Abstract
Left ventricular hypertrophy is a risk factor for cardiovascular morbidity and mortality. Hypertrophic cardiomyopathy (HCM) is considered a model disease to study causal molecular factors underlying isolated cardiac hypertrophy. However, HCM manifests with various clinical symptoms, even in families bearing the same genetic defects, suggesting that additional factors contribute to hypertrophy. The gene encoding the cardiac myosin binding protein C (cMYBPC) is one of the most frequently implicated genes in HCM. Recently another myosin binding protein, myosin binding protein H (MYBPH) was shown to function in concert with cMYBPC in regulating cardiomyocyte contraction. Given the similarity in sequence, structure and the critical role MYBPH plays in sarcomere contraction, we proposed that MYBPH may be involved in HCM pathogenesis. Family-based genetic association analysis was employed to investigate the contribution of MYBPH in modifying hypertrophy. Seven single nucleotide polymorphisms and haplotypes in MYBPH were investigated for hypertrophy modifying effects in 388 individuals (27 families), in which three unique South African HCM-causing founder mutations (p.R403W and pA797T in β-myosin heavy chain gene (MYH7) and p.R92W in the cardiac troponin T gene (TNNT2)) segregate. We observed a significant association between rs2250509 and hypertrophy traits in the p.A797TMYH7 mutation group. Additionally, haplotype GGTACTT significantly affected hypertrophy within the same mutation group. MYBPH was for the first time assessed as a candidate hypertrophy modifying gene. We identified a novel association between MYBPH and hypertrophy traits in HCM patients carrying the p.A797TMYH7 mutation, suggesting that variation in MYBPH can modulate the severity of hypertrophy in HCM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Left ventricular hypertrophy (LVH) is a major risk factor for cardiovascular morbidity and mortality (Lorell and Carabello 2000; Frey and Olson 2003), and understanding the mechanisms influencing its development and identifying high-risk markers for the development of extensive hypertrophy is of importance, as it may lead to improved management and timeous therapeutic intervention in susceptible individuals. Hypertrophic cardiomyopathy, an inherited disease with cardiac hypertrophy as its cardinal, but variable feature, is often considered a model disease for studying the mechanisms underlying hypertrophy.
HCM presents with various phenotypes and clinical symptoms, even in families bearing the same genetic defects (Thierfelder et al. 1994). Currently, more than 1300 mutations in at least 13 genes encoding sarcomere or sarcomere-related proteins have been implicated in HCM (Marian and Roberts 2001; Ho 2010; Seidman and Seidman 2011; Maron et al. 2014; Ho et al. 2015). Thorough screening of known HCM-causing genes typically identifies causal mutations in only 50–60 % of cases, implying that as-yet unknown genes contribute to the patho-aetiology of the condition (Girolami et al. 2006). Moreover, there is a great deal of phenotypic variability in individuals harbouring the same causal mutation, suggesting that the phenotype is modified by other genetic factors (Marian 2002). These modifier genes are known to affect the severity of the phenotype, including cardiac hypertrophy (Marian et al. 1993; Lechin et al. 1995; van der Merwe et al. 2008; Su et al. 2014).
The gene encoding cardiac myosin binding protein C (cMYBPC) is one of the most frequently implicated genes in HCM. However, the role of another member of the myosin binding protein family, myosin binding protein H (MYBPH) is poorly understood. It has recently been shown that MYBPH functions in concert with cMYBPC in regulating cardiomyocyte contraction in response to β-adrenergic stress (Mouton et al. 2014). Individual knockdown of either MYBPH or cMYBPC had little effect on cardiomyocyte contraction, while concurrent knockdown significantly reduced the ability of the cells to contract. MYBPH and cMYBPC were shown to functionally compensate for one another and play critical roles in cardiomyocyte contraction.
Therefore, given the similarity between cMYBPC and MYBPH in sequence homology and structure and the important role that MYBPH plays in cardiomyocyte contraction, we proposed that MYBPH, like cMYBPC, may be involved in HCM pathogenesis. Although, to date, no disease-causing mutation has been found in MYBPH, we hypothesized that variants in MYBPH may still play a role in modifying the hypertrophic phenotype. Here, we tested this theory using a family-based genetic association analysis approach in South African HCM families bearing founder HCM-causing mutations.
