Abstract
Introduction
Peroral endoscopic myotomy (POEM) is a novel intervention for the treatment of achalasia, which combines the advantages of endoscopic access and myotomy. The purpose of this study was to perform a systematic review of the literature to evaluate the efficacy and safety of POEM.
Methods
The systematic review was conducted following the PRISMA guidelines. Evidence-Based Medicine Reviews, Cochrane Central Register of Controlled Trials, Ovid MEDLINE (R) including in-process and non-indexed citations were searched for POEM studies using the keywords: esophageal achalasia, POEM, endoscopy, natural orifice surgery, laparoscopic Heller myotomy (LHM), and related terms. Eckardt score, lower esophageal sphincter (LES) pressure, and reported complications were the main outcomes. Two authors reviewed the search result independently. A third reviewer resolved all disagreements. Data abstraction was pilot-tested and approved by all authors. Data were examined for clinical, methodological, and statistical heterogeneity with the aim of determining whether evidence synthesis using meta- analysis was possible.
Results
The search strategy retrieved 2894 citations. After removing duplicates and applying the exclusion criteria, 54 studies were selected for full-text review of which a total of 19 studies were considered eligible for further analysis. There were 10 retrospective and 9 prospective studies, including 1299 POEM procedures. No randomized control trial (RCT) was identified. Overall, the pre- and post-POEM Eckardt scores and LES pressure were significantly different. The most frequently reported complications were mucosal perforation, subcutaneous emphysema, pneumoperitoneum, pneumothorax, pneumomediastinum, pleural effusion, and pneumonia. The median follow-up was 13 months (range 3–24).
Conclusion
POEM is a safe and effective alternative for the treatment of achalasia. However, only short-term follow-up data compared with LHM are available. RCTs and long-term follow-up studies are needed to establish the efficacy and safety of POEM in the management of patients with achalasia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Achalasia is an esophageal motility disorder manometrically characterized by a non-relaxing lower esophageal sphincter (LES) in association with aperistalsis of the esophageal body. It is a rare condition, with an incidence of 0.3–1.63–100,000 adults/year and prevalence of 8.7–10.8–100,000 [1, 2]. Although multiple theories (viral, inflammatory, autoimmune) targeting esophageal ganglion cells have been studied, the cause of neuronal degeneration in the esophageal wall remains unknown.
Achalasia was recognized more than 300 years ago as a disease that impairs the ability to swallow. At that time, the proposed treatment consisted of traumatic dilation of the gastroesophageal junction using a whalebone [3]. In 1913, Ernest Heller performed the first successful operation for achalasia describing an anterior and posterior lower esophageal myotomy through a laparotomy. The surgical technique evolved into a single anterior myotomy, through a left posterior thoracotomy resulting in a symptomatic success rate of 60–94 % [4]. Nonetheless, the relatively high morbidity of this approach made it less attractive than dilation techniques until the advent of the minimally invasive surgical approach in the early 1990s [5, 6].
Despite the fact that surgical technique has changed, the target of reducing the LES gradient pressure remains the same. Furthermore, the extension of the myotomy 3 cm onto the proximal stomach in order to divide the gastric sling fibers to further decrease LES pressure has been associated with improved results. The resulting gastroesophageal reflux is addressed with an antireflux procedure [7].
Laparoscopic Heller myotomy (LHM) is considered the standard of care since it provides superior and long-lasting symptom relief for patients with achalasia compared to other modalities of treatment, reserving endoscopic treatments to frail and/or aged patients or those who refuse to have an operation [8–12]. However, advances in endoscopic procedures which are even less invasive than laparoscopy have brought a novel endoscopic option named peroral endoscopic myotomy (POEM) into the discussion.
The use of POEM for the treatment of achalasia was first reported in 1980. This technique was described by Ortega et al. [13] as a mucosal and circular muscle myotomy that was performed above the gastroesophageal junction (GEJ) and using an endoscopic knife developed by the same group. Nevertheless, it was not universally accepted due to concerns of high risk of perforation. In 2007, Pasricha et al. [14, 15] reported the feasibility of performing endoscopic esophageal myotomy in four pigs by creating a submucosal esophageal tunnel; however, it was not until 2010 when the first human study was published. Since then, the procedure has expanded and is becoming more widely adopted by gastroenterologists and surgeons.
With the increased interest in replacing LHM with the less invasive POEM over the last 5–6 years, it is essential to assess the available efficacy and safety data of POEM to guide management decisions and future research. We aim to evaluate the effect of POEM in reducing LES resting pressure and symptom improvement.
Methods
Protocol
A systematic search was performed in Medline, Embase, Cochrane Central Register, and PubMed to identify all citations investigating the efficacy and or safety of POEM to treat patients with achalasia until February 2015. Our search strategy is shown in Appendix 1 in electronic supplementary material. Keywords including esophageal achalasia, peroral endoscopic myotomy, endoscopy, natural orifice surgery, laparoscopic Heller myotomy, and related terms were used. Studies using human subjects with no ethnicity, age, or language restrictions were included. Narrative letters or reviews and studies reporting less than 10 subjects were excluded for full-text eligibility.
After full-text analysis, we also excluded studies with less than 3 months of follow-up, repetitive data, and lack of LES resting pressure and Eckardt score. The systematic review was preformed following the (PRISMA) guidelines [16].
Articles in non-English language were translated with SYSTRAN software. At the time of the search, no published RCT was found. Thus, we consulted clinicaltrials.gov, confirming the status of “recruiting patients” for two ongoing randomized trials comparing POEM versus LHM (identifiers: NCT02138643 and NCT01601678). Additional records were obtained from bibliography and abstracts searched from the Society of American Gastrointestinal and Endoscopic Surgeons and Digestive Disease conferences between 2010 and 2015.
