Abstract
Background
The incidence of bile duct injuries (BDI) after cholecystectomy, which is a life-threatening condition that has several medical and legal implications, currently stands at about 0.6 %. The aim of this study is to describe our experience as the first center to use a laparoscopic approach for BDI repair.
Methods
A prospective study between June 2012 and September 2014 was developed. Twenty-nine consecutive patients with BDI secondary to cholecystectomy were included. Demographics, comorbidities, presenting symptoms, details of index surgery, type of lesion, preoperative and postoperative diagnostic work-up, and therapeutic interventions were registered. Videos and details of laparoscopic hepaticojejunostomy (LHJ) were recorded. Injuries were staged using Strasberg classification. A side-to-side anastomosis with Roux-en-Y reconstruction was always used. In patients with E4 and some E3 injuries, a segment 4b or 5 section was done to build a wide anastomosis. In E4 injuries, a neo-confluence was performed. Complications, mortality, and long-term evolution were recorded.
Results
Twenty-nine patients with BDI were operated. Women represented 82.7 % of the cases. The median age was 42 years (range 21–74). Injuries at or above the confluence occurred in 62 %, and primary repair at our institution was performed at 93.1 % of the cases. Eight neo-confluences were performed in all E4 injuries (27.5 %). The median operative time was 240 min (range 120–585) and bleeding 200 mL (range 50–1100). Oral intake was started in the first 48 h. Bile leak occurred in 5 cases (17.2 %). Two patients required re-intervention (6.8 %). No mortality was recorded. The maximum follow-up was 36 months (range 2–36). One patient with E4 injury developed a hepaticojejunostomy (HJ) stenosis after 15 months. This was solved with endoscopic dilatation.
Conclusions
The benefits of minimally invasive approaches in BDI seem to be feasible and safe, even when this is a complex and catastrophic scenario.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The incidence of bile duct injuries (BDI) after laparoscopic cholecystectomy currently stands at about 0.6 %. Biliary injuries produced during laparoscopic cholecystectomy have proved to be more severe and complex. Such a complex pathology is best managed with a multidisciplinary approach involving surgeons, interventional radiologists, and endoscopists [1].
A side-to-side Roux-en-Y hepaticojejunostomy (RYHJ) is the best surgical alternative in patients with complete section of the common bile duct. Even in centers with experience at repairing BDI, complete rehabilitation is accomplished in 75–98 % of patients [2].
Up to now, laparoscopic reconstruction after BDI is limited to case reports. Nevertheless, laparoscopic biliodigestive derivations for the treatment of other biliary and pancreatic pathologies have proved to be safe and feasible [3–7].
The aim of this study is to describe our experience as the first center in Mexico to use a minimally invasive approach for BDI repair.
Materials and methods
Between June 2012 and September 2014, 29 patients with BDI secondary to cholecystectomy were treated at our hospital. Three of the injuries were inflicted at our center; the other 26 were referred from other institutions. Information regarding the demographics of patients, comorbidities, presenting symptoms, details of cholecystectomy, type of injury, preoperative and postoperative diagnostic work-up, therapeutic interventions, and details of LHJ were recorded prospectively, with prior approval of the local Committee for Human Investigation.
All patients were evaluated, and their conditions were optimized by a multidisciplinary team including nutritionists, infectologists, endoscopists, and anesthesiologists. Antibiotic therapy was indicated as needed. All patients were studied preoperatively with tri-phasic computed tomography (CT) for abscess, collections, and vascular injury assessment. When available, cholangiomagnetic resonance imaging (CMRI) was done. Classification of the injury was made according to Strasberg [8].
Either if the injury was or not identified at the primary surgery, once the initial work-up at our hospital was finished, all patients were admitted to the operating room to make a diagnostic laparoscopy. According to the operative findings and general conditions of the patient, in some cases we performed primary LHJ. In others, we drained bile collections and 3 months later made an interval RYHJ. These procedures were termed “early” when they were made within 6 weeks of injury or “delayed” when done later.
Surgical technique
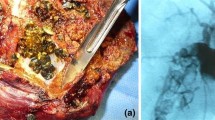
In all cases, we used four ports: an umbilical (optical) and left paramedian subcostal 12-mm trocars, a subxiphoid and right subcostal 5-mm trocars (Fig. 1). After diagnostic laparoscopy, bile collections were drained and dissection of all intraabdominal adhesions was made. Afterward, the inferior surface of the liver and porta hepatis was exposed. We systematically made an intraoperative cholangiogram in order to identify all segments of the intrahepatic biliary tree (Fig. 2). To assess basal microscopic liver status, hepatic biopsies were always taken. Proliferation of bile ducts at portal tract margins, periductal fibrosis, and active periportal fibroplasia was reported in two of our patients.