Materials and methods
Compliance with ethical standards
The Ethical Review Committee of the Faculty of Health Science at Stellenbosch University, South Africa, (N04/C3/062) granted institutional approval for this study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Study participants
A panel of 115 South African HCM unrelated probands, who were consecutively recruited from Tygerberg Hospital in the Western Cape, South Africa, or were referred to us from elsewhere, were previously screened for mutations in 11 sarcomeric genes. This led to the identification of 27 probands, each harbouring one of three South African HCM founder mutations, namely p.R403W and p.A797T in the β-myosin heavy chain gene (MYH7) and p.R92W in the cardiac troponin T gene (TNNT2) (Moolman-Smook et al. 1999). Family members of these 27 probands were subsequently recruited into the study. The final cohort comprised of 388 genetically and clinically affected and unaffected individuals older than 18 years, of self-reported Caucasian or Mixed Ancestry descent, in which at least one of the three South African HCM founder mutations were found.
Clinical evaluation
All participating individuals were clinically characterized by an experienced echocardiographer who was blinded to patient’s mutation carrier status. Inter-observer variability was excluded since all echocardiography measurements were taken by the same individual at the same core facility located at Tygerberg Hospital. Intra-observer variability was calculated to be less than 5 % (data not shown). M-mode, transthoracic two-dimensional (2D) echocardiography and Doppler imaging were performed. Echocardiograms were analysed using measurement conventions as outlined in the American Society of Echocardiography (ASE) (Schiller et al. 1989) for the assessment of patients with HCM, as previously described (Revera et al. 2008).
Ventricular wall thickness [maximal left ventricular wall thickness (mLVWT), maximal posterior wall thickness (mPWT) and maximal intraventricular septum thickness (mIVST)] were assessed by 16 2D-echocardiographic measurements taken at the mitral valve-, papillary muscle- and supra-apex levels as previously described (Revera et al. 2008). Additionally, medical history and additional cofounders for cardiac hypertrophy, such as age, sex, body surface area (BSA), heart rate (HR), and arterial blood pressure, were recorded for each individual. These basic characteristics of the study cohort are summarized in Table 1. When participants had blood pressure of more than 140 and 90 mmHg systolic and diastolic pressure, respectively, or were being treated for hypertension, they were considered hypertensive.
SNP selection
Single nucleotide polymorphisms (SNPs) spanning MYBPH were selected using the SNPbrowserTM v4.1 software (De La Vega et al. 2006). SNPs were selected to achieve an even coverage of 0.5 LD Units (LDUs) in the HapMap CEU and YRI populations. Markers were further prioritized with a minor allele frequency (MAF) of ≥0.05 (De La Vega 2007). Details of the SNPs selected for genotyping are presented in Table 2.
SNP genotyping and allelic discrimination
DNA was extracted from peripheral blood lymphocytes using an previously described method (Corfield et al. 1993) and used for genotyping of the selected SNPs. Genotyping was performed using PCR-based KASP™ genotyping (KBiosiences; LGC Genomics Ltd., Hertz, UK). The software programme SNPviewer2 v3.2.2.16, supplied by LGC KBiosciences was used for allele discrimination and viewing of allelic discrimination plots.
Statistical analysis
Mendelian inheritance within families was checked with Pedstats v6.11 (Wigginton and Abecasis 2005) and genotyping inconsistencies were resolved by regenotyping. Haploview v4.2 (Barrett et al. 2005) was used to assess the genotyping efficiency of SNPs for all the individuals for whom DNA was available, as well as Hardy–Weinberg equilibrium (HWE), LD, and allele frequencies in selected groups of 40 maximally informative unrelated individuals. Since our cohort consisted of complex families with multiple generations, the same unrelated individuals were not always selected, and for those sets, we report medians from 100 consecutive runs. The most probable fully typed maternal and paternal haplotype pairs for each individual were inferred.
