Abstract
Background
Staple line leaks represent a major concern in all laparoscopic operations but are particularly important in bariatric surgery, where leak complications carry significant morbidity and mortality. Therefore, several means of staple line reinforcement have been described, but none is totally accepted. In this study, we attempt to illuminate any clear benefit of staple line reinforcement through a systematic review and meta-analysis of reported articles.
Methods
Two major databases (PubMed and Cochrane) were searched and assessed by two reviewers. Inclusion criteria were: detailed description of operative technique, especially concerning staple line reinforcement, and possible existence of proven staple line leak. Selected studies were evaluated by systematic review and meta-analysis according to their eligibility. The study population was finally divided into two groups: reinforcement (of any type) and no reinforcement.
Results
In the initial search, 126 studies were obtained. Then, 17 full papers, both randomised controlled trials (RCTs) and non-RCTs, were included in the systematic review. Seven studies, comprising 3,299 patients, were examined for evaluation of population odds of leak (7.69), which was considered clinically significant. Meta-analysis of three studies comprising 1,899 patients revealed no clear benefit of reinforcement group, though with marginal significance.
Conclusions
Although several drawbacks exist, this study illustrates two important aspects: that current staplers may not be uniformly reliable, and that staple line reinforcement does not seem to have any clear benefit, at least concerning leak rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
For decades, surgical staplers have been a significant adjunct in gastric, colorectal and thoracic surgery, although they evolved from pure necessity. The end of World War II saw the USSR with a shortage of trained surgeons, therefore the Scientific Institute for Surgical Devices and Instruments encouraged the development of stapling devices in an attempt to alleviate this health care crisis. These devices, the ancestors of modern staplers, facilitated several surgical emergency procedures, which eventually could be carried out by surgeons with limited training and experience [1]. In the laparoscopic era, staplers became a necessity, as intracorporeal suturing and knot-tying are substantially more demanding than in open surgery. As a result, novel technologies and devices have emerged in order to minimise the necessity for advanced skills and allow the expansion of laparoscopic surgery. In the same regard, robotic surgery may provide a theoretical advantage of more accurate and safer tissue manipulation, which could potentially ameliorate suturing procedures [2], but such speculative improvements require validation in large-scale controlled clinical trials and establishment in widespread real-life use.
Staple line leaks are particularly significant in bariatric laparoscopic procedures. Poor general health of these patients makes them particularly vulnerable to complications, as even “minor” leaks may provoke prolonged recovery, or death [1]. Reported leak rate in laparoscopic Roux-en-Y gastric bypass (LRYGBP), the most commonly performed bariatric operation in the USA, varies widely from 0 to 8% [3]. Unfortunately, anastomotic staple line leak (ASL) is responsible for 37.5% of mortality related to LRYGBP [4]. Furthermore, sepsis and mortality rates following unrecognised leakage exceed 50% [5]. The financial consequence of prolonged hospitalisation is also impressive, as cumulative expenses for ASL often exceed US $200.000 [5].
As revealed by the above, reliability and safety of stapling devices are crucial but as yet not ensured. To diminish leaks, numerous techniques and materials have been described. Suture reinforcement of staple line, fibrin sealants and buttressing materials (absorbable or non-absorbable) represent the main categories.
The aim of the present study is to examine any possible clear benefit of staple line reinforcement according to the most recent literature, considering that operative technique and stapling technology have been adequately standardised.
Materials and methods
Literature search
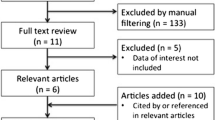
Medline and Cochrane databases were searched using the keywords “laparoscopic surgery staple line leak”, “bariatric surgery staple line leak” and “staple line reinforcement”, without imposing any limitation. Literature search was not initially limited to bariatric procedures, in order to identify the largest number of papers available. Manual cross-reference search was also performed, with the same aim. Eligibility of studies was assessed primarily by title and then by abstract. Finally, studies that appeared relevant were obtained as full papers and evaluated by two reviewers (G.A.G. and S.P.E.). Eventually, the selected studies were divided into two groups: those eligible for systematic review and those for meta-analysis. Study population was also divided into two groups: the no-reinforcement group, where only staplers were used for anastomosis or bowel division, and the reinforcement group, in all other cases (suture reinforcement, fibrin sealant, buttressing material and combination of buttressing and fibrin sealant).
