Abstract
Aims
To use meta-analytic techniques to compare peri-operative and short term post-operative outcomes for patients undergoing cholecystectomy via the laparoscopic or mini-open approach.
Methods
Randomised control trials published between 1992 and 2005, cited in the literature of elective laparoscopic (LC) versus mini-open cholecystectomy (MoC) for symptomatic gallstone disease were included. End points evaluated were adverse events, operative and functional outcomes. A random effects meta-analytical model was used and between-study heterogeneity assessed. Subgroup analysis was performed to evaluate the difference in results for study size and quality and data reported from 2000.
Results
Nine randomised studies of 2032 patients were included in the analysis. There was considerable variation in the size and type of incision used for MoC in the studies. There was a significantly longer operating time for the LC group, by 14.14 minutes (95% CI 2.08, 26.19; p < 0.0001). Length of stay was reduced in the LC group by 0.37 days (95% CI −0.53, −0.21; p < 0.0001), with no significant heterogeneity for either outcome. For all other operative and post-operative outcomes, there was no significant difference between the two groups.
Conclusion
MoC appeared to have similar outcomes compared to LC, however LC did reduce the length of hospital stay. MoC is a viable and safe option for healthcare providers without the financial resources for laparoscopic equipment and appropriately trained surgical teams.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic cholecystectomy (LC) has become readily acceptable as the treatment of choice for symptomatic gallstone pathology [1]. It has been shown to have better outcomes compared to the traditional open technique [2]. Although well established in developed countries, a recent cost analysis has shown that LC will only gain economic feasibility over conventional cholecystectomy in less developed health care systems when costs of laparoscopic equipment are reduced and personnel earnings increase sufficiently [3]. A meta-analysis including data from more than 90,000 patients has demonstrated wide variability in the data gathered but generally lower morbidity, despite higher bile duct injury rates, for LC compared to open surgery [4].
Small incision or mini-open cholecystectomy (MoC) has been evaluated as an alternative to LC due to the cost of the equipment, staff and learning curves needed for the latter. Small capital costs for surgical procedures are particularly essential for surgical units with reduced financial resources and yet high volume of patients. A recent study from a rural surgical unit has even assessed the feasibility and usefulness of MoC as a day case procedure, with positive results [5]. There have been several randomized control trials comparing LC versus MoC [6–14], however, currently these data have not been pooled for evaluation of overall outcomes.
The aim of the present study was to use meta-analytical techniques to compare operative and post-operative outcomes from randomised studies of LC versus MoC in patients undergoing elective cholecystectomy for symptomatic gallstone disease.
Methods
Study selection
A Medline (using Pubmed as the search engine), Embase, Ovid, Cochrane database and GoogleTM Scholar search was performed on all studies between 1992 and 2005 for randomised trials comparing elective laparoscopic cholecystectomy (LC) and small incision or mini-open technique (MoC) surgery for symptomatic gallstone disease. The following Mesh search headings were used: “Cholecystectomy”, “laparoscopic cholecystectomy”, “laparoscopy”, “mini-laparotomy”, “mini-open cholecystectomy”, “gallstones / biliary disease / *pathology / *surgery”, “gallstone / *pathology / surgery”, “randomised study”, and “treatment outcome”. The “related articles” function was used in Pubmed to broaden the search, and all titles, abstracts, studies, and citations scanned were reviewed. References of the articles acquired in full were also reviewed. No language restrictions were made. The latest date for this search was 9th May 2006.
Data extraction
Two reviewers (SP and PG) independently extracted the following from each study: first author, year of publication, study population characteristics, study design, inclusion and exclusion criteria, matching criteria, number of subjects operated on with each technique, male to female ratio, conversion rates and outcomes of interest.
Inclusion criteria
In order to be included in the analysis, studies had to: (1) Compare laparoscopic and mini-open techniques in patients undergoing elective cholecystectomy for symptomatic gallstone disease. (2) Report on at least one of the outcome measures mentioned below. (3) Clearly document technique as “laparoscopic” or “min-open”. (4) Clearly report the indications for surgery. When two studies were reported by the same institution and/or authors, they were included only if there was no overlap between the results of the studies. Otherwise, the larger, higher quality studies were included in the analysis.
