Abstract
Purpose
To evaluate the role of radioembolization and systemic chemotherapy as a combined modality therapy for unresectable colorectal liver metastases.
Patients and methods
Prospective database of a major yttrium-90 microsphere radioembolization treatment center in Sydney, Australia, that included 140 patients with unresectable colorectal liver metastases was analyzed. Tumor response, overall survival, treatment-related complications and an evaluation of its role as a combined modality therapy with systemic chemotherapy were performed.
Results
One hundred and thirty-three patients (95%) had a single treatment, and seven patients (5%) had repeated treatments. Response following treatment was complete in two patients (1%), partial in 43 patients (31%), stable in 44 patients (31%), and 51 patients (37%) developed progressive disease. Combining chemotherapy with radioembolization was associated with a favorable treatment response (P = 0.007). The median overall survival was 9 (95% CI 6.4–11.3) months with a 1-, 2-, and 3-year survival rate of 42, 22, and 20%, respectively. Primary tumor site (P = 0.019), presence of extrahepatic disease (P = 0.033), and a favorable treatment response (P < 0.001) were identified as independent predictors for survival.
Conclusion
Combined modality therapy appears to improve tumor response rates. Survival is influenced by tumor site, presence of extrahepatic disease, and response to therapy. Yttrium-90 microsphere radioembolization is safe and may best be combined with systemic chemotherapy for patients with unresectable colorectal liver metastases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The liver is the most common site of metastatic disease in colorectal cancer. Colorectal liver metastases (CLM) occur in 25% of patients at first diagnosis (Bengmark and Hafstrom 1969; Fong et al. 1996) and as a site of disease recurrence in 50–75% of patients after initial treatment (Kemeny and Fata 1999; Steele and Ravikumar 1989). Historical studies of patients with untreated CLM have demonstrated 1- and 3-year survival of 50 and 12%, respectively (Wood et al. 1976; Wagner et al. 1984). Today, it is universally accepted that hepatic resection of CLM is regarded as the standard of care (Khatri et al. 2005). This surgical option is available to an estimated 10–15% of patients with CLM, whose disease is considered resectable. There have been a number of strategies that include chemotherapy regimens and other innovative interventions that have expanded the criteria for resectability, rendering patients with previously unresectable disease resectable (Pawlik et al. 2008). After hepatic resection of CLM, results from tertiary referral centers have reported actual 10-year survival rate of up to 17%, which is regarded as the definition of cure (Tomlinson et al. 2007; Viganò et al. 2008). Hence, one in six sufferers of CLM who are candidates for hepatic resection may be cured. As a disease entity, however, resectable CLM represents only a small fraction of the entire population of CLM sufferers, for which the majority would have truly inoperable disease.
Current management of unresectable CLM involves improving tumor response rates with conversion systemic chemotherapy such that tumors may be adequately downsize to eventually undergo resection or resection with ablation (Adam et al. 2009; Folprecht et al. 2010). If downsizing to allow a hepatic resection is not feasible, continuous chemotherapy treatment even in combination with biological agents including bevacizumab and cetuximab for patients previously treated with standard chemotherapy would unlikely achieve a median survival that extends beyond 1 year (Giantonio et al. 2007; Sobrero et al. 2008). In patients with previously untreated metastatic colorectal cancer, treatment with oxaliplatin and Irinotecan regimen as FOLFOX or FOLFIRI may achieve median survival of up to 16 months (Saltz et al. 2000), and when combined with bevacizumab and cetuximab, the median survival may be further improved to 20 months (Hurwitz et al. 2004; Colucci et al. 2005; Cassidy et al. 2008; Porschen et al. 2007; Saltz et al. 2008; Falcone et al. 2007).