Study selection criteria
Systematic review (SR) included studies pertaining to three laparoscopic bariatric operations, regardless of initial body mass index (BMI), age, sex, comorbidities or which staplers were used. Operations were LRYGBP, laparoscopic vertical banded gastroplasty (LVBG) and laparoscopic sleeve gastrectomy (LSG). Separate evaluation for each operation was not considered imperative, as all three were well-established bariatric procedures, applied in the same organs, and stapling devices were used. The sole parameter examined was post-operative staple line leak, confirmed either by radiologic upper gastrointestinal (GI) study or by re-operation. Studies describing re-operation for peritonitis of unclear origin were not evaluated. Intra-operative leaks detected by methylene blue infusion or air insufflation were also not evaluated, as they could have evolved from device misuse or device failure. Six-row linear staplers and/or circular staplers were used in LRYGBP and LVBG procedures, while in LSG only six-row linear staplers were applied. The studies included were not necessarily designed for evaluation of leaks. Randomised controlled trials (RCTs) and non-RCTs were included for the SR, as the outcome of a proven leak cannot be biased. Detailed description of operative technique and potential staple reinforcement was prerequisite for inclusion. Occasional placement of sutures or clips and enterotomy closure with sutures were not considered as reinforcement. In order to perform meta-analysis, exclusively studies with comparisons between groups were selected.
However, several drawbacks do exist. Operations such as LRYGBP involve both linear as well as circular staplers; reinforcement means are not evaluated separately. Moreover, staple lines were present in both organ division and anastomosis, and the total stapled tissue length differs not only between various procedures but even between operations of the same type. Nevertheless, we consider that the examined variable is simple and could be evaluated even under these circumstances, especially when the number of reported RCTs is rather limited. Heterogeneity of included studies is substantial, but has been taken into consideration.
Statistical analysis
Meta-analysis was performed by the random-effects model of DerSimonian and Laird, estimated by using the restricted maximum-likelihood method, which takes into account both study sample size and the estimate of between-study variation (i.e. study heterogeneity) when weighting study effects [6]. The specialised MIX software for meta-analysis (version 1.7) was applied [7]. To evaluate whether the results of the studies were homogeneous, we used Cochran’s Q test (large heterogeneity is present when p < 0.10). We also calculated the quantity I 2, which describes the percentage variation across studies that is a result of heterogeneity rather than chance, according to the equation I 2 = 100% × (Cochran Q − degrees of freedom)/Cochran Q [8]. Because negative values of I 2 were set equal to zero, I 2 lay between 0 and 100%. A value of 0% indicates no observed heterogeneity, whereas larger values indicate increasing heterogeneity.
Results
One hundred twenty-six articles were initially obtained. Seventy-five articles were excluded by title and another 28 were rejected by abstract. Overall, 17 full papers were obtained and evaluated by systematic review (Table 1). Most of the publications were recent (from 2004 to 2009), so it is rational to state that operative technique and stapling technology have been adequately standardised.
Seven authors reported no reinforcement, whereas ten described some type of reinforcement. LRYGBP was performed in nine studies, LSG in five, LSG/biliopancreatic diversion (BPD) in two and LVBG in one. Reinforcement materials that have been used were SeamGuard™ (W.L. Gore & Associates, Flagstaff, AZ, USA), Peristrips Dry™ (Synovis Surgical Innovations, St Paul, MN, USA), PSD Veritas™ (Synovis Surgical Innovations, St Paul, MN, USA) and Tisseel VH™ (Baxter Healthcare Corp., Deerfield, IL, USA). Surgicel™ (Ethicon, Cincinnati, OH, USA) was used in one study [9] as a haemostatic agent rather than as a fibrin sealant, which was not considered as reinforcement. In one study [10] the reinforcement material was applied in circular stapler.
Three of the overall extracted studies were RCTs, while seven studies, including 3,299 patients in total, reported staple line leaks (events) and were meta-analysed for evaluation of the population odds risk for leak. Finally, three studies reporting comparisons of events between groups were evaluated in order to estimate the relative risk for leak in cases with staple line reinforcement versus control (Table 2). Cochran’s Q test resulted in P = 0.10 (Q = 10.71), and the corresponding I 2 value was 44%, both indicating that heterogeneity among studies was moderate to large.