Two authors reviewed all identified citations from the literature search. Those studies that aim to explore POEM efficacy using Eckardt score and/or LES pressure and those reporting complications were selected for full-text review to determine whether they met inclusion criteria. A third reviewer resolved all disagreements. A data abstraction form was pilot-tested and approved by all authors. Two authors performed data extraction independently.
We explored heterogeneity among studies to determine the appropriateness and validity of pooling evidence across the studies using meta-analysis. Clinical and methodological heterogeneity was assessed through a careful examination of study, intervention, and patient characteristics. Statistical heterogeneity was examined (and quantified) using the I 2 statistic. Analysis was done for preoperative and postoperative data separately as well as for mean change between pre- and postoperation data. In the analysis involving mean change, complete data including standard error of mean change were not provided in all the studies. When incomplete, correlation between pre- and postoperative outcomes was calculated from studies with complete data. Standard error of the mean change was, consequently, imputed using the standard errors of preoperative and postoperative mean values and correlation estimates from similar studies. NIH tools and guidelines for case series, case control, and before and after studies were independently and dually utilized to assess risk of bias (18). Due to marked variability in study design, quality of the data, participants, and outcome measures as well as the observed high statistical heterogeneity, study-level estimates are presented in forest plots without pooling the estimates across the studies. The heterogeneity estimates are also presented.
Types of intervention
Only the intervention of peroral endoscopic myotomy (POEM) as described by Inoue et al. [15] was included. This procedure follows four consecutive steps: (a) mucosal incision and entry in the submucosa; (b) creation of the submucosal tunnel; (c) esophageal myotomy; (d) closure of the mucosal incision.
The laparoscopic Heller myotomy with fundoplication which included the following main steps: (a) mobilization of the gastric fundus and mediastinal esophagus; (b) esophagogastric myotomy; (c) partial fundoplication (Dor or Toupet).
Outcome
The outcomes of interest were efficacy and safety. Efficacy was evaluated as improvement in symptom scores and LES pressure profile measured by manometry. Eckardt score is the most commonly used symptom score for assessing the severity of achalasia [17]; it is the sum of the scores for dysphagia, regurgitation, and chest pain on a scale from 0 to 3 (0 = absent, 1 = occasional, 2 = daily, 3 = each meal) and weight loss (0 = no weight loss, 1 = <5 kg, 2 = 5–10 kg, 3 = >10 kg). The total score ranges from 0 to 12 points. Clinical remission was defined as an Eckardt score of ≤3.
Safety of the procedure was assessed by reported complications including the development of gastroesophageal reflux disease (GERD) measured by postoperative 24-h pH studies.
Study selection for analysis
To avoid duplicate data, we include the latest paper and/or the one with the biggest sample size from the same author or center when there was juxtaposition of author names or centers. Seven of the ten investigators who were contacted to clarify study eligibility responded. We developed a data abstraction form considering relevant outcomes to answer the research question. The form was pilot-tested by one of the authors and accepted with modifications by all authors in consensus.
Extracted data included study characteristics, demographics (BMI, age, and gender), previous treatments, details of the surgical intervention, primary outcome results, GERD assessment, and length of follow-up.
Results
General description
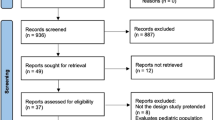
Our search strategy identified 2894 citations. After duplicates were removed, two reviewers assessed 2112 citations, of which 54 studies were eligible for full-text evaluation (see Fig. 1, PRISMA flow diagram). No randomized control trials were found. All 54 studies were considered in our qualitative analysis; nevertheless, some of the studies were excluded due to data repetition and other important characteristics we present below. A total of 19 of 54 studies were included in the final qualitative analysis [15, 18–70].
Among 54 studies, five compared efficacy of POEM versus LHM [22, 27, 31, 33, 54] as shown in Table 1. Another study compared the extension of the myotomy to normalize EGJ distensibility between POEM and LHM [46]. Other comparisons included POEM in patients with and without previous endoscopic treatment [20, 29, 48], longitudinal versus modified mucosal incision [60, 69], water jet versus conventional dissection [23]. There were no comparisons with PD.
Exclusion of studies
Twenty-eight studies reported repetitive data from the same center/cohort of patients [14, 17, 20, 22–25, 27–43, 45, 46, 49, 54], five reported outcomes with less than 3 months of follow-up [18, 19, 21, 26, 50], and two did not report outcomes using Eckardt score or LES pressure [44, 48]. All were excluded for qualitative synthesis.
Qualitative analysis of the included studies
Nineteen studies were included in the qualitative analysis. Success rate of completing the procedure and the effectiveness in achieving a postoperative Eckardt score of lower than 3 were high. Of 1310 POEM procedures attempted, 1299 were completed (99 %) of which post-procedural Eckardt score was available in 1228 patients. The procedure was considered effective in 1171 patients (Eckardt score < 3 in all studies except one which used Eckardt score < 4) [65]. Post-procedure LES resting pressure was reported in 836 cases (Table 2). Age and sex were reported in 17 of 19 studies. Only 3 studies reported BMI [47, 52, 64]. Ten retrospective and nine prospective studies were identified. No randomized control trial was found. Seventeen studies reported the presence of previous treatment, but the type of intervention or number of pre-POEM treatments was not uniformly described. Thus, we grouped any previous endoscopic treatment (n = 289) and previous Heller myotomy (n = 36). Nine studies reported the presence of sigmoid esophagus in 99 patients (Table 2).