Exclusion criteria
Studies were excluded from the analysis if: (1) The outcomes of interest were not reported for the two techniques. (2) It was impossible to extrapolate or calculate the necessary data from the published results. (3) There was considerable overlap between authors, centres or patient cohorts evaluated in the published literature.
Outcomes of interest and definitions
The following outcomes were used to compare the laparoscopic surgery (LC) group compared with the mini-open surgery (MoC) group:
-
1.
Operative outcomes included blood loss, operative time and conversion to open procedure.
-
2.
Adverse events included abdominal complications (wound infections, haematoma, bile leak, common bile duct strictures, jaundice, incisional/port site hernias, urinary retention and urinary tract infections) and extra-abdominal complications (pulmonary complications, thromboembolism and cardiac complications).
-
3.
Functional outcomes included length of hospital stay, sick leave, the need for readmission and the need for reoperation.
Mini-open cholecystectomy had to be clearly defined as a less invasive procedure compared to the traditional open cholecystectomy and described in the included studies.
Statistical Analysis
Meta-analysis was performed in line with recommendations from the Cochrane Collaboration and the Quality of Reporting of Meta-analyses (QUORUM) guidelines [15]. Statistical analysis for dichotomous variables was carried out using the odds ratio as the summary statistic. This ratio represents the odds of an adverse event occurring in the LC group compared with the MoC group.
The Mantel-Haenszel method was used to combine the odds ratio for the outcomes of interest using a “random effect” meta-analytical technique. In a random effect model it is assumed that there is variation between studies and the calculated odds ratio thus has a more conservative value [16]. In surgical research, meta-analysis using the random effect model is preferable particularly because patients that are operated on in different centres have varying risk profiles and selection criteria for each surgical technique. Yates’ correction was used for those studies that contained a zero in one cell for the number of events of interest in one of the two groups [17, 18]. These “zero cells” created problems with the computation of ratio measure and its standard error of the treatment effect. This was resolved by adding the value 0.5 in each cell of the 2 × 2 table for the study in question, and if there were no events for both the LC and MoC groups the study was discarded from the meta-analysis. For continuous variables such as operative time or length of stay, statistical analysis was carried out using the weighted mean difference (WMD) as the summary statistic [16].
The quality of the studies was assessed by using the Jadad Score [19, 20]. Studies achieving three or more points (from a maximum of five) were considered as being of high quality. Subgroup analysis was performed by considering studies with greater than 100 patients, high quality studies only, studies published in or since 2000.
Three strategies were employed to quantitatively assess heterogeneity. First, data was re-analysed using both random and fixed effect models. Second, graphical exploration with funnel plots was used to evaluate publication bias [21, 22]. Thirdly subgroup analysis was undertaken using the subgroups described above. Analysis was conducted by using Review Manager Version 4.2 (The Cochrane Collaboration®, Software Update, Oxford).
Results
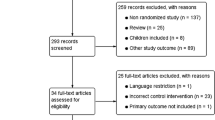
Eligible studies (Figure 1)
One hundred and twenty four reports were identified using the above search keywords. Title and abstract examination resulted in the exclusion of 103 studies (36 case series, 14 letters, 12 reviews, 3 robotic studies, 13 studies on traditional open cholecystectomy and 25 studies on other laparoscopic procedures). This resulted in 21 studies for evaluation in full, of which a further 7 were excluded (5 studies with significant potential for overlapping cohorts and therefore only the largest, highest quality study was included (i.e. 4 studies excluded), 2 studies that only reported outcomes on respiratory function and one study where the data was not extractable). This resulted in 14 comparative studies evaluated [6–14, 23–27], of these 9 were randomised control trials [6–14], including 2032 patients and were therefore included in the meta-analysis. The study characteristics of these 9 trials are shown in Table 1.