As it is challenging to find a single echocardiographic measure that can accurately quantify the extent of hypertrophy in all HCM patients, since the hypertrophy phenotype observed in HCM patients is extremely variable in terms of extent as well as location, and as echocardiographically defined LVM is not an accurate measure of hypertrophy given its geometric assumptions, we chose to use mLVWT and PC1 (first principal component). PC1 is a principal component score outcome variable, viz., the weighted average of 16 transformed wall thickness measurements. PC1 takes into account the variability in distribution, and extent of hypertrophy between patients in the cohort, in all 16 measurements combined, and accounts for approximately 75 % of overall hypertrophy variability. The percentage contribution of genetic components to the variability of each measured trait was very highly significant (p < 0.001), after adjusting for confounders (data not shown).
Genetic association between each variant and haplotype, and both of these hypertrophy traits were analysed with a specialized mixed-effects linear model. SNP associations were assessed on 256 individuals as clinical information were not available for all 388 individuals. SNPs or haplotypes were assessed as fixed effects in the models. SNPs were coded 0, 1, or 2, according to the number of minor alleles (the so-called additive allelic or allelic dose–response model). Haplotypes were coded in a similar way to the SNPs, i.e. the number of copies (0, 1 or 2) of each specific haplotype carried by the individual. This model enabled us to correct for the degree of relatedness and corresponding higher correlation in inherited traits between pairs of individuals, using kinship coefficients for random effects. A per family (shared environment) random effect corrects for trait correlation resulting from a possible shared environment.
Due to the heterogeneity of the HCM phenotype, the distribution of trait values is not normally distributed. Any deviation from the normal distribution of trait values affect the outcome of the analysis, since statistical models for association analysis of quantitative traits assume normal distribution of trait values (Lange et al. 2002; Diao and Lin 2006). Trait values were, therefore, transformed to approximate normality (Pilia et al. 2006) prior to statistical analysis, to ensure the validity of assumptions underlying the models.
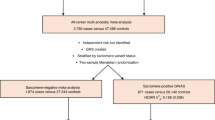
All analyses were adjusted for covariates that are known to modulate cardiac hypertrophy, by including them in the model as fixed effects. Mutation carriers are not associated with a distinct HCM phenotype; however, mutation carrier status and the identity of the HCM-causing founder mutations, viz., p.R92W in TNNT2, p.R403W and p.A797T in MYH7 were adjusted for. Furthermore, our pedigree-based mixed-effects linear models simultaneously adjusted for hypertension (including treatment for hypertension), mean arterial blood pressure, sex, age, ethnicity, BSA, and HR (as a proxy measure for tachycardia). We adjusted for age, since disease severity and progression of disease may occur independent of the timing of assessment. Association within mutation groups was assessed by including the interaction between mutation group and genetic factor in the models as fixed effects. These models provide all p values reported. Effect sizes were estimated by modelling raw, untransformed, (non-quantile normalized) trait values, to estimate the effect sizes in clinically meaningful units of measurement. Fixed effects included self-reported ethnicity to control for population stratification and random effects included individual-specific random effects (kinship coefficients measure relatedness) and family random effects, allowing for testing associations within and between families, all of which would also help to adjust for population structure (Price et al. 2010). Specifically, 82 individuals were included in the analyses purely to establish the degree of relatedness between all individuals; 256 related individuals were used for association testing, and 40 maximally informative unrelated individuals were selected for estimation of minor allele frequencies, and HWE and LD analyses.
Simwallk v2.91 (Sobel and Lange 1996) was used to infer the most probable fully typed maternal and paternal haplotype pairs for each individual. Genetic association between the SNPs and haplotypes and the hypertrophic phenotypes were assessed with specialized pedigree mixed-effects linear models using functions from R packages coxme v2.2-3 (http://CRAN.R-project.org/package=coxme) and kinship2 v1.5.0 (http://CRAN.R-project.org/package=kinship2).
Results
All 388 study participants included in our study were tested for each of the three South African HCM-causing founder mutations. No individual was found to be compound heterozygous for any of the HCM founder mutations. A total of 256 of the study participants were clinically assessed and the basic characteristics of the cohort are summarized in Table 1. Participants are grouped according to their HCM-causing founder mutation carrier status, i.e. mutation carrier (MC) and non-carrier (NC). Individuals grouped in MC or NC are individuals from different or the same families. All participants diagnosed with HCM were in the MC group which excluded the possibility that HCM in some participants could have been due to secondary causes such as hypertension.