Technical aspects of POEM
Myotomy length was not uniformly reported. Seventeen of 19 studies reported the total length of myotomy, and only seven studies reported the length of gastric extension. The total length of myotomy was variable from 5.4 to 26 cm (Table 3). The most frequent myotomy technique was reported as a “partial” or “circular,” referring to the dissection involving only the circular muscle layer, preserving the longitudinal muscle layer. There was a paucity of data reporting the number of “full-thickness” myotomies either intentionally or inadvertently as part of the procedure (Table 3).
Main outcomes and heterogeneity among studies
All 19 studies reported pre- and post-POEM Eckardt score and/or LES pressure. However, 5 studies did not provide any measure of variability (e.g., SD, IQR, or range) for the preoperative Eckardt score and hence were not included in the statistical analysis. A very high statistical heterogeneity was observed in both the pre- and postoperative Eckardt scores. Fourteen studies reported the preoperative Eckardt score (I 2 = 89.45 %), and 13 studies reported the postoperative Eckardt score (I 2 = 97.28 %) (Fig. 2). We also investigated the distribution of mean change in POEM Eckardt score between pre- and postoperation across the studies for which data are available. The results show that an improvement was observed across all the studies; however, there is high level of heterogeneity (I 2 = 90.24 %) in mean change from preoperation. Heterogeneity in mean change was still high when prospective and retrospective studies are considered separately, where I 2 = 80.95 % for prospective studies and I 2 = 94.71 % for retrospective studies. Given the high level of heterogeneity, pooling of the estimates is not recommended, and hence pooled estimates are not provided. Study-level mean change in Eckardt score between pre- and postoperation with the corresponding 95 % CI is shown in a forest plot (Fig. 3).
Preoperative LES pressure profiles were reported in 11 studies. Of those, 10 reported postoperative data for comparative analysis. Similar to the Eckardt score, a high level of heterogeneity (Fig. 3) was observed in both pre- and postoperative LES pressures (I 2 = 98.47 % and I 2 = 99.41 %, respectively). Overall, results from examining the distribution of mean change in LES pressure between pre- and postoperation show that there is a significant improvement in LES pressure. However, a high level of heterogeneity in mean change from preoperation was observed across the studies (I 2 = 97.10 %). Heterogeneity was also still high when prospective and retrospective studies are considered separately in a subgroup analysis, where I 2 = 96.34 % and I 2 = 93.33 % are observed for prospective and retrospective studies, respectively. Similar to Eckardt score, pooling is not recommended due to high level of heterogeneity. Study-level mean change in LES pressure with the corresponding 95 % CI is provided in forest plots (Fig. 4).
Complications
The most frequently reported complications (Table 4) were mucosal perforation (n = 118), pneumothorax (n = 69), pneumoperitoneum (n = 221), pneumomediastinum (n = 58), subcutaneous emphysema (n = 131), pleural effusion (n = 132), and pneumonia (n = 103). Two studies reported no complications [55, 59]. Another two studies used CT to assess complications [56, 62].
All complications related to the procedure were managed conservatively using endoscopic clipping, suturing, or hemostasis interventions. Veress needle decompression was commonly used to treat pneumoperitoneum. The majority of pleural effusions and pneumothoraces resolved spontaneously. Only 7 pleural effusions and 3 pneumothoraces required thoracic drainage. One contained perforation of the EGJ required endoscopic drainage and laparoscopy failed to demonstrate the esophageal defect.
There was no mortality reported. None of the POEM procedures had to be converted to surgery. Three patients with persistent symptoms after POEM underwent LHM (n = 2) and pneumatic dilation (n = 1).
Only 4 studies evaluating 147 patients assessed GERD after POEM, using 24-h pH monitoring. The range of abnormal esophageal acid exposure varied from 20 to 53 %; all patients were symptomatically controlled with proton pump inhibitors (Table 4).
Discussion
Laparoscopic Heller myotomy is considered the standard of care for patients with achalasia. However, POEM appears to be a promising option in replacing LHM. Our systematic review identified 19 studies assessing the efficacy and safety of POEM including 10 retrospective and 9 prospective studies. There was no randomized control trial. Our analysis of the data revealed important findings: (1) POEM is effective in terms of reducing Eckardt scores and resting LES pressure in patients with achalasia. (2) High heterogeneity of data in reporting outcomes prevents a meta-analysis. (3) POEM appears to be safe in terms of low complication rates. (4) There is a lack of objective esophageal acid exposure assessment using 24-h pH monitoring.
POEM effectiveness and heterogeneity of data
The differences between preoperative and postoperative Eckardt score and LES pressure are highly significant for all the studies considered in our analysis. Two systematic reviews have analyzed the effectiveness of POEM in terms of subjective (Eckardt scores) and objective (LES resting pressure) outcomes through meta-analysis or “pooling” results [71, 72]. However, our study highlights the high level of statistical heterogeneity (I 2 = 90.24 % and I 2 = 97.10 % for Eckardt score and LES pressure, respectively), which technically prevented us from performing a meta-analysis.
Pooling of results comparing LHM versus POEM was also not possible due to a lack in reporting data (Table 3). Only one study [23] reported pre- and post-Eckardt scores, pre- and post-LES pressure, and postoperative objective pH measurement, comparing 37 POEM versus 64 LHM showing that patient symptoms and esophageal physiology were equally improved.
