Abstract
Background
Endoscopic stapler diverticulotomy (ESD) has become an accepted primary treatment for Zenker’s diverticulum (ZD). Recurrence of symptoms after surgical treatment of ZD is not uncommon, and traditionally patients with recurrent symptomatic ZD were referred to revision surgery by the transcervical Zenker’s diverticulectomy approach. Our objective was to evaluate the technical feasibility, safety and effectiveness of revision endoscopic stapler diverticulotomy (RESD) for recurrent ZD.
Methods
A case series with chart review study conducted in a tertiary referral center. The records of all patients who underwent ESD at our institute between 2002 and 2013 were retrieved and those who underwent RESD were identified and screened for primary surgical history, symptoms of recurrent ZD, time to recurrence, intraoperative and postoperative RESD course, complications and symptom resolution. The surgical history and outcome results of RESD and primary ESD (PESD) patients were compared.
Results
Eighty-nine ESDs were performed. Twenty were RESDs for recurrent ZD, and 69 were PESDs. Nine RESDs were performed for recurrent ZD after transcervical Zenker’s diverticulectomy, 10 RESDs for recurrent ZD after ESD, and one initial surgical approach was unknown. The mean time from first operation for ZD to RESD was 4.7 years. The average RESD surgery time and hospital stay were 21.4 min and 2.8 days, respectively. Endoscopic stapling of the ZD was feasible in 19 of 20 RESDs. Relief of symptoms without recurrence was achieved after 18 RESDs. Four RESD patients experienced minor postoperative complications. There were no significant differences in operative time, technical feasibility, hospital stay and complication rate between the RESD and PESD groups (P > .05).
Conclusion
RESD for ZD is technically feasible, safe and effective. The results are comparable to those of PESD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hypopharyngeal (Zenker’s) diverticulum is an esophageal pouch presenting posterolateral to the pharynx just above the level of the upper esophageal sphincter. First described in 1769 by Ludlow [1], this disorder was characterized more accurately by Zenker and Ziemssen in 1877 [2]. Traditionally, the ZD was either excised using a transcervical approach (diverticulectomy) or treated with transcervical diverticulopexy. The transcervical approaches were eventually substituted by an endoscopic approach (diverticulotomy), first described by Mosher in 1917 [3]. In 1993, Collard et al. [4] introduced the endoscopic stapling technique using an endosurgical stapler that simultaneously divides the wall between the esophagus and the pouch and then staples the wound’s edges closed. Its advantages over the standard transcervical diverticulectomy, as reported in many series [5, 6], include a shorter operative time, hospital stay and interval between surgery and oral intake, as well as a lower rate of complications, lower morbidity and mortality rates, and decreased costs [7, 8].
The risk of ZD recurrence after treatment has been reported as being between 0 and 16 % [9–12]. Recurrent ZD may be treated either by transcervical Zenker’s diverticulectomy or by RESD. Traditionally, patients with recurrent symptomatic ZD after RESD or after RESD surgical failure were referred to transcervical Zenker’s diverticulectomy surgery. Reports on RESD after PESD or after transcervical Zenker’s diverticulectomy are sparse, and its efficacy and safety in the treatment of RESD have not yet been determined. In this study, we present our experience in performing RESD. We sought to evaluate the technical feasibility, safety and effectiveness of RESD for recurrent ZD and compare these findings with those we achieved for PESD.
Materials and methods
The study was approved by the Institutional Review Board of Tel-Aviv Sourasky Medical Center, a tertiary referral center. The medical records of all the patients with ZD treated by ESD at our institute between 2002 and 2013 were reviewed retrospectively. The database included demographic variables, preoperative symptoms, time to RESD from initial surgery for ZD, operative time, length of hospital stay, and complications and recurrence rates. We defined recurrence as partial or complete return of symptoms that justified revision ESD at any point in time after ESD or transcervical Zenker’s diverticulectomy for ZD.
