Abstract
Mefloquine, an antimalarial drug, has been found to be effective against various stages of schistosomes in vivo. The purpose of the study is to explore the in vitro effect of mefloquine against adult and juvenile Schistosoma japonicum and to compare its efficacy with praziquantel. Three-hour-old schistosomula were prepared by penetrating the mouse skin with schistosome cercariae, while schistosomes 7-, 14-, and 35-day-old were collected from mice infected with S. japonicum cercariae for 7, 14, and 35 days by perfusion. Schistosomes were placed to each of 24 wells of a Falcon plate and maintained in Hanks’ balanced salt solution–20% calf serum. Besides observation on the direct in vitro effect of mefloquine and praziquantel, adult worms exposed to mefloquine and praziquantel for 1 and 4 h were transferred to the medium without the drugs and incubated continuously for another 72 h. The reversible effect of mefloquine and praziquantel was assessed by the recovery of the worm motor activity and parasite survival. The minimal effective concentration of mefloquine against adult schistosomes in vitro was 10 μg/mL, which revealed that the worm motor activity was first stimulated, then decreased significantly, followed by bleb formation, focal swelling and elongation of the worm body, cessation of gut peristalsis, and death of 56.3% (18/32) worms within 24–72 h. Similar appearance was seen in the adult worms exposed to higher mefloquine concentration of 20 and 30 μg/mL, but all worms died within 4–24 h. The adult schistosomes exposed to praziquantel 1–30 μg/mL showed fast spasmodic contraction of the worm body, followed by bleb formation along the tegument, feeble movement of oral sucker, and death of a part of males and females 72 h after incubation. When male and female schistosomes exposed to mefloquine 10 and 20 μg/mL for 1 and 4 h were transferred to the medium without the drug, no apparent recovery of worm motor activity and survival was seen. In case of worms exposed to praziquantel at the same concentration for 1 and 4 h before replacement of drug-free medium, a well recovery of worm motor activity, looseness of worm body, and reduction or disappearance of blebs along the tegument were observed. Mefloquine also exhibited in vitro effect against 3-h-old and 7- and 14-day-old schistosomula which was similar to that seen in adult worms, but all or parts of worms showed decrease in motor activity or even death (3-h-old and 7-day-old schistosomula) at a lower mefloquine concentration of 5 μg/mL. In 14 day-old schistosomula exposed to praziquantel 1–30 μg/mL, spasmodic contraction and significant decrease in motor activity of the worm body with movement of oral and ventral suckers were observed, but no death of worm was seen during a 3-day incubation period. The results indicate that in vitro mefloquine exhibits a direct killing effect against adult and juvenile S. japonicum which is different from that of praziquantel. Meanwhile, the juvenile schistosomes are more susceptible to mefloquine than the adult ones. Furthermore, the in vitro effect of mefloquine against adult schistosomes is irreversible, while that of praziquantel is reversible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The in vitro test with schistosomes is one of useful tools to explore the antischistosomal properties of a known effective drug and also helpful to analyze the mode of action against schistosomes. Currently, praziquantel is the only drug of choice in the treatment of three major species of schistosomes infecting humans (Fenwick et al. 2006; Doenhoff et al. 2009). A series of in vitro tests revealed that praziquantel exhibited three major pharmacological actions on schistosomes which were stimulation of worm motor activity, spasmodic contraction of the worm musculatures, and extensive damage to the worm tegument (Becker et al. 1980; Mehlhorn et al. 1981; Day et al. 1992; Xiao et al. 1998; Xiao 2007). All these manifestations induced by praziquantel in vitro may explain the fast hepatic shift of the worms with shrinkage of the worm body and severe vesiculaton of tegument that result in exposure of worm surface antigen and lead to serious immunopathological reaction of the host to kill the worms. Although exact cidal mechanism of praziquantel is still not very well known up to date, it has been shown that all these major effects of praziquantel against schistosomes are calcium-dependent (Day et al. 1992; Xiao 2007, Doenhoff et al. 2008). On the other hand, artemether, a methoxy derivative of artemisinin, is not only one of the key drugs in treatment of malaria but also exhibits antischistosomal properties (Xiao 2005a, b; Utzinger et al. 2007). By the end of last century, artemether has been developed as a prophylactic agent against schistosomiasis as detailed laboratory studies showed that the juvenile stages of the parasite were more susceptible to artemether than the adults (Le et al. 1982; Xiao et al. 1995). Although artemether induced worm hepatic shift and extensive effects on carbohydrate, nucleic acid, protein metabolism, and antioxidant system of the adult schistosomes in vivo after artemether administration (Xiao et al. 2000; Xiao 2005b), no apparent action on the adults in vitro at a higher concentration of 100 μg/mL was observed (Xiao and Catto 1989). Since blood cells are taken up by both malaria and schistosomes for nutrition and generation of pigment after metabolism (Kloetzel and Lewert 1966), it is similar to malaria (Meshnick et al. 1996) that an interaction between artemether and hemin, or other iron compounds may occur in schistosomes which results in cleavage of endoperoxide bond of the artemisinin compound, followed by formation of free radical and series of biochemical reactions toxic to the worms (Xiao et al. 2003). Further in vitro study indicated that when schistosomes exposed to lower concentration of artemether together with hemin resulted in a decrease in worm motor activity, followed by severe tegumental damage, dilatation of gut, cloudiness of the worm body, and death (Xiao et al. 2001). The aforementioned data demonstrate that study on in vitro effect of a known antischistosomal drug is an important way to better understand the antischistosomal properties and provides the possibility to explore its mode of action on schistosomes.
