Abstract
Background
The role of duodenal bypass as an underlying mechanism of action in gastric bypass surgery has received considerable attention. We report the initial feasibility study of a totally endoscopically delivered and retrieved duodenal–jejunal bypass sleeve in a chronic porcine model.
Methods
The implant consists of a 60-cm fluoropolymer sleeve that is endoscopically deployed via a coaxial catheter system into the jejunum and fixed in the proximal duodenum with a Nitinol anchor. The system creates a proximal biliopancreatic diversion. Six female Yorkshire pigs were endoscopically implanted; all survived. Four animals (group 1) were slated to survive 90 days, two animals (group 2) for 120 days, and three animals (group 3) underwent sham endoscopy and were survived 120 days. Animals were fed standard dry pig chow 0.5 kg three times daily. Data points included daily general health, weekly weight, serum blood tests (complete blood count, amylase, lipase, liver function tests), and monthly evaluation of anchor/sleeve position/patency by fluoroscopy and endoscopy. Following the in-vivo period, the devices were endoscopically removed and the animals were sacrificed. Duodenal and jejunal tissue samples were assessed histologically.
Results
All six test animals were implanted and explanted without significant adverse events. In group 1, the first animal had no device-related issues. The second animal had a pivoted anchor requiring repositioning at day 63. That animal had no further difficulties. The third animal had an incidental partial rotation of the anchor noted at the 90 day explantation. The fourth animal was incidentally implanted with a crossover of the anchor struts, which was endoscopically corrected on day 14. However, on day 20 the animal had persistent vomiting, and the device was explanted. Both group 2 animals survived 120 days. One animal had a partially rotated anchor but was asymptomatic. The average weight gain between test and sham groups was 0.23 kg/day and 0.42 kg/day, respectively (p = 0.01).
Conclusions
A totally endoscopic and reversible bypass of the duodenum and proximal jejunum has been achieved for 90–120 days. Initial experience suggests patency of the sleeve and acceptable tissue response. Reduced weight gain in the test animals suggests device efficacy. Further investigation is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
While the true mechanisms of action of Roux-en-Y gastric bypass surgery continue to be the subject of considerable debate, it appears likely that the associated duodenal–jejunal bypass plays an important role [5]. A device has been developed that is capable of achieving an endoscopic duodenal jejunal bypass. In theory, the duodenal–jejunal bypass sleeve (DJBS) is capable of achieving duodenal–jejunal exclusion and bilopancreatic diversion without the need for stapling or anastomosis. While we postulate that these mechanisms may have considerable effects on glucose tolerance and body weight, the focus of this study was to establish the safety of a chronic indwelling device in a porcine model.
Since our first feasibility study, over 200 DJBS devices have been endoscopically delivered, left in-situ for variable amounts of time, and endoscopically removed in porcine models. This cumulative experience and the numerous iterations that resulted yielded a reproducible delivery and retrieval system and a stable anchor and sleeve design. This report details our most recent long term in-vivo experience with the DJBS in a porcine model.
Methods
The DJBS consists of an implant that is endoscopically delivered, anchored in the proximal duodenum and extended into the jejunum (Fig. 1). The implant consists of a custom self-expanding nickel–titanium alloy (Nitinol) anchor and fluoropolymer sleeve that extends 60 cm into the proximal bowel (Fig. 2). The anchor expands to a 25–50 mm diameter and contains barbs that engage the tissue for stability. Chyme from the stomach passes through the inside of the impermeable liner, thereby creating a proximal intestinal bypass/biliopancreatic diversion.