Safety of POEM
POEM is considered a very safe procedure due to the very low rate of serious complications. The rate of reported complications however varies significantly from 0 % to more than 30 % among reviews [71–73]. This variability is likely related to the variability in reporting complications. Furthermore, this new endoscopic procedure which shares more features of a surgical procedure rather than a classical endoscopic procedure results in a significant challenge and lack of consensus in defining what constitutes a complication. Many of the reported complications including pneumoperitoneum, pneumomediastinum, full-thickness myotomy, and mucosal perforation are common occurrences which are easily managed intraoperatively and are often of little to no clinical significance. In this setting, we found two factors that may play a role in variability of reporting complications. First, the utilization of CO2 instead of ambient air reduces the postoperative rate of complications since CO2 is more absorbable than ambient air. It is well known that during endoscopic submucosal dissection, longitudinal muscles can be exposed or split provoking air passage into the mediastinum. The use of a more absorbable gas for insufflation during the procedure may reduce the volume of the leakage. Cai et al. reported on their initial experience with room air in 157 POEM patients compared to their late series of 143 POEM patients for whom CO2 was available. The use of ambient air was associated with an increased rate of pneumothorax (p < 0.001) [45].
Secondly, routine CT scan can detect small amounts of CO2 post-POEM which may detect changes post-procedure, rather than clinical complications. Yang et al. evaluated 108 patients within 30 h after POEM (all with CO2 insufflation). Pneumoperitoneum and/or pneumomediastinum was detected in 53.7 % of patients. There was no statistically significant relationship between the presence of pneumoperitoneum and or pneumomediastinum detected on CT and the development of complications such as minor inflammation of lungs, pleural effusion, subcutaneous emphysema, segmental atelectasis of lungs, ascites or severe complications, including delayed hemorrhage, esophageal perforation, retroperitoneal abscess [74].
GERD after POEM
The incidence and severity of postoperative GERD following POEM remains an important issue. The results in this systematic review vary among the studies depending on the method utilized to evaluate reflux. Comparative pre- and post-POEM endoscopy showed an increased incidence of esophagitis from 0 to 19 % [38, 40, 60]. Although endoscopy provides excellent evidence for the diagnosis of GERD when esophagitis is present, this condition has been found in only 30 % of patients off acid suppression treatment and in an even smaller proportion when treated with PPI [75]. As conventional histology from random biopsies has poor performance for the diagnosis of GERD, ambulatory 24-h pH monitoring is the gold standard in the diagnosis of GERD [76].
Previous experience with Heller myotomy has shown that the postoperative incidence of reflux, measured with 24-h pH monitoring at 6 months was significantly higher without fundoplication (43 %) compared to the group with partial fundoplication (9 %) [77]. Gastroesophageal reflux after Heller myotomy with partial fundoplication has been found in about 25–35 % of patients and is usually well controlled with medical therapy [78]. Thus, partial fundoplication (Dor or Toupet) is commonly added to Heller myotomy to prevent high incidence of postoperative reflux. A multicenter, prospective, randomized-controlled trial showed no significant difference in the acid exposure of the distal esophagus among 60 patients who underwent Dor (36) or Toupet (24) fundoplications after Heller myotomy at 6–12 months. Abnormal acid reflux was present in 10 of 24 patients in the Dor group (41.7 %) and in 4 of 19 patients in the Toupet (21.0 %) (p < 0.152) [79]. Only a few studies in our review reported postoperative 24-h pH monitoring [52, 59, 65, 66]. The range of abnormal 24-h pH monitoring reported in these studies was 20–53 %, which is comparable to previous data on Heller myotomy alone. However, additional studies are needed to further address the question of postoperative reflux in patients undergoing POEM.
Limitations
Our study has several limitations. We aimed to include studies with more than 10 cases and to address pre- and post-op Eckardt scores and/or LES pressure, but that strategy excluded the few studies comparing LHM and POEM. In addition, the length of myotomy is not uniformly performed and reported. In our analysis, only 7 studies differentiated esophageal from gastric length, showing a large variation in gastric (1.1–7 cm), esophageal (3–13 cm), and total (2.6–26 cm) length (Table 3), making the data difficult to compare. Lastly, sigmoid esophagus and the presence of previous treatments may make POEM more challenging and data less comparable. In our analysis, fourteen studies reported the presence of sigmoid esophagus involving 99 patients treated with POEM.
Future research
The role of POEM in the treatment of achalasia should be defined comparing it with the standard of care. A meta-analysis of RCTs compared different treatment options for achalasia showing that pneumatic dilation has better remission rate and lower relapse rate than botulinum toxin injection (BTI) [9] and at least four RCTs including around 450 patients have compared pneumatic dilation versus LHM, showing better long-term outcomes for latest [12, 80–82]. Other meta-analyses have confirmed these results positioning LHM as the standard of care for the treatment of achalasia [8, 10, 11]. Thus, we consider that future research should be directed to compare POEM to LHM in a randomized fashion. Estimation of the number of patients and the appropriate power calculation should be made for future trials. Moreover, the design should consider long-term follow-up (5–10 years) as established with studies comparing PD versus LHM.
Based on our systematic review, we are unable to clearly identify the group of patients where POEM represents a better option than LHM. The main reasons are heterogeneity of the data and the lack of comparisons with LHM. Perhaps, in cases of failed surgical treatment for achalasia, POEM has the advantage of preventing mucosal perforations since it can be performed endoluminally in the posterior esophageal wall, avoiding the scar tissue of previous surgery, but more studies are needed to confirm this hypothesis.
Conclusion
POEM appears to be a promising, effective, and safe option for the treatment of achalasia. However, the high heterogeneity and lack of RCTs make current published data difficult to compare.
