Abstract
Gigaxonin, the product of GAN gene localized to chromosome 16, is associated with the early onset neuronal degeneration disease giant axonal neuropathy (GAN). Gigaxonin is an E3 ubiquitin ligase adaptor protein involved in intermediate filament processing in neural cells, and vimentin filaments in fibroblasts. Mutations of the gene cause pre-neural filaments to accumulate and form giant axons resulting in the inhibition of neural cell signaling. Analysis of the catalog of somatic mutations in cancer, driver DB and IDGC data portal databases containing 21,000 tumor genomic sequences has identified GAN patient mutations in cancer cell lines and primary tumors. The database search has also shown the presence of identical missense and nonsense gigaxonin mutations in GAN and colon cancer. These mutations frequently occur in the domains associated with protein homodimerization and substrate interaction such as Broad-Complex, Tramtrack and Bric a brac (BTB), BTB associated C-terminal KELCH (BACK), and KELCH repeats. Analysis of the International HapMap Project database containing 1200 normal genomic sequences has identified a single nucleotide polymorphism (SNP), rs2608555, in exon 8 of the gigaxonin sequence. While this SNP is present in >40 % of Caucasian population, it is present in less than 10 % of Japanese and Chinese populations. Although the role of gigaxonin polymorphism is not yet known, CFTR and MDR1 gene studies have shown that silent mutations play a role in the instability and aberrant splicing and folding of mRNAs. We believe that molecular and functional investigation of gigaxonin mutations including the exon 8 polymorphism could lead to an improved understanding of the relationship between GAN and cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gigaxonin, also known as KLHL16, is a member of the BTB-KELCH family of proteins and is encoded by the GAN gene on chromosome 16q24 (Cavalier et al. 2000). Mutations of the GAN gene were found to be causative in the rare autosomal recessive neurodegenerative disorder giant axonal neuropathy (GAN, OMIM 256850) (Bomont et al. 2000). GAN is characterized by a progressive neuropathy affecting both sensory and motor nerves in both the central and peripheral nervous systems, and was first described in the 1970 (Asbury et al. 1972; Berg et al. 1972). Patients usually begin manifesting symptoms in childhood, and most patients die by the second or third decade of life (Johnson-Kerner et al. 2014). Histologically, neurons in GAN patients show large axonal accumulations, giving the disorder its name. Although gigaxonin is mutated in GAN, the precise molecular function of this ubiquitous protein is not yet fully understood. The normal physiological role of gigaxonin is in the maintenance of cytoskeletal structure in normal tissues that include processing of intermediate neural filaments in neural cells and vimentin in fibroblasts and endothelial cells (Donaghy et al. 1988; Bomont et al. 2000; Bomont and Koenig 2003; Mahammad et al. 2013). Many studies have shown that gigaxonin is involved in the ubiquitin–proteasome pathway, controlling the degradation of intermediate filaments and other cytoskeletal components (Ding et al. 2002; Allen et al. 2005; Mahammad et al. 2013). Here we summarize what is known about gigaxonin’s role in cellular functions, and point out gigaxonin mutations that may play a role in cancer development.
Gigaxonin and the ubiquitin proteasome complex
Gigaxonin is a 65 kilodalton protein composed of an N-terminal BTB domain followed by six KELCH repeats (Fig. 1). By northern blotting of the mouse tissues, Ding et al. (2002) have found ubiquitous expression of gigaxonin in all tissues, but more so in the brain, heart, and muscle. By western blotting, these authors have confirmed higher gigaxonin protein expression in the brain, heart and muscle. Ganay et al. (2011) have shown higher expression of gigaxonin protein in the tissues of the nervous system and lower expression in muscle, heart, kidney and liver. Differences in the pattern of protein expression in the same tissues could be due to differences in the mouse species studied and/or difference in the antibody used for the expression analysis. Since intermediate filaments are the hallmark of GAN patients, the role of gigaxonin in maintaining the cytoskeleton network has been studied by several investigators. Gigaxonin mutations were found to be associated with the accumulation of vimentin intermediate filaments (IFs), an important IF expressed in mesenchymal cells (Cleveland et al. 2009).