Study characteristics (Table 1)
Each study fulfilled the inclusion and exclusion criteria and only randomised elective surgical case data was used. All the studies except two [8, 13] utilised some form of matching criteria. All the studies except one [6] reported on the conversion rates in both the LC and MoC groups. Although all the studies explicitly stated that the comparison was between LC and MoC, the exact definitions for the latter were variable. Six of the studies used the measured length of the subcostal skin incision as their definition for MoC [7, 10–14]. However this ranged from “3–5 cm” [7] to “5–10 cm” [11, 13]. One study used a high transverse sub-xiphoid incision where “the length of the incision was tailored to the individual patient and kept to the minimum necessary to allow safe and adequate access to the gallbladder” [9]. One study varied the length of the subcostal incision according to the depth of the incision from skin to cystic duct [8]. One study described the use of a small transverse incision in the right upper quadrant used by 6 surgeons in the study and a small midline incision used by one surgeon [6]. Four studies reported how many port sites were used [7, 10–12], of these 3 used 4 ports sites [7, 11, 12] and one used 3–4 port sites [10].
Results from overall meta-analysis (Table 2, figures 2a and 2b)
Results from the overall meta-analysis are outlined in table 2 and illustrated as a forest plot in figures 2a and 2b. Using random effects modelling, the overall results demonstrated that there was a significantly longer operating time for the LC group by 14.14 minutes (95% CI 2.08, 26.19; p < 0.0001) with no significant heterogeneity. Length of stay was reduced in the LC group (WMD −0.37days, 95% CI −0.53, −0.21; p < 0.0001) with no significant heterogeneity. For all other operative and post-operative outcomes, there was no significant difference between the two groups. Overall, only the results for conversion rate, abdominal complications and duration of sick leave demonstrated significant heterogeneity (p = 0.02, p = 0.006 and p = 0.009 respectively).
Results from subgroup analysis (Table 3)
Subgroup analysis for studies with more than 150 patients and a Jadad score or 3 or more continued to demonstrate that operative time was significantly longer in the LC group by 18.69 (95% CI 13.08, 24.30; p < 0.0001) and 16.65 (95% CI 13.39, 19.91; p < 0.0001) minutes respectively, with no significant heterogeneity. When studies published from the year 2000 were analysed separately, there was no significant difference in operative time (WMD = −1.95 95% CI −3.04, −0.85; p = 0.20). This effect may be explained by the fact that the more recent publications included surgeons and teams performing laparoscopic cases at a higher point in the learning curve as LC had become more routine surgical cases. This latter subgroup of more recent studies also maintained a significantly reduced length of stay (WMD = −0.40 95%CI −0.47, −0.33; p < 0.0001) and demonstrated reduced sick leave (WMD = −0.30 95%CI −0.44, −0.17; p < 0.0001) with no heterogeneity. However there was no significant difference in the length of stay or amount of sick leave needed in the other two subgroups assessed.
Discussion
The present meta-analysis has illustrated how short-term adverse events are comparable following cholecystectomy performed either by a laparoscopic or mini-open approach. MoC offers a small but statistically significant benefit in the duration of surgery while laparoscopic patients are discharged from hospital on average 0.37 days sooner. While the effects of such differences in length of stay and duration of surgery are unlikely to be clinically significant for individual patients, in the context of a hospital or the wider healthcare system they may have important implications.
Advantages of the present study include the aggregation of a large volume of clinical data (on 2,032 patients) from randomised controlled trials. The appropriate pooling of data is highlighted by the fact that heterogeneity between studies was found to be statistically significant for only three of the 21 outcomes considered on overall meta-analysis, and for none of those outcomes where significant differences between the laparoscopic and mini-laparotomy groups were shown.
The major limitation of this study lies in the accurate definition of ‘mini-laparotomy’ used by the analysed studies. Reported lengths of incision varied from 3–10 cm [11, 13] and it is therefore surprising that a greater degree of heterogeneity between studies was not observed. Other authors have recently highlighted this problem, suggesting that incisions which require some degree of division of the rectus muscle should be considered conversion to a ‘conventional laparotomy’ [7]. The inability to perform meta-analysis of the costs of surgery and post-operative analgesic requirements as well cosmetic and quality of life outcomes, due to inconsistencies in the way that these outcomes were reported, also limit the conclusions that can be drawn.