Our preoperative protocol is to administer intravenous second-generation cephalosporin and dexamethasone. All procedures are conducted with the patient under general anesthesia and with a microlaryngeal endotracheal tube in place. A Weerda® laryngoscope (Karl Storz, Tuttlingen, Germany) is inserted into the hypopharynx. The inferior blade of the Weerda® laryngoscope is introduced into the lumen of the diverticulum, and the superior blade of the Weerda® laryngoscope is inserted into the esophagus. A 5-mm 0° endoscope is then inserted alongside an EndoGIA 35-mm endoscopic stapler (Ethicon Inc., Somerville, NJ, USA) through the Weerda® laryngoscope into the esophagus. The EndoGIA 35-mm endoscopic stapler blades are then applied to the dividing wall between the esophagus and diverticulum, one above and one below the wall, under endoscopic vision. The stapler is then engaged on the wall and fired, dividing the common wall between the esophagus and the diverticulum. One or two applications of the stapler are performed until the common wall is completely divided. The operative field is inspected for bleeding, and the Weerda laryngoscope is removed. After completion of the procedure, the patient is transferred to the surgical ward and remains with no food or drink per-os until the next morning. A chest X-ray is obtained on the day after surgery to rule out free air or widening of the mediastinum. If the chest X-ray is confirmed as being intact, the patient is then allowed a soft diet. The patients are kept hospitalized 2–3 days postoperatively monitoring vital signs, pain and amount of oral intake to confirm full oral intake without signs of complications. Patients are seen in the outpatient clinic 1 week after hospital discharge and assessed for improvement in their dysphagia, complications and satisfaction. Follow-up evaluations are then continued in our outpatient clinic at variable intervals according to the clinical course and relief of symptoms.
The results were collected and entered into a Microsoft Excel® sheet. The two-tailed Fisher exact test was used to generate p values. Results yielding p values <.05 were considered statistically significant.
Results
A total of 89 ESDs were performed in our department from January 2002 to December 2013. Twenty were RESDs for recurrent ZD, and 69 were PESDs. Nine RESDs were performed for recurrent ZD after transcervical Zenker’s diverticulectomy, ten ESRDs for recurrent ZD after ESD (eight had undergone PESDs in our institute), and one initial surgical approach was unknown. We did not encounter patients with recurrent ZD after flexible endoscopic laser-assisted diverticulotomy or after transcervical diverticulopexy in our series. One patient underwent RESD twice, thus resulting in 20 RESDs having been performed for 19 patients. The mean time from PESD to RESD was 4.7 years. The male-to-female ratio in the RESD group and in the PESD group was 4.75:1 and 1.7:1, respectively (P = .02). The mean age at RESD and at PESD was 66.1 and 60.1 years, respectively (P > .05).
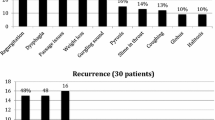
Presenting symptoms included dysphagia, food regurgitation, weight loss, coughing, globus sensation, recurrent pneumonia and reduced compliance with medical treatment because of inability to swallow tablets and capsules. All the patients were proven to have ZD by a preoperative barium esophagogram.
During esophagoscopy, an intact wall between the ZD and esophagus was noted in most the cases of RESD. Rarely, staples on the partitioning wall or scarring of the wall were noted. Stapling of the ZD was technically feasible in 19 of 20 RESDs (95 %) and in 65 of 69 PESDs (94.2 %) (P > .05). Between 1 and 2 stapler applications were used to divide the parting wall (mean 1.8). The ZD was not identified endoscopically, and the procedure was aborted in 1 patient who underwent RESD. This patient had undergone a previous ESD attempt in another medical center, which failed due to the same difficulty. She later underwent transcervical Zenker’s diverticulectomy, which was complicated by esophageal perforation and vocal fold paresis. In the PESD group, ESD was aborted after esophagoscopy in four patients due to inadequate exposure of the common wall or inability to apply the stapling device safely because of severe micrognathia in two cases and severe osteoarthrosis of the neck in two cases. The average RESD and PESD operative time was 21.4 and 23.6 min, respectively (P > .05), and the average hospital stay time was 2.8 and 3.3 days, respectively (P > .05, Table 1). The median hospitalization time was 2 days in both groups.
