Abstract
Background
Utilization of bariatric surgery has changed dramatically over the past two decades. The aim of this study was to update the trends in volume and procedural type of bariatric surgery in the USA. Data were derived from the National Inpatient Sample from 2009 through 2012.
Methods
We used ICD-9 diagnosis and procedural codes to identify all hospitalizations during which a bariatric procedure was performed for the treatment of severe obesity. The data were reviewed for patient demographics and characteristics, annual number of bariatric operations, and specific procedural types and proportion of laparoscopic cases. The US Census data were used to calculate the population-based annual rate of bariatric surgery per 100,000 adults.
Results
Between 2009 and 2012, the number of inpatient bariatric operations ranged between 81,005 and 114,780 cases annually. During this time period, the annual rate of bariatric procedures was highest for 2012 at 47.3 procedures per 100,000 adults. The bariatric surgery approach most commonly performed continues to be laparoscopic, ranging between 93.1 and 97.1 %. In 2012, there was a precipitous reduction in the number of gastric bypass and gastric banding operations and replaced by an increase in the number of sleeve gastrectomy operation. The in-hospital mortality rate remains low, ranging from 0.07 to 0.10 %.
Conclusions
In the USA, the annual volume of inpatient bariatric surgery continues to be stable. Utilization of the laparoscopic approach to bariatric surgery remains high, while the in-hospital mortality continues to be low at ≤0.10 % throughout the 4-year period.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Surgery continues to be the only long-term effective weight loss option for patients suffering from severe obesity. Over the past two decades, the field of bariatric surgery has changed dramatically. Prior to the development of the laparoscopic approach to bariatric surgery, the number of bariatric operations performed in the USA was reported as 9189 procedures in 1993, increasing modestly to 12,541 procedures in 1997 [1]. With the advent of the laparoscopic gastric bypass operation, the number of bariatric operations increased substantially to 70,256 procedures in 2002 [2]. The volume of bariatric surgery in the USA then peaked at 135,985 procedures in 2004 and stabilized at 124,838 procedures in 2008 [3]. While the number of bariatric operations increased, there was a precipitous reduction in the mortality rate associated with bariatric surgery. In 1998, the in-hospital mortality associated with bariatric surgery was high at 0.8 % [3]. A decade later in 2008, the in-hospital mortality associated with bariatric surgery was substantially reduced at 0.1 % [3, 4]. By 2005, the number of laparoscopic gastric bypass operations exceeded that of the open gastric bypass operations [3]. We previously reported in detail on trends in the use of bariatric surgery between 2003 and 2008 [3]. Using administrative data from the National Inpatient Sample (NIS), the aim of the current study was to examine and update the trends in utilization of volume and procedural type of bariatric surgery for the treatment of severe obesity during the ensuing four-year period, 2009–2012.
Methods
Discharge data from the NIS between 2009 and 2012 were obtained from the Healthcare Cost and Utilization Project (HCUP), sponsored by the Agency for Healthcare Research and Quality. The NIS is the largest all-payer inpatient care database in the USA, containing data on almost 8 million hospital stays from about 1000 hospitals. This sample represents approximately 20 % of US community hospitals. To produce national estimates, we used weight discharges in the NIS core files to the discharges from all US community as instructed by the NIS methodology. The NIS includes public hospitals and academic medical centers. We obtained information from the NIS database concerning the annual total number of bariatric operations; the proportion of Roux-en-Y gastric bypass, gastric banding, sleeve gastrectomy, and gastroplasty; the proportion of laparoscopic cases; patient characteristics (age, gender, and race) and comorbidities; and postoperative outcomes including median length of stay and in-hospital mortality. Approval for the use of the HCUP patient data was obtained from the HCUP.