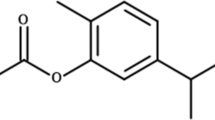
In 2008, another antimalarial drug, mefloquine—an aminoalcohol compound (Ohnmacht et al. 1971) was reported to be effective in significant reduction of egg production in Schistosoma mansoni-infected mice after administration of a lower dose of 150 mg/kg, but the drug had no effect on worm burden (Van Nassauw et al. 2008). Interestingly, mefloquine exhibited potential effect against juvenile stages and adult S. mansoni and Schistosoma japonicum when a higher dose of 400 mg/kg was administered to the infected mice (Keiser et al. 2009). The characteristics concerning the antischistosomal properties of mefloquine are different from praziquantel and artemether. It is already recognized that praziquantel is effective against adult schistosomes and very early stage of schistosomula a few hours after penetrating into host’s skin, but an important shortcoming of praziquantel is its much less efficacy against young developing stages of schistosomula (Yue et al. 1985; Sabah et al. 1986; Xiao et al. 1987). This might impact on the cure rate of the patients treated with praziquantel or reinfection of individuals after treatment with praziquantel in areas of heavy schistosomiasis transmission (Wu et al. 1993; Dabo et al. 2000; Danso-Appiah and de Vlas 2002; N'Goran et al. 2003). Although artemether has been developed as a prophylactic agent against schistosomiasis, its frequent administration of the drug every 2 weeks during transmission season hinders its promoted application (Xiao 2005b).
Experimental studies indicate that mefloquine exhibits similar efficacy against various developmental stages of schistosomes including adult worms (Keiser et al. 2009). Histopathological and morphological observations demonstrated that mefloquine induced an extensive damage to the worm's digestive system, tegument, musculature, parenchymal tissues, and reproductive system (Zhang et al. 2009; Xiao et al. 2009a, b), but no knowledge is available in dealing with the in vitro effect of mefloquine against schistosomes, which is useful for a better understanding on the antischistosome properties of the drug. The present paper reports the in vitro effect of mefloquine against both adult and juvenile S. japonicum in comparison with that of praziquantel.
Materials and methods
Parasites and host animals
S. japonicum cercariae (Anhui isolate), released from infected Oncomelania hupensis snails, were provided by the Department of Vector Biology, National Institute of Parasitic Diseases, Chinese Center for Disease Control and Prevention (Shanghai, China). Eighty-nine female Kunming strain mice, weighing 22–24 g, purchased from Shanghai Animal Center, Chinese Academy of Sciences (Shanghai, China) were maintained on rodent food and water ad libitum.
Infection and collection of schistosomes
Mice were infected with 80–100 S. japonicum cercariae via shaved abdominal skin. Five to seven mice were killed by bleeding 7-, 14-, or 35-day postinfection, and the juvenile (7- or 14-day-old) and adult schistosomes (35-day-old) were collected by perfusion (Yolles et al. 1947) with ice-cold Hanks’s balanced salt solution (HBSS) from mesenteric veins and livers. The juvenile or adult schistosomes were rinsed three times with HBSS containing 100 IU/mL penicillin and 100 IU/mL streptomycin and kept in an ice bath before incubation. For preparation of 3-h-old schistosomula, four mice were killed, and the shaved abdominal skin of each mouse was then cut off, and S. japonicum cercariae were subjected to penetrate the mouse skin according to the method of Clegg and Smithers (1972).
Drugs and chemicals
Mefloquine and praziquantel were provided by Libang Pharmaceutical Co. Ltd. (Xian, China) and Shanghai Sixth Pharmaceutical Factory (Shanghai, China), respectively. A stock solution of mefloquine or praziquantel was prepared by dissolving 1 mg of the drug (free base in mefloquine) in 0.4 ml dimethyl sulfoxide (DMSO) and then adding 0.6 ml HBSS to give a stock solution with 1 mg mefloquine or 1 mg praziquantel per milliliter. Stock solution of each compound was diluted with HBSS for use.
Schistosome incubation in vitro
HBSS supplemented with 20% heat-inactivated calf serum, 0.4% glucose, 100 IU/mL penicillin sodium, 100 IU/mL streptomycin, and 0.25 μg/mL amphotericin B (HBSS–20% calf serum) was used to maintain the schistosomes in vitro. The volume of medium added to each of the 24 wells of a Falcon plate was 1.85–2.00 mL, and then, two pairs of worms or four male and two female worms were placed in each well. For juvenile incubation, 50 μL of 3-h-old and 7- and 14-day-old schistosomula suspended in the medium were added to each well of the plate. The plate was incubated at 37°C in 95% air + 5% CO2 for 30–60 min before addition of mefloquine or praziquantel at various concentrations. The final volume in each well was 2.0 mL. Control wells contained the worms and medium only, or 0.8% and 1.2% DMSO alone, i.e., the corresponding concentrations of DMSO used in the concentrations of mefloquine and praziquantel at 20 and 30 μg/mL, respectively, in a final volume of 2.0 mL. After addition of the aforementioned substances, the plates were incubated continuously for 72 h, and each test with juvenile or adult schistosomes were repeated two to three times.