Frequency distributions of the genotyped SNPs did not deviate from HWE (p > 0.01). Minor allele frequencies together with MAFs for the CEU and YRI populations are shown in Table 2. All pairs of SNPs were in complete LD (D′ = 1), although not perfect LD (r = 1), except for two pairs; rs3737872 with rs2642531 (D′ = 0.23) and rs3737872 with rs4950926 (D′ = 0.92).
No statistically significant evidence for association was observed between the investigated SNPs and the respective hypertrophy traits in the total cohort, after adjusting for the confounders described earlier (results not shown). However, there was significant evidence for association between rs2250509 and hypertrophy traits in the p.A797TMYH7 HCM founder mutation group. More specifically the A allele of rs2250509 was associated with an increase of 2.70 mm in mLVWT (p = 0.017) and 1.25 mm in PC1 (p = 0.016) within the p.A797TMYH7 mutation group (Table 3).
Table 4 shows the p values for the association between MYBPH haplotypes and hypertrophy traits within HCM founder mutation groups and the haplotype frequencies in the total cohort. Haplotype GGTACTT was estimated to increase mLVWT with 2.51 mm (p = 0.036) and PC1 with 1.15 mm (p = 0.041) within the p.A797TMYH7 mutation group.
Discussion
In this study, the MYBPH SNP rs2250509 showed significant association with hypertrophy traits in the p.A797TMYH7 mutation group. The A allele of rs2250509 was associated with increases in the investigated hypertrophy traits (2.70 mm in mLVWT and 1.25 mm in the PC1 score). Moreover, haplotype GGTACTT, which includes this A allele, was observed in the p.A797TMYH7 mutation group at a frequency of 16 %, and was significantly associated with hypertrophy: each GGTACTT haplotype resulted in an increase of 2.51 mm in mLVWT and 1.15 mm in PC1. The absence of evidence for association in the other founder mutation groups may be ascribed to the sample size (the p.A797TMYH7 mutation group was the largest HCM founder mutation group), or an effect that is more directly related to the function of the causal protein and mutation involved in this group.
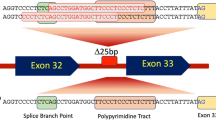
SNP rs2250509 is positioned intronically, and hence, to investigate whether variants at this position have any functional effect, we performed in silico analyses using the software programmes NetGene2 (http://www.cbs.dtu.dk/services/NetGene2/) and ASSP (http://wangcomputing.com/assp/index.html). However, this SNP did not seem to affect any splice site motifs (Brunak et al. 1991; Hebsgaard et al. 1996). Thus, the significant effects of this variant may be ascribed to that of an unknown functional variant in LD with rs2250509. This is not an unreasonable proposition, as, when we performed an in silico analysis of the other SNPs investigated here, using SNPinspector, within the Genomatix software suite v2.5 (http://www.genomatix.de/), we found that the C allele of rs762625 abolished a transcription factor binding site for the transcription factor HAND2, which is known to be involved in the expression of some cardiac genes. Based on a random selection of 40 unrelated individuals, and not the 256 individuals included in the association analysis, rs2250509 was in complete LD with rs762625, as indicated by D′ = 1; however, the LD estimates were such that they are possibly not in complete LD and are certainly not in perfect LD (r = 1) in the underlying population, which may account for the lack of evidence of association of rs762625 with the hypertrophy indices investigated.
This study had some limitations. The number of individuals of the HCM cohort genotyped in this study is considered modest; however, this is to be expected since HCM is rare (prevalence of 1:500) (Maron et al. 1995). We included all available family members of the 27 HCM founder families, which is the largest HCM cohort with known genotypes used in a modifier study reported to date. To address confounding due to family structure, cryptic relatedness and population stratification, we applied a specialized mixed-effects model that was able to incorporate random effects with coefficients describing relatedness between individuals (Price et al. 2010).