ZD recurred in 1 of 19 (5.3 %) RESD cases and in 8 of 69 (11.6 %) PESD cases (P = .02). Relief of symptoms without recurrence was achieved in 18 RESD cases. One patient underwent RESD twice (after a primary transcervical Zenker’s diverticulotomy) before resolution of symptoms was achieved. Notably, a 94.5 % success rate could be expected when RESD was technically feasible.
We compared the characteristics of PESD patients who had recurrence to those who did not (Table 2). The mean ages were 51.7 and 66.6 years, respectively (P < .05), the mean operative time was 27 and 23 min, respectively (P > .05), and the mean hospitalization time was 2.1 and 3.5 days, respectively (P < .05). The median hospitalization time in both groups was 2 days.
Four patients in the RESD group (20 %) experienced minor postoperative complications, including palatal laceration and stomatitis, delirium, fever and rash. Ten patients in the PESD group (14.4 %) had minor complications, including dental damage (n = 3), oropharyngeal mucosal erosions (n = 2), subcutaneous emphysema in the upper cervical region which resolved without sequelae (n = 2), bradycardia (n = 1), aspiration and fever (n = 1), and diarrhea (n = 1). Four patients (5.7 %) in the PESD group had major complications. One patient experienced esophageal perforation and pneumomediastinum, which was treated conservatively (parenteral nutrition and antibiotics). One developed global dysphagia after discharge and was diagnosed with severe esophageal edema in another medical center where a gastrostomy was performed. The gastrostomy was removed after resolution of esophageal edema. One patient had perforation of the ZD during the esophagoscopy, which was stapled endoscopically. One patient experienced unilateral paramedian vocal fold paralysis. We suspect the vocal fold paralysis was caused by pressure of the Weerda laryngoscope on branches of the recurrent laryngeal nerve in the lateral postcricoid area.
Discussion
The surgical management of ZD has evolved considerably over the past 2 decades, with growing interest and experience in managing Zenker’s diverticulum endoscopically. Recurrence of symptoms after surgical treatment of ZD is not uncommon [9–11]. Traditionally, patients with recurrent symptomatic ZD, either after PESD or after transcervical diverticulectomy, were referred to revision surgery by the transcervical approach. Reports on RESD after PESD or after transcervical Zenker’s diverticulectomy are sparse, and its efficacy and safety in the treatment of recurrent ZD have not yet been determined. Kaoy et al. [13] reported their experience with 3 RESD cases, Scher et al. [14] studied 18 RESD cases, and Adam et al. [12] reported 4 RESD cases. Our study goal was to evaluate the technical feasibility, safety and effectiveness of RESD for recurrent ZD and compare these findings with those we had achieved for PESD.
We defined recurrence as partial or complete return of symptoms that justifies revision surgery for ZD at any point in time after a prior ESD or transcervical Zenker’s diverticulectomy. The mean reported recurrence rate is estimated as 5 % (range 0–19 %) for the external approaches and 6 % (range 0–22 %) for ESD. Our recurrence rate after PESD (11.6 %) is therefore comparable to that reported in the literature, while our recurrence rate after RESD was significantly lower (5.3 vs. 11.6 %, P = .02). A comparison of patients who experienced ZD recurrence to those who did not revealed that patients who had recurrence were younger and had shorter average hospitalization time at PESD (Table 2). We do not know why young age was a risk factor for recurrence. We speculate that the higher recurrence rate in this subgroup may be partially associated, as was our experience when operating on younger patients with ZD, with a technically more difficult esophagoscopy, positioning of the Weerda laryngoscope and ZD visualization due to higher neck muscle bulk and tone. Another possible mechanism may be a higher tendency for scar formation and more rapid healing of the dividing wall between the ZD and esophagus in younger patients. The shorter hospitalization time may be contributed to their younger age, better general health and fewer co-morbidities.
