Abstract
Background
Establishing and sustaining the routine practice of laparoscopy in resource-limited settings is extremely challenging. We present our experience implementing laparoscopic surgery at the Obafemi Awolowo University Teaching Hospital in Western Nigeria and the associated modifications that were necessary for success.
Methods
We reviewed all laparoscopic cases performed at our institution from January 2009 through December 2011. Operating surgeons were trained locally. Laparoscopic equipment and instrumentation was procured by both local and foreign sources.
Results
One hundred eighty-one procedures were performed in 175 patients whose ages ranged between 18 and 72 years. The procedures included cholecystectomies (n = 48, 24.5 %), appendectomies (n = 36, 20 %), diagnostic laparoscopies for staging and biopsy of intra-abdominal masses (n = 53, 30.9 %), adhesiolyses (n = 18, 11.6 %), hernia repairs (n = 6, 3.2 %), colorectal surgeries (n = 2, 1.3 %), and others (n = 18, 8.4 %). Diagnostic procedures were performed as day cases. Duration of stay for hospital admissions was 1–3 days. There were four conversions to open operation due to technical difficulties with equipment. No deaths were recorded. Local adaptation techniques facilitated cost reduction. Overall, there was improvement in the acceptance of the laparoscopic procedures among our patients and coworkers.
Conclusion
Our local institution has successfully adopted laparoscopic techniques to treat surgical diseases. Specific improvisations have helped establish and sustain this technology. We advocate similar local adaptations to increase the use of laparoscopic surgery in hospitals located in limited resource settings.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Since the introduction of laparoscopic surgery in general surgery practice, it has been gaining ground on open traditional surgery in many centers in advanced countries. It is attractive because it is minimally invasive and so is associated with much reduced postoperative pain and surgical site infection and with a shorter hospital stay [1]. However, laparoscopic surgery and other forms of minimally invasive surgery are not routinely found in developing countries such as Nigeria, not even in most public tertiary health-care services, possibly because of limited access to and the high cost of initial setup, technological support, and specialized training [2].
Minimally invasive surgery (MIS) would confer particular advantages if used for the diseases encountered at facilities such as ours. For instance, the high rate postoperative surgical site infections in developing countries could be reduced significantly by MIS. Laparoscopic surgery is a good adjunct to basic radiological investigations in the absence of modern imaging techniques for patients with intra-abdominal conditions [3, 4].
Our hospital is in a semiurban location that serves a largely agrarian population. When we attempted routine laparoscopy in our general surgical practice in 2008, we were unable to sustain it largely because of resource and facility limitations [5]. From 2009 on, we implemented various local adaptations and improvisations that enabled us to sustain use of laparoscopy and reduce its cost. This article describes our experience with laparoscopy in a general surgery unit with a view to highlighting how such modifications could improve acceptance and use of the service.
Methodology
Setting
This was a descriptive study of the initiation of and improvement in the laparoscopic services introduced in one of the two general surgery units of the Ife Hospital Unit, Obafemi Awolowo University Teaching Hospitals Complex, Ile-Ife, Osun State, Southwestern Nigeria. The hospital serves a semiurban, largely agrarian population with referrals commonly from adjoining states.
Facilities and setups
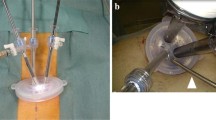
At inception, the setup consisted of a regular television that served as a monitor along with a light source, which also provided manual carbon dioxide insufflations. A few diagnostic procedures were carried out with this setup. Gradual upgrade was made possible thereafter with the addition of a digital insufflator with quadromanometric parameter monitoring and a xenon cold lamp light source, followed by a flat screen television (Fig. 1). The first few procedures were performed with a few disposable hand instruments, which were leftovers from a laparoscopic surgery mission from abroad. Reusable instruments were then acquired, some of which are still in use, lasting over 3 years.
To routinely document procedures to maintain patient information and teach surgical residents, students, and nurses, a USB/TV card was interfaced between the camera data processor and a laptop computer. This allowed direct recording to the computer while the screen of the laptop was an additional monitor that the assistant surgeon and/or nurses could view.
Spectrum of procedures
Initially, the rudimentary setup permitted only diagnostic and staging procedures. However, this progressed to performing therapeutic procedures with improvement in the setup and with greater confidence of the team; the nurses in particular became more familiar with the setup. On discharge, the total bill incurred by the patient was documented.
