Abstract
Introduction
Fine-needle aspiration (FNA) is a well-established technique to obtain cytological specimens, but it does not permit the extraction of histological tissue-core samples, which, if available, may increase the yield and accuracy of the histopathological diagnosis. This prospective study was designed to assess the yield and diagnostic accuracy of endoscopic ultrasound (EUS)-guided Trucut needle biopsy (TNB) as first-line diagnostic method for suspected malignant lesions identified by upper gastrointestinal EUS.
Methods
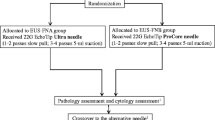
In a prospective case series, 24 consecutive patients (14 women; median age, 68 (range, 38–84) years) with suspected malignancy underwent EUS-TNB with a 19-gauge needle. EUS was performed with a linear scanning echo endoscope. When the EUS-TNB device did not collect adequate samples, subsequent EUS-FNA was performed. The presence or absence of malignancy was confirmed by postoperative histopathology or diagnostic imaging follow-up for at least 9 months.
Results
Adequate tissue specimens were obtained in 20 of 24 (83%) patients by TNB. An accurate diagnosis was achieved in 19 of 20 (95%) patients in whom TNB was successful with a sensitivity and specificity of 93% and 100%, respectively. In 11 patients malignant disease was found, whereas 8 patients showed benign lesions on TNB-obtained histopathology. Thirteen patients underwent additional EUS-FNA. The diagnosis by TNB was confirmed in seven of nine (78%) patients with additional FNA. In three of four patients with inadequate TNB, the diagnosis was established by FNA. The overall accuracy of EUS-TNB was 79% (19/24) for all patients and 92% (22/24) with subsequent FNA. The positive and negative predictive values for the diagnosis of a malignant lesion by EUS-TNB were 57.9% and 88.9%, respectively. Neither method had any procedure-related complications.
Conclusions
EUS-guided TNB is a safe and accurate technique to obtain core specimen for histopathologic diagnosis in patients with suspected malignancies on upper gastrointestinal EUS. FNA can serve as rescue technique and should be performed if TNB fails to obtain adequate tissue samples.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Endoscopic ultrasound (EUS) is a well-established method for the evaluation of intraintestinal and extraintestinal mass lesions as well as for paraintestinal lymphadenopathy in the gastrointestinal tract [1]. EUS-guided fine-needle aspiration (EUS-FNA) has emerged as an important addition to EUS that permits the cytological evaluation of suspected mass lesions [2]. The diagnostic yield of EUS-FNA is approximately 90–95%, with an overall sensitivity and specificity of 90% and 100%, respectively [3, 4]. Although EUS-FNA has been shown to be a safe and feasible procedure, the overall diagnostic accuracy ranges between 68.4% and 84.3%, depending on several factors [5, 6]. First, the accuracy of the diagnosis relies on immediate review of the specimen for sampling adequacy by an on-site cytopathologist, which is rarely available during the procedure [7]. Second, some neoplasms, such as well-differentiated adenocarcinomas, stromal tumors, or lymphomas, are difficult to diagnose based solely on cytology because EUS-FNA typically destroys the tissue architecture and immunocytology often is not possible.
Compared with EUS-FNA a recently developed EUS-guided Trucut biopsy needle (EUS-TNB) has been shown to provide core-tissue specimens suitable for conventional histology and with the potential of a higher diagnostic accuracy compared with cytology samples obtained by EUS-FNA [8, 9]. This study was designed to assess the feasibility, safety, yield, and diagnostic accuracy of EUS-TNB as a first-line diagnostic method in patients with suspected malignancies, as well as the diagnostic impact of additional EUS-FNA as a rescue method in cases of EUS-TNB sampling failure.
Patients and methods
All patients were investigated after written, informed consent and according to the guidelines of the local ethics committee. Between March 2003 and September 2006, 24 consecutive patients (14 women; median age, 68 (range, 38–84) years) with suspected malignant lesions identified by diagnostic imaging or endoscopy and within reach of upper gastrointestinal EUS, such as pancreatic masses, mediastinal or perigastric masses, and enlarged lymph nodes, were recruited into the study. All patients underwent EUS-TNB using a linear-array echo endoscope with a 3.7-mm diameter working channel (GF-UCT 140, Olympus, Hamburg). EUS-TNB was performed with a 19-gauge Trucut needle (Quick-Core, Cook Medical, Bloomington, IN). Each EUS-TNB specimen was immediately reviewed by the endoscopist. When the procedure was suspected to have failed to obtain an adequate sample for diagnosis (e.g., small or friable specimens), subsequent EUS-FNA was performed with a 22-gauge FNA needle (Echotip Echo-1-22, Cook Medical).
