Abstract
Background
The abnormality of bone marrow-derived mesenchymal stem cells (BM-MSCs) has been reported to contribute to the pathogenesis of acute myeloid leukemia (AML). T cell immunodeficiencies play important roles in the progression of leukemia. This study investigated the effect of CD4+ T cells from AML patients on the proliferation of BM-MSCs.
Methods
The growth rate of BM-MSCs from AML patients and healthy donor was compared. CD4+ T cells were separated and identified from AML patients. Through co-culturing CD4+ T cells from AML patients and BM-MSCs from healthy, we detected the proliferation of BM-MSCs from healthy by MTT assay. qRT-PCR was performed to examine the expression of miR-10a. Luciferase reporter assay was used to analyze the regulation of miR-10a on the expression of BCL6.
Results
Here, we observed that BM-MSC from AML patients grew slower than that from healthy. CD4+ T cells from AML patients inhibited the proliferation of BM-MSCs through secreting miR-10a. In addition, miR-10a was found to target BCL6 and regulated its expression in transcription and translation levels. Correlation analysis revealed that the level of miR-10a in serum of AML patients was negatively correlated with BCL6 in BM-MSC.
Conclusion
This study provides evidence that CD4+ T cells from AML patients suppress the proliferation of BM-MSCs via secreting miR-10a.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute myeloid leukemia (AML) is a progressive and malignant cancer characterized by the rapid proliferation and accumulation of clonal leukemia cells, which disturbs normal hematopoiesis and causes marrow failure (Ferrara and Schiffer 2013). AML commonly occurs in the bone marrow, and several cells participate in the pathogenesis of AML, such as mesenchymal stromal cells (MSCs), adipocytes, endothelial cells (EC), monocytes and fibroblasts (Huang et al. 2015). Among them, MSCs are important non-hematopoietic progenitors with the capacity to differentiate toward multiple mature cell types (Dominici and Blanc 2006). In addition, MSCs have been shown to protect tumor cells against the effects of chemotherapy (Houthuijzen et al. 2012). However, the mechanisms of the alterations observed in MSCs from patients with leukemia remain unclear.
Recent studies have revealed that T cell immunodeficiencies are common characteristics in hematological malignancies and play an important role in leukemia progression and promote the expansion of malignant clones (Shi et al. 2015). In addition, immunosuppressive microenvironment in the bone marrow where both innate and adaptive immune responses are profoundly dysregulated sustains and modulates the proliferation, survival and drug resistance of AML (Isidori et al. 2014). Mounting evidence indicated that regulatory T cell (Treg) which comprises 5–10 % of peripheral CD4+ T cells mediates vigorous suppression via contact-dependent and contact-independent mechanisms (Szczepanski et al. 2009). It has been shown that the prevalence of CD4+, CD25high and Treg in the peripheral blood of AML patients is increased in comparison with normal individuals (Wang et al. 2005).
To date, increasing research has demonstrated that various microRNAs (miRNAs) expression signatures are involved in the clinical heterogeneity of AML. The dysregulation of miRNAs generally contributes to multiple processes including cell apoptosis, proliferation, cell-cycle regulation and invasion in various diseases. Recently, miR-10a was found to have significantly different expression levels in nucleophosmin-mutated AML patients (Havelange et al. 2014). Through analysis of the association of miR-10a expression with the clinical characteristics at diagnosis in AML patients, miR-10a might be served as a biomarker for AML (Zhi et al. 2015). Hayato Takahashi et al. (2012) indicated that miR-10a attenuated phenotypic conversion of regulatory T cells to helper T cells through targeting BCL-6. In this study, we measured the effect of CD4+ T cell from AML patients on the growth of MSCs from healthy control and investigated the significances of miR-10a in this process.