Results
One hundred eighty-one laparoscopic procedures were performed in the index period on 175 patients, ranging in age from 18 to 72 years. There were 120 (68.6 %) females and 55 (31.4 %) males. The procedures included 48 (24.5 %) cholecystectomies, 36 (20.0 %) appendectomies, 53 (30.9 %) diagnostic laparoscopies for staging and biopsy of intra-abdominal masses, 18 (11.6 %) adhesiolyses, 2 (1.3 %) colorectal surgeries, 6 (3.2 %) hernia repairs, and 18 (8.4 %) other miscellaneous operations such as laparoscopic retrieval of an intrauterine device that had perforated the uterus and orchidectomy in an adult with testicular feminization syndrome among others (Table 1). The overwhelming majority of laparoscopic cases were performed by one attending surgeon. There were a few procedures performed by senior residents under his supervision near the end of the review period. Operating time ranged from 24 to 116 min; there was a marked reduction in operating time as the team became more familiar with the setup and acquired more experience. All diagnostic procedures were performed as day cases. The length of hospital stay ranged from 1 to 3 days for therapeutic procedures.
Equipment failure and technical difficulties led to conversion to an open procedure on four occasions. On two occasions there was loss of view of the operating field due to a faulty cable that could not be immediately resolved by the technical staff. Excessive intraoperative bleeding led to the other two conversions. Postoperatively, superficial port site infection was observed in 11 (6.1 %) patients. Six of these patients had periappendiceal abscesses while two had gallbladder empyema. Wound infection was more common in contaminated and dirty wound categories as shown in Table 2. No deaths were recorded. The total cost of admission and the procedure ranged from 15,000 to 45,000 Nigerian naira (approximately 95–285 USD).
Discussion
At the March 2012 Meeting of the Society of American Gastrointestinal Endoscopic Surgeons (SAGES) in San Diego, California, an innovative session was introduced in which panelists were encouraged to share their experiences performing laparoscopic surgery in resource-poor settings. While the appropriateness of introducing laparoscopy in resource-poor settings continues to be debated, an increasing number of practitioners are beginning to see its value. Many of the benefits of laparoscopic surgery, such as a lower rate of surgical site infections and an earlier return to work and daily activities, produce greater benefits when the patient happens be the only laborer and bread winner for a large family. This tends to be the case in most poor communities and is aptly proposed in the statement “It is more important for a poor person to have laparoscopic surgery than a rich person.”Footnote 1
From our experience in Nigeria, we know that the affluent can seek immediate attention in a private hospital or travel abroad for treatment, but the roadside trader with little money and no health insurance can only compete for space on congested surgical wards at the public hospital. Traditionally, congestion on these wards is worsened by a combination of open surgery and attending infection. Laparoscopic surgery directly addresses the overcrowding of overburdened hospitals by reducing postoperative wound complications and the length of stay. Considering the lack of advanced radiologic modalities such as CT and MRI, laparoscopy also serves as a reliable diagnostic tool for intra-abdominal pathology.
Perhaps the greatest challenge to the practice of laparoscopy and minimal access surgery in developing economies is the attempt to replicate the exact operating room setting that is standard in Western countries. Almost always, the gap in development on the streets is equally reflected in the operating theatres. In many instances, this dynamic is rooted in experiences with international surgical missions from Western countries. These surgical trips are often outfitted with all that is required for highly specialized surgery during their stay without consideration for the sustainability of services by local practitioners. We believe that visits from international teams should be used only to assist the local surgeons in identifying areas for skill acquisition and equipment or procedure modification and adaptations that would enhance local capacity. In many instances, this may necessitate a gradual process over a period of time. In our hospital, after exhausting the donated materials, we could not perform laparoscopy for a while before the period of this study. We observed that many surgeons who faced a similar situation usually resorted to different local adaptations to aid their practice [3, 6].
Another major factor affecting sustainability is cost. In the absence of a well-functioning health insurance scheme, the majority of these patients have to bear the direct cost of laparoscopic surgery. This is one of the main reasons why until recently laparoscopic surgery has been offered in only a few private hospitals in Nigeria. The success of the pioneers of laparoscopic surgery in India pointed out that cost reduction measures will ultimately determine the outcome of efforts to deliver laparoscopy in resource-limited settings [7, 8]. In our experience, we were able to adopt some cost-reducing adaptations. We invested in reusable hand instruments, the majority of which have lasted over 3 years, thereby distributing the initial cost of purchase over the 175 patients. To avoid the use of disposable camera covers for each case, we made tube drapes that can be washed and autoclaved for each case. We also limited the use of other consumables such as retrieval bags in appendectomies to those patients with a markedly inflamed or purulent specimen. Less inflamed appendices were ligated to avoid spillage, dragged into a 10 mm port, and extracted. Similarly, we performed extracorporeal suture ligation of the base of the appendix in most instances and of the cystic duct on a few occasions in order to reduce the cost of surgery. We routinely use reloadable clips with the reusable clip applicator, which adds to operation time but avoids using costly disposable preloaded clip applicators [9]. We have also found that clips along with the diathermy are generally adequate for dissections and hemostasis in the absence of more advanced energy sources such as the harmonic scalpel.