In order to observe the reversible effect of mefloquine and praziquantel, two pairs of worms placed in each of 24 wells of a Falcon plate were exposed to the medium of HBSS–20% calf serum containing mefloquine or praziquantel at a final concentration of 10 or 20 μg/mL for 1–4 h. Then, the medium with the drug was removed, and the worms were rinsed three times with HBSS. Afterwards, the worms were incubated continuously in the medium without drug for another 72 h. The tests were repeated two times.
Assessment of drug effect
After juvenile and adult schistosomes were exposed to mefloquine or praziquantel for 1, 4, 24, 48, and 72 h, motor activity, tegumental alterations, and parasite survival were evaluated by examination under an inverted microscope (Olympus CK×41, Japan) and recorded. The reversible effect of mefloquine and praziquantel was assessed by the recovery of worm motor activity and survival of the worms. Parasite death was defined as no motor activity during 2-min observation plus morphological and tegumental alterations.
Result
Effect on adult (35-day-old) schistosomes
Change in motor activity and morphology
Mefloquine
Adult male and female schistosomes exposed to mefloquine in vitro at concentrations of 1–5 μg/mL for 72 h exhibited no apparent change in their motor activity and morphology. At a concentration of 10 μg/mL, exciting in motor activity and unnatural body attitude were seen in both males and females within 10–30 min. Particularly, the gut pigments were vomited by the females, and the anterior portion of female worms elongated with distortion and swayed strongly and frequently. In addition, the portion around oral sucker revealed swelling gradually, and the worm body tissues turned to light gray in color. Four to 24 h after incubation, the motor activity and morphology of the worms exhibited the following alterations, i.e., (1) significant elongation in anterior portion of female worm body was universally seen which revealed the curl and unbending alternately and swayed frequently; (2) the males exhibited stiff manner and unnatural activity with stretched worm head without contraction of the oral sucker; (3) focal swelling was usually seen along the whole body of both the males and females and was more severe in the posterior portion of females; (4) the motor activity decreased significantly in both males and females, followed by the stimulation of worm activity and blebs with various sizes emerged along the tegument 2–4 h post incubation. Twenty-four hours after incubation, parts of male and female worms started dying. Meanwhile, a part of female worm body still showed sway frequently, but most male worms and a part of female worms exhibited feeble motor activity. In addition, some enlarged blebs collapsed along the tegument of male and female worms which resulted in roughness of tegumental surface. Meanwhile, deformation of female worm head and cloudiness of the male worm body with feeble movement were also seen. Forty-eight hours after incubation, the appearances of the male and female worms were similar to that observed at 24 h after incubation, but many debris of damage tegument were observed in the medium. Up to 72 h after incubation, parts of male and female worms died, while others still showed very feeble motor activity of worm body with moderate or severe damage to the tegument.
When male and female worms were exposed to mefloquine at a concentration of 20 μg/mL for 10–30 min, the motor activity of the worms exhibited a significant decrease after a short stimulation, followed by separation of the female worms from the gynecophoric canal of the paired male worm. Meanwhile, male and female worms elongated their body gradually, especially the female worms, and focal swelling along the posterior portion of the worm body was universal. In addition, the female worms vomited parts of gut pigment from the oral sucker followed by cessation of gut peristalsis which resulted in dilatation of gut filled with focal accumulation of gut pigment. About 20 min after exposure, several blebs with various sizes emerged in parts of female worms and individual male worms. Up to 2 h after exposure, blebs were found in all male and female worms. Initially, the blebs distributed on the tegumental surface sparsely which were quite different from the very small blebs emerged on the tegument of worms exposed to praziquantel. Interestingly, the blebs induced by mefloquine enlarged gradually followed by collapse which resulted in roughness of the worm surface. In addition, focal swelling of the worm body spread over the whole worm, especially in female worms; severe swelling of the anterior end caused the sucker to lose its definition. In male worms, the suckers did not usually exhibit any movement because of the stretch in the anterior end of the worm, but feeble sway of the male worm head could be seen. Four hours after incubation, all worms appeared in stretched manner, and many blebs with various sizes emerged along the tegument, and some of them that enlarged with time resulted in collapse. Meanwhile, a part of male and female worms with severe damage to the tegument died at this time point. The remaining worms still showed very feeble activity and died within 24 h after incubation. Similar manifestation was seen in male and female schistosomes exposed to mefloquine of 30 μg/mL, but stimulation of worm activity sustained a very short period of time followed by decrease in motor activity, vesiculation along the tegument, and elongation as well as swelling of the worm body. Four hours after incubation, all male and female worms situated in lax manner with severe damage to the tegument and focal swelling of the worm body. Meanwhile, most male and female worms did not exhibit any motor activity and were assessed to be dead.