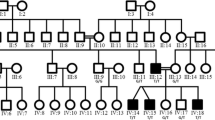
Gigaxonin mutations common to both giant axonal neuropathy (GAN) and cancer patients. a GAN mutations from GAN were compared with GAN mutations in cancers recorded in the catalog of somatic mutations in cancer (COSMIC). There are 9 discovered common mutations between the two pathologies: a single silent mutation is shown in green, 4 missense mutations are shown in blue and 4 nonsense mutations are shown in red. Nucleotide and protein numbers start from the coding region of gigaxonin, 148 bps from the exon 1 start site. Map is not drawn to scale. b Structures of gigaxonin Broad-Complex, Tramtrack and Bric a brac (BTB) and BTB and C-terminal Kelch (BACK) region homo dimer, and actin-binding protein Mayven (KLHL2) Kelch domain were obtained from Research Collaboratory for Structural Bioinformatics Protein Database (RCSB PDB). The predicted full structure was processed on the SWISS-MODEL Repository
Extensive studies have shown that vimentin binding and processing is the major function of gigaxonin in the maintenance of normal cytoskeletal structures (Bomont et al. 2000; Bomont and Koenig 2003; Cleveland et al. 2009; Mahammad et al. 2013). Further, GAN gene replacement studies in vitro using AAV2 viral particles into GAN patient primary skin fibroblasts has shown that gigaxonin is involved in the processing of vimentin intermediate filaments (Mussche et al. 2013). Proteomic studies of the gigaxonin transfected GAN fibroblasts further showed reversal of protein accumulation in 32 proteins and three have previously been shown to be associated with the GAN phenotype.
Dequeen et al. (2008) created a GAN exon 1 deletion mutant mice (GANΔexon1; Δexon1) as a model of the GAN disease. Although these mice contained neural IF defects, accumulation of NF-L filaments, they did not resemble the human disease phenotype of neurodegeneration. Similarly, GAN exon 3–5 deletion mutant mice showed neural cytoskeletal abnormalities and mild motor and sensory defects without neuronal degeneration of the human disease (Ganay et al. 2011). However, intracisternal injection of AAV9/GAN into GAN deletion mutant mice caused a complete clearance of peripherin, an IF aggregate of gigaxonin deficiency clearly pointing out that neural IFs are the direct targets of gigaxonin (Mussche et al. 2013). Another study has also shown normal processing of peripherin and neurofilament NF-L aggregates after GAN gene introduction through lentiviral or stable transgene into 3 different GAN negative-induced pluripotent stem cells (iPSCs) (Johnson-Kerner et al. 2015). This study further pointed out that overexpression of gigaxonin is not toxic to the iPSC motor neurons pointing to the possibility of gene therapeutic studies in GAN patients. The in vitro and in vivo animal model studies have, thus, confirmed the role of gigaxonin as an ubiquitin ligase adapter with a direct impact on the structural integrity and cytoskeletal structure of normal neuronal and non-neuronal cells. Studies have also shown that microtubule related proteins MAP1B, tubulin folding cofactor B (TBCB) and MAP8 to be binding partners of gigaxonin and ubiquitinated by gigaxonin (Wang et al. 2005; Dequeen et al. 2008). However, the in vitro and animal model studies have found that these proteins are not accumulated or microtubule disorganization is not seen in GAN mutant fibroblasts, iPSC derived motor neurons or GAN mutant mice indicating that microtubule disorganization do not play a role in the GAN disease (Cleveland et al. 2009; Ganay et al. 2011; Johnson-Kerner et al. 2015.
The ubiquitin–proteasome system is a highly evolutionarily conserved process critical for protein homeostasis and proper cell function, and involves tagging proteins with multiple ubiquitin molecules and subsequent degradation of the tagged protein via the proteasome complex (Glickman and Ciechanover 2002). The first of these steps, also called ubiquitination, is highly controlled process dependent on three enzymatic activities: ubiquitin activation (E1), conjugation (E2), and ligation (E3) (Furukawa et al. 2003). Malfunction at any step in this complex system can lead to a variety of human diseases, including malignancies, neurodegenerative disorders, immune and inflammatory disorders, and genetic diseases (Glickman and Ciechanover 2002). Allen et al. (2005) have found that gigaxonin binds to the ubiquitin-activating enzyme E1 via its N-terminal BTB domain while its C-terminal kelch domain interacts with the cytoskeletal protein MAP1B-LC, leading to degradation of this protein (Allen et al. 2005).
