Abstract
To date, there is no efficient treatment for cryptosporidiosis and parasite eradication relies on innate and acquired immunity. In this study, we investigated the effect of administration of probiotic bacteria on the development and progression of the experimental infection in suckling rats. Rats were fed daily with 2.107 CFU of Lactobacillus casei-containing mixture, starting 2 days before the infection until the spontaneous clearance of the parasite. Effects on weight gain, parasite burden, mucosal histology and production of mucosal cytokines (IFNγ, IL10 and TNFα) were studied. Although a trend to a more rapid clearance of parasites was noted in rats treated with probiotics, no significant effect of probiotics administration was observed in terms of weight gain, parasite burden, mucosal damage, or kinetics of mucosal cytokines during the course of infection. Overall, our results showed that the daily administration of L. casei-containing mixtures was unable to eradicate the parasite in our model.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cryptosporidium parvum is an Apicomplexa protozoan parasite that infects intestinal epithelial cells of humans and various other mammals causing watery diarrhoea and malabsorption. The infection is more severe in young children and immunocompromised individuals leading to prolonged diarrhoea with major alterations of the intestinal epithelium and malnutrition. In HIV-infected patients, the severity of the infection is directly related to the degree of immunosuppression, leading to chronic infection when CD4 count is below 150/mm3. In contrast, the disease is self-limited in immunocompetent hosts, showing a major role for host defence factors in controlling the infection.
Mucosal immune response, especially IFNγ secretion, is known to play a key role in resistance to C. parvum infection (Ungar et al. 1991; Chen et al. 1993; Kapel et al. 1996; You and Mead 1998). A type 2 response involving IL4 and IL10 has been more recently related to parasite clearance (Lacroix et al. 2001).
Besides the determinant role of immunity, there is clear evidence that colonisation of the intestine by Cryptosporidium depends on the intestinal microflora as newborn mice or adult mice raised in germ-free conditions are far more susceptible to this parasite than conventional adult mice (Harp et al. 1992, 1998). These arguments altogether support the hypothesis that cryptosporidiosis might be controlled by administration of probiotics, which seem able to modulate both innate and acquired immunity at mucosal and systemic levels (Vaarala 2003; Picard et al. 2005). A previous work has already shown the beneficial effect of Lactobacillus reuteri and Lactobacillus acidophilus on Cryptosporidium infection in mice that had been co-infected by the LP-BM5 murine leukaemia virus. However, in this background of profound immunodeficiency, the effect of probiotics on cellular immune response could not be investigated (Alak et al. 1997, 1999). Such preventive or therapeutic approach would be particularly relevant for cryptosporidiosis as paromomycin and nitazoxanide, i.e. the two drugs that can be proposed for treatment of cryptosporidiosis, have only limited efficiency and cannot eradicate the parasite (Smith and Corcoran 2004).
Our objective was to evaluate the effects of administration of probiotics in an immunocompetent host and to focus on the influence of probiotics on the mucosal cellular immunity. The suckling rat model was chosen because it allows a good implantation, development of the parasite without immunosuppression, mucosal immune responses and a natural eradication of the parasite at weaning (Martin-Gomez et al. 2006). Two different mixtures containing various probiotic strains were evaluated.
Materials and methods
Cryptosporidium oocysts
C. parvum oocysts (genotype 2) (gift from M. Naciri, INRA, Nouzilly) were maintained by regular passage in suckling rats (Capet et al. 1999). C. parvum oocysts were purified through sucrose gradient and 1.25% sodium hypochlorite treatment just before inoculation. The viability of the oocysts was measured by DAPI and PI.
The suckling rat model of cryptosporisiosis
Specific-pathogen-free pregnant Sprague–Dawley rats were obtained from Janvier laboratory (Le Genest St Isle, France) and handled according to the regulations of the French Ministry of Agriculture. Food and water were available ad libitum. At D4, pups were infected by gavage with C. parvum oocysts in 100 μl of phosphate-buffered saline (PBS). Animals were then weighed every 2 days until they were killed.