The anchor and sleeve are delivered via an over-the-wire catheter system that is both endoscopically and fluoroscopically guided (Fig. 3). The anchor and sleeve are supplied pre-loaded into the capsule at the distal end of the catheter. The capsule is tracked over a guidewire and advanced into the duodenum. The distal end of the sleeve is attached to the distal end of the inner catheter with a removable wire. This wire also holds an atraumatic leading ball on the distal end of the inner catheter. To advance the sleeve into the bowel, the inner catheter is pushed from the proximal end with a handle. The atraumatic ball negotiates the bowel and aids in distal sleeve deployment. Once the sleeve is fully deployed, the ball and the sleeve are detached from the catheter. The atraumatic ball is released into the bowel and expelled via normal peristalsis. The catheter is then removed from the bowel leaving the sleeve in place. The anchor is then pushed out of the capsule in place in the bulbous duodenum. The anchor barbs engage the duodenal tissue to prevent movement of the implant.
At the time of explant, the anchor is collapsed by grabbing one of the two drawstrings located at the proximal end of the anchor using a custom grasper (Fig. 4). Pulling the drawstring collapses the anchor and pulls the barbs out of the tissue. Once collapsed, the anchor is pulled inside a retrieval hood located on the distal end of the gastroscope. The hood protects tissue from the barbs during withdrawal thus precluding the need for an overtube.
Six female Yorkshire pigs were anesthetized with Telazol (12 mg/kg) and Zylazen (8 mg/kg) intramuscularly and the device was endoscopically implanted as described above. The animals were then survived with the DJBS as defined below. The porcine model was used as they are omnivores and their gastrointestinal anatomy is similar in size to the human. Animals were roughly 3 months old when implanted and were in their rapid growth phase during the length of the study.
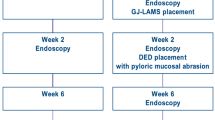
Three groups of animals were studied. Four animals (group 1) were slated to survive 90 days, two animals (group 2) for 120 days, and three animals (group 3) underwent sham endoscopy and were kept alive 120 days. Animals were fed standard dry pig chow 0.5 kg three times daily. Data points included daily general health, weekly weight, pre-implant and post-explant serum blood tests (complete blood count, amylase, lipase, liver function tests). Monthly evaluations were made of the anchor and sleeve position and patency by fluoroscopy and endoscopy.
In the absence of unusual symptoms and following the predetermined in-vivo period, the devices were endoscopically removed and the animals were euthanized and a complete necropsy was performed. The necropsy and histologic analysis was performed by an independent pathologist (Lincoln Associates, St. Paul, MN). The stomach, duodenum, and jejunum were located and gross observations such as adhesions were noted, and then dissected as a block and immersion fixed.
The fixed tissue block was reviewed, and serial cross-sections from the distal pylorus continuing to the proximal jejunum were made at 8–12-mm increments. Following review of observations for each cross-section, selected cross-sections were submitted for preparation of glass slides. Sections were stained with either H&E or Masson’s trichrome.
For one case, the anchor was left in position and fixed. Following fixation, the tissue block was trimmed to a length extending 1 cm proximal and distal to the dilated duodenum containing the anchor. The trimmed tissue block was embedded in polymethylmethacrylate and then 1-mm-thick wafers made with a diamond saw and then ground and polished optically flat at a 100-μm section thickness and stained with H&E.
Results
All six test animals were endoscopically implanted and explanted without significant adverse events. All three sham animals underwent successful upper endoscopy without sequela and survived 120 days without incident. In group 1, three animals survived 90 days with the implant. Of these, one animal had no device-related issues. One animal was found to have a pivoted anchor that was repositioned at day 63. The animal went on to 90 days without incident. The third animal was explanted at 90 days, but the anchor was found partially rotated sideways in a transverse orientation with respect to the bowel wall. The animal had been asymptomatic. The fourth animal was accidentally implanted with a crossover of the anchor struts. This was endoscopically repaired on day 14 but explanted on day 20 when the animal had persistent vomiting. The follow-up endoscopy on this animal showed a patent and functioning device. However, histologic examination revealed multiple foci of non-obstructing intestinal ulcerations throughout the duodenum and jejunum even beyond the sleeve.