Hepatic arterial delivery of yttrium-90 microsphere takes advantage of the unique vasculature of the tumor whose blood supply is primarily derived from the hepatic artery. Microspheres lodge within the tumor vessel plexus, hence allowing selective radioembolization of tumor-bearing liver parenchyma where ionizing radiation of above 120 Gy to the tumor compartment may be achieved while maintaining a tolerable level of radiation exposure to the normal adjacent liver parenchyma (Campbell et al. 2001). Previously, this therapy was rigorously evaluated in trials with hepatic arterial chemotherapy, where it demonstrated synergistic effects between the loco-regional chemotherapy administration and the effects of radioembolization to improve tumor response rates (Gray et al. 2001). Hepatic artery catheter-related complications, risks of extrahepatic deposition of microspheres, and the propensity for extrahepatic disease recurrence in the metastatic setting pose a limitation of this therapeutic strategy (Allen et al. 2005).
Radioembolization when delivered in combination with systemic chemotherapy is hailed as a potentially advantageous option. Its use with effective systemic therapies of the current era may hold the promise of improving tumor response rates and overall survival in this palliative setting for patients with liver-dominant metastatic disease. The purpose of this large single institution study is to evaluate the response to treatment and survival outcomes, to report the complications of treatment, and to determine the relative efficacy when this therapy is adopted as a combined modality therapy with systemic chemotherapy or when used alone as a salvage therapy for patients with chemorefractory disease.
Materials and methods
Patient selection
One hundred and forty consecutive patients with unresectable colorectal liver metastases was referred to the interventional radiology unit of a tertiary treatment center for yttrium-90 microsphere radioembolization (SIR-spheres, Sirtex Medical, Sydney, Australia) between March 2006 and May 2009. Unresectability was due to insufficient estimated future liver remnant, vascular invasion, progression under chemotherapy, or an unresectable extrahepatic lesion. Patients with liver-dominant metastatic disease and limited extrahepatic metastases at one site, such as a solitary pulmonary metastasis, were not a contraindication for treatment.
Inclusion criteria were as follows: (a) radiologically proven liver metastasis from colorectal cancer not amenable to curative surgical resection; (b) aged 18–85 years; (c) ability to undergo angiography and selective visceral catheterization; (d) Eastern Cooperative Oncology Group (ECOG) performance status of 0–2; and (e) adequate hematology (granulocyte count ≥ 1.5 × 109/l, platelets ≥ 50 × 109/l), renal function (creatinine level ≤ 2.0 mg/dl), and hepatic function (bilirubin level ≤ 2.0 mg/dl).
Yttrium-90 microsphere radioembolization protocol
Prior to radioembolization, patients underwent routine baseline serology including liver function tests and computerized topography (CT) imaging scans of the liver. In addition, each patient underwent a liver angiography with 99m technetium-labeled macroaggregated albumin (99mTc-MAA) scintigraph to identify any aberrant hepatic anatomy and percentage of lung shunting. Temporary balloon occlusion was performed if arteriovenous lung shunting was >20% on 99mTc-MAA to reduce the risk of pneumonitis (Bester and Salem 2007). Activity of yttrium-90 microsphere treatment was measured in gigabecquerels (GBq) and adjusted to tumor volume and lung shunting fraction. Dosages were calculated according to patient surface area, as previously described (Salem and Thurston 2006). For patients who had concomitant systemic chemotherapy with 5-fluorouracil, the dosages were also based on patient surface area (225 mg/m2), with continuous infusion administered for 7 days as a radiosensitizer, commencing 1 day prior to radioembolization.
A standard dose of yttrium-90 radioactivity contains approximately 50 million resin microspheres measuring 29–35 μm each and provides 2 GBq. Yttrium-90 is a pure β emitter with a half-life of 64.2 h and decays into stable zirconium-90. The beta emission of yttrium-90 has a mean tissue penetration of 2.5 mm (maximum of 10 mm) and has an average energy emission of 0.937 MeV. The microspheres were injected through a temporary hepatic artery catheter placed percutaneously through the femoral or brachial artery. Unless contraindicated, treatment for bilobar liver disease was performed in the same procedure, with two-thirds of microspheres injected first into the right hepatic artery, followed by partial withdrawal and repositioning of the catheter into the left hepatic artery to allow the remaining one-third to be infused.
