Abstract
Background
Laparoscopic surgery has dramatically improved surgical care of patients reducing postoperative pain, wound infection rate, hospital stay, inability to work, risk of hernia, and cosmetic result. Natural orifice transluminal endoscopic surgery (NOTES) is even less traumatic to the abdominal wall and might further improve minimal invasive surgery of patients, but might also increase surgical risk when used by a transgastric or transcolonic approach with flexible endoscopes. Therefore we decided to use a transvaginal approach using rigid laparoscopic instruments for cholecystectomies.
Methods
Through a 5-mm incision deep in the umbilicus a pneumoperitoneum was created. The optic and a dissector were inserted through the posterior fornix of the vagina under laparoscopic control from the umbilicus and a transvaginal gallbladder removal was performed.
Results
20 patients were successfully operated in a 4.5-month period. Operating time was 62 (35–100) min. No intra- or postoperative complications occurred in any patient. Gynecological examination after 8 days showed no negative findings and the cosmetic result was ideal with no visible scars.
Conclusion
In our series we showed that cholecystectomies can be routinely performed in a NOTES technique without visible scar. The transvaginal approach is the safe in NOTES and common laparoscopic instruments can be used as long as there are no better flexible endoscopes for this purpose.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Natural orifice transluminal endoscopic surgery (NOTES) is currently a very important topic for surgeons and gastroenterologists. Rao and Reddy reported about their transgastric appendectomies at several congresses. This was followed by a lot of experimental operations performed in animals [1–6]. In 2007 the first cholecystectomies in human beings were performed with different NOTES techniques [7–10]. From the first case on we have used laparoscopic instruments instead of a flexible endoscope [10]. In this study we report about a series of 20 patients who underwent cholecystectomy without visible scar in a combined transvaginal and transumbilical technique.
Method
The choice of the operative technique finally depended on the patient’s decision. Only patients with a high probability of severe adhesions in the lower abdomen and patients with a body mass index (BMI) > 40 kg/m2 were excluded.
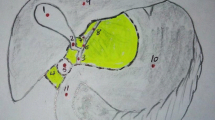
With the patient in lithotomy position we made a 5-mm incision deep in the umbilicus and insufflated the abdomen with a Verres needle. Diagnostic laparoscopy was performed with a 5-mm optic. In steep Trendelenburg position the mandrin of a 5-mm trocar was inserted through posterior fornix of the vagina under laparoscopic control and replaced by a 5-mm extra-long dissector (Aesculap, Tuttlingen, Germany). Aside this instrument a 10-mm trocar was inserted (Fig. 1). From now on we used the extra-long 10-mm 45° optic (Olympus, Hamburg, Germany). The optic in the umbilicus was replaced by another dissector. In anti-Trendelenburg position we then retracted the gallbladder with the instrument coming through the vagina and dissected it through the umbilical trocar. When the cystic duct and the cystic artery were identified, they were clipped through the umbilicus with a 5-mm clip device (Ethicon, Hamburg, Germany) and divided from there. The gallbladder was then mobilized from the liver with an electric hook. For removal we again used the 5-mm optic from the umbilicus and pulled the gallbladder through the 10-mm colpotomy, which was enlarged bluntly with a clamp if needed. The defects in the vagina were sutured with resorbable thread.
As this operative technique is just a combination of daily gynecological practice (transvaginal hydrolaparoscopy) and daily surgical practice, specific ethical considerations were not necessary. However, patients were informed that the combination of these two daily practices was new.
Results
In a 4.5-months period from June until November 2007 we performed 162 cholecystectomies, 114 in female patients, and 20 of them in the above described technique. All these 20 operations were finished successfully. In the first seven cases the insertion of the instruments through the vagina and the removal of the specimen were performed by a gynecologist. The gallbladder was dissected by two surgeons. From case 8 on the whole operation was performed by two surgeons. The average operation time was 62 (35–100) min.