Materials and methods
Isolation and expansion of patients’ MSCs from bone marrow
The study was approved by the Ethic Committee of Qilu Hospital of Shandong University, and written informed consent was obtained from subjects. MSC cultures were obtained from BM aspirates of 20 AML patients and 20 healthy donors following marrow harvests. Total nucleated cells were obtained and washed, and then cells were resuspended in low-glucose Dulbecco’s modified Eagle’s medium containing 15 % FBS and seeded at 1.3 × 105 cells/cm2 in T-75-cm2 plastic tissue flasks. Cell cultures underwent medium change weekly and were maintained in the same culture dish until plastic-adherent spindle-shaped cells were observed. When cell cultures reached 80 % confluency, cells were trypsinized and harvested for further passaging. Cell numbers and viability were checked after every passage using trypan blue and a hemocytometer under an inverted light microscope.
Flow cytometry
The surface expression on BM-MSC was tested by flow cytometry using R-phycoerythrin-conjugated anti-CD14, anti-CD73, allophycocyanin-conjugated anti-CD90, CD34 or CD45, biotin-conjugated anti-CD19, PerCP Cy5-5-conjugated anti-CD105 and PerCp-conjugated anti-HLA-DR. Surface markers of CD4+ T cells were evaluated by FACS Canto, Calibur or Verse (BD).
MTT assay
The MTT (3-(3,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) assay was performed as described previously (Stölzel et al. 2010). The absorbance was measured with a spectrophotometer (Bio-Rad Laboratories, CA, USA).
Western blot analysis
Proteins were isolated and separated on 12 % acrylamide gels. Nitrocellulose membranes (Takara, Dalian, China; diluted 1:500) were incubated with primary antibodies specific for BCL6 overnight at 4 °C. Blots were washed and incubated with horseradish peroxidase-goat anti-mouse secondary antibodies (Takara, Dalian, China; diluted 1: 2000). Western blots were developed by chemiluminescence using the ECL Plus chemiluminescence detection kit (Takara, Dalian, China).
Quantitative real-time PCR
Total RNA was extracted with the miRNeasy RNA isolation kit following the manufacturer’s protocol. For miRNA quantitative analysis, RNA was reverse-transcribed using the miscript system with NCode™ SYBR ® Green miRNA quantitative real-time PCR (qRT-PCR) kit (Invitrogen, Carlsbad, CA, USA). All qRT-PCR was performed with the Bio-Rad CFX96. Real-time PCR arrays were acquired from SABiosciences and performed according to manufacturer’s instructions. Each sample was analyzed by the comparative threshold cycle (Ct) method. The expression levels of miR-10a were normalized to U6, and the expression levels of BCL6 were normalized to GAPDH.
Cell transfection and luciferase reporter assays
Cells were transfected with miR-10a mimic/inhibitor or control with Lipofectamine 2000 (Invitrogen, CA, USA) according to the manufacturer’s instruction. Cells were harvested after 48 h for following experiments. For luciferase reporter assays, BM-MSC cells were seeded in 24-well plates and transfected with recombinant vectors plus miR-10a mimic/inhibitor with Lipofectamine 2000. Firefly and Renilla luciferase activities were measured 24 h later using the dual-luciferase reporter assay system from cell lysates.
Statistical analysis
Data were expressed as mean ± SD. Statistical significance was determined by Student’s t test. A p value <0.05 was considered significant.
Results
The growth of AML BM-MSCs and healthy BM-MSCs was compared
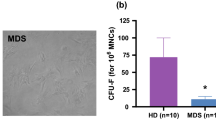
As BM-MSCs play a fundamental role in AML pathogenesis, we compared the morphology and characterization of BM-MSCs from AML patients and healthy control. According to the results in Fig. 1a, we found that AML BM-MSCs appeared to be more sparse and heterogeneous in morphology under light microscopy compared with healthy BM-MSCs. Surface marker expression of AML BM-MSCs and healthy BM-MSCs was measured by flow cytometry, such as the positive makers of CD73, CD90 and CD105, and the negative makers of CD45, CD14, CD19, CD34 and HLA-DR. As shown in Fig. 1b, BM-MSCs from AML patients and healthy donors expressed comparable amounts of these surface markers. The positive rates of both were over 98 %, and negative rates of both were below 2 %. In addition, we observed that BM-MSC from AML grew slower than that from healthy people (Fig. 1c). However, the reason is unknown.