Following treatment, patients were hospitalized overnight. Patients were initially followed up after 1 month and then at 3-month intervals with abdominal CT scans performed at six-monthly interval until death.
Data acquisition
Clinical and treatment-related data were extracted from the database. Response to treatment was assessed by an experienced radiologist (L.B.) in accordance with the Response Criteria in Solid Tumors (RECIST) guidelines by comparison of each follow-up examination with the baseline examination (Therasse et al. 2000). In brief, a complete response (CR) is defined as disappearance of lesions; partial response (PR), as a ≥30% decrease in the sum of the longest diameter of the index lesions; stable disease (SD), as a <30% decrease or <20% increase in the sum of the longest diameter of the index lesions; and progressive disease (PD), as a ≥20% increase in the sum of the longest diameter of the index lesions or appearance of new lesions. Combined modality therapy was regarded as patients who receive concomitant chemotherapy or chemotherapy after radioembolization. Patients received combined modality therapy was described with the acronym Chemo-SIRT. Complications were recorded at two time intervals; immediate during days one to 30 (pain, nausea, vomiting, pneumonitis, gall bladder and biliary complications, gastritis, intestinal ulceration, and abdominal pain), delayed during days 30–90 (pneumonitis, gall bladder and biliary complications, intestinal ulceration, and radiation-induced liver dysfunction).
Statistical analysis
Clinical and treatment-related variables were analyzed for an association with favorable responders (complete response or partial response) and overall survival. Categorical variables were compared using χ2 analysis or Fisher’s exact test where appropriate. Survival analysis was performed by using Kaplan–Meier method and compared using the log-rank test. Multivariate analysis was performed using the binary logistic regression model and the Cox regression model. Statistical analyses were performed using the Statistical Package for Social Sciences for Windows (Version 16.0; SPSS GmbH, Munich Germany). A significant difference was defined as P < 0.05.
Results
Of 140 patients treated, there were 88 men (63%) and 52 women (37%). The median age of the cohort was 64 (range 37–85) years. The performance status of the patients scored according to the Eastern Cooperative Oncology Group scale was zero in 115 patients (82%), one in 19 patients (14%), two in four patients (3%), and three in two patients (1%). The primary tumor was located in the colon in 112 patients (80%) and rectum in 28 patients (20%). One hundred and thirty-three patients (95%) had a single treatment, and seven patients (5%) had repeated treatments. The extent of CLM was graded to involve 0–25% of the liver in 78 patients (55%), 26–50% of the liver in 50 patients (36%), and 51–75% of the liver in 12 patients (9%). Fourteen patients (10%) had unilobar metastases, and 126 patients (90%) had bilobar metastases. Hepatic resection of CLM was performed previously in 38 patients (27%), and ablation was performed in eight patients (6%). Extrahepatic disease was present in 51 patients (36%). The number of lines of chemotherapy treatment administered was zero in eight patients (6%), one in 72 patients (51%), two in 36 patients (26%), three in eight patients (6%), four in seven patients (5%), five in three patients (2%), and six in six patients (4%). The mean radiation dose was 1.8 (S.D. = 0.4) GBq. Forty-eight patients (34%) had concomitant or post-radioembolization chemotherapy after radioembolization. This is summarized in Table 1.
Treatment-related complications
There was no treatment-related mortality. Thirty-six patients (26%) developed early complications from treatment. Seven patients (5%) had nausea, one patient (1%) had vomiting, three patients (2%) had gastritis, one patient (1%) had intestinal ulceration, and 20 patients (14%) had abdominal pain. Delayed complications occurred in seven patients (5%); three patients (2%) developed radiation-induced liver dysfunction, four patients (3%) had intestinal ulceration, one patient (1%) had gall bladder- and biliary-related complication.