In the beginning we chose “easy” cases and then enlarged the indication to patients with inflammation of the gallbladder, previous surgery, and adipositas. The gallbladder had no or little signs of inflammation and adhesions in 14 cases. Three times we operated on a severe acute and three times on a chronic cholecystitis. Sixteen patients had no previous abdominal surgery. Four patients presented after Cesarean section (2), hysterectomy (1), and adnectomy (2). One patient had a BMI of 35 kg/m2. The only variation of the above described technique, which was needed in one case of chronic inflammation, was an additional incision in the upper abdomen for the insertion of a drainage (we were afraid of bile leakage after damage of the liver tissue).
Patients chose this technique because of scientific interest [2] and mostly because of the ideal cosmetic result.
The postoperative course was uneventful in all patients. Eighteen patients were discharged on the second postoperative day, the first patient on the third, and one older lady only wanted to go home after 6 days. Patients only complained about the well-known consequences of pneumoperitoneum, while none had pain caused by the vaginal manipulation. Two postmenopausal patients felt mild burning in the vagina on the first day. Postmenopausal women received hormone suppositories for 5 days. All patients were seen by the gynecologists a week after surgery, without any negative findings.
Discussion
Laparoscopic surgery has brought a lot of advantages to our patients in terms of postoperative pain, wound infection, hospital stay, inability to work, risk of hernia, and cosmetic result. NOTES is less traumatic to the abdominal wall and, thus, might further improve surgical care of patients. However, it might also increase risk of laparoscopic surgery depending on the anatomical approach and difficulties related to use of flexible endoscopes. Lack of sterilization and healing problems of the gastric or colonic wall can add severe complications to quite simple operations such as cholecystectomies and appendectomies. To date, NOTES was always performed with flexible endoscopes, which are difficult to handle in the abdominal cavity and most surgeons have little experience in flexible endoscopy.
Besides our own first case [10] there is only one publication in the scientific literature about a NOTES operation in a human being [9]. Marescaux and colleagues performed a cholecystectomy using a two-channel gastroscope inserted through the vagina and a 2-mm trocar in the right middle abdomen. The gallbladder was retracted via the 2-mm port and dissected and clipped with the gastroscope. The operation was carried out by three surgeons, a gynecologist, and a gastroenterologist. Not only the number of specialists but also the operation time of 3 h reflects the problems of this technique.
From newspapers we know about two other groups who have operated human beings. At Columbia University a woman underwent a cholecystectomy using a flexible endoscope through the vagina with the help of three abdominal trocars [7]. Swanstrom has performed three cholecystectomies with the transgastric approach, but also using two or three abdominal trocars [8].
We have experience with the transvaginal approach from the beginning of the laparoscopic era. We removed colon segments and spleens through the posterior fornix of the vagina and published this technique in 1994 [11]. Later we abandoned this technique because we performed colon resections laparoscopically assisted and removed spleens after morcellation. However, the gynecologists in our team continued to use this approach for laparoscopic diagnosis and resection. Data in the literature prove that the vaginal approach has little risk [12, 13], and our technique is even safer than these gynecological operations as we control the insertion of the vaginal instruments laparoscopically.
As a consequence we decided to perform transvaginal NOTES using common laparoscopic instruments. This results in ideal cosmetic results, because the cholecystectomy is not visible in our patients. As far as we know these are the first cholecystectomies without visible scar. The question of whether this approach also has advantages concerning pain, infection, and hernia can only be answered by a prospective randomized trial.
In our series of 20 patients we could show that this technique can be applied routinely. The average operation time of 62 min is longer than in conventional laparoscopic surgery. In 2006 we had an average operation time of 45 min in 430 cholecystectomies. We believe that it will take a little more time even after extensive experience, but this time is certainly justified in a patient with special cosmetic interest, and depending on further study results possibly also in routine cases.
As the insertion of instruments through the posterior fornix of the vagina and the closure of these wounds is easy to learn for a surgeon, we could perform our operations with two surgeons in recent cases. This is another important advantage of our technique, as it simplifies daily planning and performance of the routine program in surgery departments.
