Abstract
Background
Transanal local excision (LE) is a well-established treatment option for early rectal neoplasms not amenable to complete colonoscopic removal. Endoscopic submucosal dissection (ESD) has been introduced recently as a novel procedure that enables en bloc resection of large rectal neoplasms. To date, no report comparing the two approaches can be found in the literature. This study aimed to compare the short-term clinical outcomes between ESD and LE for early rectal neoplasms.
Methods
Between 2007 and 2010, 14 patients with early rectal neoplasms deemed not feasible for en bloc endoscopic resection using conventional techniques underwent ESD. They were compared with a matched cohort of 30 patients who had early rectal neoplasms and underwent LE between 2000 and 2009. Short-term clinical outcomes including postprocedure recovery and morbidity were compared between the two groups.
Results
The mean lesion size was comparable between the ESD and LE groups (2.9 vs 2.6 cm; P = 0.423), but the mean distance of the lesions from the anal verge was greater in the ESD group (8.6 vs 5.0 cm; P = 0.001). En bloc resection was achieved for 12 patients (85.7%) in the ESD group and for all the patients in the LE group. The ESD group exhibited a trend toward a longer operative time (77.5 vs 50.0 min; P = 0.081) but lower morbidity (7.1 vs 33.3%; P = 0.076). The time to full ambulation was shorter in the ESD group (0 vs 1 day; P = 0.005), but the hospital stay was similar in the two groups (2.5 vs 4.0 days; P = 0.129).
Conclusion
For the treatment of early rectal neoplasms, ESD offers better short-term clinical outcomes in terms of faster recovery and possibly lower morbidity than LE. Further prospective studies with a larger sample are needed to validate the benefits of rectal ESD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Many studies have proven that early colorectal cancer (CRC) screening can result in a remarkably reduced CRC incidence and mortality [1]. As the incidence of CRC has been rapidly rising in Asian countries, more and more screening colonoscopies are being performed for prevention or early detection of this fatal disease [2, 3]. Coupled with the increasing application of chromoendoscopy and magnifying endoscopy, more early colorectal neoplasms are currently being diagnosed [4]. Most of these early lesions can be removed by conventional polypectomy. However, if the colorectal neoplasm is too large or cannot be removed en bloc by conventional endoscopic techniques, operative procedures are required to reduce the risks of incomplete removal and local recurrence.
For early rectal neoplasms not amenable to conventional endoscopic removal, the alternative treatment option is local excision (LE) procedures, including direct transanal excision and transanal endoscopic microsurgery (TEM). These local procedures have proved to be safe and effective in the treatment of rectal lesions [5–9]. However, both LE approaches must be performed with the patient under either general or spinal anesthesia, and special surgical instruments are required.
Endoscopic submucosal dissection (ESD) is a novel endoscopic procedure that enables en bloc resection of colorectal lesions irrespective of the lesion’s size and location. It can be performed with the patient under conscious sedation without anesthesia. The ESD approach has a reported perforation rate of 2% to 10%, an en bloc resection rate of 80% to 90%, and a short-term recurrence rate for colorectal ESD of 0% to 2.1% [10–13].
To date, no report can be found in the literature comparing colorectal ESD and LE for early rectal neoplasms or lesions not amenable to en bloc resection by conventional endoscopic techniques. This study aimed to compare the short-term clinical outcomes for the two approaches.
Methods
The hospital charts of patients with early rectal neoplasms or lesions not amenable to en bloc resection by conventional endoscopic techniques who underwent either ESD or LE between 2000 and 2010 at our institution were retrospectively reviewed. The data pertaining to the patients’ characteristics, pathologic information, operative details, and short-term clinical outcomes were recorded. All the patients who underwent rectal ESD were compared with a matched cohort of patients who underwent LE.
ESD
We have performed colorectal ESD at our institution since 2007. In this study, the indications for ESD included early rectal neoplasms 2 cm or larger that were deemed not feasible for en bloc resection with conventional polypectomy or endoscopic mucosal resection and those without endoscopic signs of massive submucosal invasion (including excavated/depressed morphology or Kudo’s pit pattern type V). Benign submucosal lesions such as rectal carcinoid tumors also were considered good indications for ESD.