Treatment efficacy
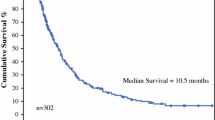
Following treatment, two patients (1%) had a complete response, 43 patients (31%) had a partial response, 44 patients (31%) had stable disease, and 51 patients (37%) had progressive disease. The overall median follow-up time was 9 (range 1–43) months. One hundred and three patients (74%) were deceased at last follow-up. The median follow-up time in the deceased patients was 6 (range 1–30) months. The median follow-up time in patients that are currently alive was 22 (range 10–43) months. The median overall survival was 9 (95% CI 6.4–11.3) months with a 1-, 2-, and 3-year survival rate of 42, 22, and 20%, respectively (Fig. 1).
Predictive factors for treatment response
To determine factors associated with a favorable treatment response (complete or partial response), 13 variables were entered into univariate analysis (Table 2). Factors associated with a favorable treatment response on univariate analysis include extent of liver metastases [favorable responses in 0–25% (41%), 26–50% (20%), 51–75% (25%); P = 0.039] and undergoing radioembolization as combined modality therapy with systemic chemotherapy (Chemo-SIRT) (favorable response for no 24%, yes 48%; P = 0.007). There was a trend toward significance for patients having prior liver resection (favorable responses for no 27%, yes 45%; P = 0.067). Multivariate analysis identified undergoing Chemo-SIRT as the single predictive factor for a favorable treatment response [hazard ratio (95% CI); 2.9 (1.3–6.1); P = 0.007] (Figs. 2, 3, 4).
Predictive factors for overall survival
From the univariate analysis, factors associated with an improved survival were sex (men 11 months, women 8 months; P = 0.034), site of the primary tumor (colon 9 months, rectum 7 months; P = 0.008), number of radioembolization treatment (one 8 months, more than one not reached; P = 0.048), number of lines of chemotherapy (≤2 lines 11 months, >2 lines 5 months; P = 0.006), Chemo-SIRT (no 7 months, yes 13 months; P = 0.017), and treatment response (unfavorable 6 months, favorable 30 months; P < 0.001) (Table 3). Factors P < 0.10 from univariate analysis were entered into the multivariate analysis. The site of the primary tumor [hazard ratio (95% CI); 1.7 (1.1–2.7); P = 0.019], presence of extrahepatic disease [hazard Ratio (95% CI); 0.6 (0.4–1.0); P = 0.033) and a favorable treatment response [hazard ratio (95% CI); 4.6 (2.7–7.8); P < 0.001)] were identified as independent predictors for survival (Table 3).
Discussion
The entity of unresectable colorectal liver metastases is managed aggressively with chemotherapy to achieve down-staging of the extent of liver metastases for subsequent liver surgery. In the CELIM randomized phase two trial of patients with unresectable CLM who were treated with modern chemotherapy with or without cetuximab, of 106 patients that commenced and completed systemic therapy, 49 patients were eventual candidates to liver surgery and underwent either resection or resection with ablation, achieving a rescue surgery rate of 46% (Folprecht et al. 2010). Adam et al. report a 5-year survival of 33% in a series of 184 consecutive patients with initially unresectable CLM who underwent hepatic resection after tumor downsizing by systemic chemotherapy (Adam et al. 2009). Although such reports of liver surgical treatments for CLM have dominated the literature, gaps continue to remain for the majority of patients who would not be eventually offered surgery. This study captures a cohort of patients in whom majority had advanced liver metastases that are unresectable following aggressive down-staging attempts, some of whom (27%) had developed disease recurrence following previous surgery. Further, the patients included have varying sensitivity to chemotherapy with 17% of patients currently receiving third-line chemotherapy. Therefore, this group of patients would be best regarded as undergoing palliative therapy for which radioembolization in this study serve as a salvage therapy.