There is extensive experience of our gynecological colleagues with the vaginal approach to the abdominal cavity (hysterectomy, laparoscopy). We do not have to expect more risks concerning infection and wound closure than in conventional laparoscopic surgery. This is an important difference from the transgastric and transcolonic approach, in which instruments entering the abdominal cavity are contaminated, and there is little and primarily experimental experience with the endoscopic closure of the gastric and colonic wall, approaches that naturally have higher risks of severe complications.
With currently available flexible endoscopes an abdominal operation is a very demanding procedure. This might become better when new instruments are available. Until then, the use of laparoscopic instruments in NOTES procedures seems to be much easier.
Concluding, a NOTES cholecystectomy with the combined transvaginal and transumbilical approach, using standard instruments and techniques, provides the best chance to optimize surgical care of patients today.
References
Kaloo AN, Singh VK, Jagannath SB, Niiyama H, Hill SL, Vaughn CA, Magee CA, Kantsevoy SV (2004) Flexible transgastric peritoneoscopy: a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc 60:114–117
Jagannath SB, Kantesevoy SV, Vaughn CA, Chung SS, Cotton PB, Gostout CJ, Hawes RH, Pasricha PJ, Scorpio DG, Magee CA, Pipitone LJ, Kalloo AN (2005) Peroral transgastric endoscopic ligation of fallopian tubes with long-term survival in porcine model. Gastrointest Endosc 61:449–453
Park PO, Bergström M, Ikeda K, Fritscher-Ravens A, Swain P (2005) Experimental studies of transgastric gallbladder surgery: cholecystectomy and cholecystogastric anastomosis. Gastrointest Endosc 61:601–606
Pai RD, Fong DG, Bundga ME, Odze RD, Rattner DW, Thompson CC (2006) Transcolonic endoscopic cholecystectomy: a NOTES survival study in a porcine model. Gastrointest Endosc 64:428–434
Kantsevoy SV, Hu B, Jagannath SB, Vaughn CA, Beitler DM, Chung SS, Cotton PB, Gostout CJ, Hawes RH, Pasricha PJ, Magee CA, Pipitone LJ, Talamini MA, Kalloo AN (2006) Transgastric endoscopic splenectomy. Is it possible? Surg Endosc 20:522–525
Fong DG, Rai RD, Thompson CC (2007) Transcolonic endoscopic abdominal exploration: a NOTES survival study in a porcine model. Gastrointest Endosc 65:312–318
Grady D (2007) Testing scarless surgery, doctors remove a gallbladder through the vagina. New York Times, 20 April 2007
Rubin R (2007) Surgery offers less scarring. USA Today, 6 August 2007, p 7D
Marescaux J, Dallemagne B, Peretta S, Wattiez A, Mutter D, Coumaros D (2007) Surgery without scars: report of transluminal cholecystectomy in a human being. Arch Surg 142:823–826
Zornig C, Mofid H, Emmermann A, Alm M, von Waldenfels HA, Felixmüller C (2007) Laparoscopic cholecystectomy without visible scar: combined transvaginal and transumbilical approach. Endoscopy 39:913–915
Zornig C, Emmermann A, von Waldenfels HA, Felixmüller C (1994) Die Kolpotomie zur Präparatebergung in der laparokopischen Chirurgie (Colpotomy for removal of specimen in laparoscopic surgery). Chirurg 65:883–885
Miesfeld RR, Giarratano RC, Moyers TG (1980) Vaginal tubal ligation—is infection a significant risk? Am J Obstet Gynecol 137:183–188
Moore ML, Cohen M, Liu GY (2003) Experience with 109 cases of transvaginal hydrolaparoscopy. J Am Assoc Gynecol Laparosc 10:282–285
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zornig, C., Mofid, H., Emmermann, A. et al. Scarless cholecystectomy with combined transvaginal and transumbilical approach in a series of 20 patients. Surg Endosc 22, 1427–1429 (2008). https://doi.org/10.1007/s00464-008-9891-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-008-9891-2