We advocate the use of tension-free Hepp-Couinaud-like side-to-side anastomosis with an ante-colic Roux-en-Y reconstruction. For adequate length and exposure of the bile duct in E1 and E2 injuries, the common hepatic duct was incised longitudinally on its anterior surface and extended to the left hepatic duct or both the left and the right hepatic ducts [9] (Fig. 3). In cases where the common hepatic duct had been devascularized during cholecystectomy, it was resected up to healthy bleeding tissue level and then incised as described.
For E3 injuries, the extrahepatic portion of the left hepatic duct was identified and a longitudinal ductotomy was performed in order to expose the confluence and part of the right duct.
Patients with E3, E4 and C injuries needed first a partial section of segment 4b and/or 5, in order to adequately expose the ducts. Their anterior aspect was opened to increase the surface to construct a wide side-to side anastomoses [9, 10]. The left duct and the right ducts were identified using the technique previously described by Strasberg [11]. For E4 injuries, we built a neo-confluence, that is, a surgical approximation of separated right and left hepatic ducts in order to perform a single HJ [2].
To build the anastomosis, laparoscope magnification and high-definition monitors were used. According to the caliber of the ducts, anastomoses between the jejunal limb and the previously dissected bile ducts were constructed with 3-0, 4-0, or 5-0 monofilament absorbable sutures with interrupted stitches and extracorporeal sliding knots.
Stenosis of the HJ is described as late complication in 13–24 % of the patients [2, 12]. In order to gain future access to the HJ, we created an enteropexy of the blind segment of the jejunal biliary limb beneath the subxiphoid incision port (access loop), as other authors have previously described [13, 14]. Percutaneous endoscopic rehabilitation of the strictured HJ could be performed through this limb with endoscopic techniques when needed.
Transhepatic stents were never used. A closed suction drain was placed routinely. Postoperative outcome, immediate and late complications as well as mortality were recorded and classified according to Strasberg [15]. Long-term evolution was followed through a standardized clinic appointments schedule at 15 days, 1, 3, 6, and 12 months, and 1 year after the procedure thereafter. Cholangitis or cholestasis was ruled out through clinical assessment and biochemical analysis. Yearly CMRI was performed to assess the anastomosis or before when biochemical or clinical evidence of cholestasis was found (Fig. 4).
Statistical analysis
Variables are summarized using median, minimum, maximum values, and percentages.
Results
In a 2-year period, 29 patients with BDI were treated at our institution. Forty-one percent of our patients had a BDI which occurred at primary open cholecystectomy, 55.1 % at a laparoscopic approach, and one patient at a converted procedure. Twenty-six patients (89.6 %) were referred to our service from an outside institution. Twenty-four (82.7 %) of them were women. The median age of our patients was 42 years (range 21–74). Table 1 shows the characteristics and demographics of patients with BDI reconstructed with LHJ.
Diagnosis and management of BDI
The diagnostic approach of all our patients is summarized in Table 2. The median time between cholecystectomy and diagnosis of BDI was 2 days (range 0–1095). In fifteen patients, the injury was recognized postoperatively. Presenting symptoms included jaundice, abdominal pain, fever, chills, and abdominal distension.
Endoscopic retrograde cholangiopancreatography (ERCP) was performed at the referral hospital in 13 patients (44.8 %).
Even though seven of our patients had right hepatic artery injury demonstrated at initial CT scan, none of them showed hepatic ischemic necrosis associated after at least 72 h from cholecystectomy.
Median time from BDI to LHJ was 11 days (range 0–1104). Only 13.7 % of our patients (n = 4) had a late bile duct reconstruction, performed more than 6 weeks after the BDI. Interval LHJ was performed in one case.
Injury classifications are presented in Table 1. Injuries at or above the confluence occurred in 18 patients (62.06 %). Twenty-seven (93.1 %) patients had a primary repair at our institution. Of the two remaining patients, one of them had a choledocho-choledochostomy. The other one had an end-to-side HJ. Both of them needed a secondary reconstruction due to anastomosis stricture, since they were no candidates to endoscopic of radiological rehabilitation. Secondary repair was performed from 5 months to more than 2 years after a primary repair was done elsewhere. One of these patients had formed intrahepatic gallstones, which were extracted during secondary repair through a simultaneous laparoendoscopic approach.