Information on past experience with RESD after PESD or after transcervical Zenker’s diverticulectomy is limited, and reports of its outcome compared to that of PESD are conflicting. Scher [14] studied 18 RESDs and noted that the outcome of RESD was similar to that of PESD. In the most recently published report, Adam et al. [12] evaluated 12 revision endoscopic Zenker’s diverticulotomies (4 RESD and 8 laser revisions) and found that the length of hospital stay and time to oral intake in the RESD group were significantly longer than in the group of PESD. In contrast to their findings, we found no significant differences between the RESD and PESD groups in terms of age, operative time, technical feasibility, hospital stay and complication rate (Table 1).
Conclusion
Our results for RESD were comparable to those for PESD in terms of patient’s age, operative time, technical feasibility, hospital stay and complication rate. We found that younger patients and patients with longer average PESD hospitalization time were at greater risk of recurrence. We therefore conclude that RESD for ZD is technically feasible, safe and effective and that it should be the treatment of choice for recurrent symptomatic ZD after PESD or transcervical Zenker’s diverticulectomy.
References
Ryland A (1921) Some contemporary notes of a case of pharyngeal pouch—first reported 1764. Epidiascopic demonstration. Proc R Soc Med 14(Laryngol Sect):47–48
Ferguson B (1991) Evolution of therapy for pharyngoesophageal (Zenker’s) diverticulum. Ann Thorac Surg 51:848–852
Mosher HP (1917) Webs and pouches of the esophagus: their diagnosis and treatment. Surg Gynecol Obstet 25:175–187
Collard JM, Otte JB, Kestens PJ (1993) Endoscopic stapling technique of esophagodiverticulostomy for Zenker’s diverticulum. Ann Thorac Surg 56:573–576
Scher RL, Richtsmeier WJ (1998) Long-term experience with endoscopic staple-assisted esophagodiverticulostomy for Zenker’s diverticulum. Laryngoscope 108:200–205
Omote K, Feussner H, Stein HJ, Ungeheuer A, Siewert JR (1999) Endoscopic stapling diverticulostomy for Zenker’s diverticulum. Surg Endosc 13:535–538
Smith SR, Genden EM, Urken ML (2002) Endoscopic stapling technique for the treatment of Zenker diverticulum vs standard open-neck technique: a direct comparison and charge analysis. Arch Otolaryngol Head Neck Surg 128:141–144
Chang CY, Payyapilli RJ, Scher RL (2003) Endoscopic staple diverticulostomy for Zenker’s diverticulum: review of literature and experience in 159 consecutive cases. Laryngoscope 113:957–965
Cook RD, Huang PC, Richstmeier WJ, Scher RL (2000) Endoscopic staple-assisted esophagodiverticulostomy: an excellent treatment of choice for Zenker’s diverticulum. Laryngoscope 110:2020–2025
Peracchia A, Bonavina L, Narne S, Segalin A, Antoniazzi L, Marotta G (1998) Minimally invasive surgery for Zenker diverticulum: analysis of results in 95 consecutive patients. Arch Surg 133:695–700
Narne S, Narne S, Cutrone C, Bonavina L, Chella B, Peracchia A (1999) Endoscopic diverticulotomy for the treatment of Zenker’s diverticulum: results in 102 patients with staple-assisted endoscopy. Ann Otol Rhinol Laryngol 108:810–815
Adam SI, Paskhover B, Sasaki CT (2013) Revision Zenker diverticulum: laser versus stapler outcomes following initial endoscopic failure. Ann Otol Rhinol Laryngol 122:247–253
Kaoy CB, Commins D, Bates GJ (1998) The role of endoscopic stapling diverticulotomy in recurrent pharyngeal pouch. J Laryngol Otol 112:954–955
Scher R (2003) Endoscopic staple diverticulostomy for recurrent Zenker’s diverticulum. Laryngoscope 113:63–67
Acknowledgments
Esther Eshkol is thanked for editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Yael Oestreicher-Kedem, Oshri Wasserzug, Boaz Sagi, Narin Nard Carmel and Daniel Zikk have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Oestreicher-Kedem, Y., Wasserzug, O., Sagi, B. et al. Revision endoscopic stapler Zenker’s diverticulotomy. Surg Endosc 30, 2022–2025 (2016). https://doi.org/10.1007/s00464-015-4435-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4435-z