Growth of AML BM-MSCs and healthy BM-MSCs was compared. a The morphology of AML BM-MSCs and healthy BM-MSCs was detected. b Surface marker expression of AML BM-MSCs and healthy BM-MSCs was determined by flow cytometry. c Cell proliferation curve of AML BM-MSCs and healthy BM-MSCs was analyzed. Data represent the mean ± SD. **p < 0.01 versus control
CD4+ T cells from AML patients secrete miR-10a and inhibit the proliferation of BM-MSCs
CD4+ T cells from AML patients were separated and purified with magnetic beads and analyzed by flow cytometry. It has been shown that 86.5 % of the cells were CD4+ T cells (Fig. 2a). To explore the effect of CD4+ T cells from AML patients on the proliferation of BM-MSCs, CD4+ T cells from AML patients and BM-MSCs from healthy donors were co-cultured in different ratio (0:1, 5:1, 10:1 and 20:1). After removing the suspended T cells, cell proliferation of BM-MSCs was detected by MTT assay. As shown in Fig. 2b, the concentration of BM-MSCs treated with CD4+ T cells was considerably lower than that treated with none. In addition, this reduction was in a concentration-dependent manner of T cells. We further detected the expression of miR-10a in T cells from AML patients and healthy donors. MiR-10a was highly expressed in T cells from AML patients (Fig. 2c). To analyze the effect of miR-10a on the growth of BM-MSCs from healthy donors, BM-MSCs were transfected with miR-10a mimic or miR-10a inhibitor or the corresponding control. It has been shown that miR-10a mimic strongly inhibited the growth of BM-MSCs and miR-10a inhibitor highly enhanced its growth (Fig. 2d).
CD4+ T cells from AML patients secreted miR-10a and inhibited the proliferation of BM-MSCs. a Flow cytometry was performed to identify the purity of T cells separated from leukemia patients. b CD4+ T cells from AML patients co-cultured with healthy BM-MSCs in different ratio (0:1, 5:1, 10:1 and 20:1). Then, CD4+ T cells suspended in BM-MSCs were removed at 0, 12, 24 and 48 h. The proliferation of BM-MSCs was detected through MTT assay. c The expression of miR-10a was examined in CD4+ T cells from AML patients and healthy control. d The effect of miR-10a on the proliferation of healthy BM-MSCs. Data represent the mean ± SD. **p < 0.01; #p < 0.01 versus mimic control
CD4+ T cells from AML patients inhibit the proliferation of BM-MSCs through secreting miR-10a
To detect the role of miR-10a in the suppressed effect of CD4+ T cells from AML patients on the BM-MSCs proliferation, T cells from AML patients were transfected with miR-10a antagomir or its control. After 24 h, qRT-PCR revealed that miR-10a antagomir significantly reduced the expression of miR-10a in T cells comparing to the control (Fig. 3a). Then, we examined the MSCs growth which were treated with the supernatant of T cells from AML patients transfected with miR-10a antagomir or its control. As shown in Fig. 3b, T cells from AML patients highly inhibited the growth of MSCs. Furthermore, the inhibited extend of T cells transfected with antagomir control was stronger than that with miR-10a antagomir. These data indicated that CD4+ T cells from AML patients inhibited the proliferation of BM-MSCs through secreting miR-10a.
