
We have previously compared the clinical outcomes between LPG with esophagogastrostomy (EG) and laparoscopic TG (LTG) for proximal EGC and concluded that EG after LPG was associated with an increased risk of reflux symptoms (32.0%) [9]. Based on this previous study, we have been attempting double tract reconstruction (DTR) after LPG for reducing reflux symptoms since 2009. Our initial case series of LPG with DTR demonstrated that it is a feasible, simple, and useful reconstruction method with excellent postoperative outcomes in terms of preventing reflux symptoms [13]. However, no comparison of the late clinical outcomes of LPG with DTR and LTG has yet been conducted.
Therefore, the aim of this study was to compare the long-term outcomes in terms of late complications and nutritional status between patients who underwent DTR after LPG and those treated by LTG.
Methods
Patients
Between June 2003 and April 2015, 256 patients with confirmed pathological stage I gastric cancer (pT1N0, T1N1, and T2N0) treated with curative LPG with DTR or LTG at the Seoul National University Bundang Hospital, were enrolled in the present study. The gastric cancer stage was classified according to the seventh edition of the American Joint Committee on Cancer and the Union for International Cancer Control guidelines.
Because other treatments and malignancies may affect the nutritional status, patients with adjuvant chemotherapy for pathological more than stage II gastric cancer, combined splenectomy, other malignancy, or recurrent gastric cancer were excluded from our analyses. Moreover, patients with an incomplete follow-up of less than 1 year were also excluded since their long-term nutritional status could not be evaluated.
The surgical procedure, namely LPG with DTR or LTG, was chosen at the discretion of the surgeons and patients. The 2010 Japanese gastric cancer treatment guidelines suggested the preservation of more than half of the distal stomach in the PG. Therefore, if the remnant stomach was too small for some functional benefit to be gained from preserving the stomach, the surgeons would perform LTG. There were 92 and 156 patients in the LPG with DTR and LTG groups, respectively.
Evaluation of clinical parameters
The clinical, operative, and pathological variables were compared between the LPG with DTR and LTG groups based on the information obtained from our prospectively collected surgical database. Early postoperative complications (occurring on postoperative days 0–30) were graded using the Clavien–Dindo classification [14]. Early postoperative complications requiring medical, radiological, or surgical interventions (grade 2 or higher) were regarded as an event. Morbidity was classified as follows: (i) local complications, including wound infection, fluid collection/abscess, anastomosis leakage, stenosis, intestinal obstruction, ileus, intraluminal bleeding, intra-abdominal bleeding, and pancreatitis and (ii) systemic complications, including pulmonary, renal, urinary, cardiac, and neurologic problems, as defined in our previous study [15].
Late postoperative complications (after postoperative day 30) requiring radiological or surgical interventions were regarded as an event; these included ileus, internal hernia, cholecystitis, reflux symptoms, and anastomotic stenosis. Reflux symptoms and anastomotic stenosis were diagnosed according to the symptoms and endoscopic findings, and the reflux symptoms were classified using the modified Visick score [16]. If a 9-mm diameter endoscope could not pass through an anastomosis of a patient complaining of dysphagia, anastomotic stenosis was diagnosed. Nutritional status and anemia were evaluated by the changes in body weight and laboratory data (total protein, albumin, cholesterol, and hemoglobin) in the first and second postoperative year. The amount of vitamin B12 supplements was also calculated.
Techniques
LPG with DTR
The lymph node (LN) stations were numbered according to the Japanese classification of gastric cancer (3rd English Edition) [17]. Our LPG with DTR technique has been previously described in detail [13]. Briefly, LN stations 1, 2, 3a, 4sa, 4sb, 7, 8a, 9, and 11p were dissected, and the left gastroepiploic and left gastric vessels were subsequently ligated. The right gastroepiploic vessels, right gastric vessels, and the hepatic and pyloric branches of the vagus nerves were routinely preserved. Intracorporeal Roux-en-Y end-to-side esophagojejunostomy (EJ) was performed using an endoscopic purse-string instrument, after the left lower port was extended to a length of approximately 3 cm in order to remove the specimen and to insert a circular stapler. Next, side-to-side GJ, 10 cm below the EJ was performed in an extracorporeal fashion using 2 laparoscopic linear staplers. Finally, end-to-side jejunojejunostomy (JJ), 20 cm below the GJ, was performed using an extracorporeal hand-sewing suture.