Using the HCUP database, we analyzed all discharge abstract data for patients who underwent bariatric surgery during the time period from January 1, 2009 through December 31, 2012. All hospitalizations during which a bariatric procedure was performed for the treatment of severe obesity were identified using appropriate diagnosis and procedure codes as specified by the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM). The principal ICD-9 diagnosis codes for obesity and morbid obesity were 278.0, 278.01, 278.00, 278.8, and 278.1, which included a subcategory of obesity and a subclassification of morbid obesity. The principal ICD-9 procedure codes for open Roux-en-Y gastric bypass were 44.31 and 44.39, which included a subcategory of gastroenterostomy without gastrectomy and a subclassification of high gastric bypass. The principal ICD-9 procedure code for laparoscopic Roux-en-Y gastric bypass was 44.38, which included a subcategory of gastroenterostomy without gastrectomy and a subclassification of laparoscopic gastroenterostomy. The principal ICD-9 procedure code for laparoscopic adjustable gastric banding was 44.95. The principal ICD-9 procedure code for gastroplasty was 44.69 and for laparoscopic sleeve gastrectomy was 43.82. We calculated the population-based rates of bariatric surgery per 100,000 adults for each year using the number of bariatric surgical procedures obtained from the NIS database and the US Census estimates of the adult population (age > 17 years) as the denominator.
Results
Volume and rates of bariatric surgery
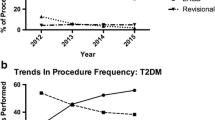
From 2009 through 2012, a total of 397,585 patients underwent bariatric surgery for the treatment of severe obesity in the USA. The volume of bariatric surgery was lowest for 2011 at 81,005 procedures and highest in 2012 at 114,780 procedures (Table 1). The type of bariatric procedure between 2009 and 2011 consisted mainly of Roux-en-Y gastric bypass (71–75 % of all bariatric procedures). However, the proportion of Roux-en-Y gastric bypass precipitously decreased to 53 % in 2012, while the proportion of laparoscopic sleeve gastrectomy increased to 42 %. Figure 1 depicts the continued growth in adoption of the laparoscopic approach to bariatric surgery in the USA. The proportion of laparoscopic bariatric operations was at an all-time high of 97.1 % in 2012. The annual rate of bariatric surgery was lowest at 32.1 procedures per 100,000 adults in 2011 and highest at 47.3 procedures in 2012 (Fig. 2).
Patient characteristics and outcomes
Between 2009 and 2012, the median age of patients who underwent bariatric surgery ranged from 44 to 45 years, with 78–79 % being female. The proportion of Caucasians ranged from 60 to 65 %. The prevalence of preoperative comorbidities is listed in Table 1. The prevalence of diabetes ranged between 33 and 35 %; hypertension ranged between 57 and 59 %; dyslipidemia ranged between 24 and 28 %; chronic liver disease ranged between 9 and 12 %; and sleep apnea ranged between 11 and 15 %. The median length of stay was 2 days. The in-hospital mortality was low, ranging from 0.10 % in 2010 to 0.07 % in 2012 (Table 1).
Discussion
Using the NIS administrative database, we found stabilization in the volume of bariatric surgery being performed in the USA since 2004. In this study, the population-based rate of bariatric surgery was lowest in 2011 at 32.1 procedures and highest in 2012 at 47.3 procedures. The proportion of laparoscopic bariatric operations continued to be very high, ranging between 93 and 97 % of cases. However, the type of bariatric operation has changed dramatically, starting in 2012. Gastric bypass operations decreased to only 53 % of cases accompanied by a precipitous reduction in gastric banding volume to 5 % of cases, while the sleeve gastrectomy procedure increased substantially to 43 % of cases.
The growth of bariatric surgery peaked in 2004 but has since plateaued. Recently, a dramatic change is being observed in the procedure type of bariatric operation in that sleeve gastrectomy is gaining popularity as a stand-alone bariatric procedure. Using a database from academic centers, we previously reported a change in the makeup of bariatric surgery with an increase in the use of laparoscopic sleeve gastrectomy, which has had an impact primarily on reducing the use of laparoscopic adjustable gastric banding [5]. In that study of academic centers, 36 % of all bariatric cases were laparoscopic sleeve gastrectomy cases in 2012, which is only a slightly lower rate than our data of 43 % of sleeve gastrectomy obtained from community hospitals within the NIS. [5] In the state of Michigan, Reams et al. [6] similarly reported an increase in the use of sleeve gastrectomy, which became the most common bariatric procedure, surpassing gastric bypass in 2012. It is likely that this trend will continue with sleeve gastrectomy becoming the most common bariatric operation in the USA. Despite this change in the makeup of bariatric surgery, the quality and safety of bariatric surgery nationwide continues to be excellent. The in-hospital mortality for bariatric surgery in the current study ranged from 0.07 to 0.10 % between 2009 and 2012.