Both group 2 animals survived 120 days and had normal clinical and endoscopic exams throughout the study period. At the time of explant, one animal was incidentally found to have a partially rotated but patent anchor. This anchor also spontaneously rotated sideways in a transverse orientation with respect to the bowel wall.
Contrast injections were performed in all test animals throughout the study period. This was accomplished with an endoscope placed within the anchor region of the implant (Fig. 5). Slow contrast injections indicated device patency and anchor seal.
During the routine monthly examinations, fluoroscopy was also used to measure the diameter of the anchor (Fig. 6). The length of the anchor was known and used as a calibration. Anchors dilated gradually over the first 3 weeks, as shown in (Fig. 7). Following this expansion, the anchor then appeared to maintain its diameter 5–10 mm below its maximum diameter.
Gross tissue analysis
The duodenum was dilated at the level of the anchor with a typical measurement of 4.5 cm (normal = 1.5 cm) (Fig. 8). Adhesions were noted between the duodenal serosa and the liver. Adhesions of the mesentery to the duodenum were also noted. Cross-sections of the dilated duodenum demonstrated a fibrotic attachment of the liver to the duodenal serosa with focal capsular fibrosis. The pancreatic tissue was normal. Hemorrhage other than associated with acute removal was not observed.
At review of the duodenal cross-sections, sites of apposition of the anchor struts to the duodenal wall were readily noted as intramural focal fibrosis, chronic inflammation, and mural tissue debris. However, there were no instances of loss of duodenal mechanical integrity. Along the length of the sleeve within the jejunum, the jejunum appeared normal. During the in-vivo period, all animals had normal serum values across all measured parameters (defined above).
Histology
Histologic observations of the anchor and barb sites were consistent with gross observations and ranged from compression of the mucosa and submucosa to mural fibrosis with replacement of the muscularis with serosal fibrosis (Fig. 8a and b). Strut sites located at the surface of the submucosa or within the muscularis demonstrated a focal chronic inflammation and granulation surrounding the strut but with normal mural anatomy closely distant to these sites. The duodenal mural structure external to the sleeve and between anchor struts was normal in appearance with the submucosa and much of the mucosa readily observed. The duodenum and jejunum distal to the anchor, but under the sleeve, was normal (Fig. 9).
Efficacy
Utilizing Student’s t-test, a statistician calculated that the average weight gain between all test and sham groups was 0.23 kg/day (± 0.12) and 0.42 kg/day (± 0.04), respectively (p = 0.01). This value represents the mean weight gain for all device and sham animals in the study. While all animals were given .5 kg of chow, 3 times daily, and all appeared to completely consume their food, no specific measurements of caloric intake were possible.
Discussion
The recent onslaught of interest in endolumenal therapies has spawned considerable economic and scientific investment in novel forms of therapeutic intervention across various disease states including obesity and diabetes. Natural orifice translumenal endoscopic surgery (NOTES) has received considerable attention of late and reports of early in-vivo experience with these exciting techniques have been published [1]. With the obesity epidemic projected to worsen over time, it is no surprise that significant efforts have been made to find novel endolumenal therapeutic alternatives [1–4, 6]. While each of these exciting and innovative treatments address some aspect of obesity treatment, none of them address the role that the enteroinsular axis may play in hunger and/or glucose metabolism. Whether aberrant release of a putative duodenal signal triggers glucose intolerance or rapid delivery of chyme to the distal small bowel upregulates incretins like GLP-1, duodenal bypass, and its physiologic effects has become the focal point of interest with respect to the underlying mechanism of action behind Roux-en-Y gastric bypass surgery and its effect on glucose tolerance [5].