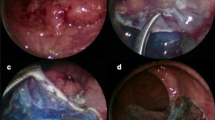
Our techniques for rectal ESD have been reported previously [14]. In short, the ESD procedure was performed using a gastroscope with a water-jet function and carbon dioxide (CO2) insufflation. A short transparent hood was attached to the tip of the gastroscope. A mixture of hyaluronic acid, normal saline, adrenaline, and indigocarmine was injected into the submucosal plane to create a visible submucosal cushion for elevation of the lesion. Mucosal incision and submucosal dissection were performed using the Dual Knife or Insulated Tip Knife (Olympus Medical System, Tokyo, Japan) depending on the individual endoscopist’s preference. All procedures were performed with the patient under conscious sedation. Specimens were fixed on a foam board for pathologic examination.
LE
The indications for LE included benign rectal neoplasms, early T1 rectal cancers, and rectal carcinoid tumors. All LE procedures (either direct transanal excision or TEM) were performed with the patient under spinal or general anesthesia. For direct transanal excision, an anal retractor was first introduced into the anal canal to maintain exposure. The lesion then was excised with electrocautery under direct vision. For TEM, a rectoscope 4 cm in diameter and 20 cm long was inserted into the rectum after anal dilation, and specially designed instruments were used for dissection. Then, partial- or full-thickness excision of rectal lesions was performed under binocular stereoscopic vision and CO2 insufflation [15, 16].
Postprocedure management
All the patients were allowed to have a full diet as tolerated and were mobilized immediately after the procedures. They were discharged home when they could void well and were fully ambulatory and complication free.
Outcome measurements
Short-term clinical outcomes were the major interest of this study. They included operative time, morbidity rate, time to full ambulation, and duration of hospital stay. Morbidity was defined as any complication that required reintervention or resulted in prolonged hospital stay. Bleeding was defined as any bleeding episode during or after the procedure that required transfusion. Perforation was either noted as a complication during the procedure or diagnosed when free intraperitoneal gas was noted on imaging after the procedure. Acute retention of urine was defined as failure to void within 24 h after the procedure. Other operative details including the operative time and the en bloc resection rate also were compared between the two groups.
Statistical analyses
Categorical data were analyzed with chi-square test or Fisher’s exact test where appropriate, whereas continuous data were analyzed with Student’s t-test or the Mann-Whitney U test. A P value less than 0.05 was considered statistically significant. All calculations were done using the SPSS statistical software package (SPSS version 15; SPSS, Chicago, IL, USA).
Results
Between 2007 and 2010, 14 patients with early rectal neoplasms or lesions underwent ESD at our institution. They were compared with a matched cohort of 30 patients who underwent LE for early rectal neoplasms or lesions between 2000 and 2009. The demographic data of the patients and the characteristics of the rectal lesions are summarized in Table 1. The two groups did not differ in terms of age, gender, American Society of Anesthesiologists grading, size of lesions, or pathologic subtypes.
Most of the lesions were benign adenomas, with the remainder including early adenocarcinoma, hyperplastic polyp, and rectal carcinoid tumor. The mean distance of the lesions from the anal verge was significantly greater in the ESD group (8.6 vs 5.0 cm; P = 0.001). En bloc resection was achieved for 12 patients (85.7%) in the ESD group and all the patients in the LE group.
The perioperative outcomes are summarized in Table 2. The ESD group exhibited a trend toward a longer operative time (78 vs 50 min; P = 0.081). The median time to full ambulation was significantly shorter in the ESD group (0 vs 1.0 day; p = 0.005). All the patients except two were fully ambulatory on the same day after ESD, whereas 18 patients were not able to mobilize fully until 1 day after LE. The hospital stay also was shorter in the ESD group (2.5 vs 4.0 days), but the difference did not reach statistical significance (P = 0.129).
Table 3 shows the details of the short-term morbidity in both groups. There was a trend toward lower morbidity in the ESD group (7.1 vs 33.3%; P = 0.076). One patient in the ESD group experienced a perforation during the procedure and was managed successfully by immediate endoscopic clipping. The patient recovered well without any sequelae.
Perforation into the peritoneal cavity as an intraoperative complication was noted for two patients in the TEM group. The perforations were closed with continuous sutures, and no subsequent adverse events were noted. Acute retention of urine (AROU) accounted for half of all the morbidities in the LE group, whereas no such complication was reported in the ESD group.