Figure 1 illustrates a high–low–close plot of summary estimate for population odds for leak derived from the calculated upper and lower boundaries of the 95% confidence intervals, which correspond to the leak rates reported in the relevant literature (seven studies). The overall percentage odds for leak rate (7.69%) is considered clinically significant, since the 95% CIs did not rule out a leak rate as high as 17%. Figure 2 shows a forest plot of the summary estimate for relative risk for leak in cases with reinforcement versus without reinforcement (three studies, including 1,899 subjects in total). This calculation, which assessed only studies with reported effect size and control group, resulted in a 5% probability (relative risk 0.95) favouring no reinforcement that reached marginal statistical significance (95% CI 0.92–0.99). Figure 3 presents a funnel plot of the three aforementioned studies included in the estimation of the relative risk for leak.
Discussion
Stapling devices are expected to overcome various compromises. First, they should provide sufficient tissue apposition and haemostasis, yet without provoking ischaemia or tissue destruction [1]. Given that different tissues have different thickness and strength, various cartridge sizes are available in order to provide successful stapling. All manufacturers suggest the theoretically optimal cartridge size for each organ, but miscellaneous topical conditions (i.e. oedema, distension) or certain organs (i.e. stomach) may need more than one cartridge size [5, 11]. Hence, in practice, cartridge selection is sometimes problematic, and improper size can be catastrophic [5, 11–13]. Human tissues consist of a liquid and a solid component, so they are considered as biphasic. Baker et al. [1] indicated that time is a crucial factor in stapling mechanics, and this is likely to represent another compromise. Adequate time allows tissue compression and creep, but if the procedure is elongated, could cause excessive tensile strength and tissue destruction. However, even when optimal application has been achieved, a stapler misfire can turn out to be disastrous. The “migratory crotch staple”, in particular, can destroy the whole staple line and, when identified, should be removed [11]. Therefore, most authors strongly recommend staple line inspection or intraoperative leak test, whenever possible.
There is no doubt that technical errors are also present in open surgery, but staple line inspection and repair is easier and faster. Advanced laparoscopic procedures, although feasible in several centres, are still a hindrance for numerous surgeons worldwide, despite gained experience. Thus, the need for reliable, safe and handy staplers is more than obvious. Fear of a possible leak, especially in difficult, obese patients, instigated intense research into staple-line reinforcement means.
The most inexpensive alternative is over-sewing of the staple line, which theoretically enhances tissue approximation and haemostasis. Schweitzer et al. [14] report a zero leak rate in 251 LRYGBP using a running suture as second layer and in their final remark state that no leaks have been observed in over 500 LRYGBPs performed to date. However, various studies are sceptical, supporting that suture placement is time consuming, can result in tissue tearing and has some degree of difficulty [5, 13]. Chen et al. [11] conclude that “in the sleeve consensus, the surgeons were not unanimous about reinforcement versus oversewing; therefore, the decision will be at the surgeon’s discretion and experience.”
Fibrin sealants (i.e. Tisseel™) have predominantly been used as haemostatic agents in both open and laparoscopic surgery. Nevertheless, several reports advocate their role in wound healing, describing their action as biological glue, through scaffolding fibroblast and reparative cells [12]. Nguyen et al. [15] report that covering the staple line with such an agent significantly reduced leak complications in an animal model and resulted in leak-free LRYGBP in 66 patients. DeMaria et al. [16] also reported a decreased leak rate using fibrin sealant. Fullum et al., however, reinforced the staple line using both buttressing material and fibrin sealant [5].
Buttressing materials were initially used in thoracic surgery to reduce air leaks [12]. Absorbable (SeamGuard, PSD Veritas) and non-absorbable (PeriStrips Dry) materials have also been used widely in colorectal and bariatric surgery [17]. The concept seems attractive, as staples are anchored, not into friable tissue, but into the buttressing material, which is denser and sturdier. Arnold et al. [12], using an animal model, reported that staple line reinforced with bovine pericardium remained intact at significant higher intraluminal pressures than without buttressing. Also, buttressing materials are reported to be effective in decreasing staple line bleeding (intra- and extraluminal) and thus operative time [18]. In fact, several studies [17, 18] have found that buttressing materials have a better impact in reducing bleeding than leak rate. Possibly, the higher burst pressure offered by buttressed stapling is valuable in special cases, such as obstruction. Debate has also evolved concerning the long-term safety of non-absorbable materials. Several authors describe that bovine pericardial strips can persist as foreign bodies and there are case reports of staple relocation [18] or migration to stomach and GI tract [11]. In contrast, others employed non-absorbable materials and do not mention such complications [13]. Despite reported advantages, it does not seem that buttressing offers clear benefit. Chen et al. [11] postulate that “there is no reason to suspect that buttressing material reduces the risk for staple line leak.”