Cholecystectomy is quoted as the most commonly performed abdominal operation in the United States, with 500,000 procedures annually [28]. Ultrasonographic studies have suggested the prevalence of gallstones to vary across the world at 10–12% in Europeans, 3–4% in Asians and around 5.2–10% in African populations [29]. There has been a steady shift away from open cholecystectomy following the introduction of LC, with the proportion of procedures performed laparoscopically having risen from 0–63% in Scotland between 1990 and 1993 [30]. Despite this it has been suggested that the incision length for open cholecystectomy had been falling at the time when LC became routine, to some extent stifling the development and evaluation of MoC [9]. The introduction of LC is associated with a substantial increase in operating theatre costs due to the purchase price of the laparoscopic equipment [30] as well as the costs of training surgical and theatre staff [9]. In contrast, MoC requires no extra instrumentation and appears to be a skill which can be acquired by surgical trainees without a marked learning curve [7]. Measures can be taken to limit the start-up costs of laparoscopic surgery [31], and some authors have argued that lower overall costs compared even to the mini-laparotomy technique, taking into account the societal costs of lost work-days, are eventually achievable [13]. However, to achieve these reduced costs, some studies have relied on data suggesting that mini-open cholecystectomy is associated with significantly higher rates of bile duct injury and wound infection, neither of which were reflected by the results of the present study or a previous meta-analysis comparing laparoscopic with open cholecystectomy [4]. Differences in convalescence periods were small in the present analysis, as were the benefits in terms of length of stay towards the laparoscopic group. It has been calculated that to equalise hospital costs between LC and MoC, the laparoscopic procedure would need to demonstrate a length of post-operative stay of more than three days less then MoC [30], an effect which is unlikely to be shown, not least in the context of a recent report which showed day-case mini-laparotomy cholecystectomy to be achievable in more than 78% of patients [5].
The results of the present study are suggestive that patients treated in units in developing countries where the start-up costs of minimally invasive surgery are considered prohibitive are not disadvantaged. Although the method of presentation of cost data from the analysed randomised studies precluded meta-analysis, individual studies have consistently shown hospital costs to be cheaper for the mini-laparotomy approach [11, 12, 27, 30], even when the costs of disposable equipment used in the laparoscopic procedure are discounted [11]. The suggestion that LC leads to lower overall costs to society, due to a more rapid return to work, has not been substantiated by the present study. Using sick-leave as a marker of the time taken to return to normal activities, there was no significant difference between the study groups on overall analysis, as well as subgroups of larger studies, and those of higher overall quality. It is only in the subgroup of studies published in or since 2000 that a statistically significant reduction in the duration of sick-leave was shown, perhaps reflecting a more aggressive post-operative policy in recent years, although the clinical relevance of a 0.30 day reduction in the time until return to work for the average patient is debatable. While it could be argued that in overall health economics terms, small benefits for individuals become significant when multiplied by the size of the population at risk. The higher incidences of gallstones appear to occur in European populations where relatively fewer financial constraints and differences in patient expectation might have a greater impact on the decision to offer LC, while in areas where minimising hospital costs is of paramount concern, MoC may be considered the optimal strategy [25].
The issues of cosmesis and quality of life have been relatively poorly addressed by existing studies. Two studies have suggested that overall the quality of life following both procedures is similar, although for those undergoing LC the post-operative improvement appears to be more rapid, equalising by around 12 weeks [6, 11]. Ros et al. reported cosmetic and quality of life data at 1 year following surgery for their trial patients [32] noting no significant differences in pain, analgesic requirements or cosmetic result between the treatment groups. In another 1 year follow-up paper, McMahon et al. [33] reported that the only significant difference in outcomes between the two treatment arms was a significantly higher rate of reported heartburn in the mini-laparotomy group.
While small benefits in the length of stay and return to normal activities may be associated with LC versus MoC, these may be offset by the shorter operating time associated with the open approach. While at approximately 14 minutes per patient overall, the effects for individual patients are not likely to be significant, in the context of a full day list of cholecystectomies such a time-saving could be responsible for an extra case per day being completed, representing a more efficient use of operating theatre time.