At D6, D8, D10, D12, D16 (or D18) and D21, two pups were killed in each litter by SC pentobarbital injection and the small intestine was removed. It was rinsed free of intestinal content and cut in four sequential 1-cm fragments taken from the cæcum. One fragment was used for histology, one for quantification of C. parvum by real-time polymerase chain reaction (PCR) analysis, one for oocysts detection by Ziehl–Neelsen staining and one for quantitative determination of cytokines mRNA by real-time RT-PCR analysis.
Experimental design
A first experiment was conducted to select the optimum infecting dosage for assessing probiotic efficacy. Animals were infected by either 100, 1,000 or 10,000 oocysts and the kinetics of oocyst shedding were compared. The criteria for this selection were to obtain 100% infection of pups, good reproducibility of parasitic burden and clearance of infection at weaning (D21).
We then evaluated the effect of oral administration of probiotics on the development of C. parvum infection.
A second set of experiments was, thus, conducted with commercial Actimel (Danone, Palaiseau, France) which is a mixture of three bacterial species (MIX) containing 108 CFU/ml of Lactobacillus casei DN-114 001, 107 CFU/ml Lactobacillus bulgaricus and 108 CFU/ml Streptococcus thermophilus. Four different experimental conditions were evaluated and each condition was applied to a minimum of two litters: no infection and no treatment (i.e. control rats, three litters), no infection and daily administration of 200 μl of MIX from D2 until the killing of the rats (two litters), infection at D4 with C. parvum and no probiotic treatment (four litters), infection at D4 and daily administration of 200 μl of MIX from D2 until sacrifice (five litters). The selected dose of probiotics has already proven effective against rotavirus-induced diarrhoea in suckling rats (Guerin-Danan et al. 2001).
In a third set of experiments, we evaluated the effect of VSL#3 (Sigma Tau, MD, USA), which is a mixture of L. acidophilus, L. casei, Lactobacillus plantarum, L. bulgaricus, Bifidobacterium longum, Bifidobacterium breve, Bifidobacterium infantis and S. thermophilus. The concentration was adjusted to 4.108 CFU/ml in PBS and 50 μl (2.107 CFU) of the probiotic was administrated daily from D2 to sacrifice. Each experimental condition was evaluated with one litter.
Weight gain
The weight gain of the suckling rats has been calculated from D6 to D21 for each litter and for each experimental condition as the ratio: (weight at a given day/weight at D4) × 100.
Mucosal parasite burden quantification
Mucosal parasite burdens were estimated using Ziehl–Neelsen staining and C. parvum real-time PCR.
Ziehl–Neelsen staining
The third small intestine fragment taken from the cæcum was cleaned free of intestinal content, weighed and homogenised in 10 vol of PBS using a glass tissue grinder (VWR, Fontenay-sous-Bois, France). Ten microliters of this solution was smeared onto a glass slide then stained according to a modified Ziehl–Neelsen method (Henriksen and Pohlenz 1981). Oocysts were numerated on the whole slide and results were expressed as oocysts number/milligram of tissue.
C. parvum real-time PCR
The second intestine fragment taken from the cæcum was cleaned free of intestinal content and weighed and the DNA was extracted by use of the High Pure PCR Template Preparation kit (Roche, Meylan, France). Oocysts lysis was performed by incubating the sample with proteinase K and tissue lysis buffer overnight at 55°C. The extracted DNA was stored in elution buffer at −20°C. A 145-bp fragment of the 18S rRNA gene was amplified by real-time quantitative PCR using primers with the following sequence: 5′-AGCTCGTAGTTGGATTTCTGTTAATAATTTA-3′ and 5′-GCATATGCCTGCTTTAAGCACTCT-3′ (Fontaine and Guillot 2003) and a TaqMan MGB (Minor Groove Binder) probe with the following sequence: 5′-TTTCTCAAAGTAAAATTTCA-3′. Real-time PCR was performed by using the Applied Biosystems 7500 thermal cycler (Applied Biosystems, Foster City, CA, USA). Quantification was allowed by using serial dilution of a quantified TOPO plasmid containing the 145-bp fragment. Results were expressed as the number of copies of 18S rRNA gene/milligram of tissue.