In our study, the overall estimated odds for leak are 7.69, and this finding is clinically significant. It seems that gained experience and current stapling technology have not succeeded in providing a uniformly safe operation. Interestingly, Gonzalez et al. [19] report that incidence of staple line leaks seems to be independent of number of LRYGBPs performed. Besides, according to our results, reinforcement of any type does not appear to have clear benefit, although with marginal statistical significance. However, the asymmetric relationship between effect and study size in our meta-analysis suggests the possibility of (1) publication bias, (2) systematic difference between smaller and larger studies (“small-study effects”) and/or (3) inappropriate effect measures. Nevertheless, it is rational to postulate that the very low or even zero leak rate that several studies report is a result mainly attributable to personal skill or operative technique rather than to standardised device application. However, this discrepancy remains inadequately explained, as in most procedures standard stapling devices have been used.
It is well established that the aetiology of staple line leaks, although multifactorial, can be classified into two main categories: mechanical/tissue causes, which occur in the first 2–3 post-operative days, and ischaemic causes, which are described to occur 5–7 days post-operatively [1]. Several authors support that the majority of leaks occur in the first 48 h, therefore being mechanical not ischaemic [1, 18]. Since no clear benefit results from reinforcement, one can state that leaks might sometimes be a consequence of stapler function per se. Baker et al. [1] report that optimal pressure for staplers is found to be 8 g/m2 for gastric tissue and 6 g/m2 for esophagus and intestine. Nevertheless, staplers, at least linear ones, close on a pre-fixed position. Possibly, a pressure-sensitive device could optimise tissue approximation further, considering a pressure limit rather than a gap limit.
A more homogeneous and accurate approach is, without doubt, necessary in evaluating staple line leaks, but for the time being, given data do not support such an analysis. Several drawbacks exist in this study, and more RCTs are needed. It could also be argued that changes in staple manufacturing represent an additional confounding factor in studies comparing bariatric surgery series from different time periods, whereas lack of support from industry is a major disincentive for designing and conducting RCTs on this topic. Nevertheless, two major points concerning laparoscopic bariatric surgery are illustrated: that stapling devices do not yet offer uniform safety, and that staple line reinforcement is questionable. Possibly, in the robotic era, a case-sensitive stapling technology will provide faster and safer operations, even with minimal experience.
References
Baker RS, Foote J, Kemmeter P, Brady R, Vroegop T, Serveld M (2004) The science of stapling and leaks. Obes Surg 14:1290–1298
Marecik SJ, Chaudhry V, Jan A, Pearl RK, Park JJ, Prasad LM (2007) A comparison of robotic, laparoscopic, and hand-sewn intestinal sutured anastomoses performed by residents. Am J Surg 193:349–355 discussion 355
Basu NN, Leschinskey D, Heath DI (2008) The use of Seamguard to buttress the suture repair of a staple line leak following laparoscopic gastric bypass for obesity. Obes Surg 18:896–897
Podnos YD, Jimenez JC, Wilson SE, Stevens CM, Nguyen NT (2003) Complications after laparoscopic gastric bypass: a review of 3464 cases. Arch Surg 138:957–961
Fullum TM, Aluka KJ, Turner PL (2009) Decreasing anastomotic and staple line leaks after laparoscopic Roux-en-Y gastric bypass. Surg Endosc 23(6):1403–1408
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Bax L, Yu LM, Ikeda N, Tsuruta H, Moons KG (2006) Development and validation of MIX: comprehensive free software for meta-analysis of causal research data. BMC Med Res Methodol 6:50