Praziquantel
When male and female schistosomes were exposed to praziquantel at concentrations of 1–30 μg/mL, the manifestations of the worms in each concentration group were similar, i.e., significant decrease in motor activity, shrinkage of the worm body, and vesiculation along the tegumental surface. During the first 4 h after incubation, the spasmodic contraction of worms in higher concentration of praziquantel was stronger, especially in the male worms. Further shrinkage of the worm body was seen in each concentration group 24 h later. After exposure of schistosomes to praziquantel at the concentrations aforementioned for 30 min to 2 h, the motor activity of male and female worms decreased significantly. In the group with a lower concentration of 1 μg/mL, apart from feeble contraction of oral sucker, occasional sway of the worm body was seen. When the concentration of praziquantel was increased to 5–30 μg/mL, only feeble contraction of oral sucker was observed in both male and female worms. Furthermore, such feeble contraction of the oral sucker was sustained, at least, for 72 h in a part of male and female worms. Within 4 h after schistosomes exposed to praziquantel of 1 μg/mL, no or a few small blebs were detected in focal tegument, but more blebs emerged from the worm tegumental surface 24 h later. In the worms exposed to praziquantel at concentrations of 5–30 μg/mL, some very small blebs that emerged from the focal tegument were seen in males 30 min after exposure. Twenty-four to 72 h after incubation, the number and size of the blebs increased with time which distributed extensively on the surface of male worms, and some of them collapsed. Meanwhile, some blebs were also seen on focal tegumental surface of female worms 24 to 72 h after incubation. Seventy-two hours after incubation, no motor activity was seen in parts of worms, and it was judged as death.
Survival of adult schistosomes
Paired schistosomes maintained in HBSS–20% calf serum kept a normal motor activity, and most male worms were attached on the bottom of the well by ventral sucker during 72-h incubation. Parts of female worms separated from the gynecophoric canal of male worms also showed normal motor activity, and gut peristalsis was usually seen. In the medium containing 0.8% or 1.2% of DMSO, no impact on worm motor activity and survival was observed which was similar to the control. In paired schistosomes exposed to mefloquine at concentrations of 1 and 5 μg/mL, no death of the worms was seen. When the concentration of mefloquine was increased to 10 μg/mL, 18 out of 32 (56.3%) worms died within 24- to 72-h postincubation. The remaining 14 worms showed severe damage to the tegument and internal structure, but very feeble or occasional sway of focal worm body was still shown. While the worms exposed to mefloquine at the concentration of 20 μg/mL, 62.5% and 37.5% of worms died 4 and 24 h after exposure, respectively. At the higher concentration of 30 μg/ml, the mortalities of the worms revealed at the same time points after exposure were 83.3% and 16.7%, respectively (Table 1).
When male and female schistosomes were exposed to praziquantel at concentrations of 1–30 μg/mL, no death of worm was seen during 24 to 48 h after incubation, although moderate and severe vesiculation appeared, especially in male worms. Seventy-two hour post exposure, 42.9–80% of male worms and 8.3–50% of female worms were dead, but no correlation was seen between the number of worm death and drug concentration (Table 1)
Reversible effect of mefloquine and praziquantel
Mefloquine
When six paired schistosomes were exposed to mefloquine 10 μg/mL for 1 h, a part of worms showed stimulation of motor activity while a part of them decreased in motor activity. Meanwhile, light elongation of female worm body, stretch in anterior portion of male worm, and few blebs emerging in parts of male and female worms were observed. After being rinsed with HBSS, transferred to the drug-free medium, and continuously incubated for 2–4 h, stimulation of worm activity was still seen in parts of male and female worms while parts of worms decreased in motor activity accompanied by focal swelling of worm body and bleb formation along the worm tegument. After incubation for 24 to72 h, four out of six male and three out of six female worms were dead due to damage to the worms including severe swelling and vesiculation along the tegument. The remaining worms also showed severe damage but still revealed very feeble and occasional activity. In worms transferred to the drug-free medium before exposure to mefloquine of 10 μg/mL for 4 h, the original damage such as swelling and vesiculation along the tegument and elongation of the worm body continued to develop. Twenty-four hours after incubation, five out of six male worms died, and the remaining one male worm died 48 h later. Similar appearance was seen in female worms, but two out of six female worms still showed life with feeble activity 72 h after incubation. In paired schistosomes exposed to mefloquine of 20 μg/mL, the motor activity of the worms decreased significantly, followed by vesiculation along the tegument, focal swelling, and elongation of the worm body. An hour later, no apparent motor activity was seen in both male and female worms. After these worms were transferred to drug-free medium and continued to incubate for 2–4 h, three out of six male or six female worms showed recovery of poor motor activity which revealed in very feeble swinging, but 24 h later, all male and female worms died accompanied by severe destruction of the worm body. Similar results were obtained from the paired schistosomes exposed to mefloquine of 20 μg/mL for 4 h before they were transferred to the medium without drug for continuing incubation (Table 2).