Histological studies
Histological studies were performed on the first small intestine fragment taken from the cæcum. Tissues collected from freshly dissected rat small intestine were fixed in ethylic alcohol/formalin/acetic acid/distilled water fixative (75/2/5/18) (AFA, Labonnord, Templemars, France) for 2 h at room temperature then in PBS at 4°C until embedding. After paraffin embedding, sections were cut at a thickness of 2 μm and stained with hematoxylin–eosin. For each animal, villous height and crypt depth were measured in five well-orientated villi using a micrometer.
Mucosal cytokine analysis
The fourth intestinal fragment taken from the cæcum was cleaned of intestinal content then used for quantification of IFNγ, IL10, TNFα and β-actin mRNAs. The fragment was immediately immerged in RNAlater, RNA stabilisation reagent, (Qiagen, Hilden, Germany) after small intestine dissection. mRNAs were extracted using the RNeasy mini-kit (Qiagen), with an initial incubation of the sample in 1% β-mercaptoethanol-added buffer RLT (Qiagen) and proteinase K overnight at 55°C. mRNAs were eluted in RNase-free water and stored at −80°C. The reverse transcription was done using the High Capacity cDNA Archive kit (Applied Biosystems). The reverse transcription program, performed on the GeneAmp PCR System 9700 thermal cycler (Applied Biosystems), was 37°C for 2 h. Real-time PCR was performed by using the Applied Biosystems 7500 thermal cycler. To normalise the results, IFNγ, IL10, TNFα and β-actin mRNAs from each sample were quantified in the same run, using β-actin as reference. Results were expressed through \(2^{{ - \Delta \Delta Ct}} \) (Livak and Schmittge 2001), with the control ΔCt being the mean of the control litters at D6. This enabled the comparison of the kinetics of mRNA expression using this mean as base value.
Statistical study
The weight gain slopes recorded for each treatment group and in controls were compared using mixed model analysis of variance (ANOVA) with linear and quadratic effects of time, fixed group effect and interactions. Random litter effects, slopes and quadratic effects were considered to account for correlation between weights in the same litter. Mean parasite burdens, villous height, crypt depth and mucosal cytokine levels were determined from D6 to D22. For each parameter, the areas under curves (AUC) were calculated and compared by two-way ANOVA.
The Fisher exact test was used to compare the numbers of infected animals in treatment and control groups.
In the experiment using VSL#3, the Student test was used to compare the mean parasite burdens at the peak of infection in treated rats and in untreated controls.
All tests were two-sided at the 0.05 significance level. Analyses were performed using R 2.0.1 statistical software (The R Development Core Team).
Results
The results of preliminary experiments using different sizes of inoculum led to select an inoculum of 1,000 oocysts as it resulted in 100% infection, reproducible kinetics of parasite burdens and clearance of infection at D21, whereas a lower inoculum was not infective for all rats (data not shown). All subsequent experiments were performed with an inoculum of 1,000 oocysts, with a range of oocyst viability between 54 and 56% as assessed by PI/DAPI staining.
Weight gain
Despite the absence of overt diarrhoea, C. parvum-infected rats had a significantly lower weight gain compared with uninfected control rats (p= 0.014). Administration of MIX did not modify the weight gain curve neither on control rats (p=0.99) nor on C. parvum-infected rats (p=0.63) (Fig. 1). As for MIX treatment, VSL#3 treatment failed to show any beneficial effect on the weight gain in C. parvum-infected rats (p=0.65).
Mucosal parasite burden quantification
The kinetics of parasite burdens in infected rats is presented on Fig. 2. In untreated infected rats, parasites were detected at D6. Parasite burden progressively increased until a peak value at D12 and then decreased to undetectable value by Ziehl–Neelsen staining at D21. A similar kinetics of parasite burdens was observed with Ziehl–Neelsen staining and C. parvum real-time PCR. However, C. parvum 18S rRNA gene copies could still be detected at D21. No significant difference in the parasitic burdens was observed between C. parvum-infected rats and those infected that have been fed daily with 200 μl of MIX. Results were similar whether mucosal parasite burden were determined by Ziehl–Neelsen staining or by real-time PCR (p=0.55 and 0.76, respectively). However, we noticed that parasite clearance (no parasite detected by Ziehl–Neelsen staining) was obtained in six of ten and four of six of treated animals at D16 and D18, respectively, compared to two of six and one of four of untreated controls at the same dates. Although nonsignificant (p=0.23), this difference indicates a tendency to a more rapid parasite clearance in L. casei-fed rats.