LTG
Our LTG technique has been previously described [18]. Briefly, in addition to the LPG with DTR procedures, the following procedures were added for LTG: the right gastric and gastroepiploic vessels were divided at their origins, and LN stations 3b, 4d, 5, and 6 were dissected. In some cases, such as clinically equivocal EGC, D2 LN dissection was attempted, in which LN stations 10, 11d, and 12a were dissected. The duodenum was transected 2 cm distal to the pylorus, using a laparoscopic linear stapler. Most cases of intracorporeal Roux-en-Y EJ with JJ were performed using the same procedures as for LPG with DTR.
Ethics statement
This study protocol was approved by the Institutional Review Board of Seoul National University Bundang Hospital (B1502-286-115).
Statistical analysis
Statistical analyses were performed using Student’s t test for continuous variables. The χ2 test was used for analysis of categorical variables. All statistical analyses were performed with PASW statistics 18 software (SPSS, New York, NY, USA), and p < 0.05 was considered statistically significant.
Results
Patient demographic, operative, and pathological characteristics
The patient demographic, operative, and pathological characteristics are provided in Table 1. The two groups were comparable in terms of age, sex, comorbidities, and body mass index.
In terms of the operative characteristics, the mean operative time was shorter (198.3 ± 38.8 vs. 225.4 ± 51.6 min, p < 0.001) and the estimated blood loss was lower in the LPG with DTR group compared to in the LTG group (84.7 ± 81.7 vs. 128.3 ± 112.5 mL, p = 0.001). D1+ LN dissection was performed in all 92 cases of LPG with DTR, whereas there were 86 and 70 cases of D1+ LN and D2 LN dissection, respectively, in the LTG group.
In terms of the pathological characteristics, there were no significant differences in the T-stage, N-stage, and proximal resection margins between the groups. The mean tumor size was larger (2.4 ± 1.3 vs. 3.2 ± 1.9 cm, p < 0.001), the distal resection margin was longer (2.9 ± 2.3 vs. 12.2 ± 4.0 cm, p < 0.001), and the number of retrieved LNs was higher (46.1 ± 19.6 vs. 60.0 ± 25.7, p < 0.001) in the LTG group compared to in the LPG with DTR group.
Postoperative course and early complications
The postoperative course and early complications are summarized in Table 2. The time of gas-passing and postoperative hospital stay were similar between the two groups, and the time of solid food initiation was also similar in the LPG with DTR group. The early complication rates were 10.9 and 18.6% in the LPG with DTR and LTG groups, respectively, and there was no statistically significant difference in the early complications between the 2 groups. Anastomotic leakage occurred in 2 patient (2.2%) in the LPG with DTR group and 3 patients (1.9%) in the LTG group (p = 0.999). There were 6 re-operations (p = 0.999) for bleeding (LPG with DTR, n = 1; LTG, n = 2) and mechanical ileus (LTG, n = 3). There was no case of mortality in the early stage (until postoperative day 30).
Late complications
Late complications occurred in 8 patients (8.7%) in the LPG with DTR group and 22 patients (14.1%) in the LTG group, with no statistically significant difference observed between the 2 groups (Table 2). In the LPG with DTR group, only one patient underwent re-operation for internal hernia at postoperative month 7. Conversely, in the LTG group, 11 patients underwent re-operations (p = 0.284) for mechanical ileus (n = 1), internal hernia (n = 7), and cholecystitis (n = 3). Four patients (LPG with DTR, n = 1; LTG, n = 3) showed reflux symptoms, all of which were classified as Visick grade II (p = 0.999). Five patients (LPG with DTR, n = 3; LTG, n = 2) with stenosis upon EJ were treated completely by balloon dilatation (p = 0.175).
Nutritional status and anemia
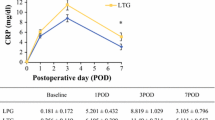
The decrease rates of body weight and laboratory data were used as indicators of postoperative nutritional status and anemia (Fig. 1). The decrease rates of the serum total protein, albumin, and total cholesterol levels (%) did not significantly differ in either the first or second postoperative year between the 2 groups (Fig. 1A–C). The rate of body weight change (%) was significantly lower in the LPG with DTR group than in the LTG group in the first and second postoperative year (Fig. 1D). Further, the decrease rate of hemoglobin (%) was significantly lower in the LPG with DTR group than in the LTG group in both the first and second postoperative years (Fig. 1E).