Praziquantel
When four groups of six paired schistosomes exposed to praziquantel of 10 or 20 μg/mL for 1 and 4 h, the appearances of the worms were similar, e.g., the worms decreased in motor activity immediately after they contacted with praziquantel, followed by spasmodic contraction of the worm body which resulted in more shortened worm body in male worms than in female ones. Besides very feeble movement of oral suckers, no motor activity was seen in male worms, but in female worms, occasional sway of anterior or posterior portion of the worm body was observed. At these time points, very fine blebs were detected along the tegument of male worms under high power microscope, but it was rarely seen in the females. After above-mentioned worms were rinsed with HBSS and transferred to the drug-free medium for 1–4 h, looseness of worm body was usually seen in both male and female worms accompanied by recovery of motor activity. After continuing incubation for 24 to 48 h, further elongation of worm body and recovery of motor activity were seen, and about one third male and female worms revealed vigorous activity with natural attitude, or the number of bleb decreased significantly along the tegument of male worms. At 72 h after incubation, bleb almost disappeared from the tegument in a part of male worms resulting in smooth worm surface. In the remaining male and female worms, apparent recovery of damaged tegument was also seen. Interestingly, in six male worms exposed to praziquantel of 10 or 20 μg/mL for 1 h before transferring to the medium without the drug, two of them recovered the ability, attaching to the bottom of well by their ventral suckers. If the exposure time was extended to 4 h, none of six male worms in each group recovered the attachment ability by ventral sucker, but all the worms showed apparent activity. In each group, six female worms usually showed apparent recovery of motor activity which revealed movement of oral or ventral suckers and contraction of the worm body (Table 2).
Effect on juvenile schistosomes
Three-hour-old schistosomula
After exposure of 3-h-old schistosomula to the medium containing mefloquine of 10 and 20 μg/mL, all worms revealed no motor activity immediately, followed by emergence of one or several small blebs along the worm surface. When the concentration of mefloquine was decreased to 5 μg/mL, almost all of the worms exhibited no motor activity within 10–30 min, followed by change in gray color of worm internal structures. Twenty-four hours after exposure, 74 out of 85 worms were dead, while the remaining 11 worm died on 48 and 72 h after exposure. No abnormality was seen in the worms exposed to mefloquine at a concentration of 1 μg/mL. They showed normal appearance and motor activity as seen in the worms maintained in the medium without DMSO or with 0.8% DMSO (Table 3).
Seven-day-old schistosomula
In 7-day-old schistosomula exposed to the medium containing mefloquine 1 μg/mL, no impact on worm motor activity and survival was seen during 72-h incubation which was similar to the worms maintained in the medium without DMSO or with 0.8% DMSO. When the drug concentration was increased to 5 μg/mL, a part of worms showed normal activity, while a part of them contracted as ellipse with slow movement and roughness in worm surface within 15 min to 1 h. After 24-h incubation, 19 out of 51 worms exhibited no motor activity, indistinction of internal structure with gray particles, emergence of one or several blebs, and focal accumulation of intestine pigment to form small mass. Other worms also showed morphological alteration with feeble activity, while two of them revealed normal appearance and activity. After incubation of the worms for 48 h, other six worms were assessed to be dead, and the appearances of the remaining worms were similar to those seen at 24 h, but more enlarged or collapsed blebs were observed. Up to 72 h after incubation, 42 out of 51 worms were dead, while the worms that survived the treatment showed severe damage with very feeble activity (Table 3). In higher mefloquine concentrations of 10 and 20 μg/mL, all worms decreased their motor activity immediately after exposure and showed focal contraction, and the color of the internal structure changed in gray. Initially, only one to several blebs were seen on focal surface of the worms, and then, the blebs enlarged and surrounded the whole worm body or even collapsed which resulted in roughness of the worm surface. All worms tested did not exhibit any motor activity 1 h after exposure to the drug and were assessed to be dead (Table 3).
Fourteen-day-old schistosomula
Mefloquine
The motor activity of 14-day-old schistosomula maintained in the HBSS–20% calf serum containing 1.2% DMSO was similar to those in the same medium without DMSO. In 14-day-old schistosomula exposed to the medium containing 1 μg/mL of mefloquine, no impact on the juvenile activity was seen. In the medium containing mefloquine of 5 μg/mL, most juveniles exhibited normal appearance, while parts of juveniles showed cloudy in the worm body, decrease in motor activity, and the worm body tissues turned to gray particles. No death of juveniles was seen during 72-h incubation. When the concentration of mefloquine increased to 10, 20, or 30 μg/mL, the worm body stretched rapidly, and the activity of the juveniles became very feeble or even ceased, followed by the worm body tissues turning to gray particles and focal swelling along the whole worm body which resulted in cloudy and indistinction of the internal structures. About 20 min after exposure, one or several blebs were emerged on the tegumental surface. Initially, the bleb was small, and then, the bleb enlarged gradually accompanied by emergence of several or many blebs with various sizes along the worm body. Finally, the enlarged blebs collapsed, and the whole worms became indistinct. Two to 4 h after incubation, 73.1% (38/52) juveniles exposed to mefloquine of 10 μg/mL were dead, while the remaining were still alive with very feeble activity. Finally, they died within 48 h after incubation (Table 3). In the juveniles exposed to mefloquine of 20 and 30 μg/mL, all were dead during 2–4-h incubation period (Table 3).