We did not use multiple testing corrections in this study. There are several methods to correct for type 1 error (false positives), of which Bonferroni adjustment is probably used most often. This approach is a particularly conservative method of stringent corrections and it assumes that all performed tests are independent; therefore, it involves multiplying each p value with the number of tests performed. It is thus possible that associations between specific genotypes and disease traits could be missed due to stringency of the correction. Currently there is no appropriate statistical method to adjust for multiple testing in studies with cohorts of extended family pedigrees and complex phenotypes such as the one used in the present study. It is thus possible that true biological effects could remain undetected if initial explorative studies are subjected to excessively stringent corrections for multiple testing. We used principal component analysis to overcome the difficulty of a comprehensibly applicable manner of capturing hypertrophy in HCM, and the hypertrophy traits used included some of the same wall thickness measurements. Moreover, since we observed some degree of LD between variants associated with the measured hypertrophy traits, we could not assume, as the Bonferroni method requires, that these variants are independent. Furthermore, since we do not have any prior information on the probability of the involvement of the variants in disease, the application of Bayesian methods for correcting for multiple testing was inappropriate (Campbell and Rudan 2002; Thomas and Clayton 2004).
In conclusion, in this study, MYBPH was for the first time assessed as a candidate hypertrophy modifying gene contributing to the variability in the hypertrophy phenotype of patients suffering from HCM. We identified a novel association between MYBPH and hypertrophy traits in HCM patients carrying the p.A797TMYH7 at SNP and haplotype level, suggesting that variation in this gene can modulate the severity of the hypertrophic phenotype in HCM as indicated by significantly increased mLVWT and PC1.
References
Barrett JC, Fry B, Maller J, Daly MJ (2005) Haploview: analysis and visualization of LD and haplotype maps. Bioinf Oxf Engl 21:263–265. doi:10.1093/bioinformatics/bth457
Brunak S, Engelbrecht J, Knudsen S (1991) Prediction of human mRNA donor and acceptor sites from the DNA sequence. J Mol Biol 220:49–65
Campbell H, Rudan I (2002) Interpretation of genetic association studies in complex disease. Pharmacogenomics J 2:349–360. doi:10.1038/sj.tpj.6500132
Corfield VA, Moolman JC, Martell R, Brink PA (1993) Polymerase chain reaction-based detection of MN blood group-specific sequences in the human genome. Transfusion (Paris) 33:119–124
De La Vega FM (2007) Selecting single-nucleotide polymorphisms for association studies with SNPbrowser software. Methods Mol Biol Clifton NJ 376:177–193. doi:10.1007/978-1-59745-389-9_13
De La Vega FM, Isaac HI, Scafe CR (2006) A tool for selecting SNPs for association studies based on observed linkage disequilibrium patterns. Pac Symp Biocomput Pac Symp Biocomput 487–498
Diao G, Lin DY (2006) Improving the power of association tests for quantitative traits in family studies. Genet Epidemiol 30:301–313. doi:10.1002/gepi.20145
Frey N, Olson EN (2003) Cardiac hypertrophy: the good, the bad, and the ugly. Annu Rev Physiol 65:45–79. doi:10.1146/annurev.physiol.65.092101.142243
Girolami F, Olivotto I, Passerini I et al (2006) A molecular screening strategy based on beta-myosin heavy chain, cardiac myosin binding protein C and troponin T genes in Italian patients with hypertrophic cardiomyopathy. J Cardiovasc Med (Hagerstown) 7:601–607
Hebsgaard SM, Korning PG, Tolstrup N et al (1996) Splice site prediction in Arabidopsis thaliana pre-mRNA by combining local and global sequence information. Nucl Acids Res 24:3439–3452
Ho CY (2010) Genetics and clinical destiny: improving care in hypertrophic cardiomyopathy. Circulation 122:2430–2440. doi:10.1161/CIRCULATIONAHA.110.978924
Ho CY, Charron P, Richard P et al (2015) Genetic advances in sarcomeric cardiomyopathies: state of the art. Cardiovasc Res 105:397–408. doi:10.1093/cvr/cvv025