All procedures were performed with the patient under conscious sedation. For EUS-FNA, a 22-gauge needle (Echotip, Cook Medical) was advanced into the lesion under real-time ultrasound visualization as described in detail by Wiersema et al. [10]. After removing the central stylet, a 10-ml syringe with extension tubing was attached to the hub of the needle and suction was applied while the needle was moved backward and forward within the lesion. After retraction of the needle and removal of the central stylet, the fluid was dispersed over cytology slides and allowed to air-dry before staining.
For EUS-TNB the needle is equipped with a 20-mm tissue tray, a 19-gauge outer cutting needle, and a spring mechanism built into the handle. Under real-time ultrasound guidance, the target lesion was punctured and the cutting needle advanced to its 20-mm limit. At this point, the spring-loaded outer needle was fired over the tissue-tray. After firing, the Trucut needle was removed from the endoscope and the tissue specimens obtained was fixed immediately in formalin.
For histological evaluation, tissue specimens were fixed with buffered formaldehyde 4.5% (Sigma-Aldrich, Germany). Sections were prepared for processing with hematoxylin and eosin stain, histochemistry, and immunohistochemistry. Immunohistochemistry was performed using the indirect immunoperoxidase technique with a typical panel of markers according to the differential diagnosis of each case (Dako, Glostrup, Denmark). Histopathological and cytological samples were reviewed by different pathologists and cytologists for specimen adequacy and diagnostic accuracy. When histopathological evaluation of the Trucut biopsy specimen was diagnostic for malignancy, this was regarded as definitive diagnosis and the patient was treated accordingly. When the evaluation was negative for malignancy further diagnostic procedures, including diagnostic imaging and/or endoscopy were performed, and a clinical follow-up of at least 9 months was required to rule out or confirm the presence of malignancy. Diagnostic accuracy was calculated for all patients who underwent EUS-TNB or for patients with usable samples from EUS-TNB alone. Sensitivity, specificity, overall accuracy, and positive and negative predictive values for malignancy were calculated.
Results
Twenty-four patients underwent EUS-TNB for 24 previously identified lesions. Tissue specimens were obtained in 20 of 24 (83%) patients of whom subsequent diagnosis was available for 19 patients. In one patient with a paraesophageal mass, no definitive diagnosis could be made, although EUS-TNB had obtained what appeared to be adequate tissue specimens. In 4 of 24 patients EUS-TNB obtained inadequate samples. The diagnostic sensitivity calculated for all 24 patients investigated was 78% (95% confidence interval (CI), 0.548–0.906) and 93% (95% CI, 0.696–0.988) for patients (20/24) with adequate tissue samples.
The mean length of the tissue cylinder obtained by EUS-TNB was 8.5 (range, 2–20) mm. The mean number of passes was 1.4 (range, 1–2) for TNB and 1.7 (range, 1–3) for FNA.
For 13 patients in whom the procedure was assumed to have failed to obtain an adequate tissue-sample for diagnosis by EUS-TNB, additional EUS-FNA was performed. For all patients investigated, EUS-TNB and EUS-FNA were performed without any procedure-related complications. The location of lesions is summarized in Table 1.
Histopathological analysis of the biopsy specimens was diagnostic for malignancy in 11 of 20 (55%) patients in whom EUS-TNB yielded adequate samples (9 adenocarcinoma, 1 squamous cell carcinoma, 1 neuroendocrine tumor). In the remaining nine patients, biopsy specimens revealed benign lesions in eight cases, which were confirmed to be benign by imaging and by additional clinical follow-up of at least 9 months. In one patient, EUS-TNB and EUS-FNA samples suggested malignancy, but the definitive diagnosis of squamous cell carcinoma could only be confirmed with the surgical resection specimen. The histological diagnoses are shown in Table 2.
Immunohistochemistry was used in 14 of 20 samples obtained by EUS-TNB. A tumor primary could be identified in 7 of 11 malignancies (metastasis of uterine carcinoma, metastasis of a cholangiocarcinoma, pancreatic adenocarcinoma, squamous cell carcinoma, metastasis of bronchiogenic carcinoma) by investigating a typical panel of surface-antigen markers, including CD19, CD20, CD34, CD45, CD117, Ki67, CEA, CA19–9, and Ca 72–4.
In three of four patients in whom EUS-TNB obtained inadequate samples, subsequent EUS-FNA recovered adequate cell specimens for diagnosis (2 adenocarcinoma, 1 non-Hodgkin’s lymphoma). In one patient with an adrenal gland mass neither EUS-TNB nor EUS-FNA could obtain adequate samples. This lesion was later classified as benign, because no change in the size was seen on follow-up imaging studies at 3 and 9 months.