Gigaxonin in oncogenesis
Multiple genes and proteins involved in neuromuscular disorders have been implicated in the oncogenesis of a variety of human cancers. For example, mutations in mitofusin-2 (MFN2), a mitochondrial protein, were found to be causative of Charcot-Marie-Tooth disease type 2A (Züchner et al. 2004). It was recently found that MFN2 is a key player in the cell cycle and cell invasion in lung adenocarcinoma (Lou et al. 2015). Similarly, Parkin, a mitochondrial protein is shown to be involved in the development of Parkinson’s disease as well as in human cancers (Shimura et al. 2000; Matsuda et al. 2015. Therefore, given the role of gigaxonin in the ubiquitin proteasome complex, it is possible that it could play a role in oncogenesis. A recent study by Veena et al. (2014) found that gigaxonin directly interacts with NF-κB, and this interaction is dependent on the interaction between p16, also known as cyclin-dependent kinase inhibitor 2A (CDKN2A). It is well known that p16 is an important tumor suppressor gene that renders cancer cells susceptible to cisplatin treatment (Veena et al. 2014). The putative role of gigaxonin in this interaction is that it helps the ubiquitination of p16 bound NF-κB, and thus the downregulation of NF-κB in turn makes tumors more susceptible to cisplatin treatment (Fig. 2). It is also possible that patients with one mutated copy of gigaxonin may not exhibit GAN, but may be more susceptible to cancer development if the ubiquitin pathway is affected by the heterozygous gigaxonin mutations.
Presence of gigaxonin mutations in cancer
Although gigaxonin mutations were originally discovered by their involvement in GAN, many cancers contain similar mutations (Fig. 1a). The reported gigaxonin mutations are spread throughout the protein structure but all result in similar symptoms of giant axonal neuropathy (Supplementary Table 1) (Boizot et al. 2014; Johnson-Kerner et al. 2014). Through postmortem pathology, a wide range of central nervous system degeneration was shown to be caused by these mutations (Johnson-Kerner et al. 2014).
Although gigaxonin mutations are seen throughout the protein, mutations are also found clustered in the BTB-BACK domain of the protein (15/54: 28 %), which could result in instability and impairment of homodimerization (Supplementary Table 1; Fig. 1b) (Cullen et al. 2004; Boizot et al. 2014). Without the ability to homodimerize, gigaxonin loses its function as an ubiquitin ligase adaptor. It has been shown that gigaxonin expression is severely decreased in these patients due to mRNA and protein instability. Further, Boizot et al. (2014) using 3D models of GAN mutations has suggested that mRNA instability could be due to nonsense-mediated decay and protein instability is related to impaired folding of the BTB-KELCH domain and instability in the binding of gigaxonin to substrates or cullin-E3 ligase. These studies, therefore, point out that nonsense and missense mutations play an important role in the functional inactivation of gigaxonin.
Although most prominent in neural cells, gigaxonin mutations are observed in several primary human cancers. There are 95 recorded cases of gigaxonin mutations in 19626 unique samples of cancer in the Catalog of Somatic Mutations in Cancer (COSMIC) database and these mutations can be found in http://cancer.sanger.ac.uk/cosmic/gene/analysis?ln=GAN#histo. These mutations are mostly localized to the large intestine (colon cancer), stomach, endometrium, lung, and skin tumors (Table 1). Although there are common mutations in GAN and cancers, there are missense and nonsense mutations found only in cancer patients (Supplementary Table 1). Most of these mutations occur in the BTB-KELCH region in exons 3–5 and 8–11 similar to the mutations in GAN. However, studies are not available relating these mutations to the gigaxonin function of IF degradation seen in GAN patients.
The COSMIC cell line mutations for the GAN gene can also be found at: http://cancer.sanger.ac.uk/cell_lines/gene/analysis?ln=GAN#hist. Of the tissues that have over 40 cell lines in COSMIC, the most common tissues are in cell lines of the bone (6.82 %), large intestine (14.28 %), hematopoietic/lymphoid (5.14 %) and lung tumors (2.79). These cell line and primary tumor mutations show that mesenchymal cells are more frequently mutated in cancer cells. Transcription studies of the Broad Institute Cancer Cell Line Encyclopedia (http://www.broadinstitute.org/ccle/home) have shown that gigaxonin mRNA is highly expressed in the cancers of the intestine, breast, and lung. It is interesting to note that the tissues with the highest mutation frequencies are also the tissues with highest expression of gigaxonin.