The DJBS represents the first endolumenal therapy capable of achieving duodenal bypass with minimal intervention. The results of this study show the feasibility and safety of a chronic indwelling device up to 120 days in a porcine model. The safety profile of the DJBS in this study was quite favorable. This trial was designed to investigate the feasibility and safety of 90 and 120 day implants. Five of the six animals maintained the device for their projected duration. Over this time period, the animals were in a normal state of health with regular feeding patterns and bowel habits. Despite the safety, three of the six anchors were found to have spontaneously rotated upon removal. While these findings appeared to be clinically silent, concern exists over the stability of the current anchor and the subsequent risk for migration. The histological examination of the anchor site, suggest a pattern of acute inflammation and erosion into but not through the submucosa. Following this period, a healing phase was apparent, and no further erosion occurs as evidenced by the fact that no transmural erosion was observed. The data show expansion of the anchor over a three week period with subsequent stability of anchor diameter thereafter. It appears that the ultimate determinant of anchor stability and safety will be the balance of anchor expansion, erosion and healing over time.
The sleeve portion of the DJBS, which was 60 cm in length, approximates the length of the biliopancreatic diversion achieved with a standard Roux-en-Y gastric bypass. To the best of our knowledge, all six animals maintained the sleeve in a fully deployed position 60 cm into the small bowel with good patency. Laboratory parameters aimed at detecting biliary tract and/or pancreatic duct obstruction were consistently within the normal range across all animals in this study.
While the focus of this study was feasibility and safety, we attempted to evaluate the device’s effect on body weight. This included utilization of a sham group that underwent endoscopy alone, standardization of diet to the best of our ability given the model, and weekly total body weight measurements. Although all animals gained weight, the device groups did so at a proportionally slower rate while maintaining similar overall behavior and eating habits. The porcine model is less than ideal with respect to weight-related efficacy, but our findings in the alteration of the weight gain curves have led to speculation that the device indeed has some effect on body weight. Current theories in support of this finding would include any or all of the following, either alone or in combination: delayed gastric emptying, early satiety, rapid delivery of undigested nutrients to the distal bowel ± upregulation of hormones such as GLP-1, enhanced delivery of bile salts to the distal bowel, or alterations in metabolic rate. Each of these concepts has been proposed as a potential mechanism of action in association with gastric bypass surgery. We believe that a similar mechanism of action may underlie the DJBS, and we feel that this preclinical feasibility study lends support to additional investigation of safety and efficacy.
References
De la Fuente S. DeMaria E. Reynolds J, Porternier D. Pryor A (2007) New developments in surgery: NOTES. Arch Surg 142:295–297
Garcia-Compean D, Mendoza-Fuerte E, Martinez JA, Villarreal I, Maldonado H (2005) Endoscopic injection of botulinum toxin in the gastric antrum for the treatment of obesity. Results of a pilot study. Gastroenterol Clin Biol 29:789–791
Gostout CJ, Rajan E (2005) Endoscopic treatments for obesity: past, present and future. Gastroenterol Clin North Am 34:143–150
Hu B, Chung SC, Sun LC, Kawashima K, Yamamoto T, Cotton PB, Gostout CJ, Hawes RH, Kalloo AN, Kantsevoy SV, Pasricha PJ (2004) Transoral obesity surgery: endolumenal gastroplasty with an endoscopic suture device. Endoscopy 37:411–414
Rubino F, Forgione A, Cummings DE Vix M, Gnuli D, Mingrone G, Castagneto M, Marescaux J (2006) The mechanism of diabetes control after gastrointestinal bypass surgery reveals a role of the proximal small intestine in the pathophysiology of type 2 diabetes. Ann Surg 244:741–749
Schweitzer M (2004) Endoscopic intraluminal suture plication of the gastric pouch and stoma in post operative Roux y gastric bypass patients. J Laparoendosc Adv Surg Tech 14:223–226
Acknowledgments
This work was supported by funding from GI Dynamics, Inc., 313 Pleasant Street, Watertown, MA 02472.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tarnoff, M., Shikora, S., Lembo, A. et al. Chronic in-vivo experience with an endoscopically delivered and retrieved duodenal-jejunal bypass sleeve in a porcine model. Surg Endosc 22, 1023–1028 (2008). https://doi.org/10.1007/s00464-007-9652-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-007-9652-7