Lange C, DeMeo DL, Laird NM (2002) Power and design considerations for a general class of family-based association tests: quantitative traits. Am J Hum Genet 71:1330–1341. doi:10.1086/344696
Lechin M, Quiñones MA, Omran A et al (1995) Angiotensin-I converting enzyme genotypes and left ventricular hypertrophy in patients with hypertrophic cardiomyopathy. Circulation 92:1808–1812
Lorell BH, Carabello BA (2000) Left ventricular hypertrophy: pathogenesis, detection, and prognosis. Circulation 102:470–479
Marian AJ (2002) Modifier genes for hypertrophic cardiomyopathy. Curr Opin Cardiol 17:242–252
Marian AJ, Roberts R (2001) The molecular genetic basis for hypertrophic cardiomyopathy. J Mol Cell Cardiol 33:655–670. doi:10.1006/jmcc.2001.1340
Marian AJ, Yu QT, Workman R et al (1993) Angiotensin-converting enzyme polymorphism in hypertrophic cardiomyopathy and sudden cardiac death. Lancet 342:1085–1086
Maron BJ, Gardin JM, Flack JM et al (1995) Prevalence of hypertrophic cardiomyopathy in a general population of young adults. Echocardiographic analysis of 4111 subjects in the CARDIA Study. Coronary artery risk development in (young) adults. Circulation 92:785–789
Maron BJ, Ommen SR, Semsarian C et al (2014) Hypertrophic cardiomyopathy. J Am Coll Cardiol 64:83–99. doi:10.1016/j.jacc.2014.05.003
Moolman-Smook JC, De Lange WJ, Bruwer EC et al (1999) The origins of hypertrophic cardiomyopathy-causing mutations in two South African subpopulations: a unique profile of both independent and founder events. Am J Hum Genet 65:1308–1320. doi:10.1086/302623
Mouton J, Loos B, Moolman-Smook JC, Kinnear CJ (2014) Ascribing novel functions to the sarcomeric protein, myosin binding protein H (MyBPH) in cardiac sarcomere contraction. Exp Cell Res. doi:10.1016/j.yexcr.2014.11.006
Pilia G, Chen W-M, Scuteri A et al (2006) Heritability of cardiovascular and personality traits in 6,148 Sardinians. PLoS Genet 2:e132. doi:10.1371/journal.pgen.0020132
Price AL, Zaitlen NA, Reich D, Patterson N (2010) New approaches to population stratification in genome-wide association studies. Nat Rev Genet 11:459–463. doi:10.1038/nrg2813
Revera M, van der ML, Heradien M et al (2008) Troponin T and beta-myosin mutations have distinct cardiac functional effects in hypertrophic cardiomyopathy patients without hypertrophy. Cardiovasc Res 77:687–694
Schiller NB, Shah PM, Crawford M et al (1989) Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr 2:358–367
Seidman CE, Seidman JG (2011) Identifying sarcomere gene mutations in hypertrophic cardiomyopathy: a personal history. Circ Res 108:743–750. doi:10.1161/CIRCRESAHA.110.223834
Sobel E, Lange K (1996) Descent graphs in pedigree analysis: applications to haplotyping, location scores, and marker-sharing statistics. Am J Hum Genet 58:1323–1337
Su M, Wang J, Kang L et al (2014) Rare variants in genes encoding MuRF1 and MuRF2 are modifiers of hypertrophic cardiomyopathy. Int J Mol Sci 15:9302–9313. doi:10.3390/ijms15069302
Thierfelder L, Watkins H, MacRae C et al (1994) Alpha-tropomyosin and cardiac troponin T mutations cause familial hypertrophic cardiomyopathy: a disease of the sarcomere. Cell 77:701–712
Thomas DC, Clayton DG (2004) Betting odds and genetic associations. J Natl Cancer Inst 96:421–423
van der Merwe L, Cloete R, Revera M et al (2008) Genetic variation in angiotensin-converting enzyme 2 gene is associated with extent of left ventricular hypertrophy in hypertrophic cardiomyopathy. Hum Genet 124:57–61. doi:10.1007/s00439-008-0524-6
Wigginton JE, Abecasis GR (2005) PEDSTATS: descriptive statistics, graphics and quality assessment for gene mapping data. Bioinf Oxf Engl 21:3445–3447. doi:10.1093/bioinformatics/bti529
Acknowledgments
We would like to thank all the participants involved in this study and Mrs. Ina le Roux for her technical assistance. This work was supported by the Wellcome Trust (International Senior Research Fellowship, fellowship GR073610MA to Hanlie Moolman-Smook), London, United Kingdom.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Mouton, J.M., van der Merwe, L., Goosen, A. et al. MYBPH acts as modifier of cardiac hypertrophy in hypertrophic cardiomyopathy (HCM) patients. Hum Genet 135, 477–483 (2016). https://doi.org/10.1007/s00439-016-1649-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00439-016-1649-7