The overall accuracy of EUS-TNB for all 24 patients in the study was 79% (19/24). When EUS-TNB was combined with subsequent EUS-FNA in cases without adequate specimens from EUS-TNB, the diagnostic accuracy increased to 92% (22/24). When analysis of diagnostic accuracy was limited to the 20 patients with adequate TNB specimens, EUS-TNB provided the correct diagnosis in 95% (19/20). The positive predictive value for a malignant lesion was 58%, and the negative predictive value was 89%.
Discussion
The composition of our patient cohort clearly tested the advantages of EUS-TNB because it included patients with mediastinal tumors of unknown primary, adrenal tumors, and pancreatic masses, in all of whom a histological, rather than cytological, diagnosis would be predicted to determine subsequent treatment. A similar approach was suggested in a recent study that recommended the use of EUS-TNB for suspected malignancy with EUS-FNA as a rescue procedure [11]. Such a rescue procedure might be even more important when the lesion can only be reached by transduodenal puncture, which is technically too challenging for EUS-TNB [12]. Despite recently available needles with larger diameters, EUS-FNA yields mostly cytological samples, which often limits an adequate assessment of the biological behavior and the correct diagnosis of the primary lesion because of the lack of tissue architecture. To obtain core-tissue specimens for histopathology a novel cutting needle device has been developed, and in this study we evaluated its use as diagnostic method for patients with suspect intestinal or extraintestinal mass lesions.
EUS-TNB obtained visible core specimens in approximately 80% of our patients, which is in accordance with previous reports [13, 14]. Although the endoscopist judged the EUS-TNB obtained sample inadequate in 13 patients (mostly for small or friable specimens), in all but one of these cases the pathologist was able to make an accurate histological diagnosis, which was confirmed by the cytology taken during subsequent EUS-FNA. In the single case in which EUS-TNB failed, EUS-FNA also could not harvest enough material for an accurate diagnosis. Because the sample was suggestive for malignant disease, a second EUS-FNA was performed; however, the second cytology sample also failed to specify the diagnosis. Overall, this indicates that with EUS-TNB, even when it does not yield an intact tissue cylinder but barely visibly tissue fragments, an accurate histopathology diagnosis can still be made and additional EUS-FNA is unnecessary in most cases. Furthermore, the obtained EUS-TNB specimens are easily assessed for adequacy by the endoscopist himself and, therefore, the on-site presence of a cytopathologist might not be necessary. This helps to reduce the required time and cost of the procedure.
In more than two-thirds of the samples obtained by EUS-TNB, additional immunohistochemistry improved the diagnostic accuracy and identified the cell proliferation rate as well as the primary tumor site of malignant lesions. Because malignancy was frequently suspected when enlarged lymph nodes or metastases were found on EUS, often in the absence of a known primary, EUS-TNB and subsequently immunohistochemical analysis were essential to establish the primary site of the cancer in many cases.
In four patients no tissue could be obtained by EUS-TNB. Although the EUS-guided needle had successfully hit the lesion, no specimen could be collected despite repeated passes with the needle. In three of these four lesions the analysis of the specimens obtained by subsequent EUS-FNA identified the lesions as necrotic cell mass. Because necrotic lesions have typically lost their tissue architecture and show a more viscous consistency, it is not surprising that no material could be harvested on the tissue-tray of the needle. Although only two patients had areas of suspected necrosis during a previously performed EUS, an attempt at Trucut needle puncture should not be restricted to patients without obvious necrotic lesions, even if our experience suggests that EUS-FNA would be preferable in the presence of necrosis.
In the course of our study, we encountered several technical problems. Because of the stiffness of the 19-gauge needle, passage through the echoendoscope was sometimes difficult, especially when the tip of the endoscope was angulated. Once the Trucut needle was threaded through the endoscope, the tip of the endoscope became much stiffer, limiting its flexion. This impaired the extraction of samples from the deeper part of the duodenum and occasionally from the head of the pancreas. Similar problems have been encountered by other investigators, and a transduodenal approach was reported to be successful in only 40% of cases [15, 16]. To overcome this difficulty and because the mean length of the tissue cylinders obtained by TNB was 8.5 mm, shorter tissue trays could be tested and would probably result in equal diagnostic efficacy. This small change may increase the flexibility of the endoscope while only marginally reducing the size of core specimens obtained. The development of a better EUS-TNB device to biopsy pancreatic lesions via the duodenal wall could improve the accuracy of the diagnosis of pancreatic cancer, which often is accompanied by an extensive desmoplastic reaction that might render the cytology inaccurate and would call for core biopsies for histopathology [5, 16, 17].