Table 3 shows the characteristics of our LHJ. Neo-confluences together with section of segment 4b were performed in all patients with E4 injuries (n = 8). In the remaining 21 patients, a side-to-side Hepp-Couinaud-like anastomosis was built as described earlier. One conversion was done because severe swelling of mesentery made impossible to mobilize a jejunal limb in order to create a tension-free HJ.
One or more perioperative complications occurred in nine patients as described in Table 4. No mortality was reported in this series.
Regarding the complications and their treatment, one of the patients developed a pneumothorax produced by a central venous catheter placement, and this was solved with a pleurostomy tube.
Of the five cases of bile leak, four of them were solved without intervention as outpatients in the first 10 days after LHJ. The presence of bile leak had no impact on the decision to start oral intake or discharge.
We performed two re-interventions in the immediate postoperative period: One because of a bile collection which was formed due to bile leak and dysfunction of the closed suction drain placed during surgery. In this case, we made a laparoscopic drainage of the bile accumulated and left a new drain. The patient had an adequate evolution during postoperative period. He started oral intake 1 day after re-intervention and was discharged 4 days later. The second case of re-intervention was performed because of intestinal obstruction due to a Petersen’s hernia. We performed a diagnostic laparoscopy. The mesentery gap was closed and afterward the patient had a satisfactory evolution.
Late complications occurred in one patient who developed stenosis of the anastomosis after 15 months of LHJ. This patient was asymptomatic but her follow-up laboratories suggested cholestasis and a CMRI showed HJ stricture. We performed an HJ endoscopic dilatation, through the access jejunal loop beneath the subxiphoid port. After 8 months of the endoscopic procedure, she remains asymptomatic and with normal liver function tests.
The maximum follow-up in our study was 36 months (range 7–36). Until now, one patient has been lost to follow-up.
Discussion
Various authors have stated that the technical aspects of repair are essential for early and long-term success of BDI reconstruction, namely well-vascularized ducts, no tension, biliary epithelium-to-mucosa anastomosis with largest possible diameter and complete drainage of all hepatic segments [2, 9]. All of these aspects can be achieved with a laparoscopic approach. Even more, there is no need to use magnification loupes due to the inherent magnification and high-definition images offered by laparoscopes.
Other series report that secondary repair is the most frequent type of reconstruction that they perform [1, 2]. In contrast, only two of our patients (6.8 %) had a prior BDR. We advocate a quick referral to our institution without prior attempts of reconstruction, either if the lesion was diagnosed during cholecystectomy or later. Most of our patients were referred in a short time after cholecystectomy. In four cases, we were called transoperatively or in the first 48 h after BDI, to perform the LHJ. We believe that this is part of the factors related to the good outcomes we have achieved.
As Hepp-Couinaud first described, a side-to-side biliary-enteric anastomosis makes unnecessary an extensive and potentially devascularizing dissection of the common bile duct [16]. Thereafter, Strasberg and Mercado have proved that this approach is ideal for E3 injuries, but can also be used for E1 and E2 injuries as well as the right side component of E4 and C injuries [2, 9]. Achieving a widely patent anastomosis is easier when the anastomotic opening in the bile duct is not limited by bile duct diameter. Creating a high anastomosis also allows access to a portion of the biliary tree well vascularized and not directly exposed to inflammatory environment of the injury [17]. We believe that following these principles with a laparoscopic approach must have similar results plus the well-known and proven benefits of minimally invasive surgery in multiple gastrointestinal pathologies such as a reduction in: intraoperative blood loss, intensity of postoperative pain [18], duration of postoperative ileus, postoperative hospital stay [18, 19], cardiac [20] and respiratory complications [20, 21], and even better quality of life [18].
The use of transanastomotic stents is controversial. Some authors place these stents as a way to lower the intraductal pressure and obtain adequate flow through the anastomosis. Nevertheless, since there is a tendency to create the anastomosis at the hilar level, no transanastomotic stents are needed [2]. Even more, they can cause pressure necrosis on the duct, promote scar formation, or cause arteriobiliary fistula formation [22, 23].
The reported rate of strictures ranges from 2.2 to 35.2 % [9, 24], finding the lowest stricture rates in series where the side-to-side approach was used [9]. Since this is the technique of reconstruction we use, we expect similar outcomes.