Praziquantel
After the juveniles were exposed to the medium containing praziquantel at concentrations of 1, 5, 10, 20, and 30 μg/mL, all worms decreased their motor activity rapidly, followed by spasmodic contraction which resulted in shortening of the worm body. In higher concentrations over 10 μg/mL, more shortened worm bodies were seen. Besides the spasmodic contraction of the worm body, the motor activity of the worm was inhibited significantly, but oral sucker usually exhibited very active movement which sustained for, at least, 72 h. Meanwhile, ventral sucker also showed some active movement, especially in the juveniles exposed to praziquantel 1–5 μg/mL. Generally, no blebs were seen on the tegument of juveniles exposed in lower concentrations of 1–5 μg/mL, but at higher concentrations at 10 μg/mL or over, some small blebs were seen along the worm surface, which were not serious. In all juveniles exposed to praziquantel at above-mentioned concentrations for 72 h, no death of the worm was seen (Table 3).
Discussion
It is interesting to note that mefloquine is the third antimalarial drug possessing antischistosomal properties after artemisinins (artemether and artesunate) and trioxolanes (Xiao 2005a, b, 2007; Utzinger et al. 2007). The preliminary study on in vitro effect indicated that mefloquine exhibited a fast, strong, and direct action against both adult and juvenile S. japonicum. The characteristics of in vitro effect against adult and juvenile schistosomes in comparison with praziquantel may be summarized as follows: Firstly, the minimal effective concentration of mefloquine against adult schistosomes which induces alteration of worm motor activity, focal swelling, elongation of the worm body, and death of part of the worms emerging 24 h post exposure to the drug was 10 μg/mL, while below this level, i.e., 5 μg/mL, mefloquine exhibited no effect on the worms, indicating that the minimal effective concentration of mefloquine required to impact on adult schistosomes in vitro is higher. When the adult schistosomes were exposed to mefloquine at higher concentrations of 20 and 30 μg/mL, the process of the drug against the worms was fast that over 50% of the worms died within 4 h, and the remaining worms died within 24 h, demonstrating that mefloquine exhibits a direct killing effect on adult schistosomes in vitro. In comparison with praziquantel, the lower concentration of 1 μg/ml up to the higher concentration of 30 μg/ml may induce similar pharmacological action on adult schistosomes. Although spasmodic contraction of the worm body and damage to the worm tegument were seen, a part of worms in each concentration tested started to die without regular pattern of 72 h post exposure. Previous studies have identified that when schistosomes exposed to an immune system containing antischistosomal antibody, neutrophils, complement, and praziquantel (1 μg/ml), the damage to the worm tegument induced by the drug and attachment of neutrophils on the worm surface aggravated the tegument injury which resulted in worm death within 24 h (Xiao et al. 1986). In mice infected with schistosomes and treated with praziquantel at a single curative dose, dead worms were seen in the liver in 24-h posttreatment (Xiao et al. 1983), which can be explained by the exposure of worm surface antigen induced by praziquantel, and thus, the worms are vulnerable to be attacked by the host immune response (Xiao et al. 1981), i.e., the antischistosomal effect of praziquantel is immune (antibody)-dependent (Doenhoff et al. 1987; Xiao 2008).
Secondly, mefloquine exhibits more potential in vitro effect against juvenile schistosomes than the adults which reveals that minimal effective concentration of mefloquine against 3-h-old and 7-day-old juvenile is 5 μg/mL. Although no 14-day-old juvenile was killed under this concentration level, parts of the juveniles showed abnormal motor activity and some changes in their morphology. Meanwhile, after the juvenile schistosomes were exposed to mefloquine, the process of action induced by mefloquine was faster and more severe than that seen in adult schistosomes which results in the death of all the juveniles within 1–4 h under exposure to mefloquine of 20 and 30 μg/mL. The juvenile schistosomes being more susceptible to mefloquine is also seen in the process of pathological alteration induced by mefloquine in vivo, i.e., the emergence of dead juvenile schistosomes is faster than that of dead adult worms in mice infected with S. japonicum cercariae for 14 and 35 days and treated with mefloquine at the same single dose of 400 mg/kg (Zhang et al. 2009; Xiao and Zhang 2009). In in vitro test with juvenile schistosomes, higher praziquantel concentrations of 10–30 μg/mL were used. Apart from the spasmodic contraction of the worm body, no death of juvenile and no or less blebs were seen which was quite different from the severe damage to the tegument of adult worms under the same concentration of praziquantel. The result is consistent to the previous observation that 7- and 14-day-old juvenile schistosomes are unsusceptible to praziquantel (You et al. 1986). Interestingly, although mefloquine exhibits potential in vitro effect against 3-h-old schistosomula (skin stage), no or poor efficacy is seen in mice infected with schistosome cercariae for 3 h and treated with mefloquine (Keiser et al. 2009; Xiao et al. 2009b). Therefore, it is suggested that no drug could be excreted and secreted from the mouse skin after oral administration of mefloquine which might be the major cause.