Of the nine common gigaxonin mutations present in GAN and cancer in the Cosmic database, large intestine was the primary tissue location of a missense mutation and all 4 nonsense mutations (Table 2). The other tissue of interest seems to be endometrium with two missense mutations. Complete transcriptional profile available for large intestinal cancer cell lines KM12 and DLD-1 containing GAN mutations (exon 4 nonsense mutations in KM12 cells and exon 1 missense mutation in DLD-1 cells) has shown gigaxonin expression to be in the average range (Table 3). While DLD-1 cells show diminished expression of CDKN2A and VIM genes pointing to a direct relationship between the expression of gigaxonin and CDKN2A and VIM genes, KM12 cells show an increased expression of CDKN2A and VIM genes indicating an inverse relationship to gigaxonin expression (Klijn et al. 2015). Further, the presence of GAN mutations (Table 2) in addition to the well-known overexpression of vimentin in colon cancers (Satelli and Li 2011; Todosi et al. 2012) indicate that a detailed analysis of genomic status and expression of gigaxonin is required to delineate the significance, if any, of GAN mutations to the development of colon cancer.
Analysis of two other databases, Driver-DB (http://driverdb.tms.cmu.edu.tw/driverdbv2/gene_data_p.php?genename=GAN&geneproteinid=&submit=submit and ICGC Data Portal (https://dcc.icgc.org/genes/ENSG00000261609) have shown GAN mutations in 247 cancer samples (Supplementary Table 2). Location of these mutations in the different tumor samples is summarized in Table 4. In this dataset, liver tumors show the highest number (73) of nonsense (stop codon) mutations. These mutations are present mostly in exons 4, 7 and 9–11 with an indication that preponderance of these mutations are at the c-terminus of the protein. Missense mutations are found in skin (13), lung, head and neck and stomach (12 each), uterus (11), colorectal (10), breast, cervix and pancreas and gall bladder (7 each), kidney (6), ovary and bladder (5 each), cervix and pancreas (5 each), CNS (4) and in prostate (3) cancers. Silent mutations are present in 13 uterine and 9 head and neck cancers. While colon cancer had the highest number of mutations in the cosmic database, the driver-DB and ICDC data portal show the highest number of mutations in the liver cancer.
Function of gigaxonin protein has also been linked to the ubiquitination of NF-κB in cisplatin-induced senescence of cancer cells (Fig. 2). The results suggested that gigaxonin could be involved in the regulation of NF-κB in normal cell cycle. As human cancers are affected by the activation of NF-κB, the absence of NF-κB degradation due to gigaxonin mutations could lead to NF-κB-mediated oncogenic signaling in cancer cells. While cellular phenotypes are vastly different in GAN and cancer, it remains to be seen whether gigaxonin mutations cause vimentin IF aggregation in cancer cells (O’Neill and Kaltschmidt 1997). What is known is overexpression of vimentin in chemo-radiation resistant cancer cells indicating the possibility that gigaxonin indeed might be playing a role in the regulation of vimentin expression during normal cell growth and development. Similarly, maintenance of transcriptional regulation by gigaxonin could be important for the prevention of tumor development. Investigation of gigaxonin mutations using in vitro cell line and xenograft animal tumor models will, therefore, be valuable for the elucidation of gigaxonin function in normal cell growth and development.
Exon 8 polymorphism, rs2608555, in the general population
HapMap studies have identified a number of intronic mutations of the gigaxonin genomic sequence in the normal population. However, only a single silent mutation, rs2608555 or c.1293C>T, is reported for the exonic sequence of the gigaxonin genome. This polymorphism exists in 22 % of the world population ranging from ~3 to 52 % in different populations (Table 5). The Caucasian population has the highest frequency (44.25 %) and the native Chinese population has the lowest frequency (2.75 %) of this polymorphism.
Veena et al. have shown that expression of gigaxonin and p16 is related to the ubiquitination of NF-κB. While p16 is inactivated through mutations and promotor hypermethylations, GAN gene contains mutations and c. 1293C>T polymorphism (silent mutation) in GAN patients (Bomont et al. 2000). Some GAN patients carrying the silent mutation could have normal gigaxonin mRNA levels possibly due to transcription upregulation of the other mutant allele as observed in patients carrying compound nonsense or deletion mutations (Boizot et al. 2014). We, therefore, hypothesize that the stability of the mRNA could depend on RNA binding miRNAs and/or secondary structures (Gao et al. 2013; Werk et al. 2014). While the polymorphism is currently assumed to be benign, it could play a role in mRNA folding and stability leading to differential expression in cancer cells.