There are several limitations to this study. The specific type of gastroplasty procedure is unclear based on the ICD-9 code for gastroplasty. The gastroplasty procedures performed between 1998 and 2002 are presumed to be mostly vertical banded gastroplasty, while the gastroplasty procedures performed between 2003 and 2011 are presumed to be laparoscopic sleeve gastrectomy. The specific ICD-9 procedural code for laparoscopic sleeve gastrectomy only first became available in October 2011. Although laparoscopic gastric banding was first approved by the Food and Drug Administration in 2001, the ICD-9 procedural code for laparoscopic adjustable gastric banding only became available in October of 2004; therefore, the proportion of laparoscopic gastric banding is likely underestimated prior to 2004. Similarly, the specific ICD-9 procedural code for laparoscopic gastric bypass also first became available in October 2004; therefore, the proportion of laparoscopic bariatric operations is likely underestimated prior to 2004. The NIS only contains data for inpatient admissions and therefore does not report outpatient procedures. Gastric banding procedures are commonly performed in an outpatient setting and are not captured within the NIS. Therefore, the decline in the number of gastric banding procedures may represent a true national decline or a transition from inpatient to outpatient gastric banding procedures or both. The NIS database is also compiled from discharge abstract data and is limited to in-hospital mortality without follow-up data. Therefore, deaths arising after discharge would not be captured in the NIS database. Our reported in-hospital mortality rate probably underestimates the “true” 30-day mortality. Despite these limitations, this study provides an update on the national trends in utilization of bariatric surgery, and characterizes the contemporary growth of sleeve gastrectomy, which has impacted the volume of gastric bypass and gastric banding.
In conclusion, the annual rates of bariatric surgery in the USA remain plateaued at 32.1–47.3 procedures per 100,000 adults between the years 2009 and 2012. The percentage of the laparoscopic approach to bariatric surgery remains high at 93–97 % of cases. The major findings from this study were the precipitous drop in the volume of gastric banding, and a modest reduction in the volume of gastric bypass cases that was countered by a substantial increase in the volume of sleeve gastrectomy cases.
References
Pope GD, Birkmeyer JD, Finlayson SR (2002) National trends in utilization and in-hospital outcomes of bariatric surgery. J Gastrointest Surg 6:855–861
Nguyen NT, Root J, Zainabadi K et al (2005) Accelerated growth of bariatric surgery with the introduction of minimally invasive surgery. Arch Surg 140:1198–1202
Nguyen NT, Masoomi H, Magno CP, Nguyen XT et al (2011) Trends in use of bariatric surgery, 2003-2008. J Am Coll Surg 213:261–266
Morton JM, Garg T, Nguyen NT (2014) Does hospital accreditation impact bariatric surgery safety? Ann Surg 260:504–508
Nguyen NT, Nguyen BM, Gebhart A, Hohmann S (2013) Changes in the makeup of bariatric surgery: a national increase in use of laparoscopic sleeve gastrectomy. J Am Coll Surg 216:252–257
Reames BN, Finks JS, Bacal D, Carlin AM, Dimick JB (2014) Changes in bariatric surgery procedure use in Michigan, 2006–2013. JAMA 312:959–961
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Drs. Ninh T. Nguyen, Natalia Bodunova, and Michael J. Phelan have no conflicts of interest or financial ties to disclose. Stephen Vu and Eric Kim have no conflicts of interest or financial ties to disclose.
Additional information
The information contained in this article was based on the National Inpatient Sample database, sponsored by the Agency for Healthcare Research and Quality.
Rights and permissions
About this article
Cite this article
Nguyen, N.T., Vu, S., Kim, E. et al. Trends in utilization of bariatric surgery, 2009–2012. Surg Endosc 30, 2723–2727 (2016). https://doi.org/10.1007/s00464-015-4535-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4535-9