Sutton AJ, Abrams KR, Jones DR, Sheldon TA (2000) Methods for meta-analysis in medical research, 1st edn. Wiley, London
Kasalicky M, Michalsky D, Housova J, Haluzik M, Housa D, Haluzikova D, Fried M (2008) Laparoscopic sleeve gastrectomy without an over-sewing of the staple line. Obes Surg 18:1257–1262
Jones WB, Myers KM, Traxler LB, Bour ES (2008) Clinical results using bioabsorbable staple line reinforcement for circular staplers. Am Surg 74:462–467 discussion 467-468
Chen B, Kiriakopoulos A, Tsakayannis D, Wachtel MS, Linos D, Frezza EE (2009) Reinforcement does not necessarily reduce the rate of staple line leaks after sleeve gastrectomy. A review of the literature and clinical experiences. Obes Surg 19:166–172
Arnold W, Shikora SA (2005) A comparison of burst pressure between buttressed versus non-buttressed staple-lines in an animal model. Obes Surg 15:164–171
Shikora SA, Kim JJ, Tarnoff ME (2008) Comparison of permanent and nonpermanent staple line buttressing materials for linear gastric staple lines during laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis 4:729–734
Schweitzer MA, Lidor A, Magnuson TH (2006) A zero leak rate in 251 consecutive laparoscopic gastric bypass operations using a two-layer gastrojejunostomy technique. J Laparoendosc Adv Surg Tech A 16:83–87
Nguyen NT, Nguyen CT, Stevens CM, Steward E, Paya M (2004) The efficacy of fibrin sealant in prevention of anastomotic leak after laparoscopic gastric bypass. J Surg Res 122:218–224
DeMaria EJ, Sugerman HJ, Kellum JM, Meador JG, Wolfe LG (2002) Results of 281 consecutive total laparoscopic Roux-en-Y gastric bypasses to treat morbid obesity. Ann Surg 235:640–645 discussion 645-647
Saber AA, Scharf KR, Turk AZ, Elgamal MH, Martinez RL (2008) Early experience with intraluminal reinforcement of stapled gastrojejunostomy during laparoscopic Roux-en-Y gastric bypass. Obes Surg 18:525–529
Miller KA, Pump A (2007) Use of bioabsorbable staple reinforcement material in gastric bypass: a prospective randomized clinical trial. Surg Obes Relat Dis 3:417–421 discussion 422
Gonzalez R, Haines K, Gallagher SF, Murr MM (2006) Does experience preclude leaks in laparoscopic gastric bypass? Surg Endosc 20:1687–1692
Dapri G, Vaz C, Cadiere GB, Himpens J (2007) A prospective randomized study comparing two different techniques for laparoscopic sleeve gastrectomy. Obes Surg 17:1435–1441
Nocca D, Aggarwal R, Blanc P, Gallix B, Di Mauro GL, Millat B, Seguin des De Hons C, Deneve E, Rodier JG, Tincani G, Pierredon MA, Fabre JM (2007) Laparoscopic vertical banded gastroplasty. A multicenter prospective study of 200 procedures. Surg Endosc 21:870–874
Simper SC, Erzinger JM, Smith SC (2007) Comparison of laparoscopic linear staplers in clinical practice. Surg Obes Relat Dis 3:446–450 discussion 450-441
Givon-Madhala O, Spector R, Wasserberg N, Beglaibter N, Lustigman H, Stein M, Arar N, Rubin M (2007) Technical aspects of laparoscopic sleeve gastrectomy in 25 morbidly obese patients. Obes Surg 17:722–727
Baltasar A, Serra C, Perez N, Bou R, Bengochea M, Ferri L (2005) Laparoscopic sleeve gastrectomy: a multi-purpose bariatric operation. Obes Surg 15:1124–1128
Consten EC, Gagner M, Pomp A, Inabnet WB (2004) Decreased bleeding after laparoscopic sleeve gastrectomy with or without duodenal switch for morbid obesity using a stapled buttressed absorbable polymer membrane. Obes Surg 14:1360–1366
Disclosures
Authors Giannopoulos, Tzanakis, Rallis, Efstathiou, Tsigris, and Nikiteas have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Giannopoulos, G.A., Tzanakis, N.E., Rallis, G.E. et al. Staple line reinforcement in laparoscopic bariatric surgery: does it actually make a difference? A systematic review and meta-analysis. Surg Endosc 24, 2782–2788 (2010). https://doi.org/10.1007/s00464-010-1047-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1047-5