Although trials of patients with metastatic colorectal cancer who have failed standard first-line fluorouracil chemotherapy and have gone onto receive modern chemotherapy as second-line therapy may achieve median survival of about 14 months with radiological response (CR/PR) rates of up to 28% (Kim et al. 2009), survival may be improved if modern chemotherapy is combined with biological therapy as shown in the EPIC trial where irinotecan was combined with cetuximab following failure of oxaliplatin-based chemotherapy and achieved response rates of 16% and median survival of 10.7 months. Responses and survival to systemic therapy are more inferior when non-standard agents are used in patients who have failed modern chemotherapy and bevacizumab therapy, with the sunitinib phase II trial showing only one partial response of 84 patients and a median overall survival time of 7 months (Saltz et al. 2007). As with these studies that report heavily pre-treated patients, in the 140 patients referred to us, 51% had failed first-line therapy, 26% of patients have failed second-line therapy, and 17% of patients have been on three or more lines of systemic therapy. Following radioembolization treatment, we achieve response rate of 32% and achieved a median survival of 9 months. The results of our treatment are consistent with survival following radioembolization as reported in a structured meta-analysis by Vente et al. (2009) who identified 19 studies of 792 patients who were treated with yttrium-90. Vente et al. 2009 reported that the median survival ranged from 6.7 to 17.0 months with variable response rates ranging between 12 and 91%.
In the study from the Wakefield Gastroenterology Centre (New Zealand), for whom majority of their 100 patients received hepatic arterial chemotherapy (HAC) after radioembolization, they demonstrate a median survival of 11 months and showed that receiving subsequent HAC was associated with improved survival (13 vs. 3 months; P = 0.002) (Stubbs et al. 2006). It has been proposed that a combined modality option involving systemic therapy and radioembolization may become a promising option in the armamentarium available for patients with metastatic colorectal cancer, for which the systemic route of chemotherapy delivery would address extra-hepatic disease present (Kuebler 2009; Nicolay et al. 2009). As with previous strategy of combination, of chemotherapy through HAC after radioembolization, our study is the first to report a series of patients who received combined modality therapy of radioembolization with concomitant or subsequent chemotherapy. In a proportion of patients (n = 48) who were receiving concomitant or had received systemic therapy after radioembolization, this led to improved tumor response rates to 48% and median survival of 13 months.
In our multivariate analysis, we identified that patients with colonic liver metastases had a more favorable survival outcome compared to patients with liver metastases from a rectal primary, patients with extrahepatic disease faired more poorly compared to patients with isolated liver metastases, and the response to therapy for which was grouped into favorable (complete/partial) versus unfavorable (stable/progression) being predictors of survival following radioembolization therapy. Salem et al. from the Rubert H. Lurie Comprehensive Cancer Center in their experience of 72 patients with unresectable CLM showed that ECOG performance status, extent of liver metastases, presence of extrahepatic disease, response to therapy and initial stage of colorectal cancer at diagnosis were associated with survival from a univariate analysis (Mary et al. 2009). The authors also showed that in patients who had received all three chemotherapy regimens (5FU, oxaliplatin, and irinotecan), the median survival was 9.4 months compared to 19.7 months for patients who still had active systemic therapy options available (Mary et al. 2009). Hence, this result together with results from the current study indicating that combined modality therapy may potentially positively influence outcome supports the notion that there are likely clinical benefits associated with radioembolization when performed in combination with systemic therapies especially in an early setting as opposed to its use in the chemorefractory setting as salvage therapy. The effectiveness of this therapy in down-staging the extent of liver metastases may demonstrate its suitability as a neoadjuvant bridging therapy to resection. However, the consequence of embolization, fibrotic changes, and associated radiotherapy-induced liver damage raises questions about the safety of hepatic resection post radioembolization (Fig. 5). In our experience, there was one patient who had received four treatments of radioembolization, who successfully underwent a right hepatectomy without major postoperative complication.