CD4+ T cells from AML patients inhibited the proliferation of BM-MSCs through secreting miR-10a. a The effect of miR-10a antagomir on the expression of miR-10a secreted by CD4+ T cells from AML patients. b The effect of supernatant of T cells transfected with miR-10a antagomir on the proliferation of BM-MSCs. Data represent the mean ± SD. **p < 0.01 versus MSC only; #p < 0.01 versus antagomir control
MiR-10a targets to BCL6
Through the bioinformatics prediction, we found that miR-10a could bind to the 3′-UTR of BCL6 (Fig. 4a). To detect the effect of miR-10a on the expression of BCL6, BM-MSCs from healthy donors were transfected with miR-10a mimic, miR-10a inhibitor and the controls. After 24 h, we analyzed the mRNA level of BCL6 and found that miR-10a mimic significantly decreased the mRNA level of BCL6 in BM-MSCs. In addition, miR-10a inhibitor enhanced the mRNA level of BCL6 (Fig. 4b). We further constructed the luciferase report containing 3′-UTR of BCL6 and co-transfected into BM-MSCs from healthy donors with miR-10a mimic or miR-10a inhibitor. The luciferase assay indicated that higher luciferase activity of 3′-UTR of BCL6 was observed in BM-MSCs transfected with miR-10a inhibitor (Fig. 4c). The protein level of BCL6 was detected by Western blot and demonstrated that miR-10a mimic also reduced the protein level of BCL6 in BM-MSCs (Fig. 4d). These findings showed that miR-10a targeted to BCL6 and regulated its expression in transcription and translation levels.
MiR-10a targeted to BCL6. a The prediction of the binding of miR-10a to BCL6. b The effect of miR-10a mimic and miR-10a inhibitor on the expression of BCL6 in healthy BM-MSCs. c The luciferase activity of BCL6 3′-UTR reporter in healthy BM-MSCs transfected with miR-10a mimic or miR-10a inhibitor. d The protein level of BCL6 in healthy BM-MSCs transfected with miR-10a mimic or miR-10a inhibitor. Data represent the mean ± SD. **p < 0.01; #p < 0.01 versus mimic control
The level of miR-10a in serum of AML patients is negatively correlated with BCL6 in BM-MSCs
Based on the above results, we detected the mRNA level of miR-10a in serum from AML patients and healthy donors. Comparing to the miR-10a level in serum from the healthy donors, the miR-10a level was greatly higher in AML patients (Fig. 5a). On the other hand, the mRNA level of BCL6 in BM-MSCs from AML patients was highly lower than that from healthy donors (Fig. 5b). To further detect the relationship between miR-10a and BCL6 level, correlation analysis was performed and revealed that the level of miR-10a in serum of AML patients was negatively correlated with BCL6 in BM-MSCs (Fig. 5c).
Level of miR-10a in serum of AML patients was negatively correlated with BCL6 in BM-MSCs. a The expression of miR-10a in serum from AML patients (n = 20) or healthy control (n = 20). b The mRNA level of BCL6 in AML BM-MSCs (n = 20) and healthy BM-MSCs (n = 20). c The correlation analysis between the level of miR-10a and BCL6. Data represent the mean ± SD
Discussion
In the present report, we examined the morphologic characteristics of MSCs derived from patients suffering AML in comparison with healthy MSCs. Consistent with the previous results, we found that the growth of healthy BM-MSCs was significantly faster than AML BM-MSCs (Huang et al. 2015). In addition, the CD4+ T cells from AML patients could secrete miR-10a and suppressed the growth of BM-MSCs from healthy. Moreover, we further observed that CD4+ T cells from AML patients inhibited the proliferation of BM-MSCs through secreting miR-10a.
Previous studies have described that marrow-derived MSCs have increased capacity to support hematopoiesis and express higher levels of HSC maintenance genes (Méndez-Ferrer et al. 2010). Stromal progenitors can also protect leukemic cells and other tumor cells. Recently, Huang et al. (2015) have reported that BM-MSCs from AML patients demonstrated cytogenetic aberrations either distinct from or overlapping with their corresponding leukemic blasts. Through comparing the functions and gene expression patterns of BM-MSCs from healthy donors and patients with AML, Chandran et al. (2015) found that MSCs from AML patients had heterogeneous morphology and displayed a wide range of proliferation capacity compared with MSCs from healthy controls. This evidence indicated that the abnormalities of MSCs in BM microenvironment may contribute to AML pathogenesis.