The study of Bomont et al. (2000) has shown that the gene is inactivated by heterozygous allelic mutations in many GAN patients. In two patients, they have reported a missense mutation and c. 1293C>T polymorphism. They have also shown that heterozygous alleles are present in one of these samples. It is likely therefore that in addition to the missense mutation, c. 1293C>T polymorphism plays a role in the functional inactivation of the GAN gene. Therefore, investigation of GAN c. 1293C>T polymorphism in cancer is warranted to determine whether a relationship exists between GAN polymorphism and chemosensitivity and/or tumor aggressiveness.
Examples of silent mutations and mRNA instability include silent mutations in cystic fibrosis that exhibit mRNA instability and aberrant splicing due to c.2811G>T polymorphism in exon 15 of the CFTR (cystic fibrosis transmembrane conductance regulator) gene (Faa’ et al. 2010). There are also silent polymorphisms in the Multidrug Resistance 1 (MDR1) gene known to affect the mRNA folding (Kimchi-Sarfaty et al. 2007). A single change in the mRNA alters its folding thereby preventing cytoplasmic translocation and translation. Thus, we believe that in vitro studies need to be performed to investigate the role of exon 8 polymorphism of the GAN gene in RNA stability and tumor development. Details of the GAN single nucleotide polymorphism (SNP) rs2608555 including its chromosomal location can be found at: http://www.ncbi.nlm.nih.gov/projects/SNP/snp_ref.cgi?rs=2608555.
Conclusion
Gigaxonin, an E3 ligase adaptor protein, is shown to be involved in the processing of neural intermediate filaments in neurons and cytoskeletal proteins such as vimentin in fibroblasts. The protein has also been found to be involved in the degradation of proteins such as NF-κB. These studies demonstrate that gigaxonin plays a crucial role in cell cycle growth and cytoskeletal homeostasis. Therefore, the inactivation of gigaxonin through mutations would result in unrestricted growth signaling leading to unrestricted cell growth. There is also an exonic polymorphic mutation that is prevalent in the Caucasian population which may play a role in the development of neural diseases and/or cancers in this population. The direct relationship in the reduced expression of p16 and gigaxonin in cancer cell lines suggests that the two genes might be co-regulated in the regulation of the cell cycle. Since p16 expression is related to senescence of aging cells, it is likely that gigaxonin expression might also be elevated leading to reduced growth of cells in the aging individuals. We could hypothesize therefore that gigaxonin mutation profile and/or expression could be a diagnostic marker of a subset of cancers that might have reduced p16 expression. Finally, p16 expression being used as a surrogate marker of HPV positivity and chemo-radiation sensitivity, we believe that gigaxonin expression could be added to this list of cancer diagnostic markers.
References
Abaan OD, Polley EC, Davis SR, Zhu YJ, Bilke S, Walker RL, Pineda M, Gindin Y, Jiang Y, Reinhold WC, Holbeck SL, Simon RM, Doroshow JH, Pommier Y, Meltzer PS (2013) The exomes of the NCI-60 panel: a genomic resource for cancer biology and systems pharmacology. Cancer Res 73:4372–4382. doi:10.1158/0008-5472.CAN-12-3342 (Epub 2013 Jul 15)
Allen E, Ding J, Wang W, Pramanik S, Chou J, Yau V, Yang Y (2005) Gigaxonin-controlled degradation of MAP1B light chain is critical to neuronal survival. Nature 438:224–228 (Epub 2005 Oct 16)