RCTs and long-term follow-up studies comparing POEM versus the standard of care (LHM) are needed to further establish the efficacy of POEM in the management of patients with achalasia. Esophageal physiology and symptoms improvement (particularly dysphagia) should be considered endpoints for future comparisons with LHM.
Research should aim to better define complications and standard postoperative changes related to the POEM procedure. In addition, the incidence of GERD following POEM should be studied with objective 24-h pH testing.
References
Farrukh A, DeCaestecker J, Mayberry JF (2008) An epidemiological study of achalasia among the South Asian population of Leicester, 1986–2005. Dysphagia 23:161–164
Sadowski DC, Ackah F, Jiang B, Svenson LW (2010) Achalasia: incidence, prevalence and survival. A population-based study. Neurogastroenterol. Motil 22:e256–e261
Willis T (1674) Pharmaceutic rationalis: sive diatriba de medicamentorum; operatimibus in humano corpore. Hagae-Comitis, London
Richter JE (2010) Achalasia—an update. J Neurogastroenterol Motil 16:232–242
Vaezi MF, Richter JE (1998) Current therapies for achalasia: comparison and efficacy. J Clin Gastroenterol 27:21–35
Pellegrini C, Wetter LA, Patti M, Leichter R, Mussan G, Mori T, Bernstein G, Way L (1992) Thoracoscopic esophagomyotomy. Initial experience with a new approach for the treatment of achalasia. Ann Surg 216:291–296 (discussion 296-299)
Oelschlager BK, Chang L, Pellegrini CA (2003) Improved outcome after extended gastric myotomy for achalasia. Archives of surgery 138:490–495 (discussion 495-497)
Campos GM, Vittinghoff E, Rabl C, Takata M, Gadenstatter M, Lin F, Ciovica R (2009) Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg 249:45–57
Wang L, Li YM, Li L (2009) Meta-analysis of randomized and controlled treatment trials for achalasia. Dig Dis Sci 54:2303–2311
Weber CE, Davis CS, Kramer HJ, Gibbs JT, Robles L, Fisichella PM (2012) Medium and long-term outcomes after pneumatic dilation or laparoscopic Heller myotomy for achalasia: a meta-analysis. Surg Laparosc Endosc Percutaneous Techn 22:289–296
Schoenberg MB, Marx S, Kersten JF, Rosch T, Belle S, Kahler G, Vassiliou MC, Luth S, von Renteln D (2013) Laparoscopic Heller myotomy versus endoscopic balloon dilatation for the treatment of achalasia: a network meta-analysis. Ann Surg 258:943–952
Persson J, Johnsson E, Kostic S, Lundell L, Smedh U (2015) Treatment of achalasia with laparoscopic myotomy or pneumatic dilatation: long-term results of a prospective, randomized study. World J Surg 39:713–720
Ortega JA, Madureri V, Perez L (1980) Endoscopic myotomy in the treatment of achalasia. Gastrointest Endosc 26:8–10
Pasricha PJ, Hawari R, Ahmed I, Chen J, Cotton PB, Hawes RH, Kalloo AN, Kantsevoy SV, Gostout CJ (2007) Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy 39:761–764
Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S (2010) Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 42:265–271
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1–34
Eckardt VFAC, Bernhard G (1992) ) Predictors of outcome in patients with achalasia treated by pneumatic dilatation. Gastroenterology 103:1732–1738
Inoue H, Kudo SE (2010) Peroral endoscopic myotomy (POEM) for 43 consecutive cases of esophageal achalasia. Nippon Rinsho Jpn J Clin Med 68:1749–1752
Gao ZQ, Huang ZG, Ren H (2014) Peroral endoscopic myotomy for treatment of esophageal achalasia: analysis of 12 cases. World Chin J Digestol (21):3100–3105
Ma RX, Zhang FX, Wang Y, Chen JY, Kang SC, Wang JW, Wang XF, Jia HM (2014) Peroral endoscopic myotomy for achalasia: Analysis of 58 cases. World Chin J Digestol (21):3095–3099
Ling T, Guo H, Zou X (2014) Effect of peroral endoscopic myotomy in achalasia patients with failure of prior pneumatic dilation: a prospective case-control study. J Gastroenterol Hepatol 29:1609–1613
Yang T, Zhang X, Ling T, Lu Y, Zou X (2014) Dynamic changes in esophageal manometry of achalasia patients receiving peroral endoscopic myotomy. Chin J Gastroenterol 19:288–290 (Chinese)
Bhayani NH, Kurian AA, Dunst CM, Sharata AM, Rieder E, Swanstrom LL (2014) A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with peroral endoscopic myotomy (POEM) for achalasia. Ann Surg 259:1098–1103
Cai MY, Zhou PH, Yao LQ, Xu MD, Zhong YS, Li QL, Chen WF, Hu JW, Cui Z, Zhu BQ (2014) Peroral endoscopic myotomy for idiopathic achalasia: randomized comparison of water-jet assisted versus conventional dissection technique. Surg Endosc 28:1158–1165