All patients in our study had lesions >20 mm in diameter, and those could be safely and readily sampled. Moreover, in all patients, we visualized the tip of the needle as well as the cutting sheath inside the lesion, which not only ensures an accurate biopsy and adequate tissue harvesting but also reduces possible complications. With this approach our patients did not experience a single complication arising from the procedure. Our experience suggests that sampling of lesions <20 mm in diameter could more easily result in complications because of perforation of the lesion by the Trucut needle. This condition also may improve by using needles with a shorter specimen tray. In previous reports the overall rate of complications from EUS-TNB was 2.5% (6/242 combined patients); adding our cohort would decrease the rate to 2.2% [5, 6, 8, 9, 11, 12, 15–24]. The complication rate for EUS-FNA is generally reported to be as much as 2% [10]. Taking this into account, EUS-TNB can be regarded as equally safe but with a higher diagnostic accuracy compared with EUS-FNA.
Our study has a few additional drawbacks, such as the inclusion of patients with lesions in various anatomical locations and with different types of benign and malignant diseases. Nevertheless this is representative for the patient selection in most tertiary referral centers with a high-volume endoscopy unit. We calculated the operating characteristics, such as sensitivity (92%), specificity (100%), and positive (58%) and negative predictive value (89%) of EUS-TNB, and these compare favorably with the data reported recently by Storch and coworkers [25].
Conclusions
We tested the diagnostic accuracy of a new EUS-guided Trucut biopsy needle as a first-line method for patients with intestinal or extraintestinal mass lesions of suspected malignancy. In cases in which TNB is not diagnostic, subsequent FNA may provide the accurate diagnosis and therefore both procedures can be used complementarily. A study by Wittmann and coworkers recently showed that the combination of EUS-FNA and EUS-TNB in lesions >2 cm in diameter significantly improves adequate sampling and diagnostic accuracy by as much as 95% [14]. Our data confirm this conclusion. Further studies warranted only after technical improvements of the device have enhanced its flexibility, especially for lesions that can only be reached via the transduodenal route. Currently we cannot recommend TNB for routine use in lesions of the head of the pancreas.
References
Shah JN, Ahmad NA, Beilstein MC, Ginsberg GG, Kochman ML (2004) Clinical impact of endoscopic ultrasonography on the management of malignancies. Clin Gastroenterol Hepatol 2:1069–1073
Savides TJ, Donohue M, Hunt G, Al-Haddad M, Aslanian H, Ben-Menachem T, Chen VK, Coyle W, Deutsch J, DeWitt J, Dhawan M, Eckardt A, Eloubeidi M, Esker A, Gordon SR, Gress F, Ikenberry S, Joyce AM, Klapman J, Lo S, Maluf-Filho F, Nickl N, Singh V, Wills J, Behling C (2007) EUS-guided FNA diagnostic yield of malignancy in solid pancreatic masses: a benchmark for quality performance measurement. Gastrointest Endosc 66:277–282
Mortensen MB, Pless T, Durup J, Ainsworth AP, Plagborg GJ, Hovendal C (2001) Clinical impact of endoscopic ultrasound-guided fine needle aspiration biopsy in patients with upper gastrointestinal tract malignancies. A prospective study. Endoscopy 33:478–483
Erickson RA (2004) EUS-guided FNA. Gastrointest Endosc 60:267–279
Iglesias Garcia J, Dominguez-Munoz JE (2007) Endoscopic ultrasound-guided biopsy for the evaluation of pancreatic tumors. Gastroenterol Hepatol 30:597–601
Saftoiu A, Vilmann P, Guldhammer Skov B, Georgescu CV (2007) Endoscopic ultrasound (EUS)-guided Trucut biopsy adds significant information to EUS-guided fine-needle aspiration in selected patients: a prospective study. Scand J Gastroenterol 42:117–125
Eloubeidi MA, Tamhane A, Jhala N, Chhieng D, Jhala D, Crowe DR, Eltoum IA (2006) Agreement between rapid onsite and final cytologic interpretations of EUS-guided FNA specimens: implications for the endosonographer and patient management. Am J Gastroenterol 101:2841–2847