Asbury AK, Gale MK, Cox SC, Baringer JR, Berg BO (1972) Giant axonal neuropathy—a unique case with segmental neurofilamentous masses. Acta Neuropathol 20:237–247
Berg BO, Rosenberg SH, Asbury AK (1972) Giant axonal neuropathy. Pediatrics 49:894–899
Boizot A, Talmat-Amar Y, Morrogh D, Kuntz NL, Halbert C, Chabrol B, Houlden H, Stojkovic T, Schulman BA, Rautenstrauss B, Bomont P (2014) The instability of the BTB-KELCH protein gigaxonin causes giant axonal neuropathy and constitutes a new penetrant and specific diagnostic test. Acta Neuropathol Commun 2:47. doi:10.1186/2051-5960-2-47
Bomont P, Koenig M (2003) Intermediate filament aggregation in fibroblasts of giant axonal neuropathy patients is aggravated in non dividing cells and by microtubule destabilization. Hum Mol Genet 12:813–822
Bomont P, Cavalier L, Blondeau F, Ben Hamida C, Belal S, Tazir M, Demir E, Topaloglu H, Korinthenberg R, Tüysüz B, Landrieu P, Hentati F, Koenig M (2000) The gene encoding gigaxonin, a new member of the cytoskeletal BTB/kelch repeat family, is mutated in giant axonal neuropathy. Nat Genet 26:370–374 (PMID: 11062483)
Cavalier L, BenHamida C, Amouri R, Belal S, Bomont P, Lagarde N, Gressin L, Callen D, Demir E, Topaloglu H, Landrieu P, Ioos C, Hamida MB, Koenig M, Hentati F (2000) Giant axonal neuropathy locus refinement to a <590 kb critical interval. Eur J Hum Genet 8:527–534
Cleveland DW, Yamanaka K, Bomont P (2009) Gigaxonin controls vimentin orGANization through a tubulin chaperone-independent pathway. Hum Mol Genet 18:1384–1394. doi:10.1093/hmg/ddp044 (Epub 2009 Jan 24)
Cullen VC, Brownlees J, Banner S, Anderton BH, Leigh PN, Shaw CE, Miller CC (2004) Gigaxonin is associated with the Golgi and dimerises via its BTB domain. NeuroReport 15:873–876 (PMID: 15073534)
Demir E, Bomont P, Erdem S, Cavalier L, Demirci M, Kose G, Muftuoglu S, Cakar AN, Tan E, Aysun S, Topcu M, Guicheney P, Koenig M, Topaloglu H (2005) Giant axonal neuropathy: clinical and genetic study in six cases. J Neurol Neurosurg Psychiatry 76:825–832 (PMID: 15897506)
Dequen F, Bomont P, Gowing G, Cleveland DW, Julien JP (2008) Modest loss of peripheral axons, muscle atrophy and formation of brain inclusions in mice with targeted deletion of gigaxonin exon 1. J Neurochem 107:253–264. doi:10.1111/j.1471-4159.2008.05601.x (Epub 2008 Jul 31. PMID: 18680552)
Ding J, Liu JJ, Kowal AS, Nardine T, Bhattacharya P, Lee A, Yang Y (2002) Microtubule-associated protein 1B: a neuronal binding partner for gigaxonin. J Cell Biol 158:427–433 (Epub 2002 Jul 29)
Donaghy M, King RH, Thomas PK, Workman JM (1988) Abnormalities of the axonal cytoskeleton in giant axonal neuropathy. J Neurocytol 17:197–208
Faa′ V, Coiana A, Incani F, Costantino L, Cao A, Rosatelli MC (2010) A synonymous mutation in the CFTR gene causes aberrant splicing in an italian patient affected by a mild form of cystic fibrosis. J Mol Diag 12:380–383. doi:10.2353/jmoldx.2010.090126 (Epub 2010 Feb 26)
Furukawa M, He YJ, Borchers C, Xiong Y (2003) Targeting of protein ubiquitination by BTB-Cullin 3-Roc1 ubiquitin ligases. Nat Cell Biol 5:1001–1007 (Epub 2003 Oct 5)
Ganay T, Boizot A, Burrer R, Chauvin JP, Bomont P (2011) Sensory-motor defecits and neurofilament disorGANization in gigaxonin-null mice. Mol Neurodegener 12(6):25
Gao F, Ihn HE, Medina MW, Krauss RM (2013) A common polymorphism in the LDL receptor gene has multiple effects on LDL receptor function. Hum Mol Genet 22:1424–1431. doi:10.1093/hmg/dds559 (Epub 2013 Jan 7)