Our team has formal training in gastrointestinal endoscopy, and this allows us to perform laparoscopic and endoscopic simultaneous approaches. For instance, when intrahepatic stones need to be retrieved during LHJ or when endoscopic rehabilitation of strictured HJ is needed. With these hybrid procedures we can overcome the limitations that each technique have separately.
Up to now, laparoscopic reconstruction after BDI is limited to case reports [25, 26]. Nevertheless, laparoscopic biliodigestive derivations for the treatment of benign and malignant biliary pathologies have proved to be safe and feasible [3–6, 27]. Amongst these biliodigestive derivations, the largest series with longest follow-up are RYHJ for the treatment of choledochal cysts in children [28–30] and adults [31]. To our knowledge, this paper is the largest published series of patients with BDI reconstructed through a laparoscopic approach.
We have attempted when possible, to have constant communication with the referring surgeon in order to obtain all the information about the cholecystectomy, and to avoid misunderstandings, managing a healthier doctor–patient relationship. Therefore, we have been able to avoid legal medical claims so far.
Conclusions
The present study demonstrates that a laparoscopic approach to BDI repair is feasible and safe. Although our series has a maximum follow-up of 36 months, we believe that the results will be equally satisfying in a long-term basis since we are using the same principles that have already proved successful, plus the well-demonstrated benefits of laparoscopic surgery.
The minimally invasive treatment of complex biliary pathologies requires advanced laparoscopic and endoscopic skills, as well as experience in bilioenteric reconstructions. Even though this is our initial report, the results seem to be promising.
Further studies with larger number of cases and longer follow-up are needed to establish the role of minimally invasive approaches in the reconstruction of BDI.
References
De Santibañes E, Palavecino M, Ardiles V, Pekolj J (2006) Bile duct injuries: management of late complications. Surg Endosc 20:1648–1653
Mercado MA, Franssen B, Domínguez I, Arriola-Cabrera JC, Ramírez-del Val F, Elnecavé-Olaiz A, Arámburo-Garcia R, García A (2011) Transition from a low-to a high-volume centre bile duct repair: changes in technique and improved outcome. HPB 13:767–773
Liu Y, Yao X, Li S, Liu W, Liu L, Liu J (2014) Comparison of therapeutic effects of laparoscopic and open operation for congenital choledochal cysts in adults. Gastroenterol Res Pract. doi:10.1155/2014/670260
Ng JL, Salim MT, Low Y (2014) Mid-term outcomes of laparoscopic versus open choledochal cyst excision in a tertiary paediatric hospital. Ann Acad Med Singapore 43:220–224
Aguirre-Olmedo I, Cuendis-Velázquez A, Morales-Chávez CE, Torres-Ruiz MF, Rojano-Rodríguez ME, Cárdenas-Lailson LE (2013) Laparoscopic choledochoduodenostomy as an optional treatment choledocholithiasis. Cir Cir 81:118–124
Chander J, Mangla V, Vindal A, Lal P, Ramteke VK (2012) Laparoscopic choledochoduodenostomy for biliary stone disease: a single-center 10-year experience. J Laparoendosc Adv Surg Tech A. doi:10.1089/lap.2011.0366
Kondratiuk OP, Khil’ko IuO, Kondratiuk VA, Kravchenko DA (2014) Laparoscopic hepaticojejunostomy in patients with inoperable tumour of pancreatic head. Klin Khir 4:64–65
Strasberg SM, Hertl M, Soper NJ (1995) An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg 180:101–125
Winslow ER, Fialkowski EA, Linehan DC, Hawkins WG, Picus DD, Strasberg SM (2009) “Sideways”: result of repair of biliary injuries using a policy of side-to-side hepatico-jejunostomy. Ann Surg 249:426–434
Mercado MA, Orozco H, de la Garza L, Lopez-Martinez LM, Contreras A, Guillen-Navarro E (1999) Biliary duct injury: partial segment IV resection for intrahepatic reconstruction of biliary lesions. Arch Surg 134:1008–1010
Strasberg SM, Picus DD, Ja Drebin (2001) Results of a new strategy for reconstruction of biliary injuries having an isolated right-sided component. J Gastrointest Surg 5:266–274