Discussion
Colorectal ESD is a well-established technique in Japan. According to the literature published by Japanese experts, colorectal ESD has a reported perforation rate of approximately 2–10% and a bleeding rate of about 1–2% [10–12, 17]. Although colorectal ESD is a relatively new technique for us, we nevertheless achieved a perforation rate of 7.1% and a bleeding rate of 0% in our study. Our en bloc resection rate was 85.7% compared with 80–90% reported in literature [10–12]. Therefore, our results are comparable with the worldwide standard despite the fact that we still are in the learning phase.
Among all the complications of colorectal ESD, perforation is the most worrisome even for experienced endoscopists. However, rectal ESD has a lower risk for perforation than colonic ESD. Anatomically, the rectum is fixed in the pelvis and has a relatively thick wall without haustraution. Hence, scope manipulation is technically easier and safer within the rectal lumen. Furthermore, because of its largely extraperitoneal location, the risk of fecal peritonitis is relatively low even if perforation of the rectum occurs. Experts therefore recommend the rectum as the best location for beginners to start practicing colorectal ESD [18].
Our study proved that ESD possibly has a lower morbidity rate than LE. Only one patient experienced perforation during ESD, which was managed successfully by endoscopic clipping. This encouraging result has further confirmed the fact that the rectum is a good location to start one’s learning curve for colorectal ESD without fear of jeopardizing the patient’s safety.
Concerning postprocedure recovery, our study showed that the time until full ambulation was significantly shorter in the ESD group. The hospital stay also was shorter in the ESD group, but the difference did not reach statistical significance. These advantages were achieved at the expense of a slightly longer operative time in the ESD group. We believe that the operative time for ESD will be further reduced with more practice and that the advantages of ESD over LE in terms of faster recovery and lower morbidity will become more obvious with accumulation of experience.
Direct transanal excision is a traditional surgical method for treating lower rectal lesions, and it also is the simplest approach. However, lesions located in the upper rectum are not within reach of traditional transanal excision. Because TEM has a greater reach into the middle and upper rectum, it was developed as a minimally invasive alternative to deal with these higher lesions.
Either spinal or general anesthesia is required for both approaches to facilitate anal dilation and application of the anal retractor or rectoscope. Unfortunately, anesthesia may have a negative impact on early postoperative recovery. For instance, patients may feel drowsy and nauseated after general anesthesia and thus refuse to have early feeding and mobilization. Furthermore, spinal anesthesia is a well-known risk factor for AROU [19, 20]. In fact, anal dilation or retraction per se may cause anal pain and also may result in urinary retention. These factors explain why the LE group had a significantly higher incidence of AROU.
On the other hand, ESD is performed with the patient under conscious sedation, and there is no need to dilate the anal sphincter. This may account for the lower morbidity rate and the shorter time until full ambulation in the ESD group.
Despite an increasing incidence of early rectal lesions and the rapid development of new therapeutic techniques, evidence comparing the old and new approaches for the treatment of these lesions still is scarce. To our knowledge, this is the first report in the literature comparing ESD and LE for early rectal neoplasms or lesions not amenable to en bloc resection by conventional endoscopic techniques.
Although this study has the limitation of being a retrospective review with a small sample size, it still can provide valuable information regarding the role of rectal ESD and can set the stage for further prospective studies. Indeed, further prospective randomized trials with a larger sample and a longer follow-up period are needed to validate the benefits of rectal ESD and to evaluate its oncologic safety.
Conclusion
For the treatment of early rectal neoplasms, ESD has better short-term clinical outcomes than LE in terms of faster recovery and possibly a lower morbidity rate. Prospective studies with larger samples are needed to validate the benefits of rectal ESD.