Giannakis M, Hodis E, Jasmine MuX, Yamauchi M, Rosenbluh J, Cibulskis K, Saksena G, Lawrence MS, Qian ZR, Nishihara R, Van Allen EM, Hahn WC, Gabriel SB, Lander ES, Getz G, Ogino S, Fuchs CS, Garraway LA (2014) RNF43 is frequently mutated in colorectal and endometrial cancers. Nat Genet 46:1264–1266. doi:10.1038/ng.3127 (Epub 2014 Oct 26)
Glickman MH, Ciechanover A (2002) The ubiquitin-proteasome proteolytic pathway: destruction for the sake of construction. Physiol Rev 82:373–428 (PMID: 11917093)
Johnson-Kerner BL, Roth L, Greene JP, Wichterle H, Sproule DM (2014) Giant axonal neuropathy: an updated perspective on its pathology and pathogenesis. Muscle Nerve 50:467–476. doi:10.1002/mus.24321
Johnson-Kerner BL, Ahmad FS, Diaz AG, Greene JP, Gray SJ, Samulski RJ, Chung WK, Van Coster R, Maertens P, Noggle SA, Henderson CE, Wichterle H (2015) Intermediate filament protein accumulation in motor neurons derived from giant axonal neuropathy iPSCs rescued by restoration of gigaxonin. Hum Mol Genet 24:1420–1431. doi:10.1093/hmg/ddu556 (Epub 2014 Nov 4)
Kimchi-Sarfaty C, Oh JM, Kim IW, Sauna ZE, Calcagno AM, Ambudkar SV, Gottesman MM (2007) A “silent” polymorphism in the MDR1 gene changes substrate specificity. Science 315:525–528 (Epub 2006 Dec 21)
Klijn C, Durinck S, Stawiski EW, Haverty PM, Jiang Z, Liu H, Degenhardt J, Mayba O, Gnad F, Liu J, Pau G, Reeder J, Cao Y, Mukhyala K, Selvaraj SK, Yu M, Zynda GJ, Brauer MJ, Wu TD, Gentleman RC, Manning G, Yauch RL, Bourgon R, Stokoe D, Modrusan Z, Neve RM, de Sauvage FJ, Settleman J, Seshagiri S, Zhang Z (2015) A comprehensive transcriptional portrait of human cancer cell lines. Nat Biotechnol 33:306–312. doi:10.1038/nbt.3080 (Epub 2014 Dec 8)
Kohsaka S, Shukla N, Ameur N, Ito T, Ng CK, Wang L, Lim D, Marchetti A, Viale A, Pirun M, Socci ND, Qin LX, Sciot R, Bridge J, Singer S, Meyers P, Wexler LH, Barr FG, Dogan S, Fletcher JA, Reis-Filho JS, Ladanyi M (2014) A recurrent neomorphic mutation in MYOD1 defines a clinically aggressive subset of embryonal rhabdomyosarcoma associated with PI3K-AKT pathway mutations. Nat Genet 46:595–600. doi:10.1038/ng.2969 (Epub 2014 May 4)
Koop O, Schirmacher A, Nelis E, Timmerman V, De Jonghe P, Ringelstein B, Rasic VM, Evrard P, Gärtner J, Claeys KG, Appenzeller S, Rautenstrauss B, Hühne K, Ramos-Arroyo MA, Wörle H, Moilanen JS, Hammans S, Kuhlenbäumer G (2007) Genotype-phenotype analysis in patients with giant axonal neuropathy (GAN). Neuromuscul Disord 17:624–630 (Epub 2007 Jun 22)
Kuhlenbäumer G, Young P, Oberwittler C, Hünermund G, Schirmacher A, Domschke K, Ringelstein B, Stögbauer F (2002) Giant axonal neuropathy (GAN): case report and two novel mutations in the gigaxonin gene. Neurology 58:1273–1276 (PMID: 11971098)
Lou Y, Li R, Liu J, Zhang Y, Zhang X, Jin B, Liu Y, Wang Z, Zhong H, Wen S, Han B (2015) Mitofusin-2 over-expresses and leads to dysregulation of cell cycle and cell invasion in lung adenocarcinoma. Med Oncol 32:132. doi:10.1007/s12032-015-0515-0 (Epub 2015 Mar 22)
Mahammad S, Murthy SN, Didonna A, Grin B, Israeli E, Perrot R, Bomont P, Julien JP, Kuczmarski E, Opal P, Goldman RD (2013) Giant axonal neuropathy-associated gigaxonin mutations impair intermediate filament protein degradation. J Clin Invest 123:1964–1975. doi:10.1172/JCI66387 (Epub 2013 Apr 15)
Matsuda S, Nakanishi A, Minami A, Wada Y, Kitagishi Y (2015) Functions and characteristics of PINK1 and Parkin in cancer. Front Biosci (landmark Ed.) 20:491–501 (PMID: 25553463)
Mouradov D, Sloggett C, Jorissen RN, Love CG, Li S, Burgess AW, Arango D, Strausberg RL, Buchanan D, Wormald S, O’Connor L, Wilding JL, Bicknell D, Tomlinson IP, Bodmer WF, Mariadason JM, Sieber OM (2014) Colorectal cancer cell lines are representative models of the main molecular subtypes of primary cancer. Cancer Res 74:3238–3247. doi:10.1158/0008-5472.CAN-14-0013 (Epub 2014 Apr 22)