Kinetics of intestinal parasitic loads in C. parvum-infected rats (D4) either not treated (four litters, △) or treated with 200 μl of MIX from D2 until they were killed (five litters, ■). Parasitic load was measured by Ziehl–Neelsen staining (a) and real-time PCR (b). Two rats par litter were killed for each time point. Results are presented as mean±SD
No significant effect of VSL#3 was observed between D6 and D12 with p=0.73 and p=0.62 for parasitic burdens measured by Ziehl–Neelsen and real-time PCR, respectively (data not shown).
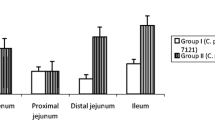
Histological analysis
Mild mucosal lesions were observed in the small intestine of C. parvum-infected rats compared to uninfected controls. A significant villous atrophy starting from D10 was observed in the distal part of the intestine (p=0.013, compared to controls). Villous were blunt, shorter and wider than normal and crypts were elongated but not significantly (p=0.12) compared with control rats. Administration of MIX to C. parvum-infected rats did not significantly modify these damages (p=0.31 and p=0.37 for villous length and crypts depth, respectively).
Mucosal cytokine analysis
A nonsignificant increase in mucosal IFNγ mRNA expression was observed in C. parvum-infected rats (p=0.14) compared with uninfected control rats (Table 1). Daily administration of MIX did not significantly modify IFNγ mRNA expression neither in control rats (p=0.30) nor in C. parvum-infected rats (p=0.78). No significant difference in IL10 mRNA expression (p=0.62) and TNFα mRNA expression (p=0.82) was observed in C. parvum-infected rats as compared to uninfected controls. Daily administration of MIX did not modify mucosal IL10 and TNFα mRNA expression compared with control rats (p=0.96 and p=0.41 for IL10 and TNFα, respectively). Furthermore, there was no significant effect of MIX administration on the expression of these two cytokines in C. parvum-infected rats (p=0.75 and p= 0.25 for IL10 and TNFα, respectively).
Discussion
In humans, one single report suggests a benefit of administration of probiotics in a case of cryptosporidiosis occurring in a patient with celiac disease (Pickerd and Tuthill 2004). In a recent clinical trial performed in Peru, Salazar-Lindo et al. (2004) found no beneficial effect after administration of a milk formula containing Lactobacillus GG in infants presenting acute diarrhoea due to various microbial agents, including C. parvum.
Using the suckling rat model of cryptosporidiosis, we failed to demonstrate a significant activity of oral administration of two different mixtures of probiotics on the kinetics of intestinal C. parvum burdens or on mucosal damage although we noticed a trend to a shorter duration of infection in L. casei-fed animals. This low level of protection had to be related to the absence of significant increase in mucosal cytokines production, especially IFNγ, during the course of infection. This was observed despite experimental conditions that have been designed to identify a mild activity on infection and local immunity.
This low activity of probiotics treatment is surprising in regard to previous published data on the beneficial effect of some probiotics on infectious diarrhoea (Szajewska and Mrukowicz 2001; Allen et al. 2004; Picard et al. 2005) and the use of a treatment dosage that proved efficient in a neonatal rat model of rotavirus-induced diarrhoea (Guerin-Danan et al. 2001). However, data are very limited for parasitic diarrhoea and rather concern extracellular parasites such as Giardia. Moreover, it should be stressed that, for most of these studies, probiotic treatment did not eradicate the parasite but resulted in a moderate benefit with decrease in parasite burden and mucosal damage and that these results were obtained after long-term feeding (7–28 days) or prolonged prefeeding (≥7 days) before infection (Szajewska and Mrukowicz 2001; Santos et al. 2004; Benyacoub et al. 2005; Humen et al. 2005). Very few experimental data document the efficacy of probiotics on C. parvum infection. In a model of cryptosporidiosis developed in adult mice that had been infected with the LP-BM-5 murine leukemia virus (“murine AIDS”), Alak et al. (1997, 1999) showed the beneficial effect of a prophylactic and prolonged daily administration of L. reuteri and L. acidophilus, (i.e. from day 13 before C. parvum infection until the end of experiment). In this model, oocyst shedding was reduced from day 7 to 14 after infection. However, this beneficial effect was not associated with a restoration of T-helper type 1 cytokines production. The use of suckling rats in our model indeed did not allow such long-term preventive treatment. We, therefore, cannot rule out its efficacy in other experimental conditions. However, other anti-cryptosporidial treatment such as oral administration of hyper-immune colostrums has been proven efficient in a similar model (Martin-Gomez et al. 2005). It is also possible that bacteria were not able to colonise the gut of our animals in the presence of protozoan pathogens. The nature of the administered probiotic might also be determinant for a therapeutic or prophylactic effect. In our study, we selected a probiotic mixture containing L. casei as it was reported effective in other studies on infectious diarrhoea and in human. In the absence of significant benefit of this mixture, the efficacy of VSL#3, i.e. a mixture of eight bacteria which was shown to be efficient in inflammatory bowel disease (Mimura et al. 2004), was examined but it also yielded negative results.