Comparison of nutritional status and anemia in the first and second postoperative years (decrease rate, %) between laparoscopic proximal gastrectomy with double tract reconstruction and laparoscopic total gastrectomy. LPG Laparoscopic proximal gastrectomy, DTR double tract reconstruction, LTG laparoscopic total gastrectomy. A Total protein, B albumin, C total cholesterol, D body weight 1 year, p = 0.036; 2 year, p = 0.049, E hemoglobin, 1 year, p = 0.004; 2 year, p = 0.002
The serum vitamin B12 levels were significantly higher in the LPG with DTR group than in the LTG group in both the first and second postoperative years (Fig. 2). Five patients (5.4%) in the LPG with DTR group and 138 patients (88.5%) in the LTG group were supplemented with vitamin B12 (actinamide 1 mg; Shin Poong Pharm., Seoul, Korea) for 2 years after the operation. Accordingly, the mean amount of vitamin B12 supplements was lower in the LPG with DTR group than in the LTG group 2 years after the operation (0.1 ± 0.4 vs. 3.1 ± 2.2 mg, p < 0.001).
Comparison of serum vitamin B12 levels in the first and second postoperative years between laparoscopic proximal gastrectomy with double tract reconstruction and laparoscopic total gastrectomy. LPG Laparoscopic proximal gastrectomy, DTR double tract reconstruction, LTG laparoscopic total gastrectomy
Recurrence and survival
There was no recurrence in the patients with confirmed stage I gastric cancer after LPG with DTR. However, there were three recurrent cases (1.9%) with stage I gastric cancer pathologically confirmed after LTG, and these three recurrent cases were excluded in the present study. The overall survival rates were similar between the 2 groups (Fig. 3): the 5-year survival rates were 96.1 and 95.9% for the LPG with DTR and LTG groups, respectively (p = 0.575).
Discussion
The epidemiological characteristics of gastric cancer have changed over the last several decades in Korea, with the incidences of EGC and proximal gastric cancer having increased continuously during the past 20 years [1]. Accordingly, the use of laparoscopic gastrectomy has also increased in recent years, owing largely to reports of its superior short-term and comparable long-term oncological outcomes [2–4]. However, LPG is not considered a suitable operation for proximal EGC. In addition, open proximal gastrectomy (OPG) has also recently lost popularity [5]. This unpopularity of OPG and LPG can be attributed to three main concerns, namely their oncological safety, functional benefits, and anastomosis-related late complications [19, 20].
In terms of OPG, these three concerns have been evaluated in numerous studies. In several recent studies, it was demonstrated that OPG and open total gastrectomy had similar 5-year overall and disease-specific survival rates for proximal gastric cancer [6–8]. The functional benefits of OPG have been also reported in terms of preventing postoperative anemia and subjective symptoms [6, 7, 21, 22]. However, although many different types of reconstruction have been attempted to solve the issues of reflux symptoms and anastomotic stenosis, two well-established complications, none has yet been successful. To date, modification of EG after OPG has shown disappointing results in the rates of both reflux symptoms and anastomotic stenosis [10–12], and hence, various types of EJ after OPG have been recently studied to prevent reflux symptoms, including jejunal interposition and jejunal pouch interposition [12, 23]. While the incidence of reflux symptoms after OPG with EJ is reportedly similar to that after open total gastrectomy with Roux-en-Y anastomosis, these procedures for reconstruction are thought to be technically complex under laparoscopy.