Thirdly, the bleb formations induced by mefloquine and praziquantel were different. In adult and juvenile schistosomes, the patterns of bleb formation induced by mefloquine are the same, and the time of bleb emergence from the worm tegument depends on the concentrations of mefloquine used. Meanwhile, all dead juvenile and adult schistosomes reveal severe bleb formation including enlargement and collapse of the blebs. No such relationship between bleb formation and death of worms was seen in in vitro test with praziquantel. Interestingly, our results show that in vitro mefloquine-induced damage to the adult schistosomes including motor activity and bleb formation is irreversible which is different from that induced by praziquantel, further demonstrating that mefloquine endorses direct killing effect on both adult and juvenile schistosomes with a similar action pattern. Therefore, the in vitro test provides a good tool to further explore and analyze the mode of action of mefloquine against schistosomes.
References
Becker B, Mehlhorn H, Andrews P, Thomas H, Eckert J (1980) Light and electron microscopic studies on the effect of praziquantel on Schistosoma mansoni, Dicrocoelium dendriticum, and Fasciola hepatica (Trematoda) in vitro. Z Parasitenkd 63:113–128
Clegg JA, Smithers SR (1972) The effects of immune rhesus monkey serum on schistosomula of Schistosoma mansoni during cultivation in vitro. Int J Parasitol 2:79–98
Dabo A, Doucoure B, Koita O, Diallo M, Kouriba B, Klinkert MQ, Doumbia S, Doumbo O (2000) Reinfection by Schistosoma haematobium and S. mansoni despite repeated praziquantel treatment in office du Niger (Mali). Med Trop (Mars) 60:351–355
Danso-Appiah A, de Vlas SJ (2002) Interpreting low praziquantel cure rates of Schistosoma mansoni infections in Senegal. Trends Parasitol 18:125–129
Day TA, Bennett L, Pax A (1992) Praziquantel: the enigmatic antiparasitic. Parasitol Today 8:342–344
Doenhoff MJ, Sabah AA, Fletcher C, Webbe G, Bain J (1987) Evidence for an immune-dependent action of praziquantel on Schistosoma mansoni in mice. Trans R Soc Trop Med Hyg 81:947–951
Doenhoff MJ, Cioli D, Utzinger J (2008) Praziquantel: mechanisms of action, resistance and new derivatives for schistosomiasis. Curr Opin Infect Dis 21:659–667
Doenhoff MJ, Hagan P, Cioli D, Southgate V, Pica-Mattoccia L, Botros S, Coles G, Tchuem Tchuenté LA, Mbaye A, Engels D (2009) Praziquantel: its use in control of schistosomiasis in sub-Saharan Africa and current research needs. Parasitology 13:1–11
Fenwick A, Rollinson D, Southgate V (2006) Implementation of human schistosomiasis control: challenges and prospects. Adv Parasitol 61:567–622
Keiser J, Chollet J, Xiao SH, Mei JY, Jiao PY, Utzinger J, Tanner M (2009) Mefloquine—an aminoalcohol with promising antischistosomal properties in mice. PLoS Negl Trop Dis 3:e350
Kloetzel K, Lewert RM (1966) Pigment formation in Schistosoma mansoni infections in the white mouse. Am J Trop Med Hyg I5:28–31
Le WJ, You JQ, Yang YQ, Mei JY, Guo HF, Yang HZ, Zhang CW (1982) Studies on the efficacy of artemether in experimental schistosomiasis. Acta Pharmaceutica Sin 17:187–193
Mehlhorn H, Becker B, Andrews P, Thomas H, Frenkel JK (1981) In vivo and in vitro experiments on the effects of praziquantel on Schistosoma mansoni. A light and electron microscopic study. Arzneimittelforschung 31(3a):544–554
Meshnick SR, Taylor TE, Kamchonwongpaisan S (1996) Artemisinin and the antimalarial endoperoxides: from herbal remedy to targeted chemotherapy. Microbiol Rev 60:301–315
N'Goran EK, Gnaka HN, Tanner M, Utzinger J (2003) Efficacy and side-effects of two praziquantel treatments against Schistosoma haematobium infection, among schoolchildren from Côte d'Ivoire. Ann Trop Med Parasitol 97:37–51
Ohnmacht CJ, Patel AR, Lutz RE (1971) Antimalarials. 7. Bis (trifluoromethyl)-(2-piperidyl)-4-quinolinemethanols. J Med Chem 14:926–928
Sabah AA, Fletcher C, Webbe G, Doenhoff MJ (1986) Schistosoma mansoni: chemotherapy of infections of different ages. Exp Parasitol 61:294–303
Utzinger J, Xiao SH, Tanner M, Keiser J (2007) Artemisinins for schistosomiasis and beyond. Curr Opin Investig Drugs 8:105–116
Van Nassauw L, Toovey S, Op V, den Bosch J, Timmermans JP, Vercruysse J (2008) Schistosomicidal activity of the antimalarial drug, mefloquine, in Schistosoma mansoni-infected mice. Travel Med Infect Dis 6:253–258
Wu Z, Bum K, Yuan L, Yang G, Zhu J, Liu Q (1993) Factors contributing to reinfection with schistosomiasis japonica after treatment in the lake region of China. Acta Trop 54:83–88