Finally, we failed to reveal a significant activity of L. casei-containing mixture against cryptosporidiosis under our experimental conditions. However, we cannot rule out some effect in other conditions, such as a prolonged administration before infection and in hosts with a mature gut flora and immune system.
References
Alak JI, Wolf BW, Mdurvwa EG, Pimentel-Smith GE, Adeyemo O (1997) Effect of Lactobacillus reuteri on intestinal resistance to Cryptosporidium parvum infection in a murine model of acquired immunodeficiency syndrome. J Infect Dis 175:218–221
Alak JI, Wolf BW, Mdurvwa EG, Pimentel-Smith GE, Kolavala S, Abdelrahman H, Suppiramaniam V (1999) Supplementation with Lactobacillus reuteri or L. acidophilus reduced intestinal shedding of Cryptosporidium parvum oocysts in immunodeficient C57BL/6 mice. Cell Mol Biol 45:855–863
Allen SJ, Okoko B, Martinez E, Gregorio G, Dans LF (2004) Probiotics for treating infectious diarrhoea. Cochrane Database Syst Rev 2:CD003048
Benyacoub J, Perez PF, Rochat F, Saudan KY, Reuteler G, Antille N, Humen M, De Antoni GL, Cavadini C, Blum S, Schiffrin EJ (2005) Enterococcus faecium SF68 enhances the immune response to Giardia intestinalis in mice. J Nutr 135:1171–1176
Capet C, Kapel N, Huneau JF, Magne D, Laikuen R, Tricottet V, Benhamou Y, Tomé D, Gobert JG (1999) Cryptosporidium parvum infection in suckling rats: impairment of mucosal permeability and Na(+)-glucose cotransport. Exp Parasitol 91:119–125
Chen W, Harp JA, Harmsen AG (1993) Requirements for CD4+ cells and gamma interferon in resolution of established Cryptosporidium parvum infection in mice. Infect Immun 61:3928–3932
Fontaine M, Guillot E (2003) Study of 18S rRNA and rDNA stability by real-time RT-PCR in heat-inactivated Cryptosporidium parvum oocysts. FEMS Microbiol Lett 226:237–243
Guerin-Danan C, Meslin JC, Chambard A, Charpilienne A, Relano P, Bouley C, Cohen J, Andrieux C (2001) Food supplementation with milk fermented by Lactobacillus casei DN-114 001 protects suckling rats from rotavirus-associated diarrhea. J Nutr 131:111–117
Harp JA, Chen W, Harmsen AG (1992) Resistance of severe combined immunodeficient mice to infection with Cryptosporidium parvum: the importance of intestinal microflora. Infect Immun 60:3509–3512
Harp JA, Wannemuehler MW, Woodmansee DB, Moon HW (1998) Susceptibility of germfree or antibiotic-treated adult mice to Cryptosporidium parvum. Infect Immun 56:2006–2010
Henriksen SA, Pohlenz JF (1981) Staining of cryptosporidia by a modified Ziehl-Neelsen technique. Acta Vet Scand 22:594–596
Humen MA, De Antoni GL, Benyacoub J, Costas ME, Cardozo MI, Kozubsky L, Saudan KY, Boenzli-Bruand A, Blum S, Schiffrin EJ, Perez PF (2005) Lactobacillus johnsonii La1 antagonizes Giardia intestinalis in vivo. Infect Immun 73:1265–1269
Kapel N, Benhamou Y, Buraud M, Magne D, Opolon P, Gobert JG (1996) Kinetics of mucosal ileal gamma-interferon response during cryptosporidiosis in immunocompetent neonatal mice. Parasitol Res 82:664–667
Lacroix S, Mancassola R, Naciri M, Laurent F (2001) Cryptosporidium parvum-specific mucosal immune response in C57BL/6 neonatal and gamma interferon-deficient mice: role of tumor necrosis factor alpha in protection. Infect Immun 69:1635–1642