Teitelbaum EN, Soper NJ, Arafat FO, Santos BF, Kahrilas PJ, Pandolfino JE, Hungness ES (2014) Analysis of a learning curve and predictors of intraoperative difficulty for peroral esophageal myotomy (POEM). J Gastrointest Surg 18:92–98 (discussion 98-99)
Familiari P, Gigante G, Marchese M, Boskoski I, Bove V, Tringali A, Perri V, Onder G, Costamagna G (2014) EndoFLIP system for the intraoperative evaluation of peroral endoscopic myotomy. United Eur Gastroenterol J 2:77–83
von Rahden BH, Filser J, Reimer S, Inoue H, Germer CT (2014) Peroral endoscopic myotomy for treatment of achalasia. Literature review and own initial experience. Chirurg 85:420–432
Teitelbaum EN, Boris L, Arafat FO, Nicodeme F, Lin Z, Kahrilas PJ, Pandolfino JE, Soper NJ, Hungness ES (2013) Comparison of esophagogastric junction distensibility changes during POEM and Heller myotomy using intraoperative FLIP. Surg Endosc 27:4547–4555
Verlaan T, Rohof WO, Bredenoord AJ, Eberl S, Rosch T, Fockens P (2013) Effect of peroral endoscopic myotomy on esophagogastric junction physiology in patients with achalasia. Gastrointest Endosc 78:39–44
Sharata A, Kurian AA, Dunst CM, Bhayani NH, Reavis KM, Swanstrom LL (2013) Peroral endoscopic myotomy (POEM) is safe and effective in the setting of prior endoscopic intervention. J Gastrointest Surg 17:1188–1192
Kurian AA, Dunst CM, Sharata A, Bhayani NH, Reavis KM, Swanstrom LL (2013) Peroral endoscopic esophageal myotomy: defining the learning curve. Gastrointest Endosc 77:719–725
Hungness ES, Teitelbaum EN, Santos BF, Arafat FO, Pandolfino JE, Kahrilas PJ, Soper NJ (2013) Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy. J Gastrointest Surg 17:228–235
Zhou PH, Li QL, Yao LQ, Xu MD, Chen WF, Cai MY, Hu JW, Li L, Zhang YQ, Zhong YS, Ma LL, Qin WZ, Cui Z (2013) Peroral endoscopic remyotomy for failed Heller myotomy: a prospective single-center study. Endoscopy 45:161–166
Teitelbaum EN, Rajeswaran S, Zhang R, Sieberg RT, Miller FH, Soper NJ, Hungness ES (2013) Peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy produce a similar short-term anatomic and functional effect. Surgery 154:885–891 (discussion 891-882)
Minami H, Yamaguchi N, Matsushima K, Akazawa Y, Ohnita K, Takeshima F, Nakayama T, Hayashi T, Inoue H, Nakao K, Isomoto H (2013) Improvement of endocytoscopic findings after per oral endoscopic myotomy (POEM) in esophageal achalasia; does POEM reduce the risk of developing esophageal carcinoma? Per oral endoscopic myotomy, endocytoscopy and carcinogenesis. BMC Gastroenterol 13:22
Zhong YS, Li L, Zhou PH, Xu MD, Ren Z, Zhu BQ, Yao LQ (2012) Effects of peroral endoscopic myotomy on esophageal dynamics in patients with esophageal achalasia. Zhonghua Weichang Waike Zazhi 15:668–670
Ren Z, Zhong Y, Zhou P, Xu M, Cai M, Li L, Shi Q, Yao L (2012) Perioperative management and treatment for complications during and after peroral endoscopic myotomy (POEM) for esophageal achalasia (EA) (data from 119 cases). Surg Endosc 26:3267–3272
Swanstrom LL, Kurian A, Dunst CM, Sharata A, Bhayani N, Rieder E (2012) Long-term outcomes of an endoscopic myotomy for achalasia: the POEM procedure. Ann Surg 256:659–667
Costamagna G, Marchese M, Familiari P, Tringali A, Inoue H, Perri V (2012) Peroral endoscopic myotomy (POEM) for oesophageal achalasia: preliminary results in humans. Dig Liver Dis 44:827–832
von Renteln D, Inoue H, Minami H, Werner YB, Pace A, Kersten JF, Much CC, Schachschal G, Mann O, Keller J, Fuchs KH, Rosch T (2012) Peroral endoscopic myotomy for the treatment of achalasia: a prospective single center study. Am J Gastroenterol 107:411–417
Zhou PH, Cai MY, Yao LQ, Zhong YS, Ren Z, Xu MD, Chen WF, Qin XY (2011) Peroral endoscopic myotomy for esophageal achalasia: report of 42 cases. Zhonghua Weichang Waike Zazhi 14:705–708
Teitelbaum EN, Soper NJ, Pandolfino JE, Kahrilas PJ, Hirano I, Boris L, Nicodeme F, Lin Z, Hungness ES (2015) Esophagogastric junction distensibility measurements during Heller myotomy and POEM for achalasia predict postoperative symptomatic outcomes. Surg Endosc 29:522–528
Khashab MA, Messallam AA, Onimaru M, Teitelbaum EN, Ujiki MB, Gitelis ME, Modayil RJ, Hungness ES, Stavropoulos SN, El Zein MH, Shiwaku H, Kunda R, Repici A, Minami H, Chiu PW, Ponsky J, Kumbhari V, Saxena P, Maydeo AP, Inoue H (2015) International multicenter experience with peroral endoscopic myotomy for the treatment of spastic esophageal disorders refractory to medical therapy (with video). Gastrointestinal endoscopy 81:1170–1177
Hu JW, Li QL, Zhou PH, Yao LQ, Xu MD, Zhang YQ, Zhong YS, Chen WF, Ma LL, Qin WZ, Cai MY (2014) Peroral endoscopic myotomy for advanced achalasia with sigmoid-shaped esophagus: long-term outcomes from a prospective, single-center study. Surg Endosc 29:2841–2850