Xiao SH (2005a) Development of antischistosomal drugs in China, with particular consideration to praziquantel and the artemisinins. Acta Trop 96:153–167
Xiao SH (2005b) Study on prevention and cure of artemether against schistosomiasis. Chin J Schisto Contr 17:310–319
Xiao SH (2007) Study progress on the mode of action of praziquantel against schistosomes. Chin J Parasitol Parasitic Dis 25:492–502
Xiao SH (2008) Impact of host factors on the schistosome-killing process induced by praziquantel. Chin J Parasitol Parasitic Dis 26:217–225
Xiao SH, Catto BA (1989) In vitro and in vivo studies of the effect of artemether on Schistosoma mansoni. Antimicrob Agents Chemother 33:1557–1562
Xiao SH, Zhang CW (2009) Histopathological alteration of juvenile Schistosoma japonicum in mice following treatment with single-dose mefloquine. Parasitol Res. doi:10.1007/s00436-009-1611-x
Xiao SH, Xue HC, Guo HF, Yang HZ, Shao BR (1981) The appearance of surface antigen of Schistosoma japonicum recovered from infected mice after the treatment with pyquiton. Shanghai J Immunol 1:9–15
Xiao SH, Yang YQ, Yang HZ, Guo HF, Shao BR (1983) Observation on tegument damage of Schistosoma japonicum and penetration of host leukocytes into the worm body caused by pyquiton. Acta Pharmaceutica Sin 18:241–246
Xiao SH, Guo HF, Xue HC, Qiu LS, Zhang RQ (1986) Attachment of mouse neutrophils in vitro on the praziquantel-damaged surface of adult Schistosoma japonicum in the presence of immune sera. Acta Pharmacol Sin 7:165–170
Xiao SH, Yue WJ, Yang YQ, You JQ (1987) Susceptibility of Schistosoma japonicum of different developmental stages to praziquantel. Chin Med J 100:759–768
Xiao SH, You JQ, Yang YQ, Wang CZ (1995) Experimental studies on early treatment of schistosomal infection with artemether. Southeast Asia J Trop Med Public Health 26:306–318
Xiao SH, You JQ, Mei JY, Hu Y, Zhou DH, Catto BA (1998) In vitro and in vivo effect of levopraziquantel, dextropraziquantel versus racemic praziquantel on different developmental stages of Schistosoma japonicum. Chin J Parasitol Parasitic Dis 16:335–341
Xiao SH, Hotez P, Tanner M (2000) Artemether, an effective new agent for chemoprophylaxis against shistosomiasis in China: its in vivo effect on the biochemical metabolism of the Asian schistosome. Southeast Asia J Trop Med Public Health 31:724–732
Xiao SH, Chollet J, Utzinger J, Matile H, Mei JY, Tanner M (2001) Artemether administered together with haem in damage schistosomes in vitro. Trans R Soc Trop Med Hyg 95:67–71
Xiao SH, Wu YL, Tanner M, Wu WM, Utizinger J, Mei JY, Scorneaux B, Chollet J, Zhai ZL (2003) Schistosoma japonicum: in vitro effects of artemether combined with haemin depend on cultivation media and appraisal of artemether products appearing in the media. Parasitol Res 89:459–466
Xiao SH, Keiser J, Chollet J, Utzinger J, Dong YX, Endriss Y, Vennerstrom JL, Tanner M (2007) In vitro and in vivo activities of synthetic trioxolanes against major human schistosome species. Antimicrob Agents Chemother 51:1440–144
Xiao SH, Chollet J, Utzinger J, Mei JY, Jiao PY, Keiser J, Tanner M (2009a) Effect of single-dose oral mefloquine on the morphology of adult Schistosoma japonicum in mice. Parasitol Res 105:853–861
Xiao SH, Mei JY, Jiao PY (2009b) Further study on mefloquine concerning several aspects in experimental treatment of mice and hamsters infected with Schistosoma japonicum. Parasitol Res. doi:10.1007/s00436-009-1640-5
Yolles TK, Morre DV, DeGusti DL, Ripsom CA, Meleney MS (1947) A technique for the perfusion of laboratory animals for the recovery of schistosomes. J Parasitol 33:419–426
You JQ, Yue WJ, Xiao XH (1986) Effect of praziquantel in vitro on different developmental stages of Schistosoma japonicum. Acta Pharmacol Sin 7:82–84
Yue WJ, You JQ, Mei JY (1985) Prophylactic activity of praziquantel in animals infected with Schistosoma japonicum. Acta Pharmacol Sin 6:186–188
Zhang CW, Xiao SH, Utzinger J, Chollet J, Keiser J, Tanner M (2009) Histopathological changes in adult Schistosoma japonicum harbored in mice treated with a single dose of mefloquine. Parasitol Res 104:1407–1416
Acknowledgment
This investigation received financial support from the National Institute of Parasitic Diseases, Chinese Center for Disease Control and Prevention (Shanghai, China).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Xiao, Sh., Mei, Jy. & Jiao, Py. The in vitro effect of mefloquine and praziquantel against juvenile and adult Schistosoma japonicum . Parasitol Res 106, 237–246 (2009). https://doi.org/10.1007/s00436-009-1656-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-009-1656-x