To the best of our knowledge, there are at least 10 phase II/III clinical trials of yttrium-90 microsphere radioembolization as treatment for unresectable CLM in various settings of the disease history. The results of our current study show that this therapeutic option is safe and effective. We provide evidence suggesting improved response and survival when used in combination with systemic therapy. We identified that patients with a colonic primary tumor, no extrahepatic disease, and patients who have responded to therapy achieved the greatest benefits. As we await the results of the ongoing clinical trials, our findings support the current evidence in the literature that this interventional oncologic therapy is becoming an increasingly attractive option in the interdisciplinary care of patients with liver-dominant metastatic colorectal cancer.
References
Adam R, Wicherts DA, de Haas RJ et al (2009) Patients with initially unresectable colorectal liver metastases: is there a possibility of cure? J Clin Oncol 27:1829–1835
Allen PJ, Nissan A, Picon AI et al (2005) Technical complications and durability of hepatic artery infusion pumps for unresectable colorectal liver metastases: an institutional experience of 544 consecutive cases. J Am Coll Surg 201:57–65
Bengmark S, Hafstrom L (1969) The natural history of primary and secondary malignant tumours of the liver. Cancer 23:198–202
Bester L, Salem R (2007) Reduction of arteriohepatovenous shunting by temporary balloon occlusion in patients undergoing radioembolization. J Vasc Interv Radiol 18:1310–1314
Campbell AM, Bailey IH, Burton MA (2001) Tumour dosimetry in human liver following hepatic 90Y microsphere therapy. Phys Med Biol 46:487–498
Cassidy J, Clarke S, Diaz-Rubio E et al (2008) Randomized phase III study of capecitabine plus oxaliplatin compared with fluorouracil/folinic acid plus oxaliplatin as first-line therapy for metastatic colorectal cancer. J Clin Oncol 26:2006–2012
Colucci G, Gebbia V, Paoletti G et al (2005) Phase III randomized trial of FOLFIRI versus FOLFOX4 in the treatment of advanced colorectal cancer: a multicenter study of the Gruppo Oncologico Dell’Italia Meridionale. J Clin Oncol 23:4866–4875
Falcone A, Ricci S, Brunetti I et al (2007) Phase III trial of infusional fluorouracil, leucovorin, oxaliplatin, and irinotecan (FOLFOXIRI) compared with infusional fluorouracil, leucovorin, and irinotecan (FOLFIRI) as first-line treatment for metastatic colorectal cancer: the Gruppo Oncologico Nord Ovest. J Clin Oncol 25:1670–1676
Folprecht G, Gruenberger T, Bechstein WO et al (2010) Tumour response and secondary resectability of colorectal liver metastases following neoadjuvant chemotherapy with cetuximab: the CELIM randomised phase 2 trial. Lancet Oncol 11:38–47
Fong Y, Kemeny N, Paty P et al (1996) Treatment of colorectal cancer: hepatic metastasis. Semin Surg Oncol 12:219–252
Giantonio BJ, Catalano PJ, Meropol NJ et al (2007) Bevacizumab in combination with oxaliplatin, fluorouracil, and leucovorin (FOLFOX4) for previously treated metastatic colorectal cancer: results from the Eastern Cooperative Oncology Group Study E3200. J Clin Oncol 25:1539–1544
Gray B, Van Hazel G, Hope M et al (2001) Randomised trial of SIR-Spheres® plus chemotherapy vs. chemotherapy alone for treating patients with liver metastases from primary large bowel cancer. Ann Oncol 12:1711–1720
Hurwitz H, Fehrenbacher L, Novotny W et al (2004) Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer [see comment]. N Engl J Med 350:2335–2342
Kemeny N, Fata F (1999) Arterial, portal or systemic chemotherapy for patients with hepatic metastasis of colorectal carcinoma. J Hepatobiliary Pancreat Surg 6:39–49
Khatri VP, Petrelli NJ, Belghiti J (2005) Extending the frontiers of surgical therapy for hepatic colorectal metastases: is there a limit? J Clin Oncol 23:8490–8499