Mussche S, Devreese B, Nagabhushan Kalburgi S, Bachaboina L, Fox JC, Shih HJ, Van Coster R, Samulski RJ, Gray SJ (2013) Restoration of cytoskeleton homeostasis after gigaxonin gene transfer for giant axonal neuropathy. Hum Gene Ther 24:209–219. doi:10.1089/hum.2012.107
Muzny DM, Bainbridge MN, Chang K, Dinh HH, Drummond JA, Fowler G, Kovar CL, Lewis LR, Morgan MB, Newsham IF, Reid JG, Santibanez J, Shinbrot E, Trevino LR, Wu YQ, Wang M, Gunaratne P, Donehower LA, Creighton CJ, Wheeler DA, Gibbs RA, Lawrence MS, Voet D, Jing R, Cibulskis K, Sivachenko A et al (2012) Cancer Genome Atlas Network. Comprehensive molecular characterization of human colon and rectal cancer. Nature 487:330–337. doi:10.1038/nature11252
O’Neill LA, Kaltschmidt C (1997) NF-kappa B: a crucial transcription factor for glial and neuronal cell function. Trends Neurosci 20:252–258 (PMID: 9185306)
Satelli A, Li S (2011) Vimentin in cancer and its potential as a molecular target for cancer therapy. Cell Mol Life Sci 68:3033–3046
Shimura H, Hattori N, Si Kubo, Mizuno Y, Asakawa S, Minoshima S, Shimizu N, Iwai K, Chiba T, Tanaka K, Suzuki T (2000) Familial Parkinson disease gene product, parkin, is a ubiquitin-protein ligase. Nat Genet 25:302–305 (PMID: 10888878)
Todosi AM, Gavrilescu MM, Anitei GM, Filip B, Scripcariu V (2012) Colon cancer at the molecular level—usefulness of epithelial mesenchymal transition analysis. Rev Med Chir Soc Med Nat Iasi 116:1106–1111
Veena MS, Wilken R, Zheng JY, Gholkar A, Venkatesan N, Vira D, Ahmed S, Basak SK, Dalgard CL, Ravichandran S, Batra RK, Kasahara N, Elashoff D, Fishbein MC, Whitelegge JP, Torres JZ, Wang MB, Srivatsan ES (2014) p16 Protein and gigaxonin are associated with the ubiquitination of NFκB in cisplatin-induced senescence of cancer cells. J Biol Chem 289:34921–34937. doi:10.1074/jbc.M114.568543 (Epub 2014 Oct 20)
Wang W, Ding J, Allen E, Zhu P, Zhang L, Vogel H, Yang Y (2005) Gigaxonin interacts with tubulin folding cofactor B and controls its degradation through the ubiquitin-proteasome pathway. Curr Biol 15:2050–2055 (PMID: 16303566)
Werk AN, Bruckmueller H, Haenisch S, Cascorbi I (2014) Genetic variants may play an important role in mRNA-miRNA interaction: evidence for haplotype-dependent downregulation of ABCC2 (MRP2) by miRNA-379. Pharmacogenet Genomics 24:283–291. doi:10.1097/FPC.0000000000000046
Züchner S, Mersiyanova IV, Muglia M, Bissar-Tadmouri N, Rochelle J, Dadali EL, Zappia M, Nelis E, Patitucci A, Senderek J, Parman Y, Evgrafov O, Jonghe PD, Takahashi Y, Tsuji S, Pericak-Vance MA, Quattrone A, Battaloglu E, Polyakov AV, Timmerman V, Schröder JM, Vance JM (2004) Mutations in the mitochondrial GTPase mitofusin 2 cause Charcot-Marie-Tooth neuropathy type 2A. Nat Genet 36:449–451 (Epub 2004 Apr 4)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Data sharing
Authors are willing to share the data with the scientific community.
Funding
The study was supported by funds from VAGLAHS, West Los Angeles Surgical Education Research Center, UCLA Academic Senate Grants (M. B. Wang), and Merit grant from the Veterans Administration, Washington, D.C. (E. S. Srivatsan).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kang, J.J., Liu, I.Y., Wang, M.B. et al. A review of gigaxonin mutations in giant axonal neuropathy (GAN) and cancer. Hum Genet 135, 675–684 (2016). https://doi.org/10.1007/s00439-016-1659-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00439-016-1659-5