Livak KJ, Schmittge TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods 25:402–408
Martin-Gomez S, Alvarez-Sanchez MA, Rojo-Vazquez FA (2005) Oral administration of hyperimmune anti-Cryptosporidium parvum ovine colostral whey confers a high level of protection against cryptosporidiosis in newborn NMRI mice. J Parasitol 91:674–678
Martin-Gomez S, Alvarez-Sanchez M, Rojo-Vazquez F (2006) A newborn mouse Cryptosporidium parvum infection model: its application to the study of therapeutic and prophylactic measures for controlling cryptosporidiosis in ruminants. Parasitol Res Jan 31:1–6
Mimura T, Rizello F, Helwig U, Poggioli G, Schreiber S, Talbot IC, Nicholls RJ, Gionchetti P, Campieri M, Kamm RA (2004) Once daily high dose probiotic therapy (VSL#3) for maintaining remission in recurrent or refractory pouchitis. Gut 53:108–114
Picard C, Fioramonti J, Francois A, Robinson T, Neant F, Matuchansky C (2005) Bifidobacteria as probiotic agents—physiological effects and clinical benefits. Aliment Pharmacol Ther 22:495–512
Pickerd N, Tuthill D (2004) Resolution of cryptosporidiosis with probiotic treatment. Postgrad Med J 80:112–113
Salazar-Lindo E, Miranda-Langschwager P, Campos-Sanchez M, Chea-Woo E, Sack RB (2004) Lactobacillus casei strain GG in the treatment of infants with acute watery diarrhea: a randomized, double-blind, placebo controlled clinical trial [ISRCTN67363048]. BMC Pediatr 4:18
Santos Jde F, Vasconcelos J, de Souza JR, Coutinho Ede M, Montenegro SM, Azevedo-Ximenes E (2004) The effect of Zymomonas mobilis culture on experimental Schistosoma mansoni infection. Rev Soc Bras Med Trop 37:502–504
Smith HV, Corcoran GD (2004) New drugs and treatment for cryptosporidiosis. Curr Opin Infect Dis 17:557–564
Szajewska H, Mrukowicz JZ (2001) Probiotics in the treatment and prevention of acute infectious diarrhea in infants and children: a systematic review of published randomized, double-blind, placebo-controlled trials. J Pediatr Gastroenterol Nutr 33:S17–S25
Ungar BL, Kao TC, Burris JA, Finkelman FD (1991) Cryptosporidium infection in an adult mouse model. Independent roles for IFN-gamma and CD4+ T lymphocytes in protective immunity. J Immunol 147:1014–1022
Vaarala O (2003) Immunological effects of probiotics with special reference to lactobacilli. Clin Exp Allergy 33:1634–1640
You X, Mead JR (1998) Characterization of experimental Cryptosporidium parvum infection in IFN-gamma knockout mice. Parasitology 117:525–531
Acknowledgements
We gratefully acknowledge the assistance of Stéphanie Belhadj and Luc Legrès (Service Commun de Pathologie des Modèles Animaux, IFR 105, hôpital Saint-Louis) for histological analysis and of Dr. Annie Sulahian for critical reading of this manuscript. All the experiments presented in this study comply with the current laws in France.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guitard, J., Menotti, J., Desveaux, A. et al. Experimental study of the effects of probiotics on Cryptosporidium parvum infection in neonatal rats. Parasitol Res 99, 522–527 (2006). https://doi.org/10.1007/s00436-006-0181-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-006-0181-4