Cai MY, Zhou PH, Yao LQ, Zhu BQ, Liang L, Li QL (2014) Thoracic CT after peroral endoscopic myotomy for the treatment of achalasia. Gastrointest Endosc 80:1046–1055
Yang S, Zeng MS, Zhang ZY, Zhang HL, Liang L, Zhang XW (2014) Pneumomediastinum and pneumoperitoneum on computed tomography after peroral endoscopic myotomy (POEM): postoperative changes or complications? Acta Radiol 56:1216–1221
Teitelbaum EN, Soper NJ, Pandolfino JE, Kahrilas PJ, Boris L, Nicodeme F, Lin Z, Hungness ES (2014) An extended proximal esophageal myotomy is necessary to normalize EGJ distensibility during Heller myotomy for achalasia, but not POEM. Surg Endosc 28:2840–2847
Vigneswaran Y, Tanaka R, Gitelis M, Carbray J, Ujiki MB (2014) Quality of life assessment after peroral endoscopic myotomy. Surg Endosc 29:1198–1202
Orenstein SB, Raigani S, Wu YV, Pauli EM, Phillips MS, Ponsky JL, Marks JM (2014) Peroral endoscopic myotomy (POEM) leads to similar results in patients with and without prior endoscopic or surgical therapy. Surg Endosc 29:1064–1070
Liu XJ, Tan YY, Yang RQ, Liu DL (2014) Short-term outcomes and quality of life after peroal endoscopy myotomy for achalasia. World Chin J Digestol 22:5315–5320 (Chinese)
Dolezel R, Martinek J, Svecova H, Spicak J, Juhasova J (2014) The effect of learning peroral endoscopic myotomy (POEM) during the first year of authentication methods in the Czech Republic. [Czech] Efekt uceni peroralni endoskopicke myotomie (POEM) behem prvniho roku overovani metody v Ceske republice. Gastroenterol Hepatol 68:294–298
Martinek J, Svecova H, Spicak J, Krajciova J, Vackova Z, Pazdro A, Harustiak T, Kieslichova E, Janousek R, Dolezel R, Fremundova L (2014) POEM—new endoscopic method of oesophageal achalasia treatment peroralni endoskopicka myotomie (POEM)—Nova endoskopicka moznost lecby achalazie jicnu. Kardiol Rev 16:205–209
Ling TS, Guo HM, Yang T, Peng CY, Zou XP, Shi RH (2014) Effectiveness of peroral endoscopic myotomy in the treatment of achalasia: a pilot trial in Chinese Han population with a minimum of one-year follow-up. J Dig Dis 15:352–358
Minami H, Isomoto H, Yamaguchi N, Matsushima K, Akazawa Y, Ohnita K, Takeshima F, Inoue H, Nakao K (2014) Peroral endoscopic myotomy for esophageal achalasia: clinical impact of 28 cases. Dig Endosc 26:43–51
Ujiki MB, Yetasook AK, Zapf M, Linn JG, Carbray JM, Denham W (2013) Peroral endoscopic myotomy: A short-term comparison with the standard laparoscopic approach. Surgery 154:893–897 (discussion 897-900)
Onimaru M, Inoue H, Ikeda H, Yoshida A, Santi EG, Sato H, Ito H, Maselli R, Kudo SE (2013) Peroral endoscopic myotomy is a viable option for failed surgical esophagocardiomyotomy instead of redo surgical Heller myotomy: a single center prospective study. J Am Coll Surg 217:598–605
Li QL, Chen WF, Zhou PH, Yao LQ, Xu MD, Hu JW, Cai MY, Zhang YQ, Qin WZ, Ren Z (2013) Peroral endoscopic myotomy for the treatment of achalasia: a clinical comparative study of endoscopic full-thickness and circular muscle myotomy. J Am Coll Surg 217:442–451
Von Renteln D, Fuchs KH, Fockens P, Bauerfeind P, Vassiliou MC, Werner YB, Fried G, Breithaupt W, Heinrich H, Bredenoord AJ, Kersten JF, Verlaan T, Trevisonno M, Rosch T (2013) Peroral endoscopic myotomy for the treatment of achalasia: an international prospective multicenter study. Gastroenterology 145:309–11.e1–3
Chiu PW, Wu JC, Teoh AY, Chan Y, Wong SK, Liu SY, Yung MY, Lam CC, Sung JJ, Chan FK, Lau JY, Ng EK (2013) Peroral endoscopic myotomy for treatment of achalasia: from bench to bedside (with video). Gastrointest Endosc 77:29–38
Lee BH, Shim KY, Hong SJ, Bok GH, Cho JH, Lee TH, Cho JY (2013) Peroral endoscopic myotomy for treatment of achalasia: initial results of a korean study. Clin Endosc 46:161–167
Zhai Y, Linghu E, Li H, Qin Z, Wang X, Du H, Meng J (2013) Comparison of peroral endoscopic myotomy with transverse entry incision versus longitudinal entry incision for achalasia. Nan Fang Yi Ke Da Xue Xue Bao J South Med Univ 33:1399–1402
Inoue H, Ikeda H, Hosoya T, Yoshida A, Onimaru M, Minami H, Kudo SE (2012) Peroral endoscopic myotomy (POEM) for esophageal achalasia. Nippon Shokakibyo Gakkai Zasshi Jpn J Gastroenterol 109:728–731
Chen WF, Li QL, Zhou PH, Yao LQ, Xu MD, Zhang YQ, Zhong YS, Ma LL, Qin WZ, Hu JW, Cai MY, He MJ, Cui Z (2015) Long-term outcomes of peroral endoscopic myotomy for achalasia in pediatric patients: a prospective, single-center study. Gastrointest Endosc 81:91–100
Patel KS, Calixte R, Modayil RJ, Friedel D, Brathwaite CE, Stavropoulos SN (2015) The light at the end of the tunnel: a single-operator learning curve analysis for per oral endoscopic myotomy. Gastrointest Endosc 81:1181–1187