Kim GP, Sargent DJ, Mahoney MR et al (2009) Phase III noninferiority trial comparing irinotecan with oxaliplatin, fluorouracil, and leucovorin in patients with advanced colorectal carcinoma previously treated with fluorouracil: N9841. J Clin Oncol 27:2848–2854
Kuebler JP (2009) Radioembolization of liver metastases in patients with colorectal cancer: a nonsurgical treatment with combined modality potential. J Clin Oncol 27:4041–4042
Mary FM, Robert JL, Saad MI et al (2009) Radioembolization of colorectal hepatic metastases using yttrium-90 microspheres. Cancer 115:1849–1858
Nicolay NH, Berry DP, Sharma RA (2009) Liver metastases from colorectal cancer: radioembolization with systemic therapy. Nat Rev Clin Oncol 6:687–697
Pawlik TM, Schulick RD, Choti MA (2008) Expanding criteria for resectability of colorectal liver metastases. Oncologist 13:51–64
Porschen R, Arkenau H-T, Kubicka S et al (2007) Phase III study of capecitabine plus oxaliplatin compared with fluorouracil and leucovorin plus oxaliplatin in metastatic colorectal cancer: a final report of the AIO Colorectal Study Group. J Clin Oncol 25:4217–4223
Salem R, Thurston KG (2006) Radioembolization with 90Yttrium microspheres: a state-of-the-art brachytherapy treatment for primary and secondary liver malignancies. Part 1: technical and methodologic considerations. J Vasc Interv Radiol 17:1251–1278
Saltz LB, Cox JV, Blanke C et al (2000) Irinotecan plus fluorouracil and leucovorin for metastatic colorectal cancer. Irinotecan Study Group [see comment]. N Engl J Med 343:905–914
Saltz LB, Rosen LS, Marshall JL et al (2007) Phase II trial of sunitinib in patients with metastatic colorectal cancer after failure of standard therapy. J Clin Oncol 25:4793–4799
Saltz LB, Clarke S, Diaz-Rubio E et al (2008) Bevacizumab in combination with oxaliplatin-based chemotherapy as first-line therapy in metastatic colorectal cancer: a randomized phase III study. J Clin Oncol 26:2013–2019
Sobrero AF, Maurel J, Fehrenbacher L et al (2008) EPIC: phase III trial of cetuximab plus irinotecan after fluoropyrimidine and oxaliplatin failure in patients with metastatic colorectal cancer. J Clin Oncol 26:2311–2319
Steele GJ, Ravikumar TS (1989) Resection of hepatic metastases from colorectal metastases: biologic perspectives. Ann Surg 210
Stubbs RS, O’Brien I, Correia MM (2006) Selective internal radiation therapy with 90Y microspheres for colorectal liver metastases: single-centre experience with 100 patients. ANZ J Surg 76:696–703
Therasse P, Arbuck SG, Eisenhauer EA et al (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216
Tomlinson JS, Jarnagin WR, DeMatteo RP et al (2007) Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol 25:4575–4580
Vente MA, Wondergem M, van der Tweel I et al (2009) Yttrium-90 microsphere radioembolization for the treatment of liver malignancies: a structured meta-analysis. Eur Radiol 19:951–959
Viganò L, Ferrero A, Lo Tesoriere R et al (2008) Liver surgery for colorectal metastases: results after 10 years of follow-up. Long-term survivors, late recurrences, and prognostic role of morbidity. Ann Surg Oncol 15:2458–2464
Wagner JS, Adson MA, Van Heerden JA et al (1984) The natural history of hepatic metastases from colorectal cancer. A comparison with resective treatment. Ann Surg 199:502–508
Wood CB, Gillis CR, Blumgart LH (1976) A retrospective study of the natural history of patients with liver metastases from colorectal cancer. Clin Oncol 2:285–288
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chua, T.C., Bester, L., Saxena, A. et al. Radioembolization and systemic chemotherapy improves response and survival for unresectable colorectal liver metastases. J Cancer Res Clin Oncol 137, 865–873 (2011). https://doi.org/10.1007/s00432-010-0948-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-010-0948-y