While this study has shown comparable outcomes between MoC and LC, there is little doubt that there is a perception that laparoscopy represents a lower magnitude of risk than open surgery. Such bias can be dangerous and lead to a lower threshold for surgical intervention in patients with borderline indications. A resultant increase in the volume of cases performed laparoscopically can lead to a paradoxical increase in healthcare costs, even if the costs of individual procedures are lower. The potential for such a trend has been a contentious issue in relation to other laparoscopic procedures, such as anti-reflux surgery [34].
In conclusion, this meta-analysis has shown how the adverse event profile for mini-laparotomy cholecystectomy is equivalent to that following laparoscopic cholecystectomy. It has not been possible to meta-analyse comparative data concerning cost, cosmesis or quality of life and these should be addressed by future studies. While laparoscopic cholecystectomy may be considered to represent the standard of care in first-world medicine, the present meta-analysis suggests that for those healthcare systems where the costs of setting up and maintaining a laparoscopic service are seen as prohibitive, or in those patients in whom laparoscopy is contra-indicated, mini-laparotomy cholecystectomy offers an effective alternative, with similar patient outcomes.
References
Bittner R (2004) The standard of laparoscopic cholecystectomy. Langenbecks Arch Surg 389: 157–163
Zacks SL, Sandler RS, Rutledge R, Brown RS Jr. (2002) A population-based cohort study comparing laparoscopic cholecystectomy and open cholecystectomy. Am J Gastroenterol 97: 334–340
Keskin A (2005) Is laparoscopic cholecystectomy cheaper? Surg Laparosc Endosc Percutan Tech 15: 191–194; discussion 194
Shea JA, Healey MJ, Berlin JA, Clarke JR, Malet PF, Staroscik RN, Schwartz JS, Williams SV (1996) Mortality and complications associated with laparoscopic cholecystectomy. A meta-analysis. Ann Surg 224: 609–620
Basu S, Giri PS, Roy D (2006) Feasibility of same day discharge after mini-laparotomy cholecystectomy – a simulation study in a rural teaching hospital. Can J Rural Med 11: 93–98
Barkun JS, Barkun AN, Sampalis JS, Fried G, Taylor B, Wexler MJ, Goresky CA, Meakins JL (1992) Randomised controlled trial of laparoscopic versus mini cholecystectomy. The McGill Gallstone Treatment Group. Lancet 340: 1116–1119
Harju J, Juvonen P, Eskelinen M, Miettinen P, Paakkonen M (2006) Minilaparotomy cholecystectomy versus laparoscopic cholecystectomy: a randomized study with special reference to obesity. Surg Endosc 20: 583–586
Kunz R, Orth K, Vogel J, Steinacker JM, Meitinger A, Bruckner U, Beger HG (1992) Laparoscopic cholecystectomy versus mini-lap-cholecystectomy. Results of a prospective, randomized study. Chirurg 63: 291–295
Majeed AW, Troy G, Nicholl JP, Smythe A, Reed MW, Stoddard CJ, Peacock J, Johnson AG (1996) Randomised, prospective, single-blind comparison of laparoscopic versus small-incision cholecystectomy. Lancet 347: 989–994
McGinn FP, Miles AJ, Uglow M, Ozmen M, Terzi C, Humby M (1995) Randomized trial of laparoscopic cholecystectomy and mini-cholecystectomy. Br J Surg 82: 1374–1377
McMahon AJ, Russell IT, Baxter JN, Ross S, Anderson JR, Morran CG, Sunderland G, Galloway D, Ramsay G, O’Dwyer PJ (1994) Laparoscopic versus minilaparotomy cholecystectomy: a randomised trial. Lancet 343: 135–138
Secco GB, Cataletti M, Bonfante P, Baldi E, Davini MD, Biasotti B, Ravera G, Ferraris R (2002) Laparoscopic versus mini-cholecystectomy: analysis of hospital costs and social costs in a prospective randomized study. Chir Ital 54: 685–692
Srivastava A, Srinivas G, Misra MC, Pandav CS, Seenu V, Goyal A (2001) Cost-effectiveness analysis of laparoscopic versus minilaparotomy cholecystectomy for gallstone disease. A randomized trial. Int J Technol Assess Health Care 17: 497–502