Teitelbaum EN, Soper NJ, Santos BF, Arafat FO, Pandolfino JE, Kahrilas PJ, Hirano I, Hungness ES (2014) Symptomatic and physiologic outcomes one year after peroral esophageal myotomy (POEM) for treatment of achalasia. Surg Endosc 28:3359–3365
Familiari P, Gigante G, Marchese M, Boskoski I, Tringali A, Perri V, Costamagna G (2014) Peroral endoscopic myotomy for esophageal achalasia: outcomes of the first 100 patients with short-term follow-up. Ann Surg 263:82–87
Wang J, Tan N, Xiao Y, Chen J, Chen B, Ma Z, Zhang D, Chen M, Cui Y (2014) Safety and efficacy of the modified peroral endoscopic myotomy with shorter myotomy for achalasia patients: a prospective study. Dis Esophagus 28:720–727
Chen X, Li QP, Ji GZ, Ge XX, Zhang XH, Zhao XY, Miao L (2014) Two-year follow-up for 45 patients with achalasia who underwent peroral endoscopic myotomy. Eur J Cardiothorac Surg 47:890–896
Sharata AM, Dunst CM, Pescarus R, Shlomovitz E, Wille AJ, Reavis KM, Swanstrom LL (2015) Peroral endoscopic myotomy (POEM) for esophageal primary motility disorders: analysis of 100 consecutive patients. J Gastrointest Surg 19:161–170
Tan YY, Liu DL, Zhang J, Li CJ, Duan TY, Zhou JF, Wang XH, Huo JR (2014) Peroral endoscopic myotomy for achalasia: a comparative study of simple longitudinal mucosal incision and modified incision. World Chin J Digestol 22:4129–4134 (Chinese)
Talukdar R, Inoue H, Reddy DN (2014) Efficacy of peroral endoscopic myotomy (POEM) in the treatment of achalasia: a systematic review and meta-analysis. Surg Endosc 29:3030–3046
Patel K, Abbassi-Ghadi N, Markar S, Kumar S, Jethwa P, Zaninotto G (2015) Peroral endoscopic myotomy for the treatment of esophageal achalasia: systematic review and pooled analysis. Dis Esophagus. doi:10.1111/dote.12387
Barbieri LA, Hassan C, Rosati R, Romario UF, Correale L, Repici A (2015) Systematic review and meta-analysis: efficacy and safety of POEM for achalasia. United Eur Gastroenterol J 3:325–334
Yang S, Zeng MS, Zhang ZY, Zhang HL, Liang L, Zhang XW (2015) Pneumomediastinum and pneumoperitoneum on computed tomography after peroral endoscopic myotomy (POEM): postoperative changes or complications? Acta Radiol 56:1216–1221
Lind T, Havelund T, Carlsson R, Anker-Hansen O, Glise H, Hernqvist H, Junghard O, Lauritsen K, Lundell L, Pedersen SA, Stubberod A (1997) Heartburn without oesophagitis: efficacy of omeprazole therapy and features determining therapeutic response. Scand J Gastroenterol 32:974–979
Pandolfino JE, Vela MF (2009) Esophageal-reflux monitoring. Gastrointest Endosc 69:917–30–930.e1
Richards WO, Torquati A, Holzman MD, Khaitan L, Byrne D, Lutfi R, Sharp KW (2004) Heller myotomy versus Heller myotomy with Dor fundoplication for achalasia: a prospective randomized double-blind clinical trial. Ann Surg 240:405–412 (discussion 412-405)
Stefanidis D, Richardson W, Farrell TM, Kohn GP, Augenstein V, Fanelli RD (2012) SAGES guidelines for the surgical treatment of esophageal achalasia. Surg Endosc 26:296–311
Rawlings A, Soper NJ, Oelschlager B, Swanstrom L, Matthews BD, Pellegrini C, Pierce RA, Pryor A, Martin V, Frisella MM, Cassera M, Brunt LM (2012) Laparoscopic Dor versus Toupet fundoplication following Heller myotomy for achalasia: results of a multicenter, prospective, randomized-controlled trial. Surg Endosc 26:18–26
Novais PA, Lemme EM (2010) 24-h pH monitoring patterns and clinical response after achalasia treatment with pneumatic dilation or laparoscopic Heller myotomy. Aliment Pharmacol Ther 32:1257–1265
Kostic S, Kjellin A, Ruth M, Lonroth H, Johnsson E, Andersson M, Lundell L (2007) Pneumatic dilatation or laparoscopic cardiomyotomy in the management of newly diagnosed idiopathic achalasia. Results of a randomized controlled trial. World J Surg 31:470–478
Boeckxstaens GE, Annese V, des Varannes SB, Chaussade S, Costantini M, Cuttitta A, Elizalde JI, Fumagalli U, Gaudric M, Rohof WO, Smout AJ, Tack J, Zwinderman AH, Zaninotto G, Busch OR, European Achalasia Trial I (2011) Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med 364:1807–1816
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Oscar M. Crespin, Louis W.C. Liu, Ambica Parmar, Timothy D. Jackson, Jemila Hamid, Eran Shlomovitz, and Allan Okrainec have no conflicts of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Crespin, O.M., Liu, L.W.C., Parmar, A. et al. Safety and efficacy of POEM for treatment of achalasia: a systematic review of the literature. Surg Endosc 31, 2187–2201 (2017). https://doi.org/10.1007/s00464-016-5217-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5217-y