Because of these unsolved late complications associated with OPG and the technical demanding procedure of reconstruction by LPG, there are relatively few cases of LPG, and the reports comparing LPG with LTG are therefore scarce. At our institution, LPG with EG has also been performed since May 2003, and we have previously reported that the 5-year overall survival rate was similar between patients treated with LPG with EG and LTG [9]. In the present study, there was no recurrent case in patients confirmed with stage I gastric cancer after LPG with DTR, whereas there were three recurrent cases (1.9%) among the 189 patients with pathologically confirmed stage I gastric cancer after LTG. However, we excluded patients treated with adjuvant chemotherapy for pathological more than stage II gastric cancer from this analysis, including 8 cases (8.0%) in the LPG with DTR group and 30 cases (16.1%) in the LTG group, as the addition of chemotherapy may affect the nutritional status and laboratory results. In addition, the overall survival and disease-specific survival rates were also similar between the two groups, including in the excluded cases undergoing adjuvant chemotherapy; however, the mean follow-up period was relatively short (26.6 ± 10.3 months) in the LPG with DTR group. Moreover, tumor recurrence was found in 2 out of 8 patients with adjuvant chemotherapy in the LPG with DTR group; hepatic metastasis was found in one patient with pathologically confirmed stage IIIb at 30 months after LPG with DTR; and peritoneal carcinomatosis was found in the other patient with confirmed stage IIb disease at 24 months after LPG with DTR. Importantly, among the 8 patients with adjuvant chemotherapy, only one recurrent patient diagnosed with hepatic metastasis expired; therefore, further studies with longer follow-up periods are required for evaluating the long-term survival rates.
The present study showed that LPG with DTR is a feasible and safe technique in terms of the operative time, estimated blood loss, and early and late complications. In our previous report, in which we found that LPG with EG stomy is also a feasible and safe technique, the late complication rates, especially for reflux symptoms and anastomotic stenosis, were substantially high [9], and therefore, we could not conclude that LPG with EG was a good alternative to LTG. However, in the present study, the late complication rates were similar in the LPG with DTR and LTG groups, and there were no patients with a Visick score of III or IV in either group. All anastomosis-related late complications of LTG and LPG with DTR occurred before May 2009 and October 2011, respectively, indicating that the anastomosis-related complication rates decreased significantly after the learning curve of LTG was overcome [24]. In terms of LPG with DTR, we have changed the distance from the EJ to GJ; in the early period, the GJ was made at 10 cm below the EJ. Using this previous approach, after we closed the common entry hole using a linear stapler, we found that the distance from the EJ to the GJ was only about 5–7 cm. Previous studies have reported that there is a close relationship between the distance of anastomosis and anastomosis-related late complications in the jejunal interposition after OPG. Therefore, we changed the distance of anastomosis from 10 cm before the closure of common entry hole to 10 cm after the closure (Fig. 4). Thus, we now create the GJ at approximately 15 cm below the EJ at the late phase. After changing the distance of the anastomosis, we have not encountered any anastomosis-related late complications among the 76 cases of LPG with DTR.
In the present study, functional benefits of LPG with DTR were observed in terms of preventing postoperative anemia. We supplemented vitamin B12 to the patients whose serum vitamin B12 levels were less than 200 pg/mL or continuously decreasing, and the serum vitamin B12 level of the LPG with DTR group was found to be significantly higher than that of the LTG group. Furthermore, while 138 (88.5%) patients in the LTG group were supplemented with intravenous injection of vitamin B12 for 2 years postoperatively, only 5 (5.4%) patients in the LPG with DTR group were supplemented. However, nonetheless, the hemoglobin level of the LTG group was significantly lower than that of LPG with DTR in spite of the vitamin B12 supplementation in the second postoperative year.
The regular endoscopic evaluations of patients undergoing LPG with DTR have been reported to lead to earlier detection and curative resection of remnant gastric cancer. It has been reported that the rate of remnant gastric cancer is 5–5.4% after OPG [6, 25], and we have previously reported that 3 intubation failures occurred among 43 patients undergoing LPG with DTR during the examination for remnant distal stomach cancer [13]. However, the endoscopists were able to evaluate the distal remnant stomach of these 3 patients at the next endoscopic follow-up, after the surgeons had explained to the endoscopists how to re-make the double tract reconstruction. In our institution, the distal remnant stomach of all patients undergoing LPG with DTR is evaluated by endoscopists, and, to date, tumor recurrence has not been found in the remnant stomach of any patient undergoing LPG with DTR (mean follow-up period, 26.6 months). Thus, regular and repeated communication between surgeons and endoscopists is recommended for the early detection of remnant gastric cancer after LPG with DTR.
The present study has some limitations, including its retrospective design. Moreover, we did not assess the quality of life of the patients, as we do not routinely use a validated questionnaire in the out-patient clinic. However, to our knowledge, this is the first study to report the superiority of LPG with DTR over LTG, and this observed superiority has lead us to plan a phase III multicenter prospective randomized clinical trial comparing LPG with DTR with LTG (Korean Laparoscopic Gastrointestinal Surgery Study Group (KLASS)—05).