Levy MJ, Jondal ML, Clain J, Wiersema MJ (2003) Preliminary experience with an EUS-guided Trucut biopsy needle compared with EUS-guided FNA. Gastrointest Endosc 57:101–106
Varadarajulu S, Fraig M, Schmulewitz N, Roberts S, Wildi S, Hawes RH, Hoffman BJ, Wallace MB (2004) Comparison of EUS-guided 19-gauge Trucut needle biopsy with EUS-guided fine-needle aspiration. Endoscopy 36:397–401
Wiersema MJ, Hawes RH, Tao LC, Wiersema LM, Kopecky KK, Rex DK, Kumar S, Lehman GA (1992) Endoscopic ultrasonography as an adjunct to fine needle aspiration cytology of the upper and lower gastrointestinal tract. Gastrointest Endosc 38:35–39
Gines A, Wiersema MJ, Clain JE, Pochron NL, Rajan E, Levy MJ (2005) Prospective study of a Trucut needle for performing EUS-guided biopsy with EUS-guided FNA rescue. Gastrointest Endosc 62:597–601
DeWitt J, McGreevy K, LeBlanc J, McHenry L, Cummings O, Sherman S (2005) EUS-guided Trucut biopsy of suspected nonfocal chronic pancreatitis. Gastrointest Endosc 62:76–84
Aithal GP, Anagnostopoulos GK, Tam W, Dean J, Zaitoun A, Kocjan G, Ragunath K, Pereira SP (2007) EUS-guided tissue sampling: comparison of “dual sampling” (Trucut biopsy plus FNA) with “sequential sampling” (Trucut biopsy and then FNA as required). Endoscopy 39:725–730
Wittmann J, Kocjan G, Sgouros SN, Deheragoda M, Pereira SP (2006) Endoscopic ultrasound-guided tissue sampling by combined fine needle aspiration and Trucut needle biopsy: a prospective study. Cytopathology 17:27–33
Larghi A, Verna EC, Stavropoulos SN, Rotterdam H, Lightdale CJ, Stevens PD (2004) EUS-guided Trucut needle biopsies in patients with solid pancreatic masses: a prospective study. Gastrointest Endosc 59:185–190
Itoi T, Itokawa F, Sofuni A, Nakamura K, Tsuchida A, Yamao K, Kawai T, Moriyasu F (2005) Puncture of solid pancreatic tumors guided by endoscopic ultrasonography: a pilot study series comparing Trucut and 19-gauge and 22-gauge aspiration needles. Endoscopy 37:362–366
Levy MJ, Wiersema MJ (2005) EUS-guided Trucut biopsy. Gastrointest Endosc 62:417–426
Pungpapong S, Wallace MB (2005) EUS-guided Trucut needle biopsy: is more tissue really better? Gastrointest Endosc 62:602–604
Levy MJ, Reddy RP, Wiersema MJ, Smyrk TC, Clain JE, Harewood GC, Pearson RK, Rajan E, Topazian MD, Yusuf TE, Chari ST, Petersen BT (2005) EUS-guided Trucut biopsy in establishing autoimmune pancreatitis as the cause of obstructive jaundice. Gastrointest Endosc 61:467–472
Yadav D, Levy MJ, Schwartz D, Jondal ML, Clain J, Wiersema MJ (2003) EUS-guided Trucut biopsy for diagnosis of an esophageal stromal tumor: case report. Gastrointest Endosc 58:457–460
Ribeiro A, Vernon S, Quintela P (2004) EUS-guided Trucut biopsy with immunohistochemical analysis of a gastric stromal tumor. Gastrointest Endosc 60:645–648
Gleeson F, Clarke E, Kelly S, Hargadan G, Kenny E, MacMathuna P, Lennon J (2005) Diagnosis by EUS Trucut biopsy of extrapulmonary tuberculosis in a patient with Crohn’s disease treated with infliximab. Gastrointest Endosc 61:489–492
Aithal GP, Anagnostopoulos GK, Kaye P (2005) EUS-guided Trucut mural biopsies in the investigation of unexplained thickening of the esophagogastric wall. Gastrointest Endosc 62:624–629
Storch I, Shah M, Thurer R, Donna E, Ribeiro A (2008) Endoscopic ultrasound-guided fine-needle aspiration and Trucut biopsy in thoracic lesions: when tissue is the issue. Surg Endosc 22:86–90 Epub 2007 May 4
Storch I, Jorda M, Thurer R, Raez L, Rocha-Lima C, Vernon S, Ribeiro A (2006) Advantage of EUS Trucut biopsy combined with fine-needle aspiration without immediate on-site cytopathologic examination. Gastrointest Endosc 64:505–511
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wahnschaffe, U., Ullrich, R., Mayerle, J. et al. EUS-guided Trucut needle biopsies as first-line diagnostic method for patients with intestinal or extraintestinal mass lesions. Surg Endosc 23, 2351–2355 (2009). https://doi.org/10.1007/s00464-009-0345-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-009-0345-2