Ros A, Gustafsson L, Krook H, Nordgren CE, Thorell A, Wallin G, Nilsson E (2001) Laparoscopic cholecystectomy versus mini-laparotomy cholecystectomy: a prospective, randomized, single-blind study. Ann Surg 234: 741–749
Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF (2000) Improving the Quality of Reports of Meta-Analyses of Randomised Controlled Trials: The QUOROM Statement. Onkologie 23: 597–602
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7: 177–188
Mantel N, Haenszel W (1959) Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 22: 719–748
Yusuf S, Peto R, Lewis J, Collins R, Sleight P (1985) Beta blockade during and after myocardial infarction: an overview of the randomized trials. Prog Cardiovasc Dis 27: 335–371
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17: 1–12
Ezzo J, Berman B, Hadhazy VA, Jadad AR, Lao L, Singh BB (2000) Is acupuncture effective for the treatment of chronic pain? A systematic review. Pain 86: 217–225
Egger M, Smith GD (1995) Misleading meta-analysis. BMJ 310: 752–754
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315: 629–634
Lucena JR (2005) Laparoscopic versus mini-laparotomy cholecystectomy. Cir Esp 77: 332–336
Makinen AM, Nordback IH (1995) Cholecystectomy: comparison of minilaparotomy and laparoscopy. Int Surg 80: 99–101
Oyogoa SO, Komenaka IK, Ilkhani R, Wise L (2003) Mini-laparotomy cholecystectomy in the era of laparoscopic cholecystectomy: a community-based hospital perspective. Am Surg 69: 604–607
Supe AN, Bapat VN, Pandya SV, Dalvi AN, Bapat RD (1996) Laparoscopic versus mini-lap cholecystectomy for gallstone disease. Indian J Gastroenterol 15: 94–96
Syrakos T, Antonitsis P, Zacharakis E, Takis A, Manousari A, Bakogiannis K, Efthimiopoulos G, Achoulias I, Trikoupi A, Kiskinis D (2004) Small-incision (mini-laparotomy) versus laparoscopic cholecystectomy: a retrospective study in a university hospital. Langenbecks Arch Surg 389: 172–177
Nilsson E, Ros A, Rahmqvist M, Backman K, Carlsson P (2004) Cholecystectomy: costs and health-related quality of life: a comparison of two techniques. Int J Qual Health Care 16: 473–482
Kratzer W, Mason RA, Kachele V (1999) Prevalence of gallstones in sonographic surveys worldwide. J Clin Ultrasound 27: 1–7
Calvert NW, Troy GP, Johnson AG (2000) Laparoscopic cholecystectomy: a good buy? A cost comparison with small-incision (mini) cholecystectomy. Eur J Surg 166: 782–786
Champault A, Vons C, Dagher I, Amerlinck S, Franco D (2002) Low-cost laparoscopic cholecystectomy. Br J Surg 89: 1602–1607
Ros A, Nilsson E (2004) Abdominal pain and patient overall and cosmetic satisfaction one year after cholecystectomy: outcome of a randomized trial comparing laparoscopic and minilaparotomy cholecystectomy. Scand J Gastroenterol 39: 773–777
McMahon AJ, Ross S, Baxter JN, Russell IT, Anderson JR, Morran CG, Sunderland GT, Galloway DJ, O’Dwyer PJ (1995) Symptomatic outcome 1 year after laparoscopic and minilaparotomy cholecystectomy: a randomized trial. Br J Surg 82: 1378–1382
Finlayson SR, Birkmeyer JD, Laycock WS (2003) Trends in surgery for gastroesophageal reflux disease: the effect of laparoscopic surgery on utilization. Surgery 133: 147–153
Acknowledgments
The authors would like to thank Mr. Alex von Roon, Miss Rosamund Jacklin and Mr. Jesus Muñoz for their invaluable help in translating the foreign language papers included in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Purkayastha, S., Tilney, H.S., Georgiou, P. et al. Laparoscopic cholecystectomy versus mini-laparotomy cholecystectomy: a meta-analysis of randomised control trials. Surg Endosc 21, 1294–1300 (2007). https://doi.org/10.1007/s00464-007-9210-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-007-9210-3