In conclusion, we here found that LPG with DTR maintains comparable oncological safety and anastomosis-related late complications to LTG and is preferred over LTG in terms of preventing postoperative anemia and vitamin B12 deficiency.
References
Ahn HS, Lee HJ, Yoo MW, Jeong SH, Park DJ, Kim HH, Kim WH, Lee KU, Yang HK (2011) Changes in clinicopathological features and survival after gastrectomy for gastric cancer over a 20-year period. Br J Surg 98(2):255–260. doi:10.1002/bjs.7310
Kim HH, Han SU, Kim MC, Hyung WJ, Kim W, Lee HJ, Ryu SW, Cho GS, Song KY, Ryu SY (2014) Long-term results of laparoscopic gastrectomy for gastric cancer: a large-scale case-control and case-matched Korean multicenter study. J Clin Oncol 32(7):627–633. doi:10.1200/JCO.2013.48.8551
Choi YY, Bae JM, An JY, Hyung WJ, Noh SH (2013) Laparoscopic gastrectomy for advanced gastric cancer: are the long-term results comparable with conventional open gastrectomy? A systematic review and meta-analysis. J Surg Oncol 108(8):550–556. doi:10.1002/jso.23438
Wang W, Zhang X, Shen C, Zhi X, Wang B, Xu Z (2014) Laparoscopic versus open total gastrectomy for gastric cancer: an updated meta-analysis. PloS ONE 9(2):e88753. doi:10.1371/journal.pone.0088753
Jeong O, Park YK (2011) Clinicopathological features and surgical treatment of gastric cancer in South Korea: the results of 2009 nationwide survey on surgically treated gastric cancer patients. J Gastric Cancer 11(2):69–77. doi:10.5230/jgc.2011.11.2.69
Nozaki I, Hato S, Kobatake T, Ohta K, Kubo Y, Kurita A (2013) Long-term outcome after proximal gastrectomy with jejunal interposition for gastric cancer compared with total gastrectomy. World J Surg 37(3):558–564. doi:10.1007/s00268-012-1894-4
Masuzawa T, Takiguchi S, Hirao M, Imamura H, Kimura Y, Fujita J, Miyashiro I, Tamura S, Hiratsuka M, Kobayashi K, Fujiwara Y, Mori M, Doki Y (2014) Comparison of perioperative and long-term outcomes of total and proximal gastrectomy for early gastric cancer: a multi-institutional retrospective study. World J Surg 38(5):1100–1106. doi:10.1007/s00268-013-2370-5
Ikeguchi M, Kader A, Takaya S, Fukumoto Y, Osaki T, Saito H, Tatebe S, Wakatsuki T (2012) Prognosis of patients with gastric cancer who underwent proximal gastrectomy. Int Surg 97(3):275–279. doi:10.9738/CC150.1
Ahn SH, Lee JH, Park do J, Kim HH (2013) Comparative study of clinical outcomes between laparoscopy-assisted proximal gastrectomy (LAPG) and laparoscopy-assisted total gastrectomy (LATG) for proximal gastric cancer. Gastric Cancer 16(3):282–289. doi:10.1007/s10120-012-0178-x
Ronellenfitsch U, Najmeh S, Andalib A, Perera RM, Rousseau MC, Mulder DS, Ferri LE (2014) Functional outcomes and quality of life after proximal gastrectomy with esophagogastrostomy using a narrow gastric conduit. Ann Surg Oncol. doi:10.1245/s10434-014-4078-7
An JY, Youn HG, Choi MG, Noh JH, Sohn TS, Kim S (2008) The difficult choice between total and proximal gastrectomy in proximal early gastric cancer. Am J Surg 196(4):587–591. doi:10.1016/j.amjsurg.2007.09.040
Nakamura M, Nakamori M, Ojima T, Katsuda M, Iida T, Hayata K, Matsumura S, Kato T, Kitadani J, Iwahashi M, Yamaue H (2014) Reconstruction after proximal gastrectomy for early gastric cancer in the upper third of the stomach: an analysis of our 13-year experience. Surgery 156(1):57–63. doi:10.1016/j.surg.2014.02.015
Ahn SH, Jung do H, Son SY, Lee CM, Park do J, Kim HH (2014) Laparoscopic double-tract proximal gastrectomy for proximal early gastric cancer. Gastric Cancer 17(3):562–570. doi:10.1007/s10120-013-0303-5