References
Rim SH, Seeff L, Ahmed F, King JB, Coughlin SS (2009) Colorectal cancer incidence in the United States, 1999–2004 : an updated analysis of data from the National Program of Cancer Registries and the Surveillance, Epidemiology, and End Results Program. Cancer 115:1967–1976
Hyodo I, Suzuki H, Takahashi K, Saito Y, Tanaka S, Chiu HM, Kim NK, Li J, Lim R, Villalon A, Boku N (2010) Present status and perspectives of colorectal cancer in Asia: Colorectal Cancer Working Group report in 30th Asia-Pacific Cancer Conference. Jpn J Clin Oncol 40(Suppl 1):i38–i43
Zavoral M, Suchanek S, Zavada F, Dusek L, Muzik J, Seifert B, Fric P (2009) Colorectal cancer screening in Europe. World J Gastroenterol 15:5907–5915
Hurlstone DP, Cross SS, Adam I, Shorthouse AJ, Brown S, Sanders DS, Lobo AJ (2004) Efficacy of high magnification chromoscopic colonoscopy for the diagnosis of neoplasia in flat and depressed lesions of the colorectum: a prospective analysis. Gut 53:284–290
Middleton PF, Sutherland Lm, Maddern GJ (2005) Transanal endoscopic microsurgery: a systemic review. Dis Col Rectum 48:270–284
McCloud JM, Waymont N, Pahwa N, Varghese P, Richards C, Jameson JS, Scott AND (2006) Factors predicting early recurrence after transanal endoscopic microsurgery excision for rectal adenoma. Colorect Dis 8:581–585
Casadesus D (2009) Surgical resection of rectal adenoma: a rapid review. World J Gastroenterol 15:3851–3854
Pigot F, Bouchard D, Mortaji M, Castinel A, Juguet F, Chaume JC, Faivre J (2003) Local excision of large rectal villous adenomas: long-term results. Dis Colon Rectum 46:1345–1350
Featherstone JM, Grabham JA, Fozard JB (2004) Per-anal excision of large, rectal, villous adenomas. Dis Colon Rectum 47:86–89
Tanaka S, Oka S, Chayama K (2008) Colorectal endoscopic submucosal dissection: present status and future perspective, including its differentiation from endoscopic mucosal resection. J Gastroenterol 43:641–651
Saito Y, Fukuzawa M, Matsuda T, Fukunaga S, Sakamota T (2010) Clinical outcome of endoscopic submucosal dissection versus endoscopic mucosal resection of large colorectal tumors as determined by curative resection. Surg Endosc 24:343–352
Yoshida N, Wakabayashil N, Kanemasa K (2009) Endoscopic submucosal dissection for colorectal tumors: technical difficulties and rate of perforation. Endoscopy 41:758–761
Tanaka S, Oka S, Kaneko I, Hirata M, Mouri R, Kanao H, Yoshida S, Chayama K (2007) Endoscopic submucosal dissection for colorectal neoplasia: possibility of standardization. Gastrointest Endosc 66:100–107
Hon SS, Philip CW, Li JC, Lo AW, Ng SS (2010) Endoscopic submucosal dissection of a broad-based rectal polyp (video demonstration). Surg Pract 14:75–76
Buess G, Hutter F, Theiss J, Bobel M, Isslhard W, Pichlmaier H (1984) Das Syste fur die transanale endoskopische Rectumoperation. Chirurg 55:677–680
Guerrieri M, Baldarelli M, de Sanctis A, Campagnacci R, Rimini M, Lezoche E (2010) Treatment of rectal adenomas by transanal endoscopic microsurgery: 15 years’ experience. Surg Endosc 24:445–449
Yoshida N, Yagi N, Naito Y, Yoshikawa T (2010) Safe procedure in endoscopic submucosal dissection for colorectal tumors focused on preventing complications. World J Gastroenterol 16:1688–1695
Deprez PH, Bergman JJ, Meisner S, Ponchon T, Repici A, Dinis-Ribeiro M, Haringsma J (2010) Current practice with endoscopic submucosal dissection in Europe: position statement from a panel of experts. Endoscopy 42:853–858
Darrah DM, Griebling TL, Silverstein JH (2009) Postoperative urinary retention. Anesthesiol Clin 27:465–484
Baldini G, Bagry H, Aprikian A, Carli F (2009) Postoperative urinary retention: anesthetic and perioperative considerations. Anesthesiology 110:1139–1157
Disclosures
Sophie S. F. Hon, Simon S. M. Ng, Philip W. Y. Chiu, Francis K. L. Chan, Enders K. W. Ng, Jimmy C. M. Li, Janet F. Y. Lee, and K. L. Leung have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hon, S.S.F., Ng, S.S.M., Chiu, P.W.Y. et al. Endoscopic submucosal dissection versus local excision for early rectal neoplasms: a comparative study. Surg Endosc 25, 3923–3927 (2011). https://doi.org/10.1007/s00464-011-1821-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-1821-z