T cell immunodeficiency plays an important role in cancer and leukemia progression and promotes the expansion of malignant clones. It has been demonstrated that T cells showed the cytotoxicity in AML patients ( 2015). They may also impair antitumor immune responses that are known to be directed at least partly against auto-antigens expressed by the tumor cells (Greiner et al. 2008). In this study, we investigated the effect of CD4+ T cells from AML patients on the proliferation of BM-MSCs from healthy. Through co-culturing CD4+ T cells from AML patients and BM-MSCs from healthy, we observed that CD4+ T cells from AML patients significantly suppressed the proliferation of BM-MSCs from healthy. To elucidate the potential mechanism of the function of CD4+ T cells for inhibiting the growth of BM-MSCs from healthy, we detected the expression of miR-10a.
Altered expression of miR-10 family members is found to be implicated in malignant transformation of several human malignancies, such as breast cancer, glioblastoma, neurofibromatosis, hepatocellular carcinoma and pancreatic cancer (Zhang et al. 2006; Ciafre et al. 2005; Chai et al. 2010; Varnholt et al. 2008; Bloomston et al. 2007). In AML, miR-10a-5p which belonged to miR-10 family was identified as one of the six up-regulated miRNAs according to the report of Zhi et al. (2013). Bryant et al. ( 2012) have suggested that highly overexpressed miR-10a-5p was observed in nucleophosmin-1 mutated-AML. Moreover, the expression of hsa-miR-10a miRNA is down-regulated in chronic myeloid leukemia patients and that hsa-miR-10a regulates the expression of USF2 (Agirre et al. 2008). Here, in this study, miR-10a was secreted by CD4+ T cells from AML patients and inhibited the proliferation of BM-MSCs from healthy. In addition, miR-10a antagomir attenuated the suppressed effect of T cells on the growth of MSCs. To further elucidate the regulation of miR-10a in AML patients, bioinformatics prediction revealed that miR-10a could bind to the 3′-UTR of BCL6. BCL6 was also identified as the biomarkers and therapeutic targets in adult B-acute lymphoblastic leukemia, whose blockade or loss of function suppressed proliferation and survival of MLL rearrangements leukemia cells (Geng et al. 2012). BCOR, the BCL6 corepressor, is a pivotal transcriptional regulator of early embryonic development, mesenchymal stem cell function and hemopoiesis (Zagaria et al. 2014). We showed that the level of miR-10a in serum of AML patients was negatively correlated with BCL6 in BM-MSCs.
In summary, our report describes the suppressed function of CD4+ T cells from AML patients on the proliferation of BM-MSCs from healthy. Further, these abnormalities are implicated in the abnormal expression of miR-10a. Finally, we identified BCL6 to be a target of miR-10a in patients with AML. Based on these studies, the clinical impact of T cells and miR-10a in AML warrants further investigations. These findings may have implications in the understanding of AML, establishing management strategies and estimating prognosis.