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Kim HH, Hyung WJ, Cho GS, Kim MC, Han SU, Kim W, Ryu SW, Lee HJ, Song KY (2010) Morbidity and mortality of laparoscopic gastrectomy versus open gastrectomy for gastric cancer: an interim report—a phase III multicenter, prospective, randomized Trial (KLASS Trial). Ann Surg 251(3):417–420. doi:10.1097/SLA.0b013e3181cc8f6b
Goligher JC, Feather DB, Hall R, Hall RA, Hopton D, Kenny TE, Latchmore AJ, Matheson T, Shoesmith JH, Smiddy FG, Willson-Pepper J (1979) Several standard elective operations for duodenal ulcer: ten to 16 year clinical results. Ann Surg 189(1):18–24
Japanese Gastric Cancer Association (2011) Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer 14(2):101–112. doi:10.1007/s10120-011-0041-5
Lee JH, Ahn SH, Park do J, Kim HH, Lee HJ, Yang HK (2012) Laparoscopic total gastrectomy with D2 lymphadenectomy for advanced gastric cancer. World J Surg 36(10):2394–2399. doi:10.1007/s00268-012-1669-y
Ahn SH, Lee JH, Park do J, Kim HH (2013) Laparoscopy-assisted proximal gastrectomy for early gastric cancer is an ugly duckling with unsolved concerns: oncological safety, late complications, and functional benefit. Gastric Cancer 16(3):448–450. doi:10.1007/s10120-013-0245-y
Hiki N, Nunobe S, Kubota T, Jiang X (2013) Function-preserving gastrectomy for early gastric cancer. Ann Surg Oncol 20(8):2683–2692. doi:10.1245/s10434-013-2931-8
Namikawa T, Oki T, Kitagawa H, Okabayashi T, Kobayashi M, Hanazaki K (2012) Impact of jejunal pouch interposition reconstruction after proximal gastrectomy for early gastric cancer on quality of life: short- and long-term consequences. Am J Surg 204(2):203–209. doi:10.1016/j.amjsurg.2011.09.035
Takiguchi N, Takahashi M, Ikeda M, Inagawa S, Ueda S, Nobuoka T, Ota M, Iwasaki Y, Uchida N, Kodera Y, Nakada K (2014) Long-term quality-of-life comparison of total gastrectomy and proximal gastrectomy by Postgastrectomy Syndrome Assessment Scale (PGSAS-45): a nationwide multi-institutional study. Gastric Cancer 18:407–416. doi:10.1007/s10120-014-0377-8
Zhao P, Xiao SM, Tang LC, Ding Z, Zhou X, Chen XD (2014) Proximal gastrectomy with jejunal interposition and TGRY anastomosis for proximal gastric cancer. World J Gastroenterol 20(25):8268–8273. doi:10.3748/wjg.v20.i25.8268
Jung DH, Son SY, Park YS, Shin DJ, Ahn HS, Ahn SH, Park do J, Kim HH (2016) The learning curve associated with laparoscopic total gastrectomy. Gastric Cancer 19(1):264–272. doi:10.1007/s10120-014-0447-y
Ohyama S, Tokunaga M, Hiki N, Fukunaga T, Fujisaki J, Seto Y, Yamaguchi T (2009) A clinicopathological study of gastric stump carcinoma following proximal gastrectomy. Gastric Cancer 12(2):88–94. doi:10.1007/s10120-009-0502-2
Acknowledgement
The authors have been awarded the research grant from Korean National Strategic Coordinating Center of Clinical Research (Grant No.: HI10V0084010014).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Do Hyun Jung, Yoontaek Lee, Dong Wook Kim, Young Suk Park, Sang-Hoon Ahn, Do Joong Park and Hyung-Ho Kim have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Jung, D.H., Lee, Y., Kim, D.W. et al. Laparoscopic proximal gastrectomy with double tract reconstruction is superior to laparoscopic total gastrectomy for proximal early gastric cancer. Surg Endosc 31, 3961–3969 (2017). https://doi.org/10.1007/s00464-017-5429-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5429-9