Holte K, Bardram L, Wettergren A, Rasmussen A (2010) Reconstruction of major bile duct injuries after laparoscopic cholecystectomy. Dan Med Bull 57:A4135
Al-Ghnaniem R, Benjamin IS (2002) Long-term outcome of hepaticojejunostomy with routine access loop formation following iatrogenic bile duct injury. Br J Surg 89:1118–1124
Jayasundara JA, de Silva WM, Pathirana AA (2011) Changing clinical profile, management strategies and outcome of patients with biliary tract injuries at a tertiary care center in Sri Lanka. Hepatobiliary Pancreat Dis Int 10:526–532
Strasberg SM, Linehan DC, Hawkins WG (2009) The accordion severity grading system of surgical complications. Ann Surg. doi:10.1097/SLA.0b013e3181afde41
Hepp J, Couinaud C (1956) Approach to and use of the left hepatic duct in reparation of the common bile duct. Presse Med 64:947–948
Mercado MA, Chan C, Orozco H, Tielve M, Hinojosa CA (2003) Acute bile duct injury. The need for a high repair. Surg Endosc 17:1351–1355
Schwenk W, Hasse O, Neudecker J, Müller JM (2005) Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev 20:CD003145
Zhang Y, Chen XM, Sun DL (2014) Laparoscopic versus open distal pancreatectomy: a single-institution comparative study. World J Surg Oncol. doi:10.1186/1477-7819-12-327
Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA (2014) Meta-analysis of laparoscopic vs open cholecystectomy in elderly patients. W J Gastroenterol 20:17626–17634
Bablekos GD, Michaelides SA, Analitis A, Charalabopoulos KA (2014) Effects of laparoscopic cholecystectomy on lung function: a systematic review. World J Gastroenterol. doi:10.3748/wjg.v20.i46.17603
Mercado MA, Chan C, Orozco H, Cano-Gutiérrez G, Chaparro JM, Galindo E, Vilatobá M, Samaniego-Arvizu G (2002) To stent or not to stent bilioenteric anastomosis after iatrogenic injury: a dilemma not answered? Arch Surg 137:60–63
Tocchi A, Costa G, Lepre L, Liotta G, Mazzoni G, Sita A (1996) The long-term outcome of hepaticojejunostomy in the treatment of benign bile duct strictures. Ann Surg 224:162–167
Stewart L, Way L (1995) Bile duct injuries during laparoscopic cholecystectomy. Arch Surg 130:1123–1129
Palermo M, Trelles N, Gagner M (2011) Laparoscopic revisional hepaticojejunostomy for biliary stricture after open repair following common bile duct injury: a case report. Surg Innov. doi:10.1177/1553350610395033
Prasad A, De S, Mishra P, Tiwari A (2015) Robotic assisted Roux-en-Y hepaticojejunostomy in a post-cholecystectomy type E2 bile duct injury. World J Gastroenterol 21:1703–1706
Toumi Z, Aljarabah M, Ammori BJ (2011) Role of the laparoscopic approach to biliary bypass for benign and malignant biliary diseases: a systematic review. Surg Endosc 25:2105–2116
Liem NT (2013) Laparoscopic surgery for choledochal cysts. J Hepatobiliary Pancreat Sci 20:487–491
Lee JH, Kim SH, Kim HY, Choi YH, Jung SE, Park KW (2013) Early experience of laparoscopic choledochal cyst excision in children. J Korean Surg Soc 85:225–229
Liem NT, Pham HD, le Dung A, Son TN, Vu HM (2012) Early and intermediate outcomes of laparoscopic surgery for choledochal cysts with 400 patients. Laparoendosc Adv Surg Tech A 22:599–603
Duan X, Mao X, Jiang B, Wu J (2014) Totally laparoscopic cyst excision and Roux-en-Y hepaticojejunostomy for choledochal cyst in adults: a single-institute experience of 5 years. Surg Laparosc Endosc Percutan Tech 00:001–004
Acknowledgments
We thank Dr. Florencio de la Concha Bermejillo, who helped in the edition of this paper, as well as all the referring surgeons who trusted our team for the treatment of their patients.
Disclosures
Drs. Adolfo Cuendis-Velázquez, Carlos Morales-Chávez, Itzé Aguirre-Olmedo, Fernanda Torres-Ruiz, Martín Rojano-Rodríguez, Luis Fernández-Álvarez, Eduardo Cárdenas-Lailson, and Mucio Moreno-Portillo have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cuendis-Velázquez, A., Morales-Chávez, C., Aguirre-Olmedo, I. et al. Laparoscopic hepaticojejunostomy after bile duct injury. Surg Endosc 30, 876–882 (2016). https://doi.org/10.1007/s00464-015-4282-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4282-y