References
Agirre X et al (2008) Down-regulation of hsa-miR-10a in chronic myeloid leukemia CD34+ cells increases USF2-mediated cell growth. Mol Cancer Res 6(12):1830–1840
Bryant A et al (2012) miR-10a is aberrantly overexpressed in Nucleophosmin1 mutated acute myeloid leukaemia and its suppression induces cell death. Mol Cancer 11:8
Bloomston M et al (2007) MicroRNA expression patterns to differentiate pancreatic adenocarcinoma from normal pancreas and chronic pancreatitis. JAMA 297(17):1901–1908
Chai G et al (2010) MicroRNA-10b regulates tumorigenesis in neurofibromatosis type 1. Cancer Sci 101(9):1997–2004
Chandran P et al (2015) Mesenchymal stromal cells from patients with acute myeloid leukemia have altered capacity to expand differentiated hematopoietic progenitors. Leuk Res 39(4):486–493
Ciafre S et al (2005) Extensive modulation of a set of microRNAs in primary glioblastoma. Biochem Biophys Res Commun 334(4):1351–1358
Dominici M, Blanc KL (2006) Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 8(4):315–317
Ferrara F, Schiffer CA (2013) Acute myeloid leukaemia in adults. The Lancet 381(9865):484–495
Geng H et al (2012) Integrative epigenomic analysis identifies biomarkers and therapeutic targets in adult B-acute lymphoblastic leukemia. Cancer Discov 2(11):1004–1023
Greiner J et al (2008) Leukemia-associated antigens are critical for the proliferation of acute myeloid leukemia cells. Clin Cancer Res 14(22):7161–7166
Havelange V et al (2014) Implications of the miR-10 family in chemotherapy response of NPM1-mutated AML. Blood 123(15):2412–2415
Houthuijzen JM et al (2012) The role of mesenchymal stem cells in anti-cancer drug resistance and tumour progression. Br J Cancer 106(12):1901–1906
Huang JC et al (2015) Mesenchymal stromal cells derived from acute myeloid leukemia bone marrow exhibit aberrant cytogenetics and cytokine elaboration. Blood Cancer J 5:e302
Isidori A et al (2014) The role of the immunosuppressive microenvironment in acute myeloid leukemia development and treatment. Expert Rev Hematol 7(6):807–818
Méndez-Ferrer S et al (2010) Mesenchymal and haematopoietic stem cells form a unique bone marrow niche. Nature 466(7308):829–834
Shi L et al (2015) Enhancement of the TCRζ expression, polyclonal expansion, and activation of T Cells from patients with AML after IL-2, IL-7, and IL-12 induction. DNA Cell Biol 34(7):481–488
Stölzel F et al (2010) Mechanisms of resistance against PKC412 in resistant FLT3-ITD positive human acute myeloid leukemia cells. Ann Hematol 89(7):653–662
Szczepanski MJ et al (2009) Increased frequency and suppression by regulatory T cells in patients with acute myelogenous leukemia. Clin Cancer Res 15(10):3325–3332
Takahashi H et al (2012) TGF-[beta] and retinoic acid induce the microRNA miR-10a, which targets Bcl-6 and constrains the plasticity of helper T cells. Nat Immunol 13(6):587–595
Varnholt H et al (2008) MicroRNA gene expression profile of hepatitis C virus–associated hepatocellular carcinoma. Hepatology 47(4):1223–1232
Wang X et al (2005) Increased population of CD4+ CD25high regulatory T cells with their higher apoptotic and proliferating status in peripheral blood of acute myeloid leukemia patients. Eur J Haematol 75(6):468–476
Zagaria A et al (2014) BCL6 corepressor gene dysregulation due to chromosomal translocation in acute myeloid leukemia: a new mechanism based on long non-coding RNA dislocation? Leuk Lymphoma 55(9):2199–2201
Zhang L et al (2006) microRNAs exhibit high frequency genomic alterations in human cancer. Proc Natl Acad Sci 103(24):9136–9141
Zhi F et al (2013) Identification of circulating microRNAs as potential biomarkers for detecting acute myeloid leukemia. PLoS One 8(2):e56718
Zhi Y et al (2015) Serum level of miR-10-5p as a prognostic biomarker for acute myeloid leukemia. Int J Hematol 102(3):296–303
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no actual or potential conflicts of interest to declare.
Research involving human participants and/or animals
The study was approved by the Ethic Committee of Qilu Hospital of Shandong University.
Informed consent
The written informed consent was obtained from subjects.
Rights and permissions
About this article
Cite this article
Yu, Z., Li, D. & Ju, Xl. CD4+ T cells from patients with acute myeloid leukemia inhibit the proliferation of bone marrow-derived mesenchymal stem cells by secretion of miR-10a. J Cancer Res Clin Oncol 142, 733–740 (2016). https://doi.org/10.1007/s00432-015-2076-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-015-2076-1