In our hospital, the cost of a laparoscopic procedure ranges from 15,000 to 20,000 Nigerian naira (approximately 95–125 USD) for diagnostic procedures and from 30,000 to 45,000 Nigerian naira (approximately 190–285 USD) for therapeutic procedures. Even though the cost is much higher than what Dr. Udwadia and associates achieved in India [7], in terms of cost reduction we have pioneered and we remain in the vanguard of the efforts of affordable laparoscopic services to a large number of patients in our setting. Lowering the cost of the service has led to an increased patient turnover which is aiding the training of our junior colleagues and nurses in laparoscopic techniques. We look forward to the future when we hope to be better equipped for performing more advanced procedures.
The outcomes of our procedures are comparable to those in similar developing world settings [10, 11]. Laparoscopy has significantly reduced the postoperative hospital stay of patients in our setting as compared to that of our open surgeries thereby reducing the congestion on our surgical wards and ultimately allowing us to treat more patients. Our routine use of laparoscopy for evaluation of patients with suspected intra-abdominal malignancies has also reduced the morbidity and mortality that commonly follows diagnostic laparotomies for such patients. Finally, we have not had any perioperative deaths during our initial laparoscopic experience.
Conclusion
We believe that the only way forward for surgery in low-resource settings is to incorporate minimally invasive surgery. This goal can be facilitated by adopting local adaptations that enhance affordability and training of the local staff.
Notes
Proposed by Dr. Paul A. Severson, MD, FACS, Founder and President, Project Haiti Inc.
References
Nguyen NT, Goldman C, Rosenquist CJ, Arango A, Coles CJ, Lee SJ, Wolfe BM (2001) Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life and costs. Ann Surg 234(3):279–291
Adisa AO, Lawal OO, Alatise OI, Adesunkanmi AR (2011) An audit of laparoscopic surgeries in Ile-Ife, Nigeria. West Afr J Med 30:273–276
Straub CM, Price RR, Matthews D, Handrahan DL, Sergelen D (2011) Expanding laparoscopic cholecystectomy to rural Mongolia. World J Surg 35:751–759
Wichmann MW, Lang R, Beukes E, Esufali ST, Jauch KW, Hüttl TK, Hüttl TP (2010) Laparoscopic cholecystectomy—comparison of early postoperative results in an Australian rural center and a German University Hospital. Langenbecks Arch Surg 395:255–260
Adisa AO, Arowolo OA, Salako AA, Lawal OO (2009) Preliminary experience with laparoscopic surgery in Ile-Ife, Nigeria. Afr J Med Med Sci 38:351–356
Gnanaraj J (2010) Diagnostic laparoscopies in rural areas: a different use for the cystoscope. Trop Doct 40:156
Udwadia TE (2004) Diagnostic laparoscopy: a 30 year review. Surg Endosc 18:6–10
Udwadia TE (2007) Navigating laparoscopic surgery into the next decade in developing countries: a personal perspective. Langenbecks Arch Surg 392:99–104
Adisa AO, Lawal OO, Arowolo OA, Akinola DO (2011) Laparoscopic cholecystectomy in Ile-Ife, Nigeria. Afr J Med Med Sci 40:221–224
Udwadia TE, Patil SU, Udwadia RT, Bhandarkar DS (1992) Laparoscopic cholecystectomy in India. Int Surg 77(3):149–153
Esposito C, Alicchio F, Giurin I, Perricone F, Ascione G, Settimi A (2009) Lessons learned from the first 109 laparoscopic cholecystectomies performed in a single pediatric surgery center. World J Surg 33:1842–1845
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR (1999) Guideline for prevention of surgical site infection. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 20:250–280
Acknowledgments
The authors acknowledge the kind assistance of Dr. Thomas McIntyre in revising this manuscript.
Disclosures
A. O. Adisa, O. O. Lawal, O. A. Arowolo, and O. I. Alatise have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
An oral presentation of the abstract of this article was made at the 2012 SAGES conference in San Diego, CA, 7–10 March 2012.
Rights and permissions
About this article
Cite this article
Adisa, A.O., Lawal, O.O., Arowolo, O.A. et al. Local adaptations aid establishment of laparoscopic surgery in a semiurban Nigerian hospital. Surg Endosc 27, 390–393 (2013). https://doi.org/10.